Volume 13, Issue 2 (Spring 2025)
PCP 2025, 13(2): 181-190 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Habibi S, Soleimani E, Zeinali S. A Structural Model of Substance Use Tendencies: The Impact of Childhood Trauma and the Mediating Role of Self-compassion. PCP 2025; 13 (2) :181-190
URL: http://jpcp.uswr.ac.ir/article-1-991-en.html
URL: http://jpcp.uswr.ac.ir/article-1-991-en.html
1- Department of Psychology, Faculty of Letters and Humanities, Urmia University, Urmia, Iran.
2- Department of Psychology, Faculty of Letters and Humanities, Urmia University, Urmia, Iran. ,E.soleimani@urmia.ac.ir
2- Department of Psychology, Faculty of Letters and Humanities, Urmia University, Urmia, Iran. ,
Full-Text [PDF 825 kb]
(1197 Downloads)
| Abstract (HTML) (1780 Views)
Full-Text: (379 Views)
Introduction
Substance use represents a critical global issue that disrupts familial bonds and undermines the stability of social structures (Room et al., 2024). This issue mainly affects many individuals, especially young individuals (Song et al., 2022). Statistics from the World Health Organization (WHO) show an increase in the production and consumption of these substances worldwide. According to a report by WHO, nearly 200 million people worldwide, aged 15-63, use illegal substances each year (WHO, 2010). The tendency toward substance use encompasses individuals’ beliefs and attitudes regarding specific substances, as well as their perceptions of the potential positive and negative outcomes associated with their use (Davis et al., 2022). Additionally, it is considered a personality vulnerability that makes individuals more prone to engaging in substance use (Volkow & Blanco, 2023). Identifying risk factors and predispositions for substance use and preventing the development of such destructive dependencies are top priorities. This is especially important because the tendency to use substances is a significant risk factor that needs to be addressed, particularly among young people, including students. Many students struggle with coping skills to manage new challenges and emerging problems. As a result, They might resort to harmful coping strategies, like substance use, to manage psychological stress (Vafaie & Kober, 2022). The tendency toward substance use represents a multifaceted social concern influenced by a range of factors, including familial dynamics, socioeconomic status, social context, psychological variables, and experiences of childhood trauma (Belfiore et al., 2024).
Childhood trauma refers to adverse events experienced before the age of 18, generally classified into four key categories: physical abuse, sexual abuse, emotional abuse, and neglect. These incidents often occur within caregiving environments and involve behaviors or failures to act that result in harm, whether physical, sexual, or emotional, to the child (Tang et al., 2020). Physical abuse, which includes violent actions such as hitting, burning, or severe shaking, can result in both physical and psychological harm. Sexual abuse involves inappropriate sexual contact or exploitation through coercion, threats, or deception. Moreover, emotional abuse, defined by behaviors such as humiliation, insults, neglect, and intimidation, can have a lasting impact on a child’s self-esteem and confidence. Moreover, neglect, characterized by the failure to fulfill a child’s basic requirements, such as adequate nutrition, healthcare, emotional support, and psychological safety, can lead to substantial impairments in both physical and cognitive development (Massullo et al., 2023). A significant theoretical perspective on the link between trauma and substance use is the “self-medication theory.” This theory suggests that people who have gone through traumatic experiences often struggle to cope with negative emotions, leading them to seek temporary relief through substance abuse or alcohol as a way to numb their psychological and emotional distress. While drugs and alcohol can initially suppress the activity of the amygdala, the part of the brain responsible for fear and stress, over time, they increase their sensitivity, making the individual even more vulnerable (Khantzian, 1985). Orak et al. demonstrated that childhood traumatic experiences had an impact on the tendency toward substance use (Orak et al., 2023). Additionally, Chandler et al. documented a statistically significant correlation between difficult early life experiences and the likelihood of engaging in substance use (Chandler et al., 2018). The family is the primary environment where a child begins developing. Growing up in an emotionally cold and restrictive environment, combined with exposure to traumatic experiences, can contribute to the development of dysfunctional behaviors, including substance use (He et al., 2022). Consequently, investigating the long-term psychological and physiological impacts of childhood trauma on adult health is of significant importance.
Although a significant and clear relationship has been reported between childhood trauma and the tendency toward substance use, research findings suggest that direct relationships can only partially explain this connection and that mediating variables are likely involved. Therefore, the question that arises is how childhood trauma influences the tendency toward substance use. In this context, self-compassion has drawn the attention of researchers in recent years (Chen, 2019).
Self-compassion refers to an individual’s ability to navigate personal challenges and endure suffering with enhanced emotional resilience and greater ease (Ren et al., 2024). This trait serves as a supportive buffer against the tendency to engage in substance use (Arslan et al., 2024). Self-compassion consists of three fundamental aspects: treating oneself with kindness rather than harsh self-criticism, acknowledging the shared human experience instead of feeling isolated, and practicing mindfulness instead of becoming overly absorbed in or avoiding one’s emotions. The idea of common humanity underscores the understanding that everyone has flaws and makes errors, a universal aspect of the human condition. On the other hand, mindfulness involves staying fully aware and present in the moment without being overwhelmed or detaching from it (Neff, 2003). Shahin et al. indicated a substantial inverse correlation between self-compassion and substance use (Shahin et al., 2021). Moore et al. indicated that substance use is frequently linked to a deficiency in self-compassion (Moore et al., 2022). Since the basis of the structural equation model is correlation and self-compassion is considered a mediating variable, a relationship must exist between the input and output variables in the present study. Research results suggest an association between self-compassion and experiences of childhood trauma. Christoffersen et al. showed a strong connection between early life trauma and self-compassion (Christoffersen et al., 2024). Erol and Inozu indicated that the absence of self-compassion mediates the association between childhood emotional neglect and self-harm without suicidal intent, with a significant relationship observed between these factors (Erol & Inozu, 2024).
Given the psychological, cognitive, and emotional damage caused by substance use and the fact that substance use can significantly harm social, familial, and relational life, it is essential to conduct fundamental studies aimed at preventing the positive tendency toward substance use. In contrast, while several studies have examined the relationships between the variables mentioned above, there has been no investigation into the mediating role of self-compassion in the relationship between childhood trauma and the inclination toward substance use, revealing a significant gap in the existing literature. As such, the current study aims to propose a model that connects childhood trauma to substance use tendency, with self-compassion acting as a mediating variable.
Materials and Methods
Considering the study subject, the research methodology was correlational, utilizing a structural equation modeling (SEM) approach. This study’s sample population comprised all Urmia University students during the 2023-2024 academic year (N=13267). A sample of 350 participants was drawn from this population using multistage random sampling. For this purpose, three faculties were randomly selected as the first cluster from the 11 faculties at Urmia University: The Faculty of Literature and Humanities, the Faculty of Engineering, and the Faculty of Basic Sciences. An invitation was posted on the university’s virtual spaces and bulletin boards to encourage students to participate in the study. The questionnaires were placed on tables in the faculty offices, and after explaining the research objectives, the need for honest participation, and ensuring confidentiality, they were distributed to the students. The students were instructed to complete the questionnaires and submit them to the researcher. Following data collection, the data were analyzed using SPSS software, version 22 and AMOS software employing descriptive analysis and the Pearson correlation coefficient test.
The criteria for participation in the study necessitated the voluntary and informed consent of the students. In contrast, the exclusion criterion was based on submitting incomplete responses to the measurement instruments. Moreover, participants received detailed instructions on how to respond to the questions, were assured of the confidentiality of their answers, and were made aware of their right to withdraw from the study at any time without facing any adverse outcomes.
Study measures
Substance use tendency questionnaire
Created by Weed et al. (1992), the substance use tendency questionnaire includes 36 items and 5 additional items designed to assess social desirability (Weed et al., 1992). It consists of two components: proactive readiness and passive readiness. Proactive readiness is associated with antisocial behaviors, a tendency toward substance use, favorable attitudes toward substances, depression, and a strong inclination toward seeking new and intense sensations (items 3, 4, 7, 8, 10, 11, 15, 16, 18, 19, 21, 22, 25, 26, 28, 29, 31, 34, 36, 37, 38, 40, 41). However, passive readiness predominantly relates to lack of assertiveness and depression (items 1, 2, 5, 6, 9, 12, 13, 14, 17, 20, 23, 24, 27, 30, 32, 35, 39). Each statement is assessed using a scale where 0 represents “strongly disagree” and 3 represents “strongly agree.” However, the scoring for items 6, 12, 15, and 21 is reversed. The questionnaire includes a social desirability scale for items 33, 21, 15, 13, and 12. In Zargar et al.’s (2013) study, the questionnaire’s content, face, and criterion validity were deemed appropriate for assessment. Two methods were employed to assess the validity of this scale. Concerning criterion validity, the questionnaire successfully differentiated between addicted and nonaddicted groups. Construct validity was evaluated by examining its correlation with the 25-item clinical symptoms checklist, resulting in a significant correlation of 0.45. The reliability of the scale, assessed using the Cronbach α, was determined to be 0.90, suggesting a high level of internal consistency (Zargar et al., 2013). In the current study, the Cronbach α was calculated to be 0.75.
Childhood trauma questionnaire (CTQ)
The CTQ was designed by Bernstein et al. The questionnaire measures experiences of early developmental trauma and abuse (Bernstein et al., 2003). This screening tool detects childhood abuse and neglect and is suitable for both adults and adolescents. It includes 28 items, with 25 focusing on key aspects of childhood trauma and 3 assessing possible denial of past experiences. The questionnaire covers five types of maltreatment: physical abuse, sexual abuse, emotional abuse, emotional neglect, and physical neglect. In Bernstein et al.’s (2003)study, the Cronbach α values ranged from 0.78 to 0.95 for various abuse types, with concurrent validity between 0.59 and 0.78. In Iran, Ebrahimi et al. (2014) reported Cronbach α values between 0.81 and 0.98, and in the current study, the value was 0.81, confirming the tool’s reliability.
Self-compassion scale short form (SCS-SF)
The 12-item SCS-SF, also known as the self-compassion questionnaire, was developed by Neff et al. in 2011. This scale includes six dimensions: Self-kindness (items 2 and 6), self-judgment (items 11 and 12), common humanity (items 5 and 10), isolation (items 4 and 8), mindfulness (items 3 and 7), and overidentification (items 1 and 9). Responses are rated on a Likert scale ranging from 1 to 5. It includes reverse scoring for items 1, 4, 8, 9, 11 and 12. Shahbazi et al. (2015) used the 12-item short form of this scale, which comprises six subscales, each with two items, as developed by Neff et al., to measure self-compassion (Sh, 2015; Neff, 2011). The questionnaire demonstrated satisfactory content, construct, and criterion validity in their research, with the overall Cronbach α coefficient for the scale exceeding 0.70. Moreover, the Cronbach α values were reported to be 0.77, 0.92, 0.88, 0.91, 0.87, and 0.83 for the subscales self-kindness, self-judgment, common humanity, isolation, mindfulness, and overidentification, respectively. The concurrent and convergent validity of the questionnaire was also favorable. In the present study, the Cronbach α for the questionnaire was 0.77, indicating the tool’s reliability.
Results
The results indicated that among the participants in this study, 112(36.36%) were from the Faculty of Engineering, 98(29.44%) from the Faculty of Basic Sciences, and 140(39.20%) from the Faculty of Humanities. Furthermore, 206 participants (57.68%) were aged between 20 and 25 years, 96 participants (26.88%) were aged between 26 and 30 years, 32 participants (8.96%) were aged between 31 and 35 years, and 16 participants (4.48%) were over 35 years old. Regarding sex, 126 participants (35.28%) were male, and 224(64.72%) were female.
Since the SEM approach is based on the correlation matrix, Table 1 shows the Pearson correlation coefficients for the study variables and descriptive statistics. Moreover, the skewness and kurtosis values for all the observed variables ranged from -2 to +2, suggesting that the data followed a normal distribution and were appropriate for SEM analysis.
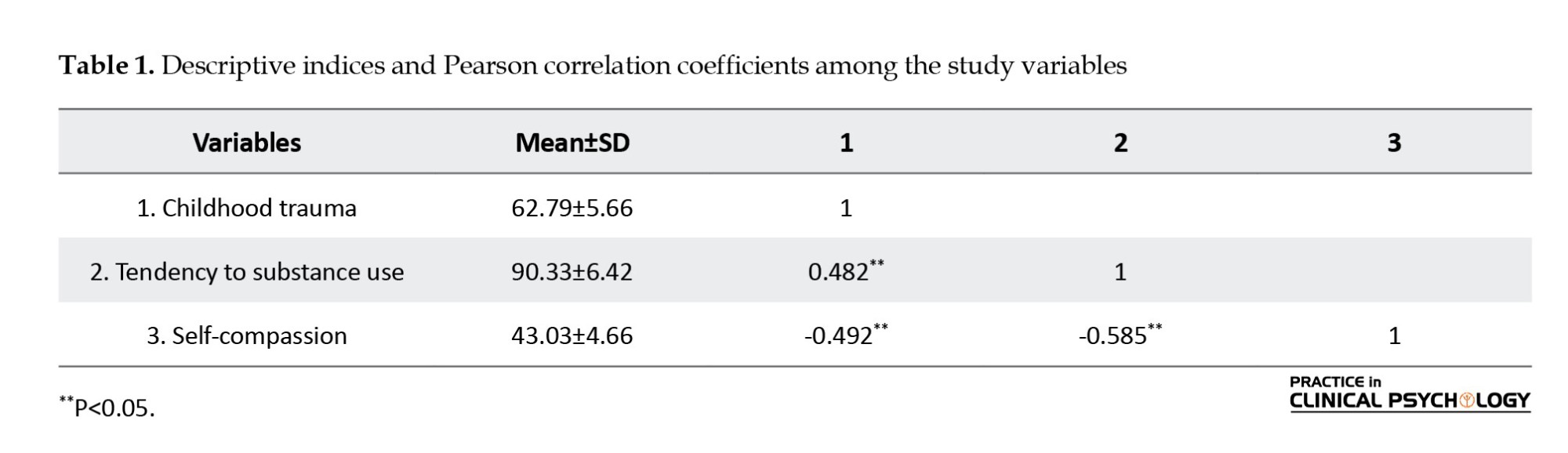
As shown in Table 1, the Mean±SD values for childhood trauma, tendency toward substance use, and self-compassion were 62.79±5.66, 90.33±6.42, and 43.03±4.66, respectively. Significant reciprocal relationships were observed among the study variables.
Before analyzing the data, the assumptions for SEM were examined. The normality of the variables was tested using the Kolmogorov-Smirnov test, with results confirming that the variables followed a normal distribution (P≥0.05). The Durbin-Watson statistic was calculated to check for autocorrelation in the errors, yielding a value of 1.63. Since this value is within the acceptable range of 1.5 to 2.5, the assumption of no autocorrelation was confirmed.
Additionally, the multicollinearity assumptions for the exogenous variables were assessed through the tolerance index and variance inflation factor (VIF). The findings indicated that multicollinearity did not pose a problem, as tolerance values for all variables were close to 1, and VIF values stayed well below the critical threshold of 2. The sample adequacy index was calculated to be 0.74, and Bartlett’s test of sphericity was also conducted (P<0.01). It also confirmed that the data met the necessary conditions for SEM. The explore command in SPSS was applied to identify outliers. The analysis revealed no outliers in any of the study variables, ensuring the suitability of the data for SEM. Similarly, box plots were used to identify univariate outliers for the observed variables, and no outliers were detected. Consequently, there were no issues regarding outliers for SEM analysis.
Table 2 shows the model fit indices for the research model.
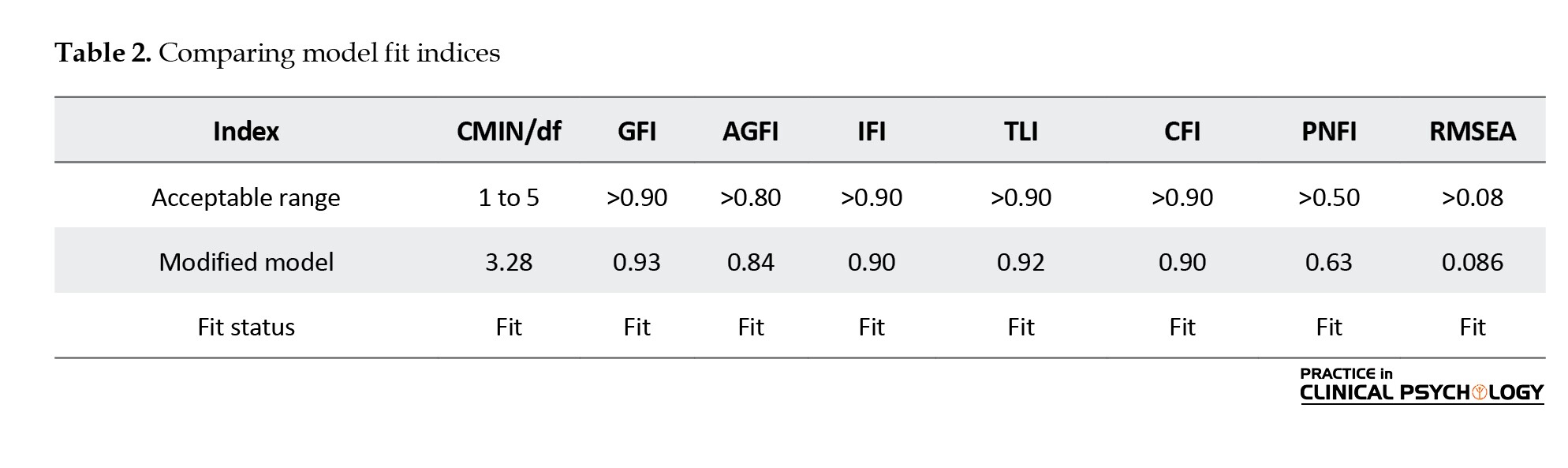
The findings presented in Table 2 demonstrate that, according to the criteria set by Hu and Bentler (1999), the model shows a satisfactory fit (Hu & Bentler, 1999). The standardized path coefficients for the model are displayed in Figure 1.
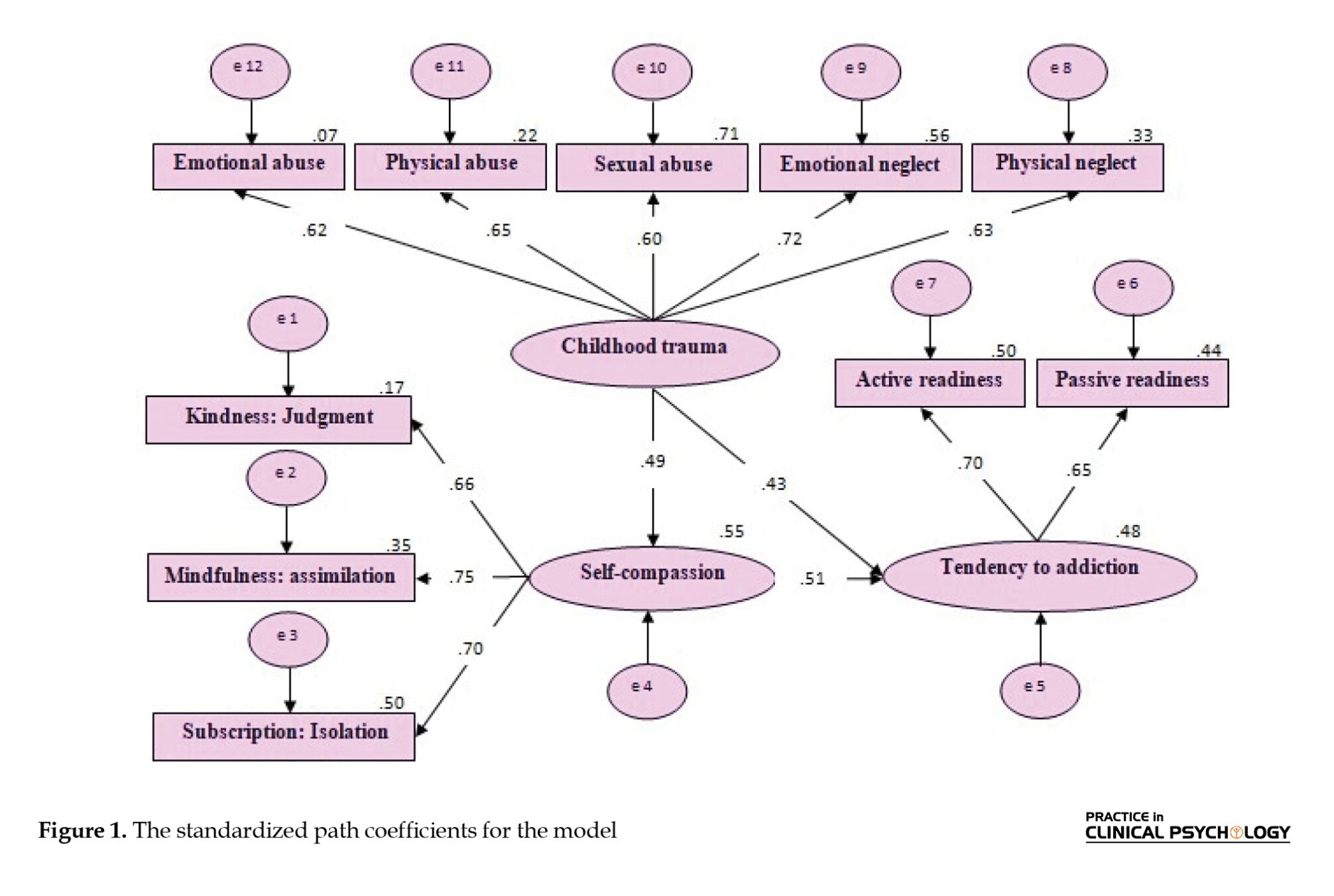
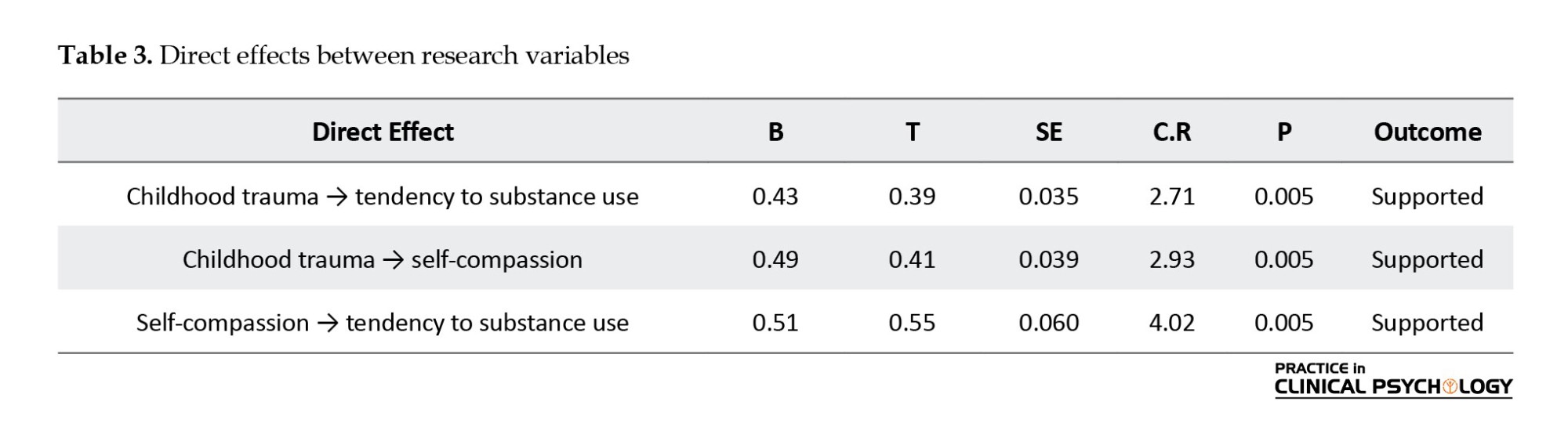
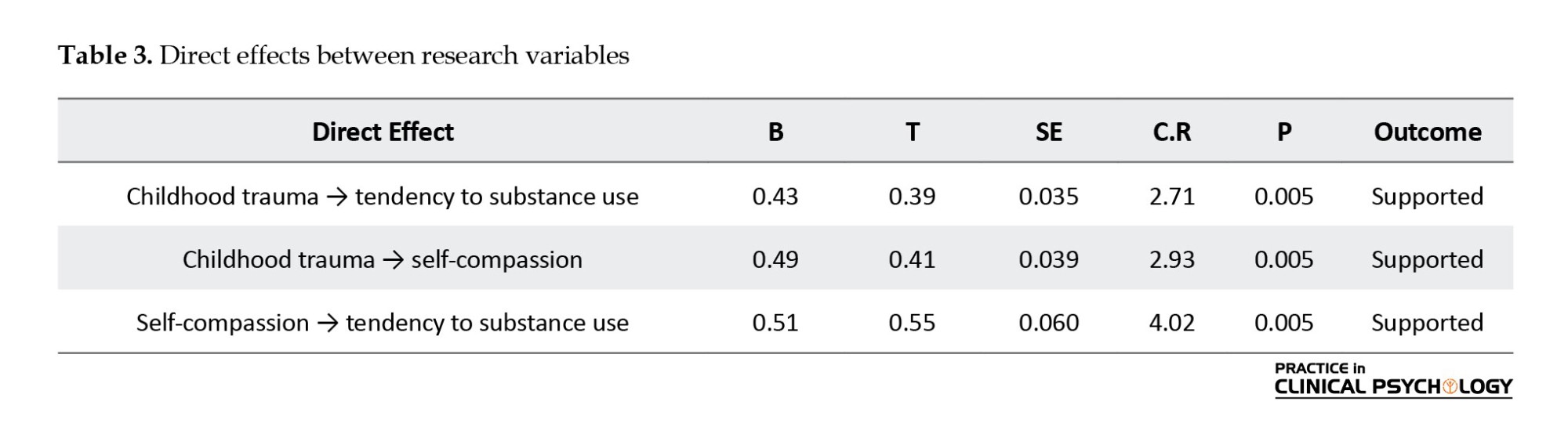
Table 3 displays the direct relationships among the research variables
As Table 3 illustrates, the path coefficients for the direct relationships between the research variables are statistically significant (P<0.005).
To examine the mediating effect of self-compassion on the relationship between childhood trauma and the propensity for substance use, a bootstrapping procedure with 2000 samples was performed using AMOS software. The findings are presented in Table 4.
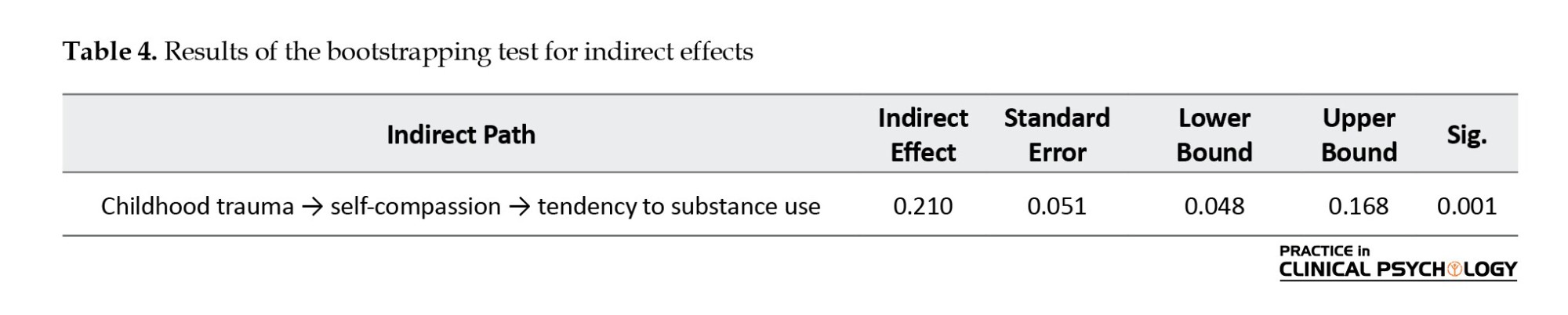
The results shown in the Table 4 suggest that the lower and upper bounds of the indirect effects of childhood trauma on substance use tendency through self-compassion do not encompass zero, indicating the significance of the indirect path and confirming the support for the model.
Discussion
The purpose of this research was to create a model that links childhood trauma to substance use tendencies while investigating the mediating effect of self-compassion among students at Urmia University. The findings revealed a significant positive correlation between childhood trauma and substance use tendencies, both directly and indirectly. In particular, individuals with a history of greater childhood trauma were more inclined to engage in substance use. This outcome supports the conclusions of previous studies (Aldemir et al., 2022; Carlyle et al., 2021; Zhang et al., 2020; Garami et al., 2019; Shin et al., 2018; Vest et al., 2018; Mandavia et al., 2016; Cuomo et al., 2008; Turkman, 2023; Shahab & Kiani Chelmardi, 2020; Mirzaei, 2023). For instance, Carlyle et al. found that individuals with a history of childhood trauma are more prone to engaging in risky and impulsive behaviors, such as substance use (Carlyle et al., 2021). One possible explanation for this finding is rooted in attachment theory. Recent views on attachment, particularly regarding the emergence of substance use tendencies and their connection to attachment-related disorders, emphasize the importance of early relationships in psychological development, especially in the face of childhood trauma and adversity (Parolin & Simonelli, 2016). According to this theory, disruptions in early attachment can lead to anxiety, which may later contribute to substance use problems. Early adverse experiences, especially with caregivers, can invalidate a child’s emotions, causing them to use maladaptive strategies like repressing negative feelings. This condition can increase the likelihood of substance use in adulthood. Additionally, childhood trauma reduces the ability to cope with challenges, resulting in undesirable emotional responses to life events. This outcome may ultimately result in psychological harm and a greater reliance on substances or other risky behaviors, such as those reported by Huang et al. (2022). People with past traumatic experiences may be more susceptible to substance use due to the mood-altering and reinforcing effects that substances offer. This tendency to use substances might reflect their efforts to cope with the biological and neurobiological impacts of childhood trauma, which can include symptoms such as hyperarousal or depersonalization (Bartoli, 2023).
Another set of results reveals a notable inverse correlation between self-compassion and the tendency toward substance use. This outcome supports the conclusions of previous studies (Shreffler et al., 2022; Shahin et al., 2021; Phelps et al., 2018; Dabiri, 2022; Alavi & Ramezani, 2021). Specifically, Kelley et al. showed that a lack of self-compassion is linked to an increased tendency toward substance use (Shreffler et al., 2022). To interpret this finding, it can be argued that self-compassion, functioning as a protective factor, may improve coping strategies for managing stress. If an individual experiences a lack of self-compassion, they may turn to substance use as a means of escaping or neutralizing their stress (Spillane et al., 2022). Furthermore, if individuals, when facing difficulties, inadequacy, or failure, experience self-compassion rather than self-criticism or devaluation, they will have a more accurate and impartial self-perception. Thus, instead of engaging in negative self-judgment, repetitive thinking, and self-blame, which concentrate on the drawbacks and enhance the tendency for substance use, individuals with self-compassion can protect themselves from negative outcomes (Dabiri, 2022). According to the emotion regulation through self-compassion theory, individuals struggling with substance use often rely on maladaptive emotion regulation mechanisms such as avoidance, suppression, or substance use to cope with stress, anxiety, or unpleasant feelings. In this context, self-compassion may be a beneficial alternative to these ineffective coping strategies (Garland, 2010).
Additionally, certain findings from the present study demonstrate a significant negative correlation between childhood trauma and self-compassion. This finding is consistent with the results of studies (Zhang et al., 2020; Pohl et al., 2021; Winders et al., 2020; Ross-Reed et al., 2019; Lessani et al., 2021; Rostami et al., 2014). Specifically, Zhang et al. reported that the more a person experiences abuse during childhood, the lower their level of self-compassion in adulthood (Zhang et al., 2020).
To explain and interpret this finding, childhood adversities, such as maltreatment, overlook, or exposure to violence, may result in feelings of humiliation, guilt, and worthlessness, making self-compassion practice challenging (Farahani et al., 2023). Individuals who do not receive adequate care during early development or grow up in stressful environments may become colder, be more self-critical, and have an underdeveloped self-soothing system alongside an overly activated threat system. These characteristics can potentially activate defensive emotions (including anxiety and depression), resulting in reduced levels of self-compassion (Gilbert & Procter, 2006).
In explaining the mediating role of self-compassion between childhood trauma and substance use tendency, it can be argued that enhancing self-compassion leads to reduced stress and better coping with the negative emotions arising from traumatic experiences. This condition enables individuals to learn healthier ways to soothe their emotions, thereby reducing the likelihood of turning to substance use (Allen & Leary, 2010). Furthermore, self-compassion helps individuals with trauma develop a better understanding of themselves and others, fostering healthy and effective relationships (Nelson et al., 2018), as unhealthy relationships are typically positively correlated with substance use (Tangney et al., 2018). On the other hand, promoting self-compassion in children who have experienced neglect or any form of abuse helps strengthen their self-confidence and sense of worth. This sense of self-worth, derived from self-compassion, can encourage individuals to make healthier and more beneficial life choices, thereby preventing poor decisions that lead to substance use and creating cognitive and behavioral inhibition. Therefore, since self-compassion acts as a protective factor, it may play a mediating role by reducing both the input and output variables in this research.
Conclusion
This research found a notable connection between childhood trauma and the inclination toward substance use, with greater levels of trauma being associated with a higher probability of engaging in substance use. Additionally, the study demonstrated that self-compassion is negatively correlated with substance use, implying that it may offer protective benefits. Fostering self-compassion could help individuals cope with the adverse emotional effects of trauma, thereby reducing the risk of substance use. Consequently, self-compassion might play a crucial role in bridging the gap between childhood trauma and the tendency to engage in substance use, acting as a key factor that influences this relationship.
Study limitations and future research
Despite efforts to ensure research accuracy, inherent limitations exist, such as using a correlational design, which cannot establish causal relationships, and the inability to control variables like family background and sociocultural context. The sample is limited to Urmia University students. To improve generalizability, replication of the study in other urban centers with larger, diverse populations is needed. Based on the findings regarding the mediating role of self-compassion, Mental health professionals should consider incorporating self-compassion methods into their treatment plans to reduce the likelihood of substance use in youth and young adults.
Ethical Considerations
Compliance with ethical guidelines
The Ethics Committee of Urmia University approved this study (Code: IR.URMIA.REC.1403.007). In line with ethical standards for voluntary participation, written informed consent was obtained from all participants. Furthermore, participants were guaranteed that their personal information would be kept confidential.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, writing the original draft, review, editing and investigation: Saba Habibi; Supervision: Esmaeil Soleimani; Methodology: Shirin Zeinali; Data collection: Saba Habibi and Shirin Zeinali; Data analysis: Esmaeil Soleimani and Shirin Zeinali.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely appreciate the contributions of the participants involved in this research.
References
Substance use represents a critical global issue that disrupts familial bonds and undermines the stability of social structures (Room et al., 2024). This issue mainly affects many individuals, especially young individuals (Song et al., 2022). Statistics from the World Health Organization (WHO) show an increase in the production and consumption of these substances worldwide. According to a report by WHO, nearly 200 million people worldwide, aged 15-63, use illegal substances each year (WHO, 2010). The tendency toward substance use encompasses individuals’ beliefs and attitudes regarding specific substances, as well as their perceptions of the potential positive and negative outcomes associated with their use (Davis et al., 2022). Additionally, it is considered a personality vulnerability that makes individuals more prone to engaging in substance use (Volkow & Blanco, 2023). Identifying risk factors and predispositions for substance use and preventing the development of such destructive dependencies are top priorities. This is especially important because the tendency to use substances is a significant risk factor that needs to be addressed, particularly among young people, including students. Many students struggle with coping skills to manage new challenges and emerging problems. As a result, They might resort to harmful coping strategies, like substance use, to manage psychological stress (Vafaie & Kober, 2022). The tendency toward substance use represents a multifaceted social concern influenced by a range of factors, including familial dynamics, socioeconomic status, social context, psychological variables, and experiences of childhood trauma (Belfiore et al., 2024).
Childhood trauma refers to adverse events experienced before the age of 18, generally classified into four key categories: physical abuse, sexual abuse, emotional abuse, and neglect. These incidents often occur within caregiving environments and involve behaviors or failures to act that result in harm, whether physical, sexual, or emotional, to the child (Tang et al., 2020). Physical abuse, which includes violent actions such as hitting, burning, or severe shaking, can result in both physical and psychological harm. Sexual abuse involves inappropriate sexual contact or exploitation through coercion, threats, or deception. Moreover, emotional abuse, defined by behaviors such as humiliation, insults, neglect, and intimidation, can have a lasting impact on a child’s self-esteem and confidence. Moreover, neglect, characterized by the failure to fulfill a child’s basic requirements, such as adequate nutrition, healthcare, emotional support, and psychological safety, can lead to substantial impairments in both physical and cognitive development (Massullo et al., 2023). A significant theoretical perspective on the link between trauma and substance use is the “self-medication theory.” This theory suggests that people who have gone through traumatic experiences often struggle to cope with negative emotions, leading them to seek temporary relief through substance abuse or alcohol as a way to numb their psychological and emotional distress. While drugs and alcohol can initially suppress the activity of the amygdala, the part of the brain responsible for fear and stress, over time, they increase their sensitivity, making the individual even more vulnerable (Khantzian, 1985). Orak et al. demonstrated that childhood traumatic experiences had an impact on the tendency toward substance use (Orak et al., 2023). Additionally, Chandler et al. documented a statistically significant correlation between difficult early life experiences and the likelihood of engaging in substance use (Chandler et al., 2018). The family is the primary environment where a child begins developing. Growing up in an emotionally cold and restrictive environment, combined with exposure to traumatic experiences, can contribute to the development of dysfunctional behaviors, including substance use (He et al., 2022). Consequently, investigating the long-term psychological and physiological impacts of childhood trauma on adult health is of significant importance.
Although a significant and clear relationship has been reported between childhood trauma and the tendency toward substance use, research findings suggest that direct relationships can only partially explain this connection and that mediating variables are likely involved. Therefore, the question that arises is how childhood trauma influences the tendency toward substance use. In this context, self-compassion has drawn the attention of researchers in recent years (Chen, 2019).
Self-compassion refers to an individual’s ability to navigate personal challenges and endure suffering with enhanced emotional resilience and greater ease (Ren et al., 2024). This trait serves as a supportive buffer against the tendency to engage in substance use (Arslan et al., 2024). Self-compassion consists of three fundamental aspects: treating oneself with kindness rather than harsh self-criticism, acknowledging the shared human experience instead of feeling isolated, and practicing mindfulness instead of becoming overly absorbed in or avoiding one’s emotions. The idea of common humanity underscores the understanding that everyone has flaws and makes errors, a universal aspect of the human condition. On the other hand, mindfulness involves staying fully aware and present in the moment without being overwhelmed or detaching from it (Neff, 2003). Shahin et al. indicated a substantial inverse correlation between self-compassion and substance use (Shahin et al., 2021). Moore et al. indicated that substance use is frequently linked to a deficiency in self-compassion (Moore et al., 2022). Since the basis of the structural equation model is correlation and self-compassion is considered a mediating variable, a relationship must exist between the input and output variables in the present study. Research results suggest an association between self-compassion and experiences of childhood trauma. Christoffersen et al. showed a strong connection between early life trauma and self-compassion (Christoffersen et al., 2024). Erol and Inozu indicated that the absence of self-compassion mediates the association between childhood emotional neglect and self-harm without suicidal intent, with a significant relationship observed between these factors (Erol & Inozu, 2024).
Given the psychological, cognitive, and emotional damage caused by substance use and the fact that substance use can significantly harm social, familial, and relational life, it is essential to conduct fundamental studies aimed at preventing the positive tendency toward substance use. In contrast, while several studies have examined the relationships between the variables mentioned above, there has been no investigation into the mediating role of self-compassion in the relationship between childhood trauma and the inclination toward substance use, revealing a significant gap in the existing literature. As such, the current study aims to propose a model that connects childhood trauma to substance use tendency, with self-compassion acting as a mediating variable.
Materials and Methods
Considering the study subject, the research methodology was correlational, utilizing a structural equation modeling (SEM) approach. This study’s sample population comprised all Urmia University students during the 2023-2024 academic year (N=13267). A sample of 350 participants was drawn from this population using multistage random sampling. For this purpose, three faculties were randomly selected as the first cluster from the 11 faculties at Urmia University: The Faculty of Literature and Humanities, the Faculty of Engineering, and the Faculty of Basic Sciences. An invitation was posted on the university’s virtual spaces and bulletin boards to encourage students to participate in the study. The questionnaires were placed on tables in the faculty offices, and after explaining the research objectives, the need for honest participation, and ensuring confidentiality, they were distributed to the students. The students were instructed to complete the questionnaires and submit them to the researcher. Following data collection, the data were analyzed using SPSS software, version 22 and AMOS software employing descriptive analysis and the Pearson correlation coefficient test.
The criteria for participation in the study necessitated the voluntary and informed consent of the students. In contrast, the exclusion criterion was based on submitting incomplete responses to the measurement instruments. Moreover, participants received detailed instructions on how to respond to the questions, were assured of the confidentiality of their answers, and were made aware of their right to withdraw from the study at any time without facing any adverse outcomes.
Study measures
Substance use tendency questionnaire
Created by Weed et al. (1992), the substance use tendency questionnaire includes 36 items and 5 additional items designed to assess social desirability (Weed et al., 1992). It consists of two components: proactive readiness and passive readiness. Proactive readiness is associated with antisocial behaviors, a tendency toward substance use, favorable attitudes toward substances, depression, and a strong inclination toward seeking new and intense sensations (items 3, 4, 7, 8, 10, 11, 15, 16, 18, 19, 21, 22, 25, 26, 28, 29, 31, 34, 36, 37, 38, 40, 41). However, passive readiness predominantly relates to lack of assertiveness and depression (items 1, 2, 5, 6, 9, 12, 13, 14, 17, 20, 23, 24, 27, 30, 32, 35, 39). Each statement is assessed using a scale where 0 represents “strongly disagree” and 3 represents “strongly agree.” However, the scoring for items 6, 12, 15, and 21 is reversed. The questionnaire includes a social desirability scale for items 33, 21, 15, 13, and 12. In Zargar et al.’s (2013) study, the questionnaire’s content, face, and criterion validity were deemed appropriate for assessment. Two methods were employed to assess the validity of this scale. Concerning criterion validity, the questionnaire successfully differentiated between addicted and nonaddicted groups. Construct validity was evaluated by examining its correlation with the 25-item clinical symptoms checklist, resulting in a significant correlation of 0.45. The reliability of the scale, assessed using the Cronbach α, was determined to be 0.90, suggesting a high level of internal consistency (Zargar et al., 2013). In the current study, the Cronbach α was calculated to be 0.75.
Childhood trauma questionnaire (CTQ)
The CTQ was designed by Bernstein et al. The questionnaire measures experiences of early developmental trauma and abuse (Bernstein et al., 2003). This screening tool detects childhood abuse and neglect and is suitable for both adults and adolescents. It includes 28 items, with 25 focusing on key aspects of childhood trauma and 3 assessing possible denial of past experiences. The questionnaire covers five types of maltreatment: physical abuse, sexual abuse, emotional abuse, emotional neglect, and physical neglect. In Bernstein et al.’s (2003)study, the Cronbach α values ranged from 0.78 to 0.95 for various abuse types, with concurrent validity between 0.59 and 0.78. In Iran, Ebrahimi et al. (2014) reported Cronbach α values between 0.81 and 0.98, and in the current study, the value was 0.81, confirming the tool’s reliability.
Self-compassion scale short form (SCS-SF)
The 12-item SCS-SF, also known as the self-compassion questionnaire, was developed by Neff et al. in 2011. This scale includes six dimensions: Self-kindness (items 2 and 6), self-judgment (items 11 and 12), common humanity (items 5 and 10), isolation (items 4 and 8), mindfulness (items 3 and 7), and overidentification (items 1 and 9). Responses are rated on a Likert scale ranging from 1 to 5. It includes reverse scoring for items 1, 4, 8, 9, 11 and 12. Shahbazi et al. (2015) used the 12-item short form of this scale, which comprises six subscales, each with two items, as developed by Neff et al., to measure self-compassion (Sh, 2015; Neff, 2011). The questionnaire demonstrated satisfactory content, construct, and criterion validity in their research, with the overall Cronbach α coefficient for the scale exceeding 0.70. Moreover, the Cronbach α values were reported to be 0.77, 0.92, 0.88, 0.91, 0.87, and 0.83 for the subscales self-kindness, self-judgment, common humanity, isolation, mindfulness, and overidentification, respectively. The concurrent and convergent validity of the questionnaire was also favorable. In the present study, the Cronbach α for the questionnaire was 0.77, indicating the tool’s reliability.
Results
The results indicated that among the participants in this study, 112(36.36%) were from the Faculty of Engineering, 98(29.44%) from the Faculty of Basic Sciences, and 140(39.20%) from the Faculty of Humanities. Furthermore, 206 participants (57.68%) were aged between 20 and 25 years, 96 participants (26.88%) were aged between 26 and 30 years, 32 participants (8.96%) were aged between 31 and 35 years, and 16 participants (4.48%) were over 35 years old. Regarding sex, 126 participants (35.28%) were male, and 224(64.72%) were female.
Since the SEM approach is based on the correlation matrix, Table 1 shows the Pearson correlation coefficients for the study variables and descriptive statistics. Moreover, the skewness and kurtosis values for all the observed variables ranged from -2 to +2, suggesting that the data followed a normal distribution and were appropriate for SEM analysis.
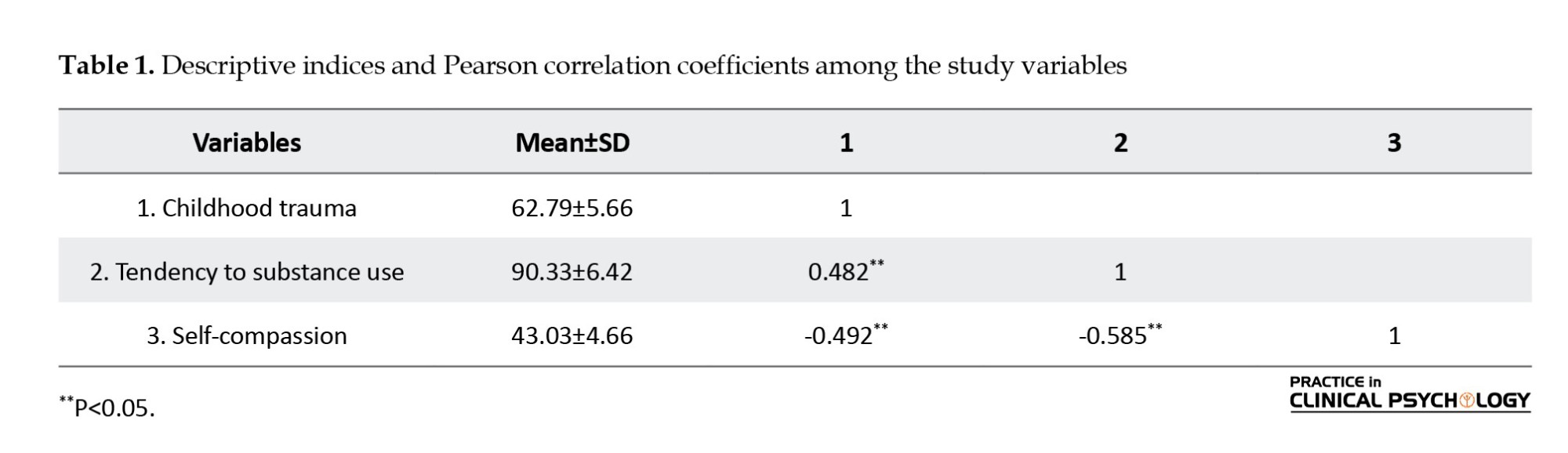
As shown in Table 1, the Mean±SD values for childhood trauma, tendency toward substance use, and self-compassion were 62.79±5.66, 90.33±6.42, and 43.03±4.66, respectively. Significant reciprocal relationships were observed among the study variables.
Before analyzing the data, the assumptions for SEM were examined. The normality of the variables was tested using the Kolmogorov-Smirnov test, with results confirming that the variables followed a normal distribution (P≥0.05). The Durbin-Watson statistic was calculated to check for autocorrelation in the errors, yielding a value of 1.63. Since this value is within the acceptable range of 1.5 to 2.5, the assumption of no autocorrelation was confirmed.
Additionally, the multicollinearity assumptions for the exogenous variables were assessed through the tolerance index and variance inflation factor (VIF). The findings indicated that multicollinearity did not pose a problem, as tolerance values for all variables were close to 1, and VIF values stayed well below the critical threshold of 2. The sample adequacy index was calculated to be 0.74, and Bartlett’s test of sphericity was also conducted (P<0.01). It also confirmed that the data met the necessary conditions for SEM. The explore command in SPSS was applied to identify outliers. The analysis revealed no outliers in any of the study variables, ensuring the suitability of the data for SEM. Similarly, box plots were used to identify univariate outliers for the observed variables, and no outliers were detected. Consequently, there were no issues regarding outliers for SEM analysis.
Table 2 shows the model fit indices for the research model.
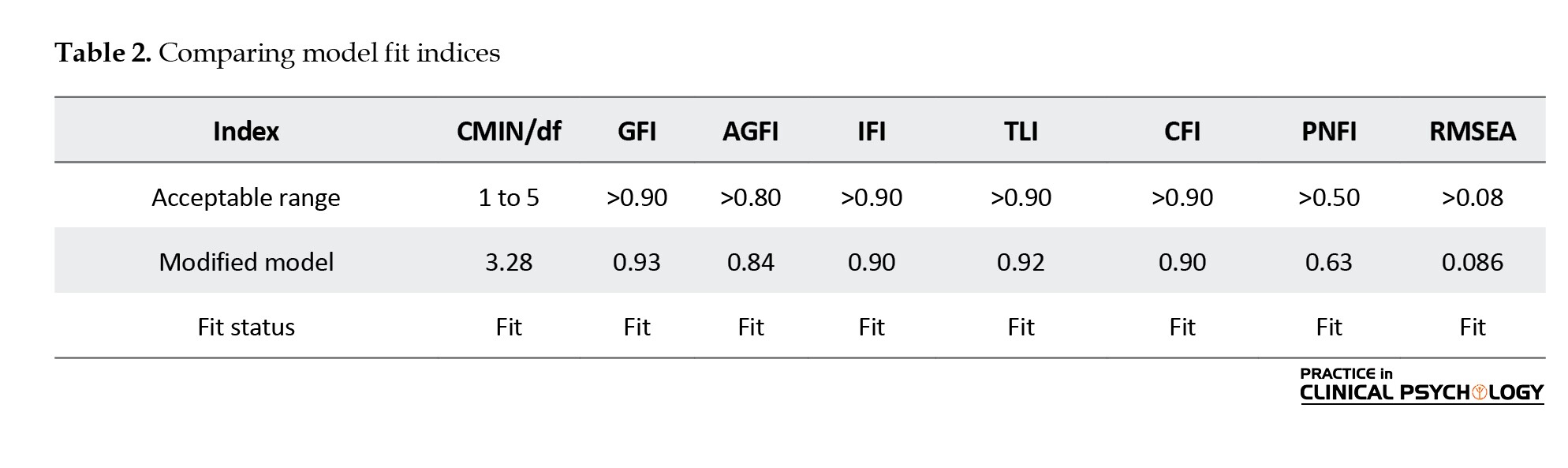
The findings presented in Table 2 demonstrate that, according to the criteria set by Hu and Bentler (1999), the model shows a satisfactory fit (Hu & Bentler, 1999). The standardized path coefficients for the model are displayed in Figure 1.
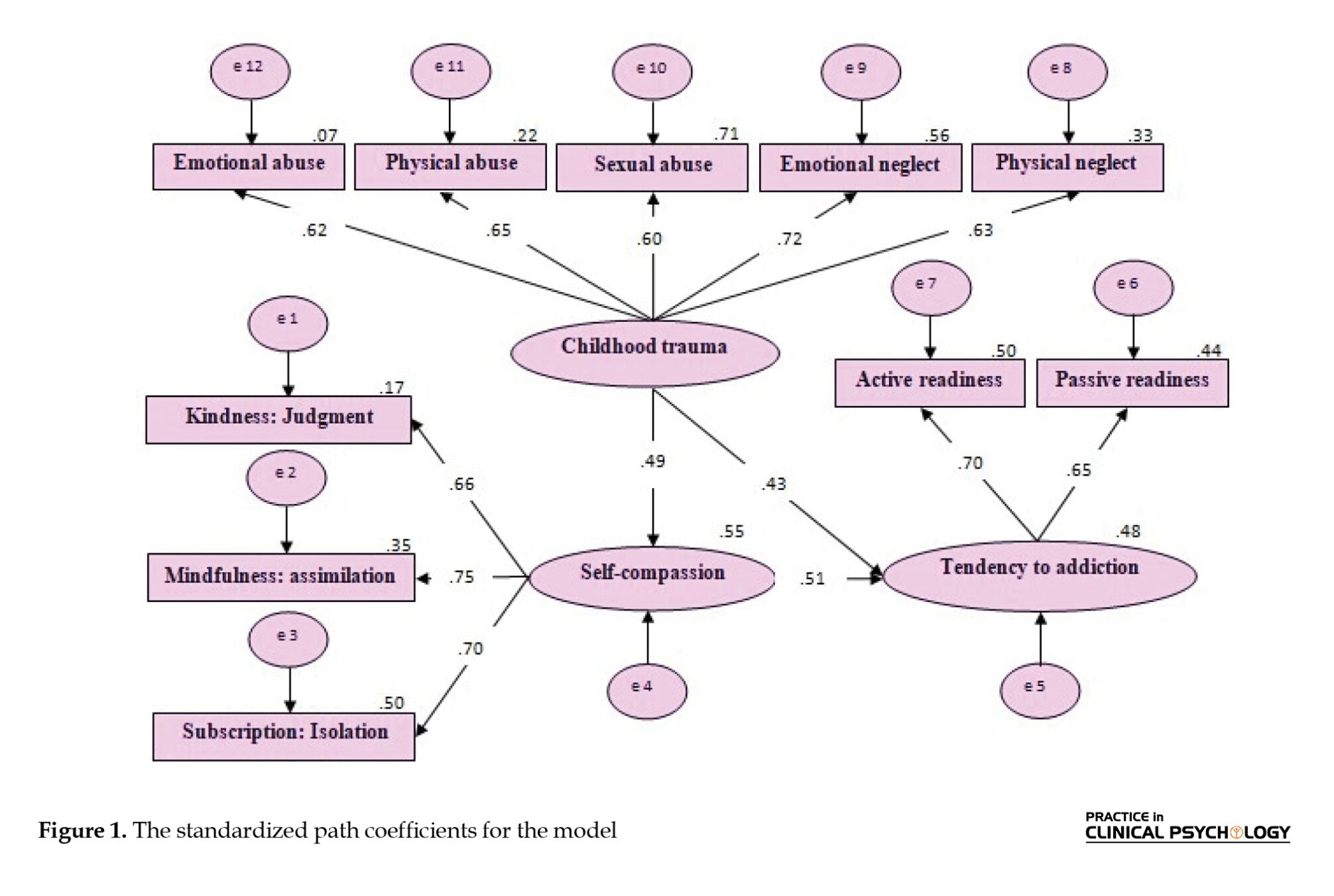
Table 3 displays the direct relationships among the research variables
As Table 3 illustrates, the path coefficients for the direct relationships between the research variables are statistically significant (P<0.005).
To examine the mediating effect of self-compassion on the relationship between childhood trauma and the propensity for substance use, a bootstrapping procedure with 2000 samples was performed using AMOS software. The findings are presented in Table 4.
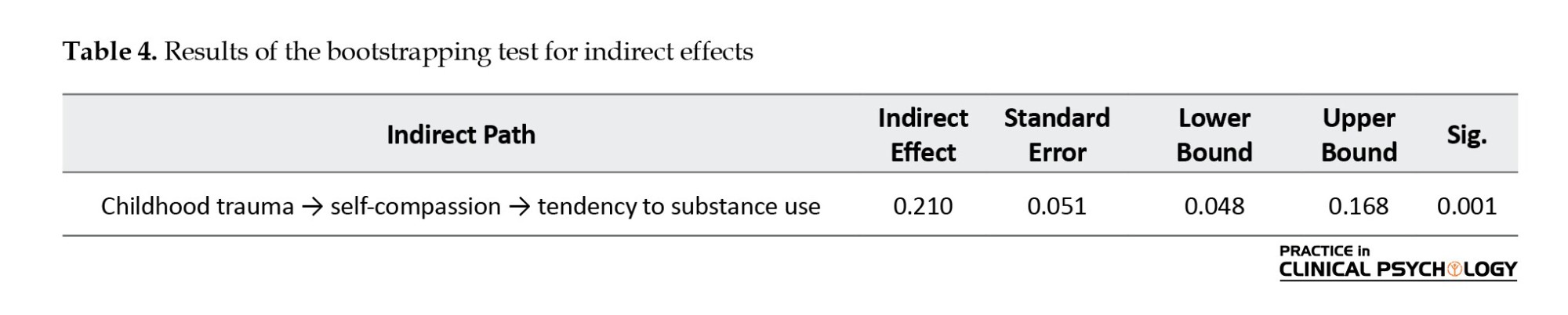
The results shown in the Table 4 suggest that the lower and upper bounds of the indirect effects of childhood trauma on substance use tendency through self-compassion do not encompass zero, indicating the significance of the indirect path and confirming the support for the model.
Discussion
The purpose of this research was to create a model that links childhood trauma to substance use tendencies while investigating the mediating effect of self-compassion among students at Urmia University. The findings revealed a significant positive correlation between childhood trauma and substance use tendencies, both directly and indirectly. In particular, individuals with a history of greater childhood trauma were more inclined to engage in substance use. This outcome supports the conclusions of previous studies (Aldemir et al., 2022; Carlyle et al., 2021; Zhang et al., 2020; Garami et al., 2019; Shin et al., 2018; Vest et al., 2018; Mandavia et al., 2016; Cuomo et al., 2008; Turkman, 2023; Shahab & Kiani Chelmardi, 2020; Mirzaei, 2023). For instance, Carlyle et al. found that individuals with a history of childhood trauma are more prone to engaging in risky and impulsive behaviors, such as substance use (Carlyle et al., 2021). One possible explanation for this finding is rooted in attachment theory. Recent views on attachment, particularly regarding the emergence of substance use tendencies and their connection to attachment-related disorders, emphasize the importance of early relationships in psychological development, especially in the face of childhood trauma and adversity (Parolin & Simonelli, 2016). According to this theory, disruptions in early attachment can lead to anxiety, which may later contribute to substance use problems. Early adverse experiences, especially with caregivers, can invalidate a child’s emotions, causing them to use maladaptive strategies like repressing negative feelings. This condition can increase the likelihood of substance use in adulthood. Additionally, childhood trauma reduces the ability to cope with challenges, resulting in undesirable emotional responses to life events. This outcome may ultimately result in psychological harm and a greater reliance on substances or other risky behaviors, such as those reported by Huang et al. (2022). People with past traumatic experiences may be more susceptible to substance use due to the mood-altering and reinforcing effects that substances offer. This tendency to use substances might reflect their efforts to cope with the biological and neurobiological impacts of childhood trauma, which can include symptoms such as hyperarousal or depersonalization (Bartoli, 2023).
Another set of results reveals a notable inverse correlation between self-compassion and the tendency toward substance use. This outcome supports the conclusions of previous studies (Shreffler et al., 2022; Shahin et al., 2021; Phelps et al., 2018; Dabiri, 2022; Alavi & Ramezani, 2021). Specifically, Kelley et al. showed that a lack of self-compassion is linked to an increased tendency toward substance use (Shreffler et al., 2022). To interpret this finding, it can be argued that self-compassion, functioning as a protective factor, may improve coping strategies for managing stress. If an individual experiences a lack of self-compassion, they may turn to substance use as a means of escaping or neutralizing their stress (Spillane et al., 2022). Furthermore, if individuals, when facing difficulties, inadequacy, or failure, experience self-compassion rather than self-criticism or devaluation, they will have a more accurate and impartial self-perception. Thus, instead of engaging in negative self-judgment, repetitive thinking, and self-blame, which concentrate on the drawbacks and enhance the tendency for substance use, individuals with self-compassion can protect themselves from negative outcomes (Dabiri, 2022). According to the emotion regulation through self-compassion theory, individuals struggling with substance use often rely on maladaptive emotion regulation mechanisms such as avoidance, suppression, or substance use to cope with stress, anxiety, or unpleasant feelings. In this context, self-compassion may be a beneficial alternative to these ineffective coping strategies (Garland, 2010).
Additionally, certain findings from the present study demonstrate a significant negative correlation between childhood trauma and self-compassion. This finding is consistent with the results of studies (Zhang et al., 2020; Pohl et al., 2021; Winders et al., 2020; Ross-Reed et al., 2019; Lessani et al., 2021; Rostami et al., 2014). Specifically, Zhang et al. reported that the more a person experiences abuse during childhood, the lower their level of self-compassion in adulthood (Zhang et al., 2020).
To explain and interpret this finding, childhood adversities, such as maltreatment, overlook, or exposure to violence, may result in feelings of humiliation, guilt, and worthlessness, making self-compassion practice challenging (Farahani et al., 2023). Individuals who do not receive adequate care during early development or grow up in stressful environments may become colder, be more self-critical, and have an underdeveloped self-soothing system alongside an overly activated threat system. These characteristics can potentially activate defensive emotions (including anxiety and depression), resulting in reduced levels of self-compassion (Gilbert & Procter, 2006).
In explaining the mediating role of self-compassion between childhood trauma and substance use tendency, it can be argued that enhancing self-compassion leads to reduced stress and better coping with the negative emotions arising from traumatic experiences. This condition enables individuals to learn healthier ways to soothe their emotions, thereby reducing the likelihood of turning to substance use (Allen & Leary, 2010). Furthermore, self-compassion helps individuals with trauma develop a better understanding of themselves and others, fostering healthy and effective relationships (Nelson et al., 2018), as unhealthy relationships are typically positively correlated with substance use (Tangney et al., 2018). On the other hand, promoting self-compassion in children who have experienced neglect or any form of abuse helps strengthen their self-confidence and sense of worth. This sense of self-worth, derived from self-compassion, can encourage individuals to make healthier and more beneficial life choices, thereby preventing poor decisions that lead to substance use and creating cognitive and behavioral inhibition. Therefore, since self-compassion acts as a protective factor, it may play a mediating role by reducing both the input and output variables in this research.
Conclusion
This research found a notable connection between childhood trauma and the inclination toward substance use, with greater levels of trauma being associated with a higher probability of engaging in substance use. Additionally, the study demonstrated that self-compassion is negatively correlated with substance use, implying that it may offer protective benefits. Fostering self-compassion could help individuals cope with the adverse emotional effects of trauma, thereby reducing the risk of substance use. Consequently, self-compassion might play a crucial role in bridging the gap between childhood trauma and the tendency to engage in substance use, acting as a key factor that influences this relationship.
Study limitations and future research
Despite efforts to ensure research accuracy, inherent limitations exist, such as using a correlational design, which cannot establish causal relationships, and the inability to control variables like family background and sociocultural context. The sample is limited to Urmia University students. To improve generalizability, replication of the study in other urban centers with larger, diverse populations is needed. Based on the findings regarding the mediating role of self-compassion, Mental health professionals should consider incorporating self-compassion methods into their treatment plans to reduce the likelihood of substance use in youth and young adults.
Ethical Considerations
Compliance with ethical guidelines
The Ethics Committee of Urmia University approved this study (Code: IR.URMIA.REC.1403.007). In line with ethical standards for voluntary participation, written informed consent was obtained from all participants. Furthermore, participants were guaranteed that their personal information would be kept confidential.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, writing the original draft, review, editing and investigation: Saba Habibi; Supervision: Esmaeil Soleimani; Methodology: Shirin Zeinali; Data collection: Saba Habibi and Shirin Zeinali; Data analysis: Esmaeil Soleimani and Shirin Zeinali.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely appreciate the contributions of the participants involved in this research.
References
Alavi, K., & Ramezani, S. (2021). [The role of perceived parenting styles and self-compassion in predicting addiction readiness in the youth (Persian)]. Scientific Quarterly Research on Addiction, 14(58), 89-112. [Link]
Aldemir, E., Akyel, B., & Havaceligi Atlam, D. (2022). Resilience and childhood trauma in a substance-dependent sample: A cross-sectional, controlled study. Journal of Substance Use, 27(5), 465-469. [DOI:10.1080/14659891.2021.1961322]
Allen, A. B., & Leary, M. R. (2010). Self‐Compassion, stress, and coping. Social and Personality Psychology Compass, 4(2), 107-118. [DOI:10.1111/j.1751-9004.2009.00246.x] [PMID]
Arslan, G., Uzun, K., Güven, A. Z., & Gürsu, O. (2024). Psychological flexibility, self-compassion, subjective well-being, and substance misuse in college students: A serial mediation model. Journal of Ethnicity in Substance Abuse, 1-22. [DOI:10.1080/15332640.2024.2366981]
Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., & Ahluvalia, T., et al. (2003). Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse & Neglect, 27(2), 169-190. [Link]
Bartoli, F. (2023). The lithium paradox: Declining prescription of the gold standard treatment for bipolar disorder. Acta Psychiatrica Scandinavica, 147(3), 314–315. [DOI:10.1111/acps.13525] [PMID]
Belfiore, C. I., Galofaro, V., Cotroneo, D., Lopis, A., Tringali, I., & Denaro, V., et al. (2024). A multi-level analysis of biological, social, and psychological determinants of substance use disorder and co-occurring mental health outcomes. Psychoactives, 3(2), 194-214. [DOI:10.3390/psychoactives3020013]
Carlyle, M., Broomby, R., Simpson, G., Hannon, R., Fawaz, L., & Mollaahmetoglu, O. M., et al. (2021). A randomised, double‐blind study investigating the relationship between early childhood trauma and the rewarding effects of morphine. Addiction Biology, 26(6), e13047. [DOI:10.1111/adb.13047] [PMID]
Chandler, G. E., Kalmakis, K. A., & Murtha, T. (2018). Screening adults with substance use disorder for adverse childhood experiences. Journal of Addictions Nursing, 29(3), 172-178. [DOI:10.1097/JAN.0000000000000233] [PMID]
Chen, G. (2019). The role of self-compassion in recovery from substance use disorders. OBM Integrative and Complementary Medicine, 4(2), 026. [DOI:10.21926/obm.icm.1902026]
Christoffersen, H., Skårderud, H. R., Vrabel, K., & Weider, S. (2024). Self-compassion as a mechanism of change in patients with eating disorders and childhood trauma receiving CFT-E; a study of within-person processes. Nordic Psychology, 76(2), 267-283. [DOI:10.1080/19012276.2023.2192396]
Cuomo, C., Sarchiapone, M., Giannantonio, M. D., Mancini, M., & Roy, A. (2008). Aggression, impulsivity, personality traits, and childhood trauma of prisoners with substance abuse and addiction. The American Journal of Drug and Alcohol Abuse, 34(3), 339-345. [DOI:10.1080/00952990802010884] [PMID]
Dabiri, S. (2022). [The role of self-control, emotions, and self-compassion in the prediction of addiction readiness (Persian)]. Scientific Quarterly Research on Addiction, 16(65), 311-332. [DOI:10.52547/etiadpajohi.16.65.311]
Davis, C. S., Lieberman, A. J., & O’Kelley-Bangsberg, M. (2022). Legality of drug checking equipment in the United States: A systematic legal analysis. Drug and Alcohol Dependence, 234, 109425. [DOI:10.1016/j.drugalcdep.2022.109425] [PMID]
Ebrahimi, H., Dezhkam, M., Soghotal-Eslam, T. (2013). Childhood traumas and suicide attempts in adulthood. Iranian Journal of Psychiatry and Clinical Psychology, 19(4), 275–282. [Link]
Erol, Y., & Inozu, M. (2024). An investigation of the mediating roles of emotion regulation difficulties, distress tolerance, self-compassion, and self-disgust in the association between childhood trauma and nonsuicidal self-injury. Archives of Suicide Research, 28(3), 815-829. [DOI:10.1080/13811118.2023.2237083] [PMID]
Farahani, H., Azadfallah, P., Watson, P., Qaderi, K., Pasha, A., & Dirmina, F., et al. (2022). Predicting the social-emotional competence based on childhood trauma, internalized shame, disability/shame Scheme, Cognitive flexibility, distress tolerance and alexithymia in an Iranian sample using Bayesian regression. Journal of Child & Adolescent Trauma, 16(2), 351-363. [DOI:10.1007/s40653-022-00501-1] [PMID]
Garami, J., Valikhani, A., Parkes, D., Haber, P., Mahlberg, J., & Misiak, B., et al. (2019). Examining perceived stress, childhood trauma and interpersonal trauma in individuals with drug addiction. Psychological Reports, 122(2), 433-450. [DOI:10.1177/0033294118764918] [PMID]
Garland, E. L., Fredrickson, B., Kring, A. M., Johnson, D. P., Meyer, P. S., & Penn, D. L. (2010). Upward spirals of positive emotions counter downward spirals of negativity: Insights from the broaden-and-build theory and affective neuroscience on the treatment of emotion dysfunctions and deficits in psychopathology. Clinical Psychology Review, 30(7), 849-864. [DOI:10.1016/j.cpr.2010.03.002] [PMID]
Gilbert, P., & Procter, S. (2006). Compassionate mind training for people with high shame and self‐criticism: Overview and pilot study of a group therapy approach. Clinical Psychology & Psychotherapy: An International Journal of Theory & Practice, 13(6), 353-379. [DOI:10.1002/cpp.507]
He, J., Yan, X., Wang, R., Zhao, J., Liu, J., & Zhou, C., et al. (2022). Does childhood adversity lead to drug addiction in adulthood? A study of serial mediators based on resilience and depression. Frontiers in Psychiatry, 13, 871459. [DOI:10.3389/fpsyt.2022.871459] [PMID]
Hu, L. t., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1-55. [DOI:10.1080/10705519909540118]
Huang, C., Yuan, Q., Ge, M., Sheng, X., Yang, M., & Shi, S., et al. (2022). Childhood trauma and non-suicidal self-injury among Chinese adolescents: The mediating role of psychological sub-health. Frontiers in Psychiatry, 13, 798369. [DOI:10.3389/fpsyt.2022.798369] [PMID]
Khantzian, E. J. (1985). Psychotherapeutic interventions with substance abusers. Journal of Substance Abuse Treatment, 2(2), 88-83. [DOI:10.1016/0740-5472(85)90031-5] [PMID]
Lessani, S., Shahgholian, M., Sarafraz, M. R., & Abdollahi, M. H. (2021). [Prediction of pathological narcissism based on childhood trauma with the mediating role of self-compassion deficit and shame (Persian)]. Journal of Psychological Science, 20(97), 77-88. [Link]
Mandavia, A., Robinson, G. G., Bradley, B., Ressler, K. J., & Powers, A. (2016). Exposure to childhood abuse and later substance use: Indirect effects of emotion dysregulation and exposure to trauma. Journal of Traumatic Stress, 29(5), 422-429. [DOI:10.1002/jts.22131] [PMID]
Massullo, C., De Rossi, E., Carbone, G. A., Imperatori, C., Ardito, R. B., & Adenzato, M., et al. (2023). Child maltreatment, abuse, and neglect: An umbrella review of their prevalence and definitions. Clinical Neuropsychiatry, 20(2), 72-99. [PMID]
Lassri, D., Gewirtz-Meydan, A., & Zamir, O. (2023). The mediating role of self-compassion between childhood maltreatment and satisfaction with intimate relationships. Mindfulness, 14(4), 970–978. [DOI:10.1007/s12671-023-02107-6]
Moore, S. K., Okst, K., Smith, L., Fatkin, T., Creedon, T., & Fredericksen, A. K., et al. (2022). “Today I can look in the mirror and like myself”: effects of a trauma-informed mindful recovery program on self-compassion. Frontiers in Psychology, 13, 780383. [DOI:10.3389/fpsyg.2022.780383] [PMID]
Neff, K. D. (2003). The development and validation of a scale to measure self-compassion. Self and Identity, 2(3), 223-250. [DOI:10.1080/15298860309027]
Neff, K. D. (2011). Self‐compassion, self‐esteem, and well‐being. Social and Personality Psychology Compass, 5(1), 1-12. [DOI:10.1111/j.1751-9004.2010.00330.x]
Nelson, J. R., Hall, B. S., Anderson, J. L., Birtles, C., & Hemming, L. (2018). Self-compassion as self-care: A simple and effective tool for counselor educators and counseling students. Journal of Creativity in Mental Health, 13(1), 121-133. [DOI:10.1080/15401383.2017.1328292]
Orak, O. S., Bilkay, H. İ., & Zengin, Ç. (2023). Effect of childhood trauma on substance users’ attitudes of coping with stress. Journal of Dependence, 24(3), 305-315. [DOI:10.51982/bagimli.1168435]
World Health Organization (WHO). (2010). Global report on antimalarial drug efficacy and drug resistance: 2000-2010. Geneva: World Health Organization. [Link]
Parolin, M., & Simonelli, A. (2016). Attachment theory and maternal drug addiction: The contribution to parenting interventions. Frontiers in Psychiatry, 7, 152. [DOI:10.3389/fpsyt.2016.00152] [PMID]
Phelps, C. L., Paniagua, S. M., Willcockson, I. U., & Potter, J. S. (2018). The relationship between self-compassion and the risk for substance use disorder. Drug and Alcohol Dependence, 183, 78-81. [DOI:10.1016/j.drugalcdep.2017.10.026] [PMID]
Pohl, S., Steuwe, C., Mainz, V., Driessen, M., & Beblo, T. (2021). Borderline personality disorder and childhood trauma: Exploring the buffering role of self‐compassion and self‐esteem. Journal of Clinical Psychology, 77(3), 837-845. [DOI:10.1002/jclp.23070] [PMID]
Ren, Y., Zhang, S., Huang, C., Zhang, J., Jiang, T., & Fang, Y. (2024). Perceived parental rearing styles and depression in Chinese adolescents: The mediating role of self-compassion. Frontiers in Psychiatry, 15, 1417355. [DOI:10.3389/fpsyt.2024.1417355] [PMID]
Room, R., Cook, M., & Laslett, A. M. (2024). Substance use and the Sustainable Development Goals: Will development bring greater problems? Drugs: Education, Prevention and Policy, 31(1), 148-157. [DOI:10.1080/09687637.2022.2150125]
Ross-Reed, D. E., Reno, J., Peñaloza, L., Green, D., & FitzGerald, C. (2019). Family, school, and peer support are associated with rates of violence victimization and self-harm among gender minority and cisgender youth. The Journal of adolescent Health: Official Publication of the Society for Adolescent Medicine, 65(6), 776–783. [DOI:10.1016/j.jadohealth.2019.07.013] [PMID]
Rostami, M., Abdi, M., & Heidari, H. (2014). [Correlation of childhood maltreatment, self-compassion and mental health in married people (Persian)]. Journal of Fundamentals of Mental Health, 16(62), 130-141. [DOI:10.22038/jfmh.2014.3269]
Sh, M. (2015). [Confirmatory factor analysis of the Persian version of the self-compassion rating scale-revised (Persian)]. Psychological Methods and Models, 6(19), 31-46. [Link]
Shahab, M., & Kiani Chelmardi, A. (2020). [Predicting addiction, anxiety and impulsivity based on adverse childhood experiences, depression, hopelessness and parental health among adolescent girls (Persian)]. Quarterly Journal of Woman and Society, 11(41), 261-278. [Link]
Shahbazi, M., Rajabi, G., Maqami, E., Jelodari, A. (2015). Confirmatory factor structure of the Persian version of the revised self-compassion scale in a group of prisoners. Quarterly Journal of Psychological Methods and Models, 6(19), 31–46. [Link]
Shahin, M. A. H., Hamed, S. A., & Taha, S. M. (2021). Correlation of self-compassion and spiritual well-being with drug craving in people with substance use disorders. Middle East Current Psychiatry, 28, 1-12. [DOI:10.1186/s43045-021-00132-6]
Shin, S. H., McDonald, S. E., & Conley, D. (2018). Patterns of adverse childhood experiences and substance use among young adults: A latent class analysis. Addictive Behaviors, 78, 187-192. [DOI:10.1016/j.addbeh.2017.11.020] [PMID]
Shreffler, J., Thomas, J. J., McGee, S., Ferguson, B., Kelley, J., & Cales, R., et al. (2022). Self-compassion in individuals with substance use disorder: The association with personal growth and well-being. Journal of Addictive Diseases, 40(3), 366-372. [DOI:10.1080/10550887.2021.2005382] [PMID]
Song, S., Zilverstand, A., Gui, W., Pan, X., & Zhou, X. (2022). Reducing craving and consumption in individuals with drug addiction, obesity or overeating through neuromodulation intervention: a systematic review and meta‐analysis of its follow‐up effects. Addiction, 117(5), 1242-1255. [DOI:10.1111/add.15686] [PMID]
Spillane, N. S., Schick, M. R., Goldstein, S. C., Nalven, T., & Kahler, C. W. (2022). The protective effects of self-compassion on alcohol-related problems among first nation adolescents. Addiction Research & Theory, 30(1), 33-40. [DOI:10.1080/16066359.2021.1902994] [PMID]
Tang, W., Hu, T., Hu, B., Jin, C., Wang, G., & Xie, C., et al. (2020). Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. Journal of Affective Disorders, 274, 1-7. [DOI:10.1016/j.jad.2020.05.009] [PMID]
Tangney, J. P., Boone, A. L., & Baumeister, R. F. (2018). High self-control predicts good adjustment, less pathology, better grades, and interpersonal success. In: Baumeister R, editor. Self-regulation and self-control (pp. 173-212). London: Routledge. [DOI:10.4324/9781315175775-5]
Torkaman, M., Davoodi, A., Naziry, G. and Fath, N. (2023). [The relationship between childhood trauma and tendency toward substance abuse considering the mediating role of cognitive flexibility and rumination in individuals with post-traumatic stress disorder (Persian)]. Quarterly Journal of Modern Psychological Researches, 17(68), 81-90. [Link]
Vafaie, N., & Kober, H. (2022). Association of drug cues and craving with drug use and relapse: A systematic review and meta-analysis. JAMA Psychiatry, 79(7), 641-650. [DOI:10.1001/jamapsychiatry.2022.1240] [PMID]
Vest, B. M., Hoopsick, R. A., Homish, D. L., Daws, R. C., & Homish, G. G. (2018). Childhood trauma, combat trauma, and substance use in National Guard and reserve soldiers. Substance Abuse, 39(4), 452-460. [DOI:10.1080/08897077.2018.1443315] [PMID]
Volkow, N. D., & Blanco, C. (2023). Substance use disorders: a comprehensive update of classification, epidemiology, neurobiology, clinical aspects, treatment and prevention. World Psychiatry, 22(2), 203-229. [DOI:10.1002/wps.21073] [PMID]
Weed, N. C., Butcher, J. N., McKenna, T., & Ben-Porath, Y. S. (1992). New measures for assessing alcohol and drug abuse with the MMPI-2: The APS and AAS. Journal of Personality Assessment, 58(2), 389-404. [DOI:10.1207/s15327752jpa5802_15] [PMID]
Winders, S. J., Murphy, O., Looney, K., & O’Reilly, G. (2020). Self‐compassion, trauma, and posttraumatic stress disorder: A systematic review. Clinical Psychology & Psychotherapy, 27(3), 300-329. [DOI:10.1002/cpp.2429] [PMID]
Zargar, Y., Rahimi Pordanjani, T., Mohamadzade Ebrahimi, A., & Noruzi, Z. (2013). A Study of Simple and Multiple Relationships between Morningness and Sleep Quality among Students with Addiction Potential in Shahid Chamran University. Jundishapur Scientific Medical Journal, 12(4). [Link]
Zhang, S., Lin, X., Liu, J., Pan, Y., Zeng, X., & Chen, F., et al. (2020). Prevalence of childhood trauma measured by the short form of the Childhood Trauma Questionnaire in people with substance use disorder: A meta-analysis. Psychiatry Research, 294, 113524. [DOI:10.1016/j.psychres.2020.113524] [PMID]
Type of Study: Original Research Article |
Subject:
Substance abuse and dependence
Received: 2025/01/15 | Accepted: 2025/03/7 | Published: 2025/04/1
Received: 2025/01/15 | Accepted: 2025/03/7 | Published: 2025/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |