Volume 13, Issue 2 (Spring 2025)
PCP 2025, 13(2): 101-112 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hamidian S, Sharifi A, Azimian M, Shakiba S. A Comprehensive Approach to Psychological Challenges in Patients With Multiple Sclerosis: The Role of Transdiagnostic Factors and Demographic Variables. PCP 2025; 13 (2) :101-112
URL: http://jpcp.uswr.ac.ir/article-1-994-en.html
URL: http://jpcp.uswr.ac.ir/article-1-994-en.html
1- Clinical Research Development Center, Rofeideh Rehabilitation Hospital, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Department of Psychological, Faculty of Psychology and Education, University of Tehran, Tehran, Iran.
3- Multiple Sclerosis Clinic, Rofeideh Rehabilitation Hospital, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
4- Department of Clinical Psychology, School of Behavioral Sciences and Mental Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,sh.shakiba@uswr.ac.ir
2- Department of Psychological, Faculty of Psychology and Education, University of Tehran, Tehran, Iran.
3- Multiple Sclerosis Clinic, Rofeideh Rehabilitation Hospital, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
4- Department of Clinical Psychology, School of Behavioral Sciences and Mental Health, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. ,
Keywords: Multiple sclerosis (MS), Mood disorders, Anxiety disorders, Transdiagnostic factors, Demographic variables, Rehabilitation studies
Full-Text [PDF 737 kb]
(403 Downloads)
| Abstract (HTML) (2028 Views)
Full-Text: (228 Views)
Introduction
Multiple sclerosis (MS) is a chronic progressive degenerative disease in the central nervous system (CNS) that causes disability in young adults. While the worldwide prevalence and incidence of MS have been reported to be 35.9 and 2.1/100000 (Walton et al., 2020), this ratio in Iran ranges from 5.3 to 89/100000 and 7 to 148.1/100000, respectively (Azami et al., 2019). This rate is predominantly higher than what its geographical position had previously suggested, and at the moment, Iran is well known for its high prevalence of MS in the world (Hosseinzadeh et al., 2019).
In recent years, many studies have considered neuropsychiatric manifestations in MS (Ron, 2018; Shail, 2017). The close relationship between neurological disorders and psychiatric disorders provides an opportunity to understand the pathophysiology of psychiatric disorders through medical illnesses. Considering the hypothesis that activation and degeneration of the immune system may affect oxidative processes in the CNS, recent attention has been paid to the association of psychiatric disorders with the immune system and neurological degenerative disorders (Carta et al., 2014). Haussleiter et al. (2009) acknowledged that the demyelination of nerve fibers affects not only the functioning of sensory and motor systems but also causes psychiatric pathological symptoms. Although the etiology of MS is not clear, there is no doubt that stress and psychological factors play an important role in exacerbating the disease and aggravating the subsequent neurological disability (McKay et al., 2018).
Comorbid psychiatric disorders in MS are shown to be associated with poorer quality of life, higher levels of fatigue and functional disability, decreased treatment adherence, and also increased severity of subsequent neurologic disability (McKay et al., 2018; Sarısoy et al., 2013). The importance of exploring psychiatric aspects of MS becomes even more critical when the studies reported that suicidal behaviors in patients with MS (PwMS) are up to two times higher than in the general population (Feinstein & Pavisian, 2017).
Depression and, to a lesser extent, anxiety disorders have been shown to affect PwMS significantly more than the general population. The prevalence of depression in PwMS is reported to be 3.80% to 68.4%, while it is about 15% in the general population (Marrie et al., 2015).
The significant burden of depression on patients involves impaired cognitive performances, fatigue, lower quality of life, physical disability, and sleep disturbances (Sparaco et al., 2021). Depression has also been associated with patients’ withdrawal from disease-modifying treatments (Turner et al., 2016).
Compared to the considerable amount of literature on mood disorders in MS, lesser attention has been paid to anxiety disorders. The most common anxiety disorders in PwMS are GAD, with a lifetime prevalence of 18.6% (Uguz et al., 2008), and obsessive-compulsive disorder (OCD) with 15% (Foroughipour et al., 2012). A systematic review by Marrie et al. reported the prevalence of diagnosed anxiety ranged from 1.24% to 36% in PwMS compared to the 19% lifetime prevalence in the general population (Marrie et al., 2015). Anxiety disorders in MS are associated with chronic pain, fatigue, suicidal ideation, and both objective and subjective cognitive dysfunction. Anxiety may also predict higher levels of future wheelchair dependence and decreased productivity at work. In addition, anxiety disorders may also reduce adherence to disease-modifying therapies, which can lead to increased morbidity and poorer quality of life (Litster et al., 2016).
In MS, transdiagnostic factors like emotion regulation and resilience play a pivotal role in determining psychological outcomes. Depending on patients’ capacities in these areas, they can act as protective factors, promoting well-being or as vulnerabilities contributing to psychiatric symptoms. Despite the high prevalence of mental health issues among MS patients, some individuals remain resilient, highlighting the importance of identifying factors that safeguard psychological cohesion and mitigate adverse outcomes (Chwastiak & Ehde, 2007).
Emotion regulation, a key transdiagnostic factor, underlies many psychiatric disorders, including depression, GAD, and OCD, often linked to difficulties in processing emotional information (Heinsch et al., 2020; Ouellet et al., 2019; Villalobos et al., 2021; Yap et al., 2018). Similarly, resilience enhances adaptive coping and protects against chronic stressors, preserving mental health and preventing the onset and persistence of psychiatric symptoms (Taylor & Carr, 2021). Hopefully, targeted training can strengthen resilience, offering a promising pathway for improving psychological outcomes in individuals with chronic disabilities (Koelmel et al., 2017).
Furthermore, in PwMS, the concept of ability/disability is affected by physical health and subjective representation. There is some evidence that in chronic disease conditions, comorbid depression may negatively influence the patient’s description of their disability due to the disease. So, the perceived disability (PDS) of the patient is another variable that is thought to interact with psychiatric symptoms in PwMS (Smith & Young, 2000).
In this study, we aim to investigate the interaction between psychological symptoms, transdiagnostic factors, and demographic variables in PwMS, as well as their impact on patients’ PDS.
Materials and Methods
Participants and procedure
Patients with MS referred to the two centers of Rofeideh Rehabilitation Hospital and the Tehran MS Society, Tehran City, Iran, were recruited for this study, totaling 154 participants. An expert neurologist diagnosed MS in this group. The inclusion criteria required participants to be literate and willing to join the study. In contrast, the exclusion criteria included severe cognitive impairments affecting comprehension, diagnosis of other neurological conditions such as epilepsy, a history of traumatic brain injury or stroke, and the use of psychotropic drugs. After recruitment, the interviewer explained the study procedure and sought patient cooperation. Those who agreed signed a consent form and completed the scales. For participants with significant physical or psychological disabilities, questionnaires were read aloud by the caregiver or interviewer, who recorded the patients’ responses.
Study measures
Demographic data form
The demographic data form is a researcher-made form designed to gather demographic information about the patients and disease-specific variables such as disease duration in terms of years, AoO, and the number of hospitalizations (nHP) during the disease period.
PDS
Patients were asked a 5-point Likert question to measure their PDS due to the illness. The question was, “Which score better describes your disability due to having MS disease?”
The Yale-Brown obsessive-compulsive scale (Y-BOCS)
Symptom checklist (SC) and severity scale (SS) of the Yale-Brown obsessive-compulsive scale (Y-BOCS) were used. The SC consists of 58 questions that measure obsessions and compulsions in a 5-point Likert scale. The SS measures the severity of symptoms and their degree of interference with everyday life (Esfahani et al., 2012). The internal consistency of the two parts of SC and SS was 0.97 and 0.95, respectively. Split-half reliability values for SC and SS were 0.93 and 0.89, respectively, and test re-test reliability was 0.99. There was a positive correlation between SC and SCL-90-R-OCS (the symptom checklist-90-revised: Obsessive-compulsive subscale) and SS with scid-i (the structured clinical interview for DSM) (P>0.001) (Esfahani et al., 2012). In the present study, the Cronbach α values for obsessions, compulsions, and total symptoms were 0.95, 0.94, and 0.97, respectively.
Beck depression inventory-2 (BDI-II)
The BDI-II has 21 questions, each measuring one of the depression symptoms. As a result, a score is obtained that varies from 0 to 63, and higher scores represent greater severity of depression. The reliability coefficient for 21 items is equal to 0.913. The correlation coefficient between BDI-II scores and the brief symptom inventory-depression scale has been reported to be -0.873 (Hamidian et al., 2016). In the present study, the Cronbach α was calculated as 0.93.
Generalized anxiety disorder 7-item (GAD-7) scale
The GAD-7 scale is a self-administered questionnaire and is used as a screening tool and severity measure for GAD. The psychometric properties of a group of the Iranian population were as follows: The internal consistency measured with the Cronbach α was 0.87. A moderate to strong correlation with the hospital anxiety and depression scale was obtained for the anxiety (r=0.782) and depression (r=0.524) subscales and with the Penn State worry questionnaire (r=0.605), confirming convergent validity (Omani-Samani et al., 2018). In the present study, the Cronbach α was 0.92.
Difficulties in emotion regulation scale (DERS)
The DERS is a 36-item, multidimensional, self-report questionnaire that assesses 6 subscales: Not accepting the emotional responses, problems in performing the behaviors leading to one’s goal, impulse control problems, lack of emotional awareness, limitation in finding emotion regulation strategies, and lack of emotional clarity. The reliability of the questionnaire in the Iranian population was calculated using split-half and Cronbach α methods, which were respectively 0.86 and 0.8 for the whole questionnaire (P<0.01), indicating acceptable coefficients for the questionnaire (Hamidian et al., 2016). In the present study, the Cronbach α value was 0.85.
Connor-Davidson resilience scale (CDRS)
The CDRS is a 25-item questionnaire that measures resiliency on a 5-point Likert scale. The psychometric properties of this scale have confirmed its reliability and validity. For the Iranian population, the reliability using the Cronbach α was reported to be 0.89. The results of exploratory factor analysis have confirmed five factors: Personal competence, high standards, and tenacity; trust in one’s instincts, tolerance of negative affect, and strengthening effects of stress; the positive acceptance of change and secure relationships; control; and spiritual influences (Samani et al., 2007). In the present study, the Cronbach α was 0.95.
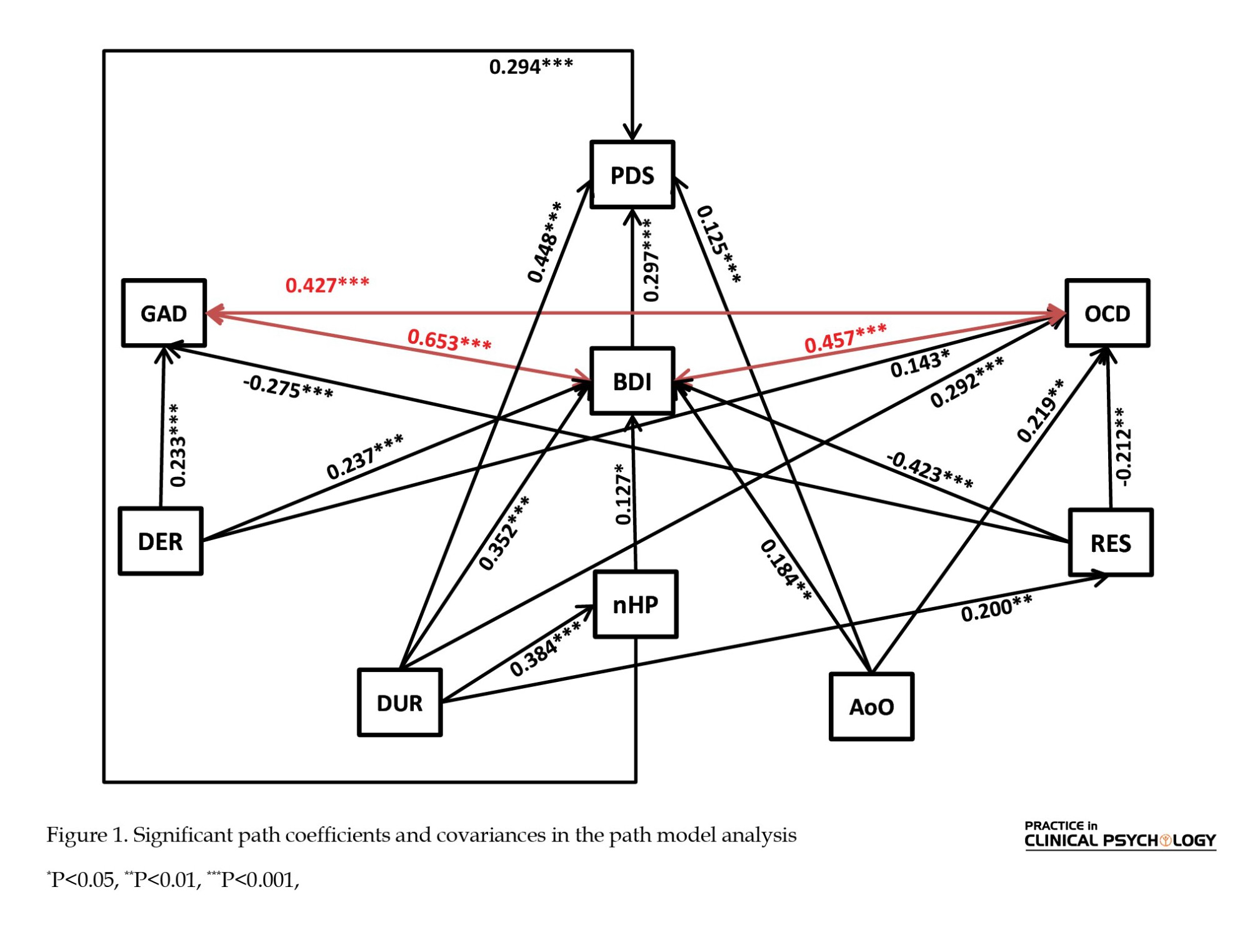
The proposed model
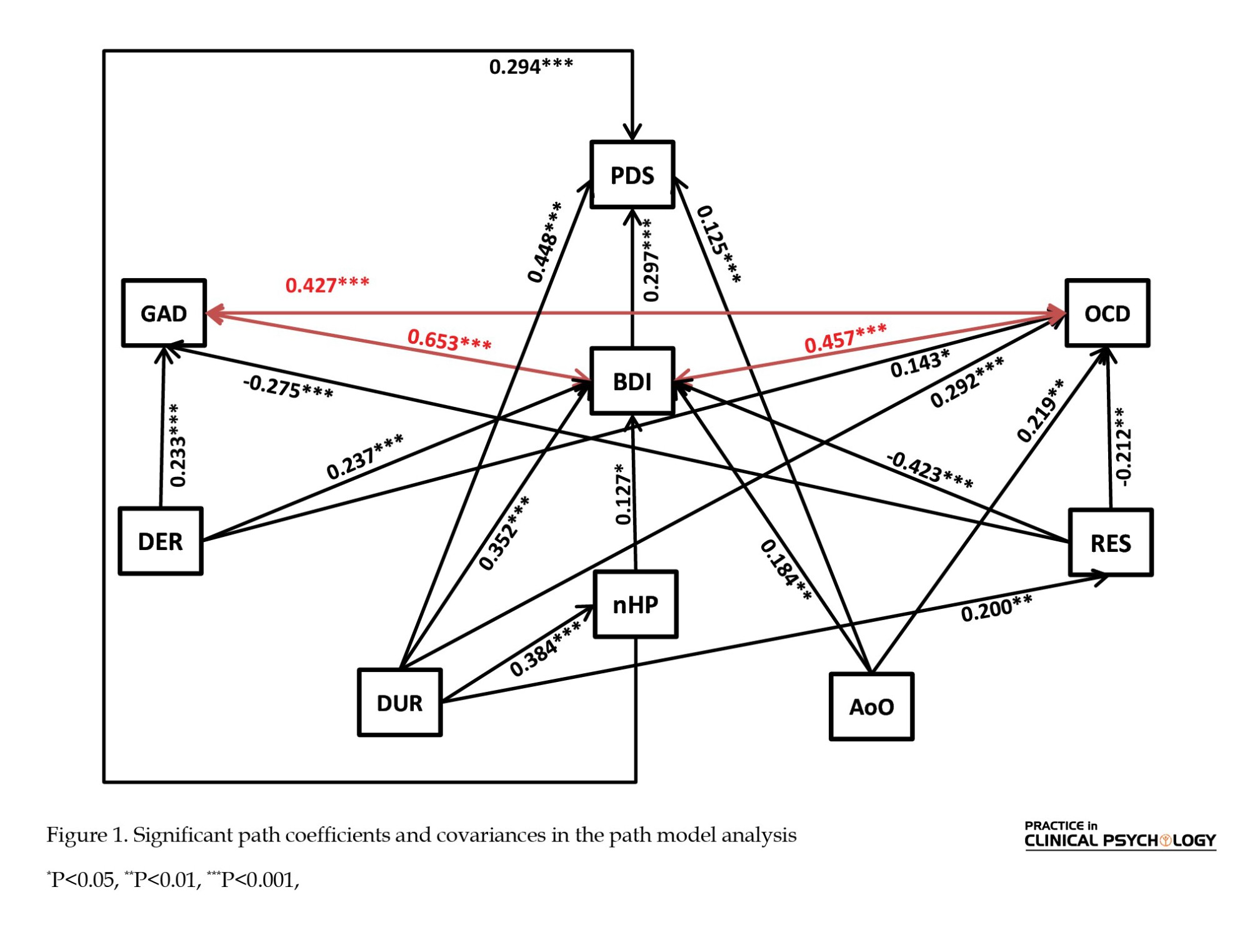
The purpose of this study is to investigate how patients’ psychiatric symptoms interact with their psychological profile and demographic characteristics and how these factors predict patients’ perceptions of their disability. For this purpose, the patient’s symptoms of depression (MDD), obsession and compulsion (OCD), and general anxiety (GAD) were evaluated to realize the patient’s psychological vulnerability. In contrast, resilience (RES) and difficulty in emotion regulation (DER) were assessed to achieve their psychological profile. In addition, the age of MS onset (AoO), duration of MS (DUR), and patient’s nHP were used as a descriptor of demographic characteristics, and PDS stands for the patient’s PDS. Figure 1 illustrates the proposed model. Covariances between variables are shown with the red double-headed arrows.
Study hypotheses
Hypothesis 1: Patients’ psychological resilience contributes to milder symptoms of psychological vulnerabilities (depression, GAD, and OCD symptoms).
Hypothesis 2: Patients’ DER contributes to more severe psychological vulnerabilities (depression, GAD, and OCD symptoms).
Hypothesis 3: Patients’ demographic characteristics (nHPs, disease duration, and AoO) contribute to more severe psychological vulnerabilities (depression, GAD, and OCD symptoms).
Hypothesis 4: Patients’ psychological vulnerabilities (depression, GAD, and OCD symptoms) contribute to a more severe perception of their disability.
Hypothesis 5: Patients’ psychological resilience contributes to a milder perception of their disability directly and indirectly.
Hypothesis 6: Patients’ DER contributes to a more severe perception of their disability directly and indirectly.
Hypothesis 7: The patient’s demographic characteristics (nHPs, disease duration, and AoO) contribute to the perception of their disability directly and indirectly.
Statistical analysis
For the path analysis of the proposed model, weighted least squares estimation (also known as asymptotically distribution-free estimation) was employed using the lavaan package in R programming language and environment for statistical computations (Rosseel, 2012; Team, 2013). For estimation, robust standard errors and adjusted mean and variance are used. To ascertain model fit, we used the chi-square test (χ2), the comparative fit index (CFI), the Tucker-Lewis index (TLI), the normative fit index (NFI), the root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR).
Results
Table 1 depicts the participants’ sociodemographic characteristics and MS profile.
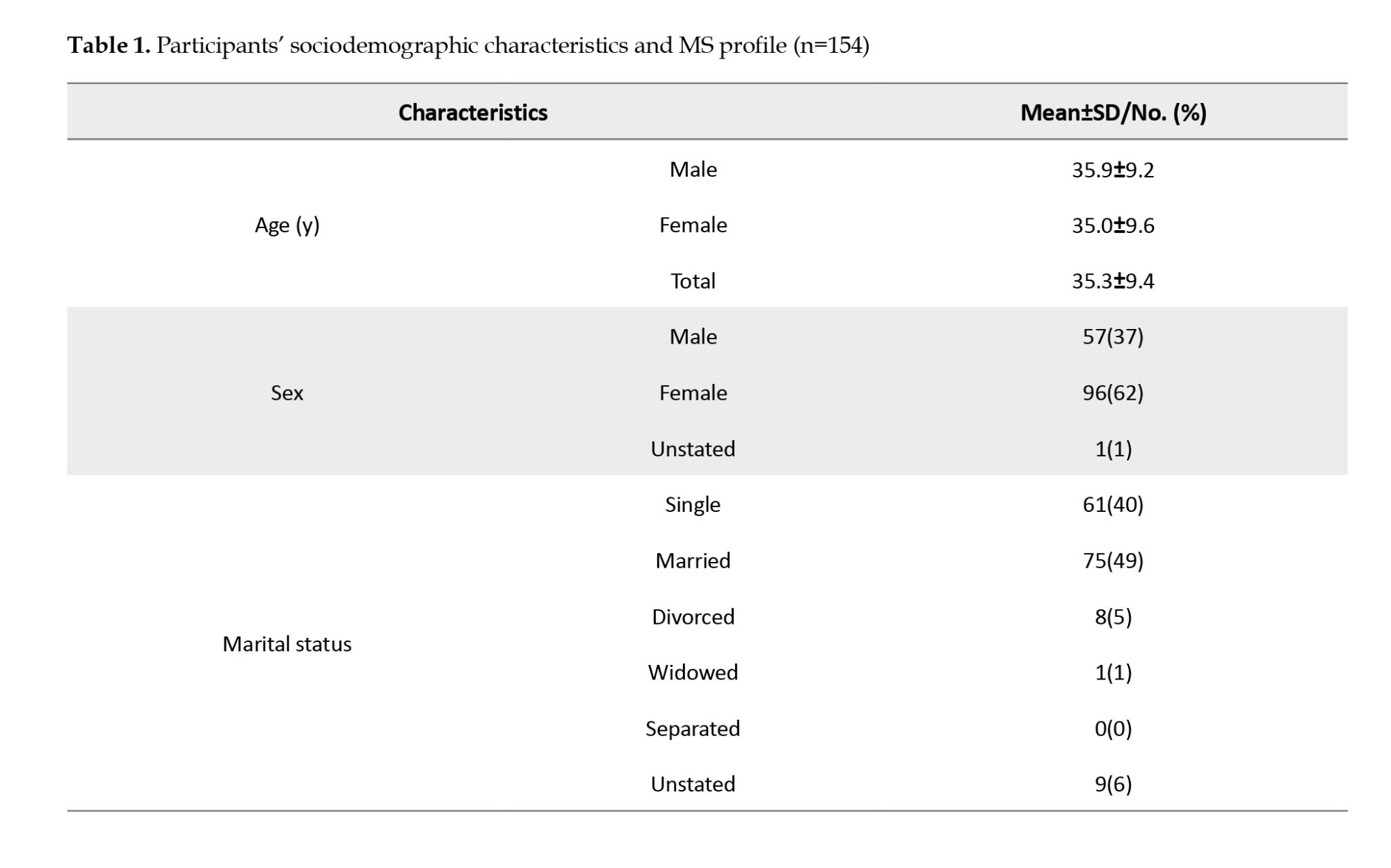
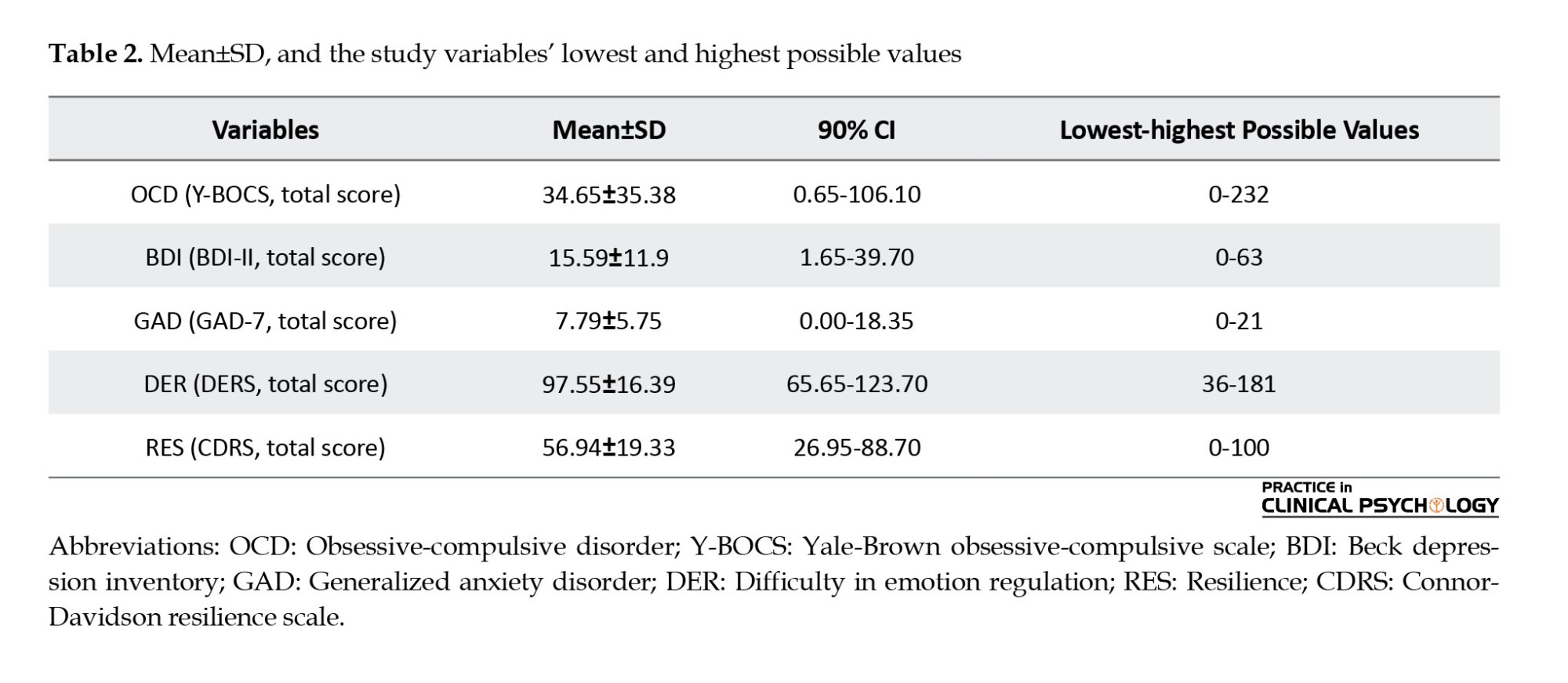
Table 2 presents the Mean±SD, and 90% CI values for OCD, BDI, GAD, DER, and RES. The lowest and highest possible values for each variable are also presented.
Based on Table 3, the path model analysis of the proposed model produced an excellent fit. The model accounted for 62% of the variance in PDS, 36% of the variance in BDI, 18% of the variance in OCD, and 16% of the variance in GAD.
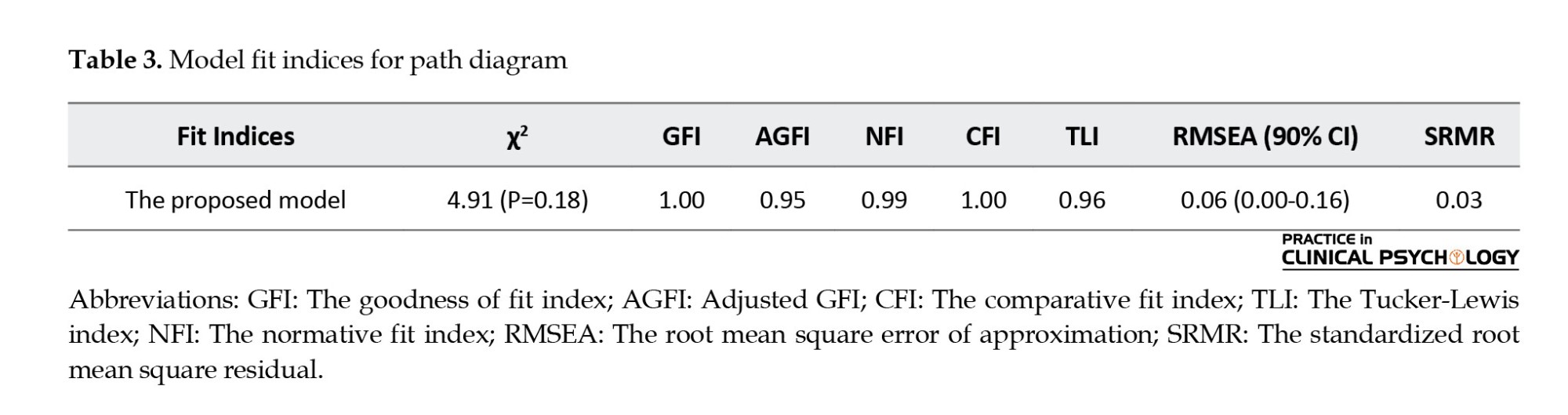
Figure 1 demonstrates significant direct path coefficients and covariances found in the path model analysis of the proposed model.
According to Figure 1 and regarding the demographic variables, higher AoO (β=0.125, P<0.001) was found to directly contribute to BDI (β=0.184, P<0.01), OCD (β=0.219, P<0.01) and PDS (β=0.125, P<0.001) among PwMS. Based on Table 4, its indirect effect (β=0.055, P<0.05) through the mediating role of BID was also statistically significant; therefore, both direct and indirect effects of AoO are valid.
The nHPs (β=0.294, P<0.001) contributed directly to PDS; however, its indirect effect was not significant. Therefore, only the direct impact of the nHPs is valid.
DUR has the strongest direct effect on BDI (β=0.352, P<0.001), OCD (β=0.292, P<0.001), and PDS (β=0.448, P<0.001). Moreover, based on Table 4, its indirect effects through the mediating role of nHP (β=0.113, P<0.001) and BDI (β=0.106, P<0.01) were also found significant. Overall, DUR’s total effect on PDS was also significant (β=0.666, P<0.001). In this regard, it is possible to say that both direct and indirect impacts of MS duration are valid.
In addition, regarding the psychological profile, RES negatively and DER positively contribute to more severe psychiatric symptoms, including BDI, OCD, and GAD. Figure 1 also shows that BDI (β=0.297, P<0.001) contributes to a perception of a more severe disability (PDS) among PwMS, while no such relation was found between either GAD or OCD with PDS. On the other hand, and based on Table 4, with the mediation role of BDI, RES (β=-0.126, P<0.001) and DER (β=0.07, P<0.05) were found to indirectly contribute to a milder and a more severe PDS among these patients respectively. Therefore, RES and DER directly affect BDI and indirectly affect PDS.
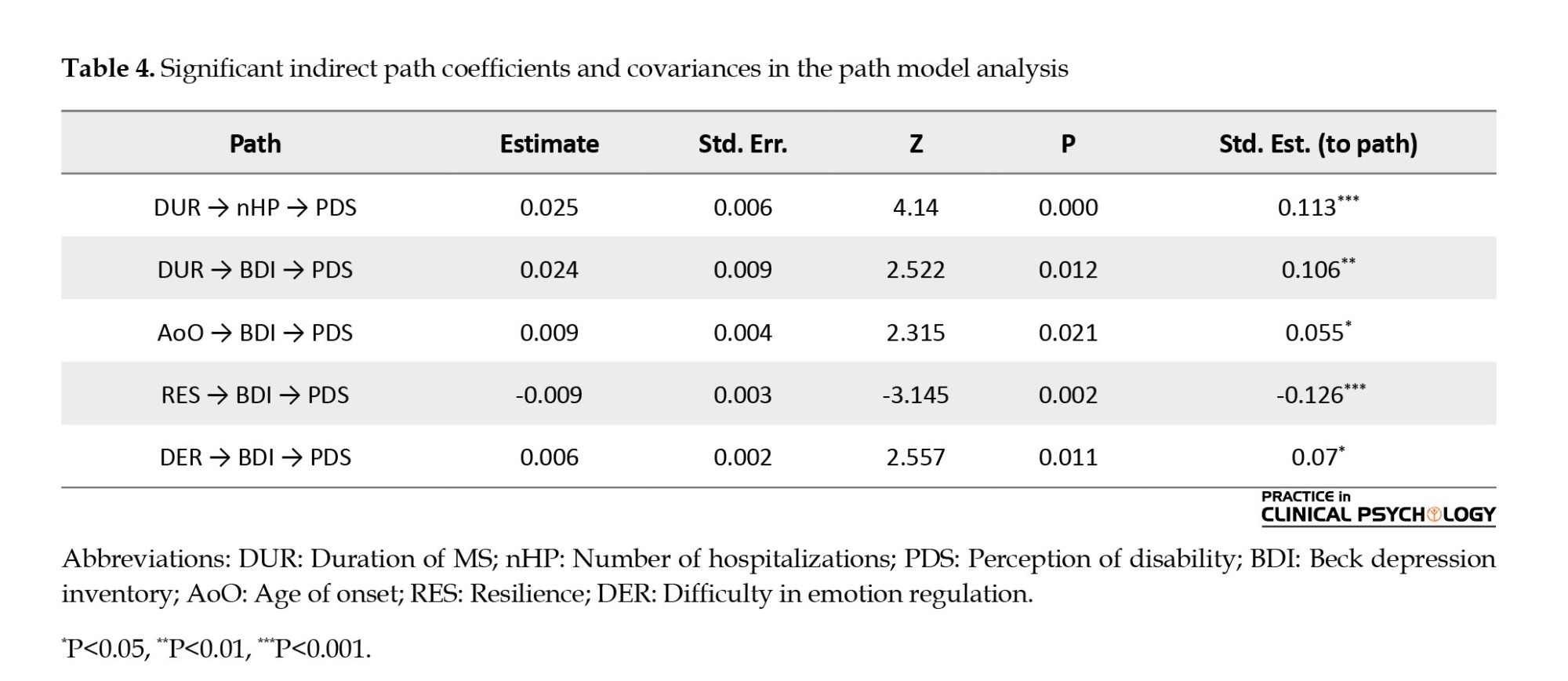
Table 4 shows the path model analysis’s significant indirect path coefficients and covariances.
Table 4 suggests that MS chronicity impacts patients’ PDS through increased hospitalizations and depression. Additionally, low resilience and difficulties in emotion regulation are risk factors for a heightened PDS.
Discussion
The results of the present study strongly support our hypothesis about the role of patients’ psychological vulnerabilities (depression, GAD, and OCD symptoms) in a more severe PDS. In PwMS, being more resilient and having more trouble in emotion regulation could predict psychiatric symptoms. These findings show the negative direct effect of resilience on the development of depression, anxiety, and OCD symptoms, which corroborated the studies of Nakazawa et al. (2018). The results are also in keeping with Prakash et al. (2019) on the impact of emotion regulation strategies in developing depression and anxiety symptoms. These observations also replicate the broader literature on the correlation of these two transdiagnostic variables with psychiatric symptoms which have been formerly reported in the general population among a group of PwMS (Gürcan-Yıldırım & Gençöz, 2020; Min et al., 2015).
Depression and OCD have also shown a correlation with the AoO. As per the previous studies, the AoO of MS is associated with anatomical factors such as ventricle expansion (Jakimovski et al., 2020) and physical indexes such as disability (Ramachandran et al., 2014). In the present study, the results suggest the older AoO as a risk factor for developing depression and OCD symptoms.
Both transdiagnostic and demographic factors play a significant role in the development of depression, which in turn directly influences patients’ PDS. This finding aligns with previous research by Janssens et al. (2003) and Smith & Young, (2000), which reported that depression mediates the relationship between disability and quality of life while also amplifying individuals’ perception of their disability. The results suggest that transdiagnostic and demographic variables impact disability primarily through depression’s decisive mediating role, highlighting the initial links in this chain of influence.
Moreover, the model underscores the significant role of disease duration in the onset of psychiatric disorders such as depression, anxiety, and OCD. Previous studies have established a correlation between MS duration and factors like disability severity (Mohaghegh et al., 2021), quality of life (Karatepe et al., 2011), and the use of active coping strategies, which are associated with better psychological outcomes(Holland et al., 2019). Consistent with these findings, the present study confirms the predictive role of disease duration in the presence of psychiatric symptoms. Considering the nHPs as an indicator of severity and disease duration as a measure of chronicity, it appears that chronicity plays a more substantial role in the development of psychiatric symptoms (Shahwar & Kidwai, 2020). This condition, in turn, increases an individual’s PDS.
Resilience plays a crucial role in mitigating psychiatric disorders, as demonstrated by several studies (Koelmel et al., 2017; Nakazawa et al., 2018). In MS, chronicity is strongly linked to the onset of psychiatric symptoms unless a modifying factor alters this relationship. In this model, resilience, shaped by specific traits and skills, can buffer the impact of disease duration on depression.
While MS chronicity contributes to psychiatric symptom development, resilience acts as a protective factor, slowing this progression. As the disease advances, adopting a resilient mindset becomes increasingly important for coping. Without it, the risk of depression, anxiety, and obsessive-compulsive symptoms rises over time, consistent with Kim et al. (2019) on the role of resilience in patients with chronic disease. Thus, disease duration serves as a warning factor; as hospitalizations increase and PDS intensifies, adapting to chronic illness becomes more challenging, making psychiatric symptoms more likely to emerge.
In other words, whilst the chronicity in MS plays a pivotal role in the development of psychiatric symptoms, the resilience factor can play the role of a preventive element that decelerates this process. This means that the more the disease progresses, the faster the person needs to acquire a resilient viewpoint to cope with it. If it does not happen, the risk of incidence of psychiatric symptoms, including depression, anxiety, and obsessive-compulsive symptoms, increases over time. Hence, disease duration is an alarming factor; as time passes and the nHPs and the person’s PDS increases, implementing strategies that enable the person to adapt to the chronic illness and be resilient is getting harder to achieve, and this is where the symptoms of psychiatric disorders start to emerge.
About the emotional regulation variable, such a correlation to the disease duration was not observed, but emotional regulation was directly and strongly correlated with depression and anxiety. From a therapeutic perspective, this skill is not only involved in symptom presentation but also as a transdiagnostic construct that should be included in any treatment planning for patients with MS. This is in line with previous studies (Fitzgerald et al., 2019; Sloan et al., 2017) suggesting that emotion regulation reflects shared neural mechanisms across both anxiety and depression, highlighting its critical role as a transdiagnostic construct. Such findings reinforce the importance of addressing emotion regulation in treatment planning for various psychological conditions, including MS.
Conclusion
These findings highlight the critical need for early mental health interventions in the management of MS, mainly focusing on resilience and emotion regulation. As psychiatric symptoms, especially depression, significantly influence PDS and disease progression, addressing these psychological factors from the outset of diagnosis can prevent further complications. The protective role of emotion regulation and resilience emphasizes the importance of incorporating psychological strategies into treatment plans, aiming to mitigate the onset of anxiety, depression and other psychiatric symptoms. Integrating these approaches early in the disease trajectory can ultimately enhance the psychological well-being and overall quality of life of individuals with MS.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1396.375). All patients signed the Informed consent form before data collection
Funding
Clinical Research Development Center of Rofeideh Rehabilitation Hospital, Tehran, Iran, financially supported the present study.
Authors' contributions
Study design and data interpretation: Shima Shakiba, and Sajedeh Hamidian; Referring patients: Ahmad Sharifi; Data collection: Shima Shakiba, Sajedeh Hamidian and Ahmad Sharifi; Data analysis: Ahmad Sharifi; Writing the original draft: Sajedeh Hamidian and Ahmad Sharifi; Review and editing: Shima Shakiba.
Conflict of interest
The authors declared no competing interests.
Acknowledgments
The authors thank the Clinical Research Development Center of Rofeideh Rehabilitation Hospital, Tehran, Iran, for their support, cooperation, and assistance throughout the study. Additionally, The authors sincerely thank all the participants for their time, effort, and valuable contributions to this research.
References
Multiple sclerosis (MS) is a chronic progressive degenerative disease in the central nervous system (CNS) that causes disability in young adults. While the worldwide prevalence and incidence of MS have been reported to be 35.9 and 2.1/100000 (Walton et al., 2020), this ratio in Iran ranges from 5.3 to 89/100000 and 7 to 148.1/100000, respectively (Azami et al., 2019). This rate is predominantly higher than what its geographical position had previously suggested, and at the moment, Iran is well known for its high prevalence of MS in the world (Hosseinzadeh et al., 2019).
In recent years, many studies have considered neuropsychiatric manifestations in MS (Ron, 2018; Shail, 2017). The close relationship between neurological disorders and psychiatric disorders provides an opportunity to understand the pathophysiology of psychiatric disorders through medical illnesses. Considering the hypothesis that activation and degeneration of the immune system may affect oxidative processes in the CNS, recent attention has been paid to the association of psychiatric disorders with the immune system and neurological degenerative disorders (Carta et al., 2014). Haussleiter et al. (2009) acknowledged that the demyelination of nerve fibers affects not only the functioning of sensory and motor systems but also causes psychiatric pathological symptoms. Although the etiology of MS is not clear, there is no doubt that stress and psychological factors play an important role in exacerbating the disease and aggravating the subsequent neurological disability (McKay et al., 2018).
Comorbid psychiatric disorders in MS are shown to be associated with poorer quality of life, higher levels of fatigue and functional disability, decreased treatment adherence, and also increased severity of subsequent neurologic disability (McKay et al., 2018; Sarısoy et al., 2013). The importance of exploring psychiatric aspects of MS becomes even more critical when the studies reported that suicidal behaviors in patients with MS (PwMS) are up to two times higher than in the general population (Feinstein & Pavisian, 2017).
Depression and, to a lesser extent, anxiety disorders have been shown to affect PwMS significantly more than the general population. The prevalence of depression in PwMS is reported to be 3.80% to 68.4%, while it is about 15% in the general population (Marrie et al., 2015).
The significant burden of depression on patients involves impaired cognitive performances, fatigue, lower quality of life, physical disability, and sleep disturbances (Sparaco et al., 2021). Depression has also been associated with patients’ withdrawal from disease-modifying treatments (Turner et al., 2016).
Compared to the considerable amount of literature on mood disorders in MS, lesser attention has been paid to anxiety disorders. The most common anxiety disorders in PwMS are GAD, with a lifetime prevalence of 18.6% (Uguz et al., 2008), and obsessive-compulsive disorder (OCD) with 15% (Foroughipour et al., 2012). A systematic review by Marrie et al. reported the prevalence of diagnosed anxiety ranged from 1.24% to 36% in PwMS compared to the 19% lifetime prevalence in the general population (Marrie et al., 2015). Anxiety disorders in MS are associated with chronic pain, fatigue, suicidal ideation, and both objective and subjective cognitive dysfunction. Anxiety may also predict higher levels of future wheelchair dependence and decreased productivity at work. In addition, anxiety disorders may also reduce adherence to disease-modifying therapies, which can lead to increased morbidity and poorer quality of life (Litster et al., 2016).
In MS, transdiagnostic factors like emotion regulation and resilience play a pivotal role in determining psychological outcomes. Depending on patients’ capacities in these areas, they can act as protective factors, promoting well-being or as vulnerabilities contributing to psychiatric symptoms. Despite the high prevalence of mental health issues among MS patients, some individuals remain resilient, highlighting the importance of identifying factors that safeguard psychological cohesion and mitigate adverse outcomes (Chwastiak & Ehde, 2007).
Emotion regulation, a key transdiagnostic factor, underlies many psychiatric disorders, including depression, GAD, and OCD, often linked to difficulties in processing emotional information (Heinsch et al., 2020; Ouellet et al., 2019; Villalobos et al., 2021; Yap et al., 2018). Similarly, resilience enhances adaptive coping and protects against chronic stressors, preserving mental health and preventing the onset and persistence of psychiatric symptoms (Taylor & Carr, 2021). Hopefully, targeted training can strengthen resilience, offering a promising pathway for improving psychological outcomes in individuals with chronic disabilities (Koelmel et al., 2017).
Furthermore, in PwMS, the concept of ability/disability is affected by physical health and subjective representation. There is some evidence that in chronic disease conditions, comorbid depression may negatively influence the patient’s description of their disability due to the disease. So, the perceived disability (PDS) of the patient is another variable that is thought to interact with psychiatric symptoms in PwMS (Smith & Young, 2000).
In this study, we aim to investigate the interaction between psychological symptoms, transdiagnostic factors, and demographic variables in PwMS, as well as their impact on patients’ PDS.
Materials and Methods
Participants and procedure
Patients with MS referred to the two centers of Rofeideh Rehabilitation Hospital and the Tehran MS Society, Tehran City, Iran, were recruited for this study, totaling 154 participants. An expert neurologist diagnosed MS in this group. The inclusion criteria required participants to be literate and willing to join the study. In contrast, the exclusion criteria included severe cognitive impairments affecting comprehension, diagnosis of other neurological conditions such as epilepsy, a history of traumatic brain injury or stroke, and the use of psychotropic drugs. After recruitment, the interviewer explained the study procedure and sought patient cooperation. Those who agreed signed a consent form and completed the scales. For participants with significant physical or psychological disabilities, questionnaires were read aloud by the caregiver or interviewer, who recorded the patients’ responses.
Study measures
Demographic data form
The demographic data form is a researcher-made form designed to gather demographic information about the patients and disease-specific variables such as disease duration in terms of years, AoO, and the number of hospitalizations (nHP) during the disease period.
PDS
Patients were asked a 5-point Likert question to measure their PDS due to the illness. The question was, “Which score better describes your disability due to having MS disease?”
The Yale-Brown obsessive-compulsive scale (Y-BOCS)
Symptom checklist (SC) and severity scale (SS) of the Yale-Brown obsessive-compulsive scale (Y-BOCS) were used. The SC consists of 58 questions that measure obsessions and compulsions in a 5-point Likert scale. The SS measures the severity of symptoms and their degree of interference with everyday life (Esfahani et al., 2012). The internal consistency of the two parts of SC and SS was 0.97 and 0.95, respectively. Split-half reliability values for SC and SS were 0.93 and 0.89, respectively, and test re-test reliability was 0.99. There was a positive correlation between SC and SCL-90-R-OCS (the symptom checklist-90-revised: Obsessive-compulsive subscale) and SS with scid-i (the structured clinical interview for DSM) (P>0.001) (Esfahani et al., 2012). In the present study, the Cronbach α values for obsessions, compulsions, and total symptoms were 0.95, 0.94, and 0.97, respectively.
Beck depression inventory-2 (BDI-II)
The BDI-II has 21 questions, each measuring one of the depression symptoms. As a result, a score is obtained that varies from 0 to 63, and higher scores represent greater severity of depression. The reliability coefficient for 21 items is equal to 0.913. The correlation coefficient between BDI-II scores and the brief symptom inventory-depression scale has been reported to be -0.873 (Hamidian et al., 2016). In the present study, the Cronbach α was calculated as 0.93.
Generalized anxiety disorder 7-item (GAD-7) scale
The GAD-7 scale is a self-administered questionnaire and is used as a screening tool and severity measure for GAD. The psychometric properties of a group of the Iranian population were as follows: The internal consistency measured with the Cronbach α was 0.87. A moderate to strong correlation with the hospital anxiety and depression scale was obtained for the anxiety (r=0.782) and depression (r=0.524) subscales and with the Penn State worry questionnaire (r=0.605), confirming convergent validity (Omani-Samani et al., 2018). In the present study, the Cronbach α was 0.92.
Difficulties in emotion regulation scale (DERS)
The DERS is a 36-item, multidimensional, self-report questionnaire that assesses 6 subscales: Not accepting the emotional responses, problems in performing the behaviors leading to one’s goal, impulse control problems, lack of emotional awareness, limitation in finding emotion regulation strategies, and lack of emotional clarity. The reliability of the questionnaire in the Iranian population was calculated using split-half and Cronbach α methods, which were respectively 0.86 and 0.8 for the whole questionnaire (P<0.01), indicating acceptable coefficients for the questionnaire (Hamidian et al., 2016). In the present study, the Cronbach α value was 0.85.
Connor-Davidson resilience scale (CDRS)
The CDRS is a 25-item questionnaire that measures resiliency on a 5-point Likert scale. The psychometric properties of this scale have confirmed its reliability and validity. For the Iranian population, the reliability using the Cronbach α was reported to be 0.89. The results of exploratory factor analysis have confirmed five factors: Personal competence, high standards, and tenacity; trust in one’s instincts, tolerance of negative affect, and strengthening effects of stress; the positive acceptance of change and secure relationships; control; and spiritual influences (Samani et al., 2007). In the present study, the Cronbach α was 0.95.
The proposed model
The purpose of this study is to investigate how patients’ psychiatric symptoms interact with their psychological profile and demographic characteristics and how these factors predict patients’ perceptions of their disability. For this purpose, the patient’s symptoms of depression (MDD), obsession and compulsion (OCD), and general anxiety (GAD) were evaluated to realize the patient’s psychological vulnerability. In contrast, resilience (RES) and difficulty in emotion regulation (DER) were assessed to achieve their psychological profile. In addition, the age of MS onset (AoO), duration of MS (DUR), and patient’s nHP were used as a descriptor of demographic characteristics, and PDS stands for the patient’s PDS. Figure 1 illustrates the proposed model. Covariances between variables are shown with the red double-headed arrows.
Study hypotheses
Hypothesis 1: Patients’ psychological resilience contributes to milder symptoms of psychological vulnerabilities (depression, GAD, and OCD symptoms).
Hypothesis 2: Patients’ DER contributes to more severe psychological vulnerabilities (depression, GAD, and OCD symptoms).
Hypothesis 3: Patients’ demographic characteristics (nHPs, disease duration, and AoO) contribute to more severe psychological vulnerabilities (depression, GAD, and OCD symptoms).
Hypothesis 4: Patients’ psychological vulnerabilities (depression, GAD, and OCD symptoms) contribute to a more severe perception of their disability.
Hypothesis 5: Patients’ psychological resilience contributes to a milder perception of their disability directly and indirectly.
Hypothesis 6: Patients’ DER contributes to a more severe perception of their disability directly and indirectly.
Hypothesis 7: The patient’s demographic characteristics (nHPs, disease duration, and AoO) contribute to the perception of their disability directly and indirectly.
Statistical analysis
For the path analysis of the proposed model, weighted least squares estimation (also known as asymptotically distribution-free estimation) was employed using the lavaan package in R programming language and environment for statistical computations (Rosseel, 2012; Team, 2013). For estimation, robust standard errors and adjusted mean and variance are used. To ascertain model fit, we used the chi-square test (χ2), the comparative fit index (CFI), the Tucker-Lewis index (TLI), the normative fit index (NFI), the root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR).
Results
Table 1 depicts the participants’ sociodemographic characteristics and MS profile.
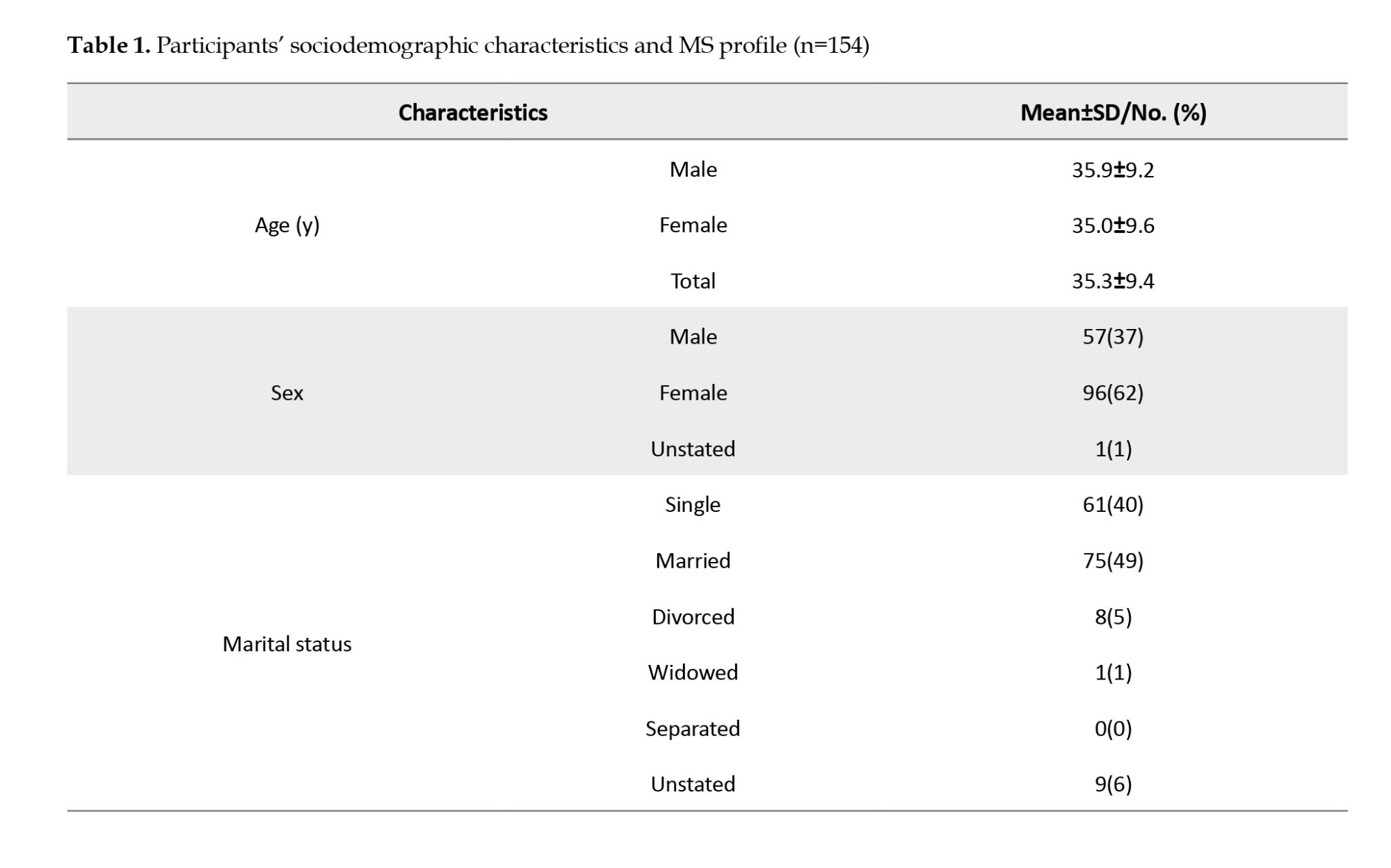
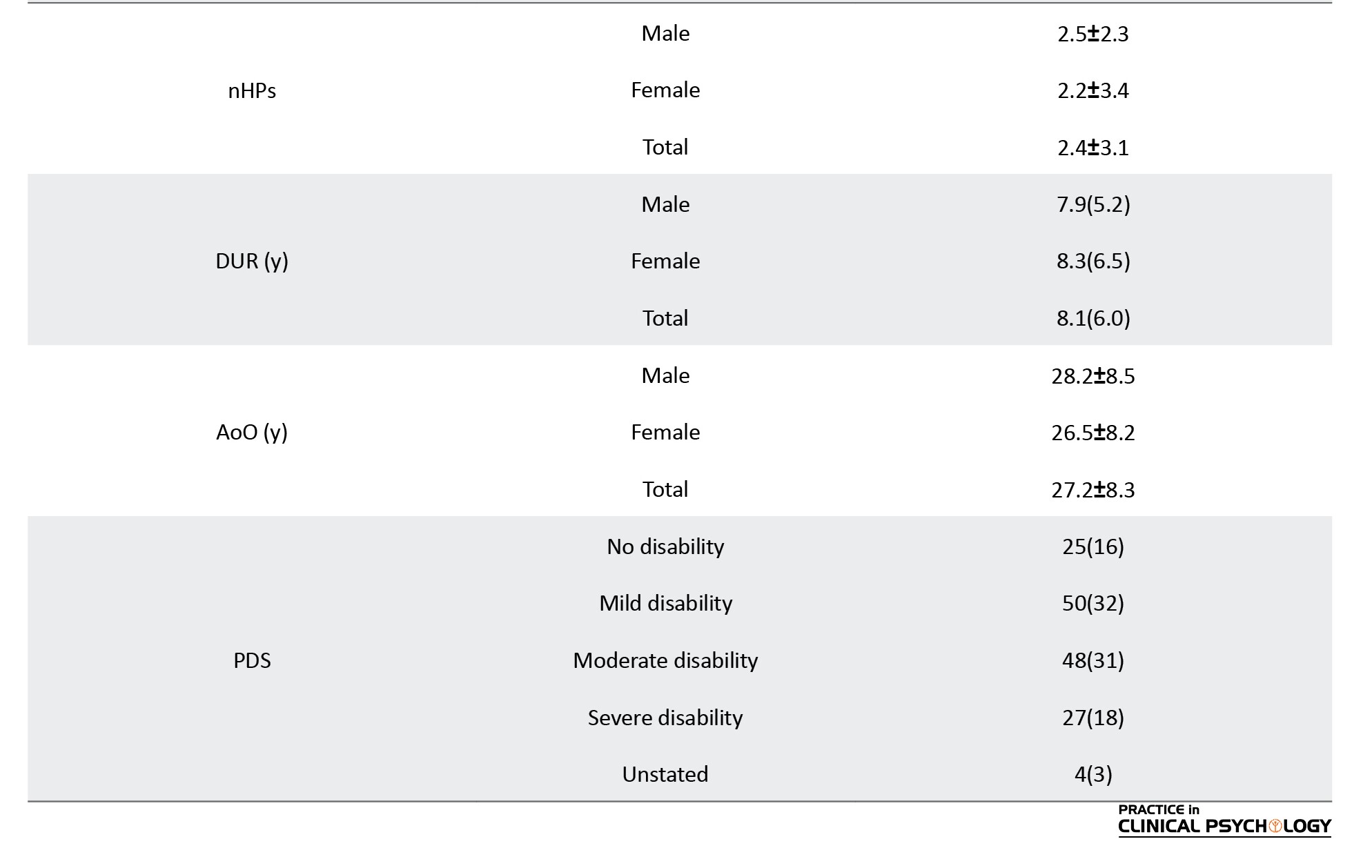
Table 2 presents the Mean±SD, and 90% CI values for OCD, BDI, GAD, DER, and RES. The lowest and highest possible values for each variable are also presented.
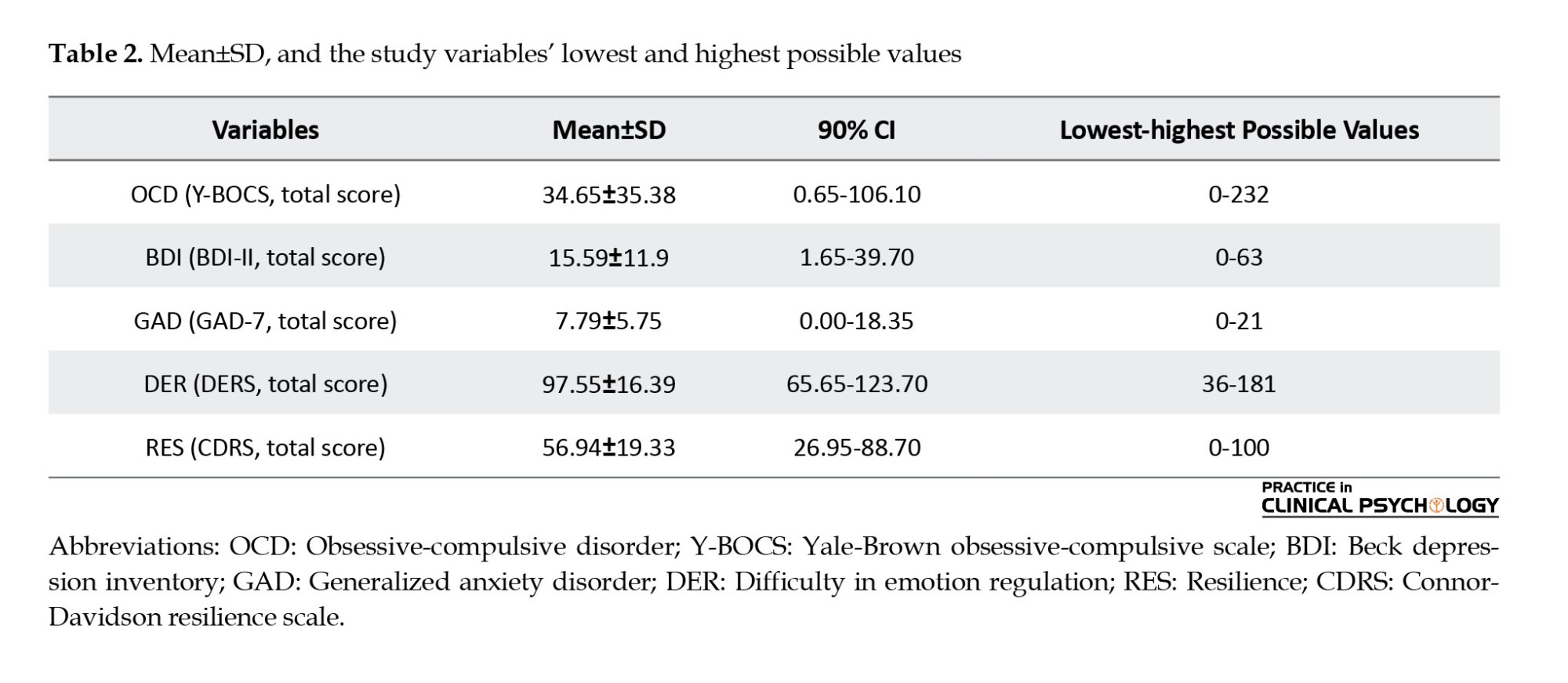
Based on Table 3, the path model analysis of the proposed model produced an excellent fit. The model accounted for 62% of the variance in PDS, 36% of the variance in BDI, 18% of the variance in OCD, and 16% of the variance in GAD.
Figure 1 demonstrates significant direct path coefficients and covariances found in the path model analysis of the proposed model.
According to Figure 1 and regarding the demographic variables, higher AoO (β=0.125, P<0.001) was found to directly contribute to BDI (β=0.184, P<0.01), OCD (β=0.219, P<0.01) and PDS (β=0.125, P<0.001) among PwMS. Based on Table 4, its indirect effect (β=0.055, P<0.05) through the mediating role of BID was also statistically significant; therefore, both direct and indirect effects of AoO are valid.
The nHPs (β=0.294, P<0.001) contributed directly to PDS; however, its indirect effect was not significant. Therefore, only the direct impact of the nHPs is valid.
DUR has the strongest direct effect on BDI (β=0.352, P<0.001), OCD (β=0.292, P<0.001), and PDS (β=0.448, P<0.001). Moreover, based on Table 4, its indirect effects through the mediating role of nHP (β=0.113, P<0.001) and BDI (β=0.106, P<0.01) were also found significant. Overall, DUR’s total effect on PDS was also significant (β=0.666, P<0.001). In this regard, it is possible to say that both direct and indirect impacts of MS duration are valid.
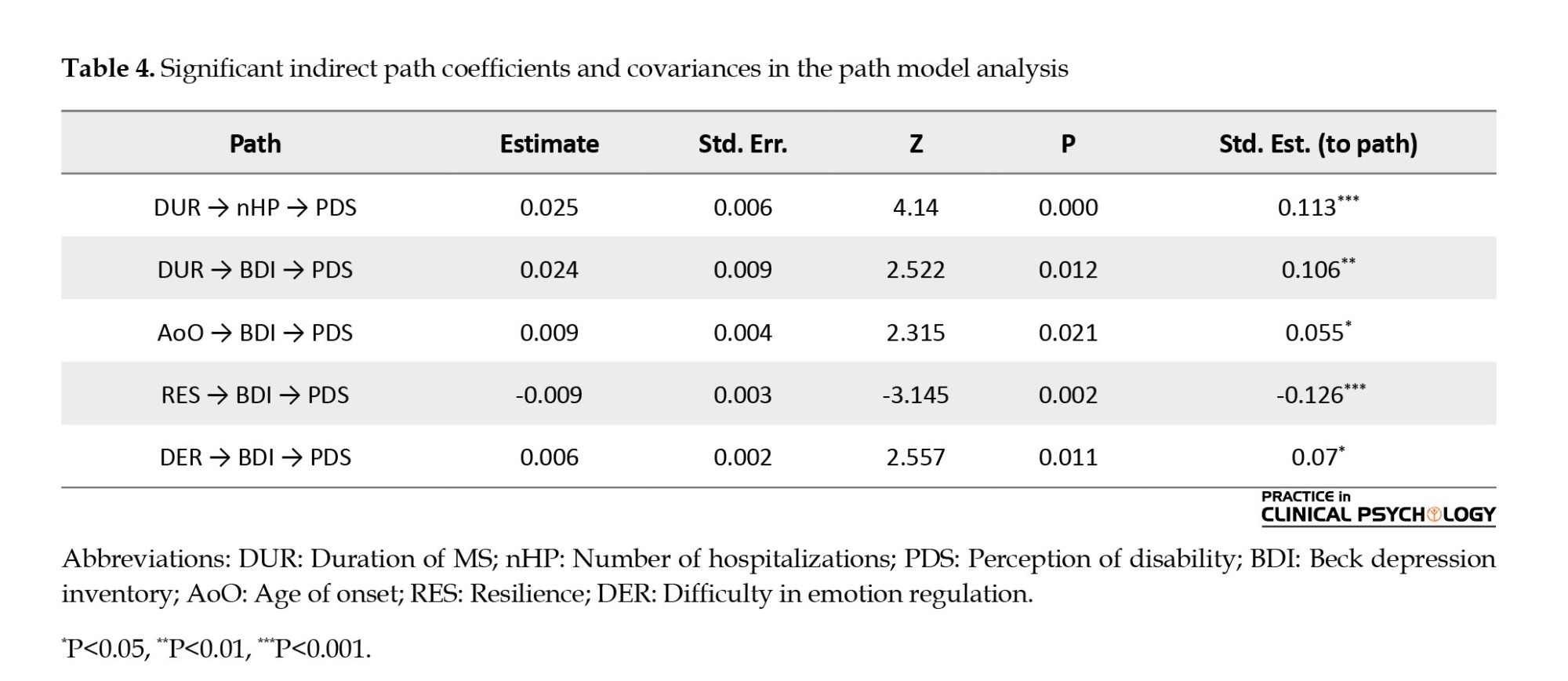
In addition, regarding the psychological profile, RES negatively and DER positively contribute to more severe psychiatric symptoms, including BDI, OCD, and GAD. Figure 1 also shows that BDI (β=0.297, P<0.001) contributes to a perception of a more severe disability (PDS) among PwMS, while no such relation was found between either GAD or OCD with PDS. On the other hand, and based on Table 4, with the mediation role of BDI, RES (β=-0.126, P<0.001) and DER (β=0.07, P<0.05) were found to indirectly contribute to a milder and a more severe PDS among these patients respectively. Therefore, RES and DER directly affect BDI and indirectly affect PDS.
Table 4 shows the path model analysis’s significant indirect path coefficients and covariances.
Table 4 suggests that MS chronicity impacts patients’ PDS through increased hospitalizations and depression. Additionally, low resilience and difficulties in emotion regulation are risk factors for a heightened PDS.
Discussion
The results of the present study strongly support our hypothesis about the role of patients’ psychological vulnerabilities (depression, GAD, and OCD symptoms) in a more severe PDS. In PwMS, being more resilient and having more trouble in emotion regulation could predict psychiatric symptoms. These findings show the negative direct effect of resilience on the development of depression, anxiety, and OCD symptoms, which corroborated the studies of Nakazawa et al. (2018). The results are also in keeping with Prakash et al. (2019) on the impact of emotion regulation strategies in developing depression and anxiety symptoms. These observations also replicate the broader literature on the correlation of these two transdiagnostic variables with psychiatric symptoms which have been formerly reported in the general population among a group of PwMS (Gürcan-Yıldırım & Gençöz, 2020; Min et al., 2015).
Depression and OCD have also shown a correlation with the AoO. As per the previous studies, the AoO of MS is associated with anatomical factors such as ventricle expansion (Jakimovski et al., 2020) and physical indexes such as disability (Ramachandran et al., 2014). In the present study, the results suggest the older AoO as a risk factor for developing depression and OCD symptoms.
Both transdiagnostic and demographic factors play a significant role in the development of depression, which in turn directly influences patients’ PDS. This finding aligns with previous research by Janssens et al. (2003) and Smith & Young, (2000), which reported that depression mediates the relationship between disability and quality of life while also amplifying individuals’ perception of their disability. The results suggest that transdiagnostic and demographic variables impact disability primarily through depression’s decisive mediating role, highlighting the initial links in this chain of influence.
Moreover, the model underscores the significant role of disease duration in the onset of psychiatric disorders such as depression, anxiety, and OCD. Previous studies have established a correlation between MS duration and factors like disability severity (Mohaghegh et al., 2021), quality of life (Karatepe et al., 2011), and the use of active coping strategies, which are associated with better psychological outcomes(Holland et al., 2019). Consistent with these findings, the present study confirms the predictive role of disease duration in the presence of psychiatric symptoms. Considering the nHPs as an indicator of severity and disease duration as a measure of chronicity, it appears that chronicity plays a more substantial role in the development of psychiatric symptoms (Shahwar & Kidwai, 2020). This condition, in turn, increases an individual’s PDS.
Resilience plays a crucial role in mitigating psychiatric disorders, as demonstrated by several studies (Koelmel et al., 2017; Nakazawa et al., 2018). In MS, chronicity is strongly linked to the onset of psychiatric symptoms unless a modifying factor alters this relationship. In this model, resilience, shaped by specific traits and skills, can buffer the impact of disease duration on depression.
While MS chronicity contributes to psychiatric symptom development, resilience acts as a protective factor, slowing this progression. As the disease advances, adopting a resilient mindset becomes increasingly important for coping. Without it, the risk of depression, anxiety, and obsessive-compulsive symptoms rises over time, consistent with Kim et al. (2019) on the role of resilience in patients with chronic disease. Thus, disease duration serves as a warning factor; as hospitalizations increase and PDS intensifies, adapting to chronic illness becomes more challenging, making psychiatric symptoms more likely to emerge.
In other words, whilst the chronicity in MS plays a pivotal role in the development of psychiatric symptoms, the resilience factor can play the role of a preventive element that decelerates this process. This means that the more the disease progresses, the faster the person needs to acquire a resilient viewpoint to cope with it. If it does not happen, the risk of incidence of psychiatric symptoms, including depression, anxiety, and obsessive-compulsive symptoms, increases over time. Hence, disease duration is an alarming factor; as time passes and the nHPs and the person’s PDS increases, implementing strategies that enable the person to adapt to the chronic illness and be resilient is getting harder to achieve, and this is where the symptoms of psychiatric disorders start to emerge.
About the emotional regulation variable, such a correlation to the disease duration was not observed, but emotional regulation was directly and strongly correlated with depression and anxiety. From a therapeutic perspective, this skill is not only involved in symptom presentation but also as a transdiagnostic construct that should be included in any treatment planning for patients with MS. This is in line with previous studies (Fitzgerald et al., 2019; Sloan et al., 2017) suggesting that emotion regulation reflects shared neural mechanisms across both anxiety and depression, highlighting its critical role as a transdiagnostic construct. Such findings reinforce the importance of addressing emotion regulation in treatment planning for various psychological conditions, including MS.
Conclusion
These findings highlight the critical need for early mental health interventions in the management of MS, mainly focusing on resilience and emotion regulation. As psychiatric symptoms, especially depression, significantly influence PDS and disease progression, addressing these psychological factors from the outset of diagnosis can prevent further complications. The protective role of emotion regulation and resilience emphasizes the importance of incorporating psychological strategies into treatment plans, aiming to mitigate the onset of anxiety, depression and other psychiatric symptoms. Integrating these approaches early in the disease trajectory can ultimately enhance the psychological well-being and overall quality of life of individuals with MS.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of the University of Social Welfare and Rehabilitation Sciences (Code: IR.USWR.REC.1396.375). All patients signed the Informed consent form before data collection
Funding
Clinical Research Development Center of Rofeideh Rehabilitation Hospital, Tehran, Iran, financially supported the present study.
Authors' contributions
Study design and data interpretation: Shima Shakiba, and Sajedeh Hamidian; Referring patients: Ahmad Sharifi; Data collection: Shima Shakiba, Sajedeh Hamidian and Ahmad Sharifi; Data analysis: Ahmad Sharifi; Writing the original draft: Sajedeh Hamidian and Ahmad Sharifi; Review and editing: Shima Shakiba.
Conflict of interest
The authors declared no competing interests.
Acknowledgments
The authors thank the Clinical Research Development Center of Rofeideh Rehabilitation Hospital, Tehran, Iran, for their support, cooperation, and assistance throughout the study. Additionally, The authors sincerely thank all the participants for their time, effort, and valuable contributions to this research.
References
Azami, M., YektaKooshali, M. H., Shohani, M., Khorshidi, A., & Mahmudi, L. (2019). Epidemiology of multiple sclerosis in Iran: A systematic review and meta-analysis. Plos One, 14(4), e0214738. [DOI:10.1371/journal.pone.0214738] [PMID]
Carta, M. G., Moro, M. F., Lorefice, L., Trincas, G., Cocco, E., & Del Giudice, E., et al. (2014). The risk of bipolar disorders in multiple sclerosis. Journal of Affective Disorders, 155, 255-260. [DOI:10.1016/j.jad.2013.11.008] [PMID]
Chwastiak, L. A., & Ehde, D. M. (2007). Psychiatric issues in multiple sclerosis. Psychiatric Clinics of North America, 30(4), 803-817. [DOI:10.1016/j.psc.2007.07.003] [PMID]
Esfahani, S. R., Motaghipour, Y., Kamkari, K., Zahiredin, A., & Janbozorgi, M. (2012). Reliability and Validity of the Persian Version of the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS). Iranian Journal of Psychiatry & Clinical Psychology, 17(4), 297–303. [Link]
Feinstein, A., & Pavisian, B. (2017). Multiple sclerosis and suicide. Multiple Sclerosis (Houndmills, Basingstoke, England), 23(7), 923–927. [DOI:10.1177/1352458517702553] [PMID]
Fitzgerald, J. M., Klumpp, H., Langenecker, S., & Phan, K. L. (2019). Transdiagnostic neural correlates of volitional emotion regulation in anxiety and depression. Depression and Anxiety, 36(5), 453-464. [DOI:10.1002/da.22859] [PMID]
Foroughipour, M., Behdani, F., Hebrani, P., Marvast, M. N., Esmatinia, F., & Akhavanrezayat, A. (2012). Frequency of obsessive-compulsive disorder in patients with multiple sclerosis: A cross-sectional study. Journal of Research in Medical Sciences : The Official Journal of Isfahan University of Medical Sciences, 17(3), 248–253. [PMID]
Gürcan-Yıldırım, D., & Gençöz, T. (2020). The association of self-discrepancy with depression and anxiety: Moderator roles of emotion regulation and resilience. Current Psychology, 41, 1821–1834. [DOI:10.1007/s12144-020-00701-8]
Hamidian, S., Omidi, A., Mousavinasab, S. M., & Naziri, G. (2016). The effect of combining mindfulness-based cognitive therapy with pharmacotherapy on depression and emotion regulation of patients with dysthymia: A clinical study. Iranian Journal of Psychiatry, 11(3), 166-172. [PMID]
Hamidian, S., Omidi, A., Naziri, G., Abolghasemi, R., & Musavinasab, M. (2016). [The effectiveness of mindfulness-based cognitive therapy on severity of depression and anger in dysthymic patients (Persian)]. Journal of Psychological Studies, 12(3), 83-102. [DOI: 10.22051/psy.2016.2602]
Haussleiter, I. S., Brüne, M., & Juckel, G. (2009). Psychopathology in multiple sclerosis: Diagnosis, prevalence and treatment. Therapeutic Advances in Neurological Disorders, 2(1), 13-29. [DOI:10.1177/1756285608100325] [PMID]
Heinsch, M., Wells, H., Sampson, D., Wootten, A., Cupples, M., & Sutton, C., et al. (2022). Protective factors for mental and psychological well-being in Australian adults: A review. Mental Health & Prevention, 25, 200192. [DOI:10.1016/j.mhp.2020.200192]
Holland, D. P., Schlüter, D. K., Young, C. A., Mills, R. J., Rog, D. J., & Ford, H. L., et al. (2019). Use of coping strategies in multiple sclerosis: Association with demographic and disease-related characteristics. Multiple Sclerosis and Related Disorders, 27, 214–222. [DOI:10.1016/j.msard.2018.10.016] [PMID]
Hosseinzadeh, A., Baneshi, M. R., Sedighi, B., Kermanchi, J., & Haghdoost, A. A. (2019). Incidence of multiple sclerosis in Iran: a nationwide, population-based study. Public Health, 175, 138–144. [DOI:10.1016/j.puhe.2019.07.013] [PMID]
Jakimovski, D., Dujmic, D., Hagemeier, J., Ramasamy, D. P., Bergsland, N., & Dwyer, M. G., et al. (2020). Late onset multiple sclerosis is associated with more severe ventricle expansion. Multiple Sclerosis and Related Disorders, 46, 102588. [DOI:10.1016/j.msard.2020.102588] [PMID]
Janssens, A. C., van Doorn, P. A., de Boer, J. B., Kalkers, N. F., van der Meche, F. G., & Passchier, J., et al. (2003). Anxiety and depression influence the relation between disability status and quality of life in multiple sclerosis. Multiple Sclerosis (Houndmills, Basingstoke, England), 9(4), 397–403. [DOI:10.1191/1352458503ms930oa] [PMID]
Karatepe, A. G., Kaya, T., Günaydn, R., Demirhan, A., Çe, P., & Gedizlioglu, M. (2011). Quality of life in patients with multiple sclerosis: The impact of depression, fatigue, and disability. International Journal of Rehabilitation Research, 34(4), 290-298. [DOI:10.1097/MRR.0b013e32834ad479] [PMID]
Kim, G. M., Lim, J. Y., Kim, E. J., & Park, S. M. (2019). Resilience of patients with chronic diseases: A systematic review. Health & Social Care in the Community, 27(4), 797-807. [DOI:10.1111/hsc.12620] [PMID]
Koelmel, E., Hughes, A. J., Alschuler, K. N., & Ehde, D. M. (2017). Resilience mediates the longitudinal relationships between social support and mental health outcomes in multiple sclerosis. Archives of Physical Medicine and Rehabilitation, 98(6), 1139-1148. [DOI:10.1016/j.apmr.2016.09.127] [PMID]
Litster, B., Fiest, K. M., Patten, S. B., Fisk, J. D., Walker, J. R., & Graff, L. A., et al. (2016). Screening tools for anxiety in people with multiple sclerosis: A systematic review. International Journal of MS Care, 18(6), 273-281. [DOI:10.7224/1537-2073.2016-004] [PMID]
Marrie, R. A., Reingold, S., Cohen, J., Stuve, O., Trojano, M., & Sorensen, P. S., et al. (2015). The incidence and prevalence of psychiatric disorders in multiple sclerosis: A systematic review. Multiple Sclerosis Journal, 21(3), 305-317. [DOI:10.1177/1352458514564487]
McKay, K. A., Tremlett, H., Fisk, J. D., Zhang, T., Patten, S. B., & Kastrukoff, L., et al. (2018). Psychiatric comorbidity is associated with disability progression in multiple sclerosis. Neurology, 90(15), e1316-e1323. [DOI:10.1212/WNL.0000000000005302] [PMID]
Min, J. A., Lee, C. U., & Chae, J. H. (2015). Resilience moderates the risk of depression and anxiety symptoms on suicidal ideation in patients with depression and/or anxiety disorders. Comprehensive Psychiatry, 56, 103-111. [DOI:10.1016/j.comppsych.2014.07.022] [PMID]
Mohaghegh, F., Moghaddasi, M., Eslami, M., Dadfar, M., & Lester, D. (2021). Disability and its association with psychological factors in multiple sclerosis patients. Multiple Sclerosis and Related Disorders, 49, 102733. [DOI:10.1016/j.msard.2020.102733] [PMID]
Nakazawa, K., Noda, T., Ichikura, K., Okamoto, T., Takahashi, Y., & Yamamura, T., et al. (2018). Resilience and depression/anxiety symptoms in multiple sclerosis and neuromyelitis optica spectrum disorder. Multiple Sclerosis and Related Disorders, 25, 309-315. [DOI:10.1016/j.msard.2018.08.023] [PMID]
Omani-Samani, R., Maroufizadeh, S., Ghaheri, A., & Navid, B. (2018). Generalized anxiety Disorder-7 (GAD-7) in people with infertility: A reliability and validity study. Middle East Fertility Society Journal, 23(4), 446-449. [DOI:10.1016/j.mefs.2018.01.013]
Ouellet, C., Langlois, F., Provencher, M., & Gosselin, P. (2019). Intolerance of uncertainty and difficulties in emotion regulation: Proposal for an integrative model of generalized anxiety disorder. European Review of Applied Psychology, 69(1), 9-18. [DOI:10.1016/j.erap.2019.01.001]
Prakash, R. S., Schirda, B., Valentine, T. R., Crotty, M., & Nicholas, J. A. (2019). Emotion dysregulation in multiple sclerosis: Impact on symptoms of depression and anxiety. Multiple Sclerosis and Related Disorders, 36, 101399. [DOI:10.1016/j.msard.2019.101399] [PMID]
Ramachandran, S., Strange, R. C., Jones, P. W., Kalra, S., Nayak, D., & Hawkins, C. P. (2014). Associations between onset age and disability in multiple sclerosis patients studied using MSSS and a progression model. Multiple Sclerosis and Related Disorders, 3(5), 593-599. [DOI:10.1016/j.msard.2014.06.002] [PMID]
Ron, M. A. (2018). The neuropsychiatry of multiple sclerosis. BJPsych Advances, 24(3), 178-187. [DOI:10.1192/bja.2017.19]
Rosseel, Y. (2012). Lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48(2), 1-36. [Link]
Samani, S., Jokar, B., & Sahragard, N. (2007). [Effects of resilience on mental health and life satisfaction (Persian)]. Iranian Journal of Psychiatry and Clinical Psychology, 13(3), 290-295. [Link]
Sarısoy, G., Terzi, M., Gümüş, K., & Pazvantoğlu, O. (2013). Psychiatric symptoms in patients with multiple sclerosis. General Hospital Psychiatry, 35(2), 134-140. [DOI:10.1016/j.genhosppsych.2012.10.011] [PMID]
Shahwar, H., & Kidwai, S. (2020). Psychiatric Issues in Multiple Sclerosis (MS). Journal of Traumatic Stress Disorders & Treatment, 9, 5. [Link]
Shail, M. S. (2017). Neuropsychiatry in demyelination disease: Using depression as a prodrome for early diagnosis and treatment of multiple sclerosis. Cureus, 9(11), e1813. [DOI:10.7759/cureus.1813] [PMID]
Sloan, E., Hall, K., Moulding, R., Bryce, S., Mildred, H., & Staiger, P. K. (2017). Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: A systematic review. Clinical Psychology Review, 57, 141-163. [DOI:10.1016/j.cpr.2017.09.002] [PMID]
Smith, S., & Young, C. (2000). The role of affect on the perception of disability in multiple sclerosis. Clinical Rehabilitation, 14(1), 50-54. [DOI:10.1191/026921500676724210] [PMID]
Sparaco, M., Lavorgna, L., & Bonavita, S. (2021). Psychiatric disorders in multiple sclerosis. Journal of Neurology, 268(1), 45-60. [DOI:10.1007/s00415-019-09426-6] [PMID]
Taylor, M. G., & Carr, D. (2021). Psychological resilience and health among older adults: A comparison of personal resources. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 76(6), 1241–1250. [DOI:10.1093/geronb/gbaa116] [PMID]
Team, R. D. C. (2013). R: A language and environment for statistical computing. Retrieved from: [Link]
Turner, A. P., Alschuler, K. N., Hughes, A. J., Beier, M., Haselkorn, J. K., & Sloan, A. P., et al. (2016). Mental health comorbidity in MS: Depression, anxiety, and bipolar disorder. Current Neurology and Neuroscience Reports, 16(12), 106. [DOI:10.1007/s11910-016-0706-x] [PMID]
Uguz, F., Akpinar, Z., Ozkan, I., & Tokgoz, S. (2008). Mood and anxiety disorders in patients with multiple sclerosis. International Journal of Psychiatry in Clinical Practice, 12(1), 19-24. [DOI:10.1080/13651500701330825] [PMID]
Villalobos, D., Pacios, J., & Vázquez, C. (2021). Cognitive control, cognitive biases and emotion regulation in depression: A new proposal for an integrative interplay model. Frontiers in Psychology, 12, 628416. [DOI:10.3389/fpsyg.2021.628416] [PMID]
Type of Study: Original Research Article |
Subject:
Rehabilitation
Received: 2025/01/21 | Accepted: 2025/03/12 | Published: 2025/04/1
Received: 2025/01/21 | Accepted: 2025/03/12 | Published: 2025/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |