Volume 13, Issue 2 (Spring 2025)
PCP 2025, 13(2): 113-128 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Farimanian S, Bayazi M H. Effectiveness of Cognitive-behavioral Therapy on the Psychological Security and Self-care Behaviors among Diabetes Patients. PCP 2025; 13 (2) :113-128
URL: http://jpcp.uswr.ac.ir/article-1-982-en.html
URL: http://jpcp.uswr.ac.ir/article-1-982-en.html
1- Department of Psychology, Faculty of Psychology, Torbat-e-Jam Branch, Islamic Azad University, Torbat-e-Jam, Iran.
2- Department of Psychology, Faculty of Psychology, Torbat-e-Jam Branch, Islamic Azad University, Torbat-e-Jam, Iran. ,bayazi123@gmail.com
2- Department of Psychology, Faculty of Psychology, Torbat-e-Jam Branch, Islamic Azad University, Torbat-e-Jam, Iran. ,
Keywords: Group cognitive-behavioral therapy (GCBT), Psychological security (PS), Self-care, Patients with type II diabetes (T2DM)
Full-Text [PDF 687 kb]
(491 Downloads)
| Abstract (HTML) (1808 Views)
Full-Text: (442 Views)
Introduction
Old age is an important part of human life and can be considered the final stage of human development and growth. Older people are more exposed to incurable diseases than other groups because their immune system is weakened, and they do not have the physical and mental strength to deal with diseases. One of the diseases observed in the older population is diabetes (Frey et al., 2018). Diabetes is considered a lifestyle and metabolic disorder, the management of which is regarded as one of the necessities of the psychological science of this century. The number of diabetic patients from 200 million in 2000 will reach 592 million in 2035, with the highest prevalence in developing countries, including the Middle East (World Health Organization [WHO], 2000). The spread of the prevalence of type II diabetes mellitus (T2DM) (90% of diabetic patients) has made the disease an epidemic issue (Yazdi et al., 2020). T2DM is caused by the inability of the body to produce or use insulin (Zhang et al., 2010) and is related to aging, obesity, glucose metabolism disorder, and physical inactivity. Usually, T2DM is associated with many long-term complications (Oyewole et al., 2023). T2DM is one of the chronic diseases that increases the possibility of mental disorders due to physical problems. Therefore, psychological interventions can probably create positive changes in the psychological activity indicators. Despite the expenses spent for the prevention and control of diabetes, the number of people suffering from it increases every day, which seems to be a weak point for patients with T2DM.
On the other hand, despite having enough information about self-care (nutrition, injecting insulin, exercise, etc.), patients with T2DM cannot take proper care of themselves. Not taking care of yourself, like any behavior, can be affected by the way of thinking, and the way of teaching philosophy can be a good way to change thinking. During the last decades, the psychological aspects of diabetes have attracted the attention of many experts because diabetes is considered one of the most demanding chronic diseases in terms of emotional and behavioral aspects (Bryan et al., 2017). While patient motivation plays an essential role in the management of diabetes, people with poor psychological health lack enough motivation and emotional strength to manage their diabetes. Psychosocial adjustment is a factor and, at the same time, an important outcome of diabetes care, both in terms of quality of life (QoL) and therapeutic effects (Snoek & Skinner, 2006). Social and psychological factors affect the QoL and often play a role in determining the outcome of dealing with a chronic disease, especially in the care of diabetes, which largely depends on the psychosocial factors of the person to manage this disease and achieve proper control.
Type 2 diabetes control involves implementing a multi-faceted self-care program that usually includes blood sugar measurement, diet, exercise, drug treatment, body weight control, and foot care. Such diabetes self-care activities (DSCA) may be laborious and often require fundamental lifestyle changes. So many patients with T2DM do not fully comply with medical and treatment recommendations despite knowing the complications of the disease, and as a result, the possibility of developing complications related to diabetes increases. Patients with T2DM face many physical problems and emotional disorders in the process of life. Therefore, emotional disturbances associated with the disease seem inevitable, and there is a likelihood of depression (Collins et al., 2008), anxiety (Li et al., 2008), stress, and depression (Krishna, 2018). This condition increases the blood sugar level of patients with T2DM and reduces effective DSCA (Morris, 2011).
One of the variables that seems to be effective in patients with T2DM is DSCA (Puig-Domingo et al., 2020). DSCA is a key concept in health promotion and includes decisions and activities that a person uses to adapt to a health problem or improve their health. DSCA refers to self-care activities, including taking medication appropriately, monitoring health fluctuations, and maintaining a healthy lifestyle (Forbes & While, 2009). One of the most important DSCA activities of patients with T2DM is to follow a healthy and balanced diet, follow up on drug treatments, monitor glucose levels to regulate diet and activity levels, and prescribe treatment (Jordan et al., 2010). DSCA is significant because diabetes is the sixth cause of death in the world and causes four million deaths in the world every year. Considering the effect of DSCA activities in determining blood sugar levels and the results of diabetes (Ricci-Cabello et al., 2014), the most critical factor behind the death of patients with T2DM can be considered as not performing DSCA activities (Christie et al., 2014). Designing and evaluating educational programs based on providing information, creating motivation, and teaching behavioral skills in the field of health-enhancing DSCA will increase patients’ adherence to DSCA and create a feeling of recovery and satisfaction with disease control (Tayefi et al., 2015; Saffariantoosi & Khaleghi, 2024).
Medication adherence in patients with T2DM in primary health clinics is poor, which causes concern as nonadherence can worsen the disease. However, changing the frailty index’s lifestyle, nutrition, physical activity, and cognitive training can reduce the complications. Research shows that T2DM increases the risk of cognitive impairment and depression, as well as increases the body’s metabolic compensation (Valenzuela et al., 2018) and reduces medication adherence. In addition, nonadherence to medical care in patients with T2DM is related to the hospitalization rate. Adherence to medical recommendations is associated with a significant reduction in hospitalization of patients and a tendency to visit less (Delevry et al., 2020). Continuous and extensive efforts in determining the current health standards, including focusing on physical and mental health and ending the continuous stress of the disease, are widely followed theoretically and empirically (Wise & Hersh, 2012), emphasizing the need to implement effective psychological interventions.
Along with medical treatments, it is necessary to control this disease and its related complications. In the meantime, one of the variables related to the existence that affects the function of older people and their satisfaction with life is the feeling of security (Montazerolhodjah et al., 2018). In this research, the researcher tries to measure the effect of GCBT training on PS variables in patients with T2DM. The occurrence of emotional, physical, and sexual injuries in childhood is one of the factors that can institutionalize a sense of insecurity and being at risk in the memory and unconsciousness of people.
Another variable that seems to be effective in patients with T2DM is psychological security (PS), which can also be called mental security or a sense of inner security (Wang et al., 2019). It is the smoothest platform for the growth of mental creativity and innovation (Xu et al., 2022; Zhang et al., 2010; Wang et al., 2019). PS is the feeling of satisfying one’s current needs (Maslow, 1942). The feeling of PS is considered the most effective way to encourage people to think and try to achieve growth and progress at different personal, family, professional, and social levels (Toobert & Glasgow, 1994; Kumar et al., 2024). This concept refers to an environment understood as “an impersonal and non-threatening environment.” Patients with T2DM suffer from depression, despair, and feelings of inferiority more than other people. Satisfying the need for security healthily and desirably throughout life can provide the basis for achieving other needs such as self-esteem, loving and being loved, and self-actualization. However, the effectiveness of a distinctive therapy depends on medication adherence. Medication adherence in patients with T2DM in primary health clinics is poor, which is a cause for concern because medication nonadherence can worsen the disease (Sun et al., 2023).
There are many treatments to adapt to the PS and DSCA of older patients with T2DM; one of these therapies is mindfulness. This approach places less emphasis on changing the content of thoughts and focuses more on changing attention, awareness, and communication with thoughts. It puts a lot of emphasis on accepting thoughts instead of changing them and emphasizes that we understand thoughts as thoughts, not as a reflection of reality. Another new treatment is self-management-based therapy. Also, there is acceptance and commitment therapy (ACT). Increasing psychological flexibility is considered the primary assumption of the mechanism of change in ACT and increasing mindfulness dimensions, which plays an essential role in the possible effects of the intervention. In this regard, Eilenberg et al. (2016) and Bonacquisti et al. (2017) declared that ACT is effective in treating anxiety and mood disorders.
Much evidence shows the effectiveness of group cognitive-behavioral therapy (GCBT) on PS, DSCA, and other health-related benefits (Samadzadeh et al., 2018). This therapy is based on the solid cooperation between the patient and the therapist. CBT-based interventions allow the patient to respond wisely instead of an immediate and ill-considered response to things. Therefore, by providing a platform for deep attention to the experiences of the disease and accepting the emotions and suffering caused by it, it intervenes. For this reason, conscientious people have a higher ability in efficiency and problem-solving than others (Emanuel et al., 2010). Based on the research, as soon as the patients reach mental security, they can achieve good results in relative recovery from their illnesses and, as a result, get a better view of their QoL and future. This outcome is also true in older people. Previous research has shown that GCBT is effective for a variety of mental problems (e.g. psychological symptoms), physical conditions (e.g. irritable bowel syndrome and fatigue syndrome), behavioral problems (overweight and antisocial behaviors) (Nakao et al., 2021), motivating and accepting responsibility for DSCA (Toobert & Glasgow, 1994), and reducing anxiety and depression (Beltman et al., 2012). A pilot study showed that GCBT effectively improves and increases DSCA, such as blood sugar control in adolescents with T2DM (Serlachius et al., 2016). ecause previous research on PS and DSCA has primarily focused on the workplace (Probst, 2002; Hu et al., 2018), the PS and DSCA of older patients with T2DM have not received sufficient attention. Tarkhan (2011) has studied the effectiveness of short-term interpersonal group therapy on the psychological well-being and QoL of spouses of people with an addiction. Nakao et al., (2021) found the effectiveness of GCBT on mental and physical variables (such as PS and psychological distress) related to patients with T2DM. Abbas et al. (2023) declared that GCBT has a significant reduction in diabetes distress, psychological distress, PS, depressive symptoms, and health anxiety and has a significant enhancement in treatment adherence, QoL, and physical activity schedule of the patients with T2DM. Pan et al. (2023) supported the effectiveness of an internet-based GCBT program for students with psychological distress. Skoglund et al. (2024) declared that GCBT decreases statistically significantly in people with comorbid PS. GCBT is short and limited in time, but it tries to help clients develop independent self-help skills. In addition, the GCBT approach relies on questioning and discovery combined with strategy and not on convincing. In this approach, which is based on inductive methods, the patient learns to look at thoughts and beliefs as hypotheses that must be tested. Finally, this approach is educational in that GCBT techniques are considered skills that must be learned through practice and entered into the patient’s environment through homework (Welschen et al., 2014). Based on GCBT intervention, skills to evaluate irrational and negative thinking are learned, and a range of standard cognitive-behavioral coping skills are taught, which is a guide for flexibility in choosing appropriate strategies. It reduces psychological symptoms (Serlachius et al., 2016). In a pilot study, it was shown that GCBT is effective in improving and increasing PS in adolescents (Nakao et al., 2021).
Since the diagnosis of diabetes has important effects on patients’ psychological and social performance, patients must devote a lot of attention and energy to self-management of the disease (Dineen-Griffin et al., 2019). The success of patients in integrating a self-management and DSCA approach with their existing lifestyle depends on the extent to which diabetes-specific events interact with the patient’s existing beliefs, thoughts, feelings, and behaviors. Diabetes is often associated with mental problems and disorders, and unfortunately, these problems reduce the patient’s ability to self-manage the disease and perform the DSCA. Decreasing the ability of patients to control diabetes aggravates their psychological problems and causes patients to get caught in a vicious cycle. These problems may even become more severe with the psychological reactions of patients that negatively impact the experience of diabetes symptoms. Identifying effective treatments to increase PS and the DSCA to be persistent for treatment is very necessary for patients with T2DM.
In general, PS and DSCA are among the basic needs of patients with T2DM, which can facilitate their interaction with family and social environment. Although previous research has emphasized the role and importance of PS and DSCA in learning and problem-causing behaviors of diabetic patients (Nakao et al., 2021; Abbas et al., 2023; Pan et al., 2023), the related variables and explaining the effectiveness of GCBT on the PS and DSCA of patients with T2DM, have not been considered. In addition, according to the background review, few researchers have investigated the effectiveness of GCBT on PS and the DSCA. Therefore, while completing this gap, this research can provide counselors, clinical psychologists, and therapists with a suitable solution for appropriate psychological interventions in patients to expand theoretical knowledge in diabetes and the effectiveness of interventions on important variables in this field. Also, the results of this study will develop knowledge of the efficacy of GCBT on PS and the DSCA. This treatment can effectively identify rational and hopeful thought patterns and increase the perception of well-being. As a result, it will positively affect constructive PS and the DSCA. Improving PS and DSCA is one of the most important steps to help patients control and manage their disease. Therefore, this research aimed to answer whether group GCBT effectively treats PS and the DSCA in people with T2DM.
Materials and Methods
Participants and design
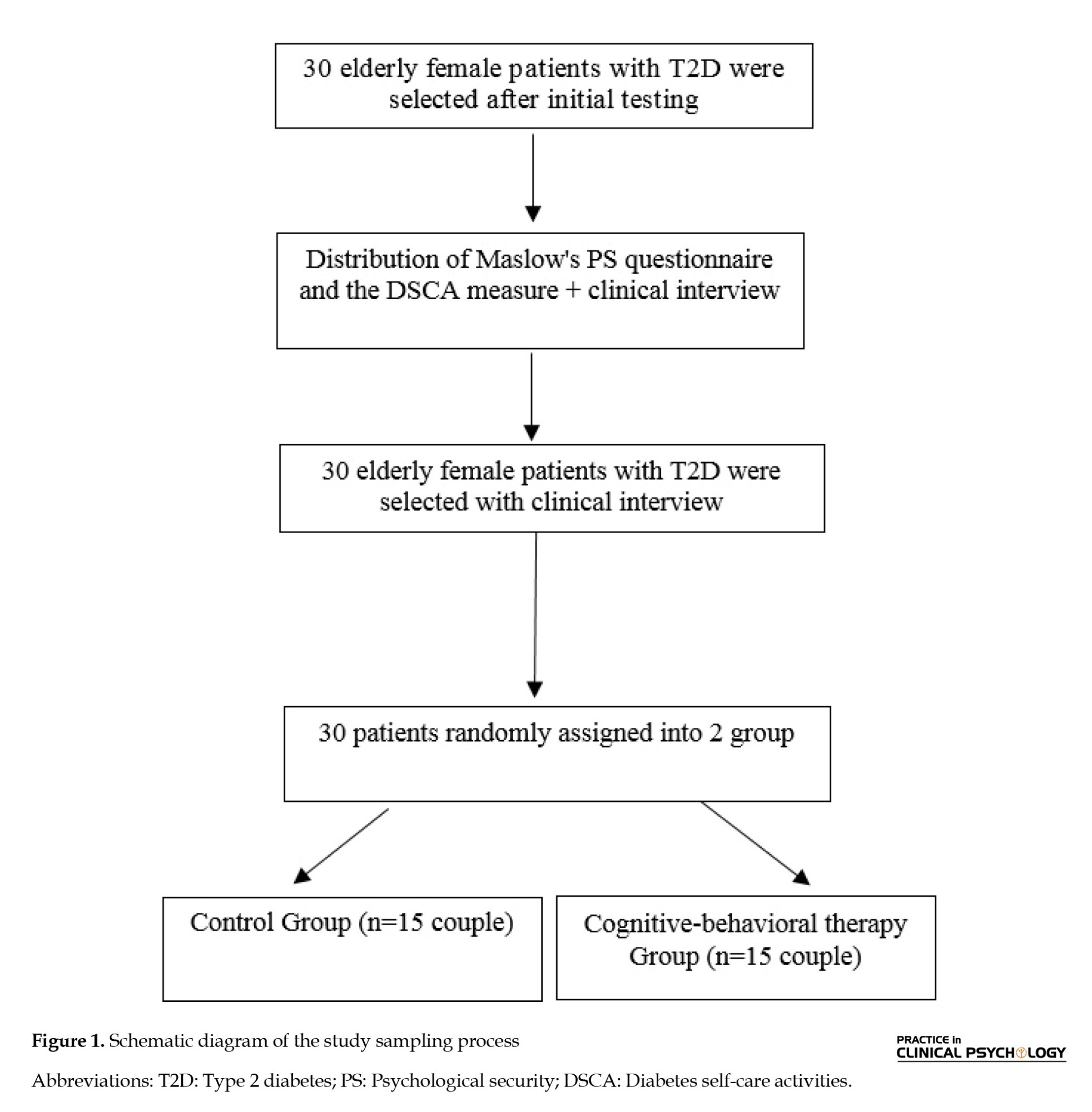
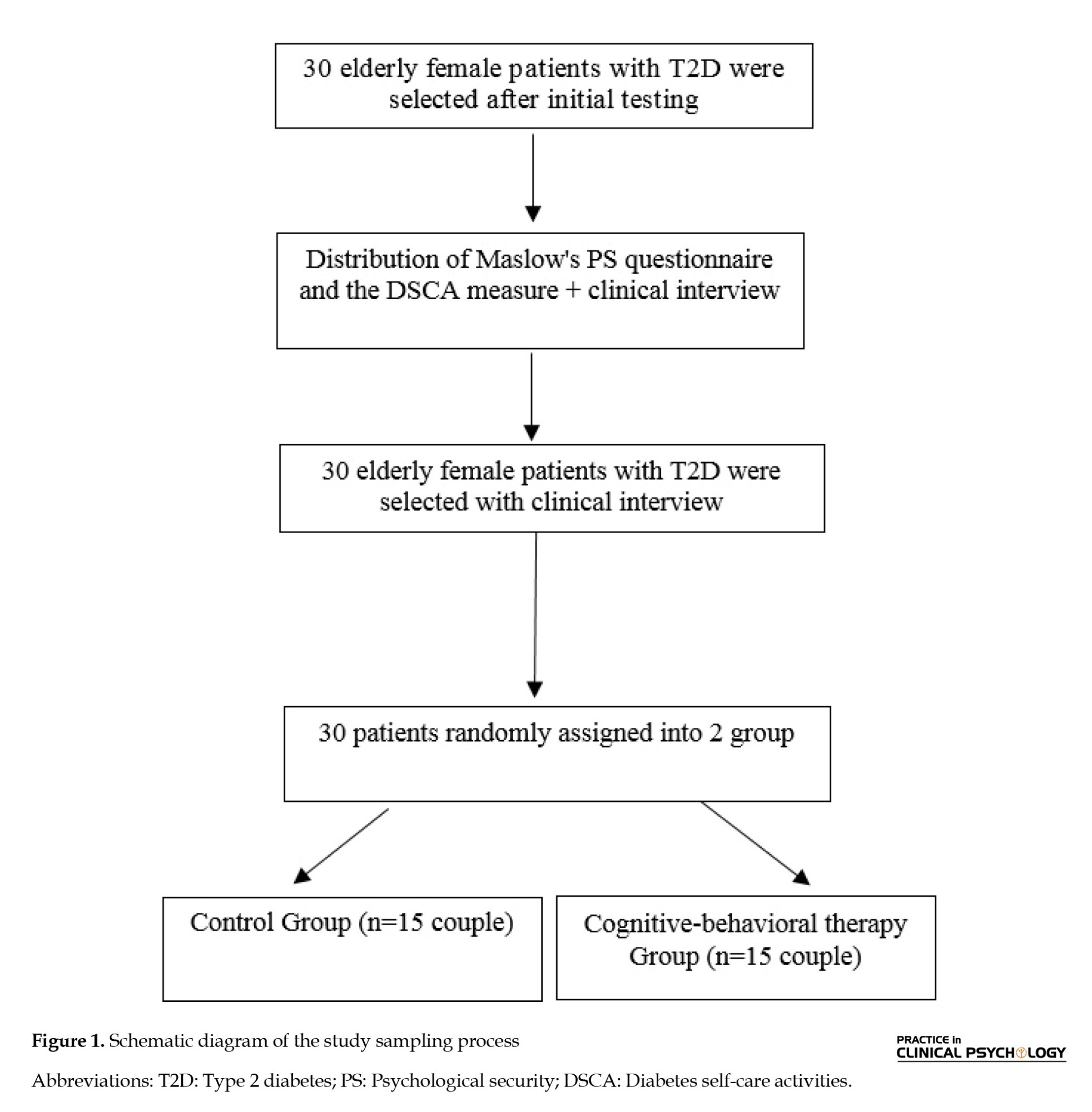
This quasi-experimental research explored the effectiveness of GCBT on the PS and DSCA in patients with T2DM. The study was conducted with a pre-test -post-test design and a control group of 30 older female diabetic patients during the summer of 2023. The patients were randomly assigned into two groups (test and control) of 15 subjects (Figure 1).
The test group, along with regular medical care, received GCBT for 8 weekly sessions of 1.5 hours. The control group received only regular medical care. Due to the research limitations, providing a placebo or alternative intervention in the control group was impossible. Still, in the end, the intervention related to the test group was also implemented in the control group. The intervention was a special protocol that had 8 sessions. The aim was to investigate the effectiveness of a short-term and cost-effective intervention according to the research objectives and the studied variables.
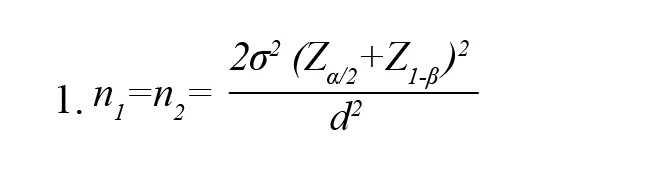
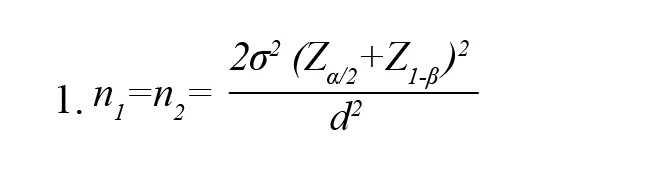
The Equation 1 was used for sampling (Sarabadani et al., 2023). According to the values of δ= 3.52 (common SD of PS and the DSCA scores), d=2.81 (the pre-test mean score differences of PS and the DSCA in the test and control groups), statistical power=0.9, and error level or α equal to 0.05, the sample size was equal to 13 people for each group. With the possibility of a sample drop in the groups, the sample size of 15 people was considered for each group.
To comply with ethical considerations, written consent was obtained from the subjects for informed participation in the research. Also, emphasis was placed on the principle of confidentiality of the participants’ information and the implementation of this training for the control group after the end of the experiment. The participants were initially numbered from 1 to 30. After matching based on demographic characteristics such as age, gender, and history of disease, they were randomly assigned to the test and control groups in odd and even pairs.
Inclusion and exclusion criteria
The inclusion criteria were as follows: A specialist doctor’s diagnosis of T2DM, having at least a diploma, being 55 years old or older, and at least 6 months had passed since the onset of the disease.
The exclusion criteria were as follows: Absence of more than two sessions, suffering from another chronic physical and mental illness, suffering from addiction or being about to divorce, having diabetes complications, and having any medical problems that prevent self-care behaviors (such as exercise and regular physical activity).
Study procedures
Demographic questionnaire
The demographic questionnaire used in this study consisted of two parts, including demographic characteristics (11 questions) and two PS and DSCA questionnaires. The first section was used to evaluate the personal information of the participants, including their birth date and educational level. Before and after the GCBT intervention, both groups were assessed in terms of PS and DSCA.
Maslow’s psychosocial security scale
Maslow, (1942) created the PS questionnaire to measure different aspects of PS. It has 62-question self-report scales and 15 subscales. Its scoring is done with “yes” and “no” options. Correct answers are given a score of 0, and incorrect answers are provided 1. Achieving a high score (62 points) indicates a person’s high PS, and a low score indicates low PS. Bowen et al. (2010) reported that Cronbach’s α coefficient was 0.92. Also, the reliability of this questionnaire was obtained through the Cronbach α of 0.74.
The summary of DSCA measure
The 12-item summary of DSCA measure was introduced by Toobert & Glasgow, (1994). A full score is 7; if it is not done on any day of the week, a score of 0 is awarded. To determine the level of desirability of the self-care situation, in addition to the average score scale, the range of scores obtained was from 0 to 70. It was divided into three parts: undesirable (0-23), semi-desirable (24-47), and desirable (47-70). An overall compliance score is obtained by adding up the scores of each question. Kuwahara et al. (2004) obtained the reliability of The summary DSCA questionnaire through the Cronbach α of 0.76, and its content validity was satisfactory. To determine the diagnostic validity, the questionnaire was administered to 40 diabetic patients and 40 healthy people, and the independent t test showed that the difference between the two groups is significant and the test has a suitable diagnostic validity. The questionnaire was conducted in 2 states with a time interval of one week to obtain retest reliability, and the findings indicated that the questionnaire has a relatively high and suitable retest. Also, the validation studies showed a correlation higher than 0.89 between questions and 4 areas (Ryff et al., 2002).
Research method
The participants (30 elderly female patients with T2MD) were initially numbered from 1 to 30. After matching based on demographic characteristics such as age, gender, and history of disease, they were randomly assigned to the test (intervention) and the control groups. Figure 1 shows no missing data during the implementation phase; all subjects completed the experimental process. Then, a pre-test was performed (PS and DSCA measures). The method of conducting the research was that after the necessary coordination with the officials of the Fariman Health Diabetes Center, written consent was obtained from the sample to participate in the study after stating the purpose of the research. The questionnaires were mainly completed by the participants and, in some cases, by the patient with the help of her companion. Based on the clinical handbook of couple therapy, the test group received GCBT for 8 weekly sessions of 2 hours with GCBT (Baucom et al., 2015). The control group was placed on the waiting list and received only regular medical care during this period. A senior clinical expert held the sessions. The GCBT program was performed for three months (August-September 2023). All patients replied to the scales before (pre-test ) and immediately after the intervention (post-test).
GCBT intervention plan
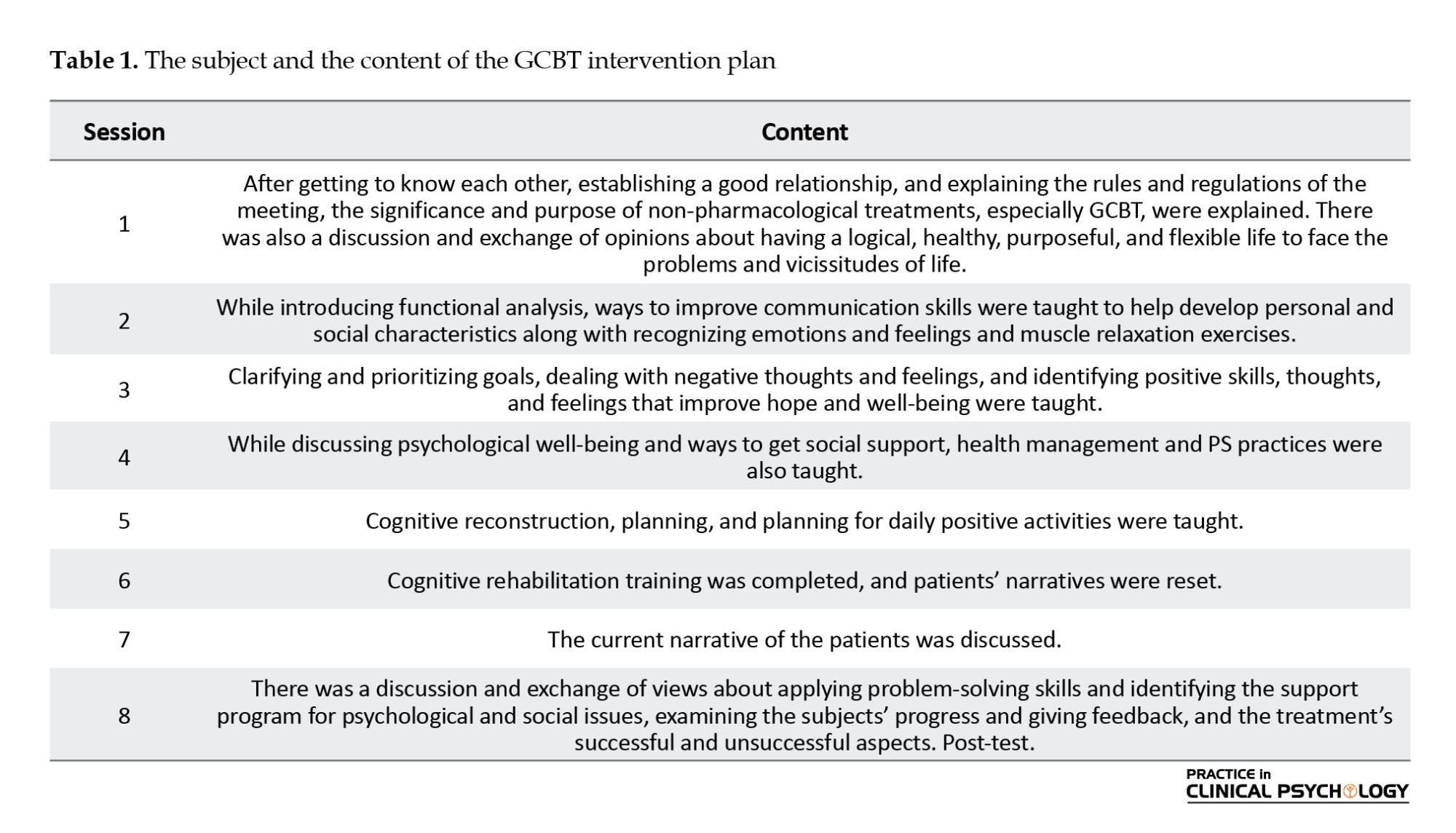
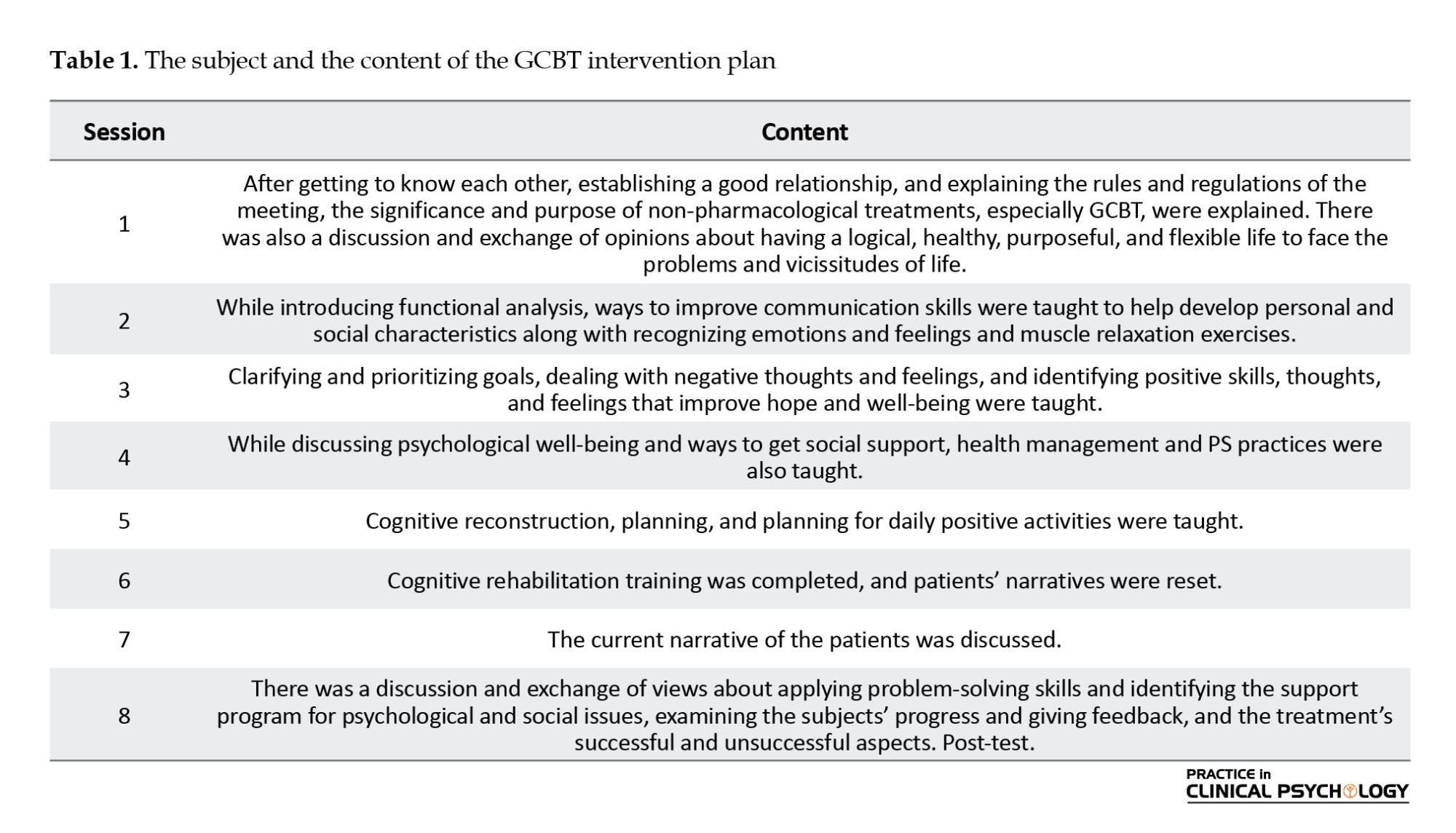
The patient’s PS and DSCA programs (the amount of time for sports activities, blood sugar monitoring, diet compliance, and foot care) were announced through a written self-report by the patient’s relatives who lived with or cared for her (feminine). It should be noted that the researcher completed the questionnaires in the form of a structured interview with the participants in 15-20 minutes. The details of the intervention in the test group are described in Table 1.
Data analysis
The data were described by descriptive statistics (Mean±SD) and analyzed by inferential statistics (analysis of covariance analysis). SPSS software, version 24 used for the statistical analysis.
Results
Descriptive findings
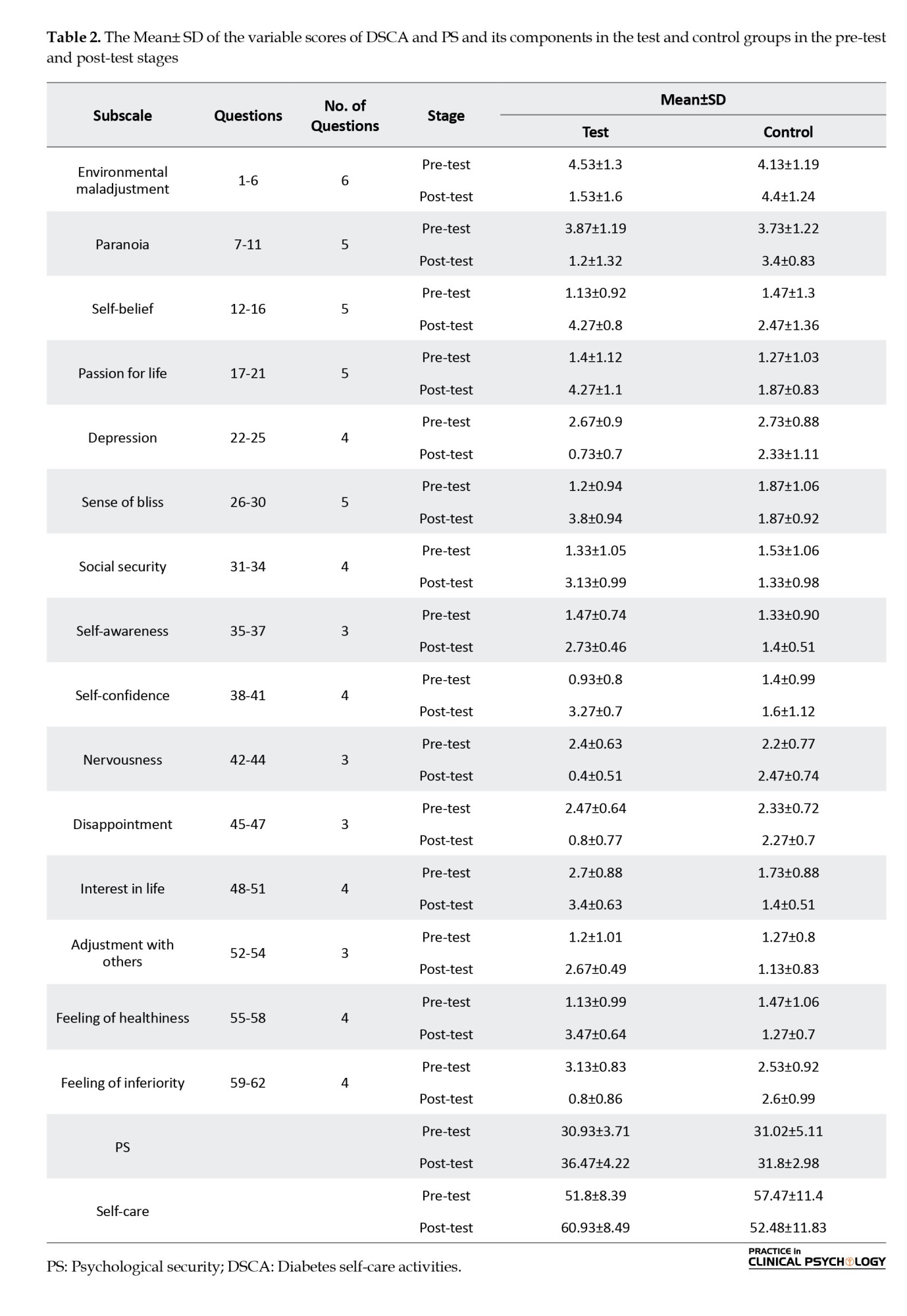
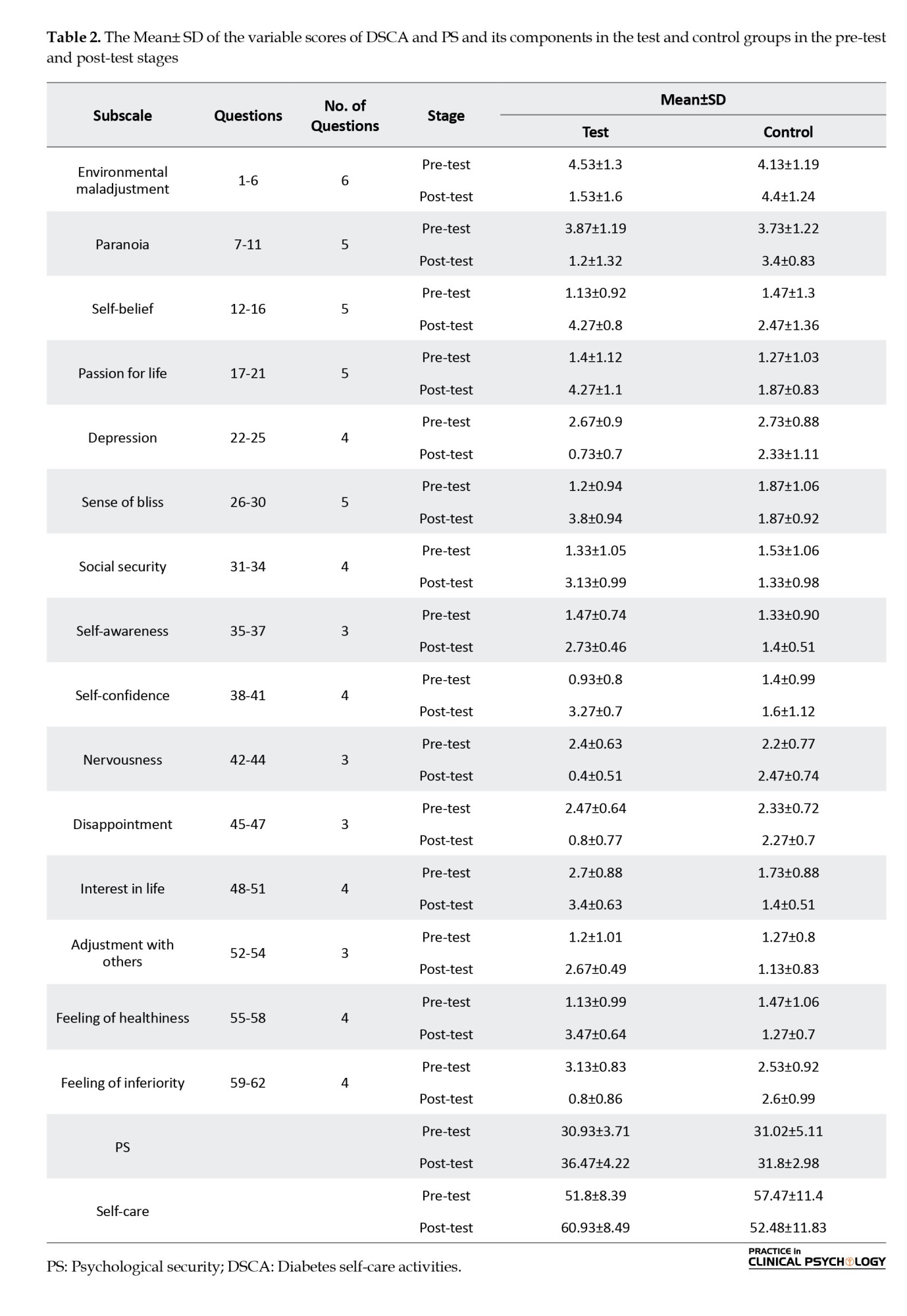
The participants of this research were 30 older female patients with T2DM. The Mean±SD of the age of the samples was 58.14±23.47 years. They were in the age range of 55 to 67 years. The highest frequency is related to the age of 55-59, and the lowest frequency is related to the age of 59-67. The subjects were randomly divided into two equal groups; these two groups were matched in terms of age. Table 2 shows the variables’ Mean±SD in the pre-test and post-test stages. As seen, the mean of the test group increased compared to the control group in PS.
Analysis of covariance
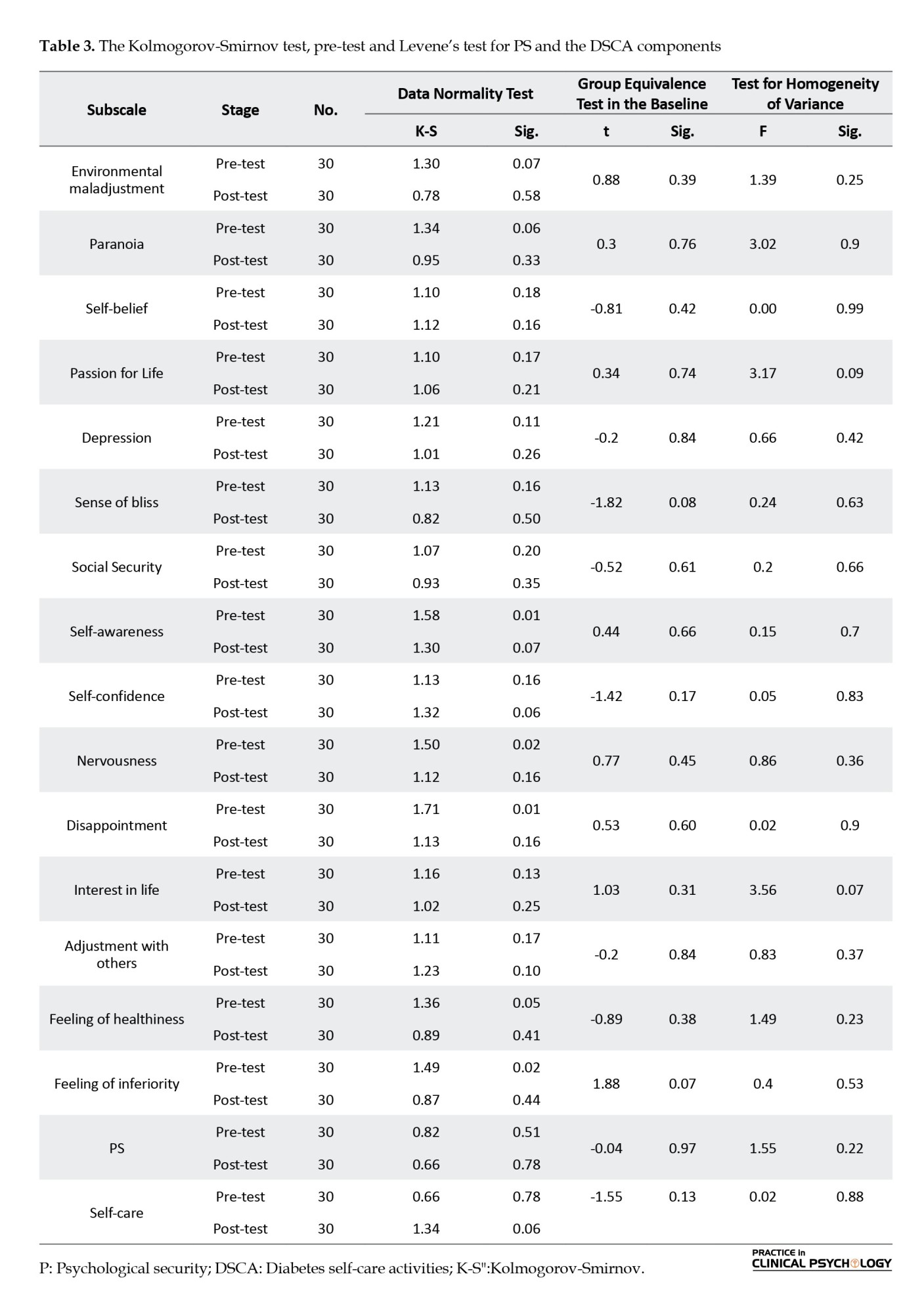
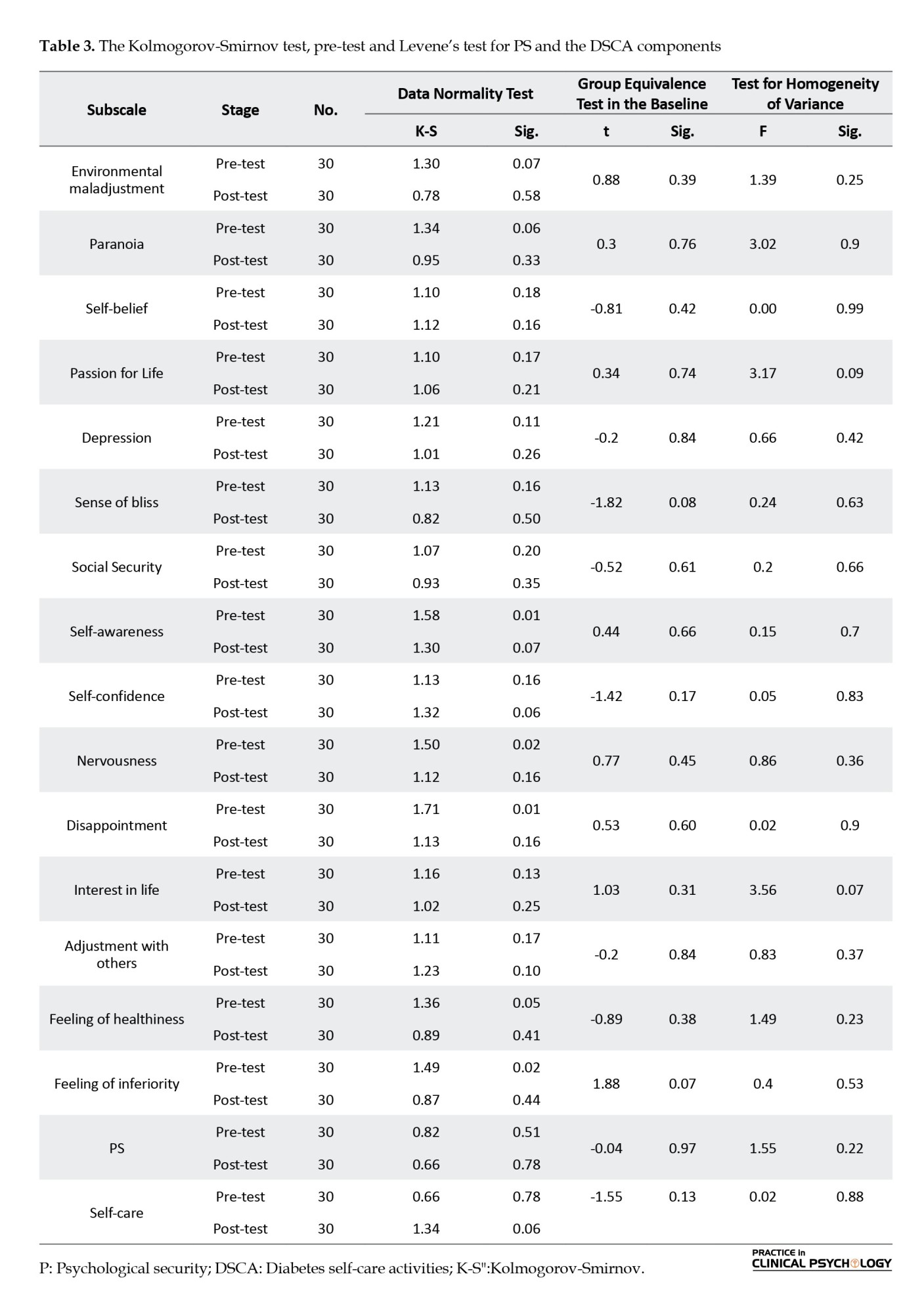
The presuppositions of covariance analysis were evaluated before analyzing the data by covariance analysis. The Kolmogorov-Smirnov (K-S) test results on PS variables were not significant for any of the variables, indicating that the assumption of the data normality test is established at a level of <0.05 (Table 2).
Also, Levene’s test for equality of variances results were not significant, indicating that the individual group covariance matrices are equal (homogeneous across groups) and that the assumption of equal variance is valid (Table 2). According to the test for homogeneity of variance, the test and control groups are not significant for the PS and the DSCA components (Table 2). Therefore, the variances of the test and the control groups are equal.
The results of the test of homogeneity of regression slopes of the research variables have shown that the F value of the interaction for the sameness of the regression line slope for the PS (F=3.72) and the DSCA (F=2.88) variables are at a significant level of 0.142 and 0.063, respectively, which are insignificant. In other words, the homogeneity of regression slopes is accepted.
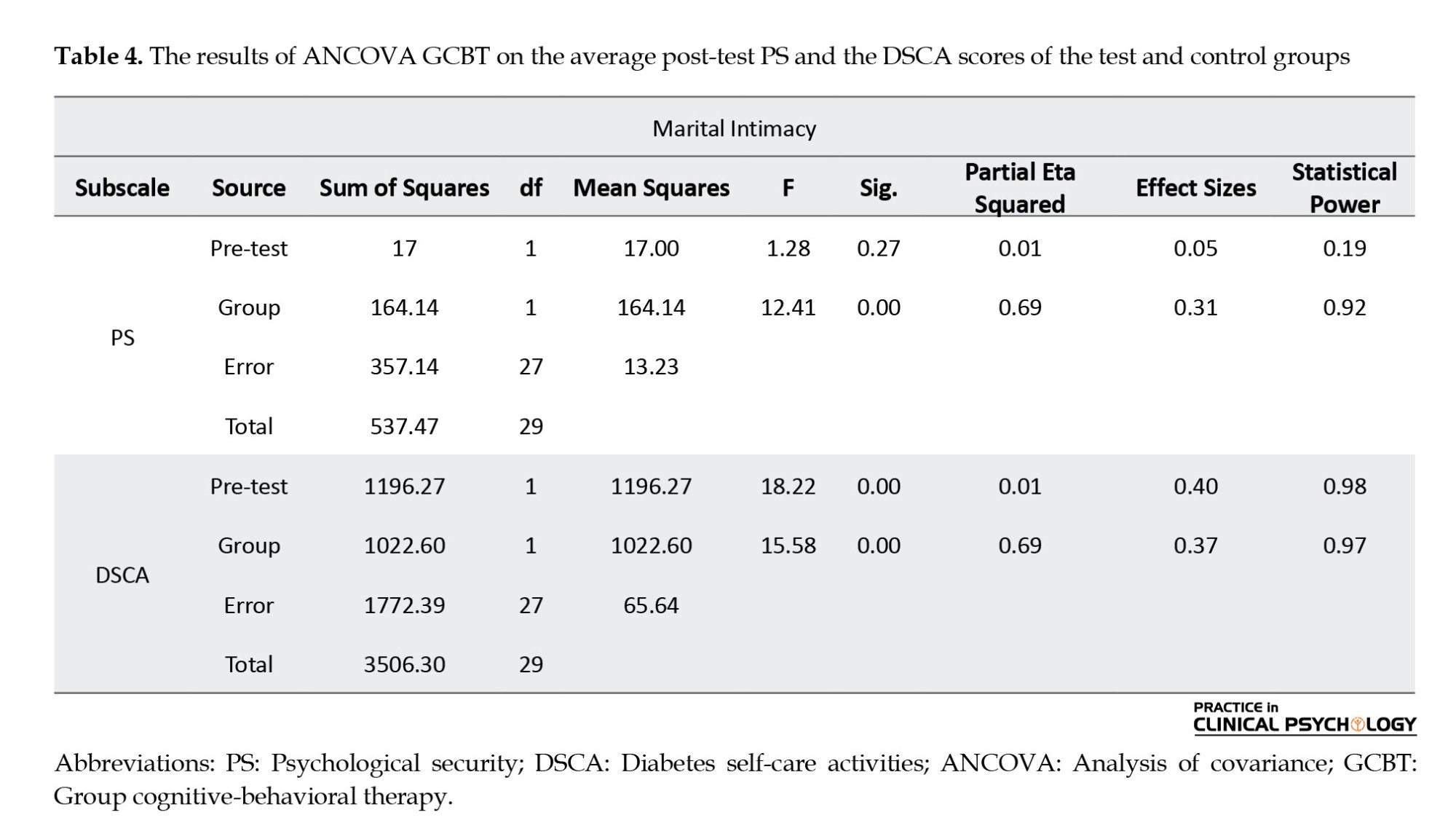
Therefore, to investigate the effect of GCBT on increasing the PS and the DSCA of patients with T2DM, the ANCOVA test was used with the control of the pre-test effect (Table 3). As can be seen, the independent variable was effective on the dependent variables. In other words, the test and control groups significantly differ in the PS and the DSCA variables (P<0.0001). Also, by controlling the pre-test effect and calculating according to the F coefficient, a significant difference is seen between the adjusted averages of PS and the DSCA scores according to group membership “test and control” in the post-test stage (P<0.0001). Therefore, the GCBT method had a greater effect on the PS and DSCA of patients with T2DM in the test group participants.
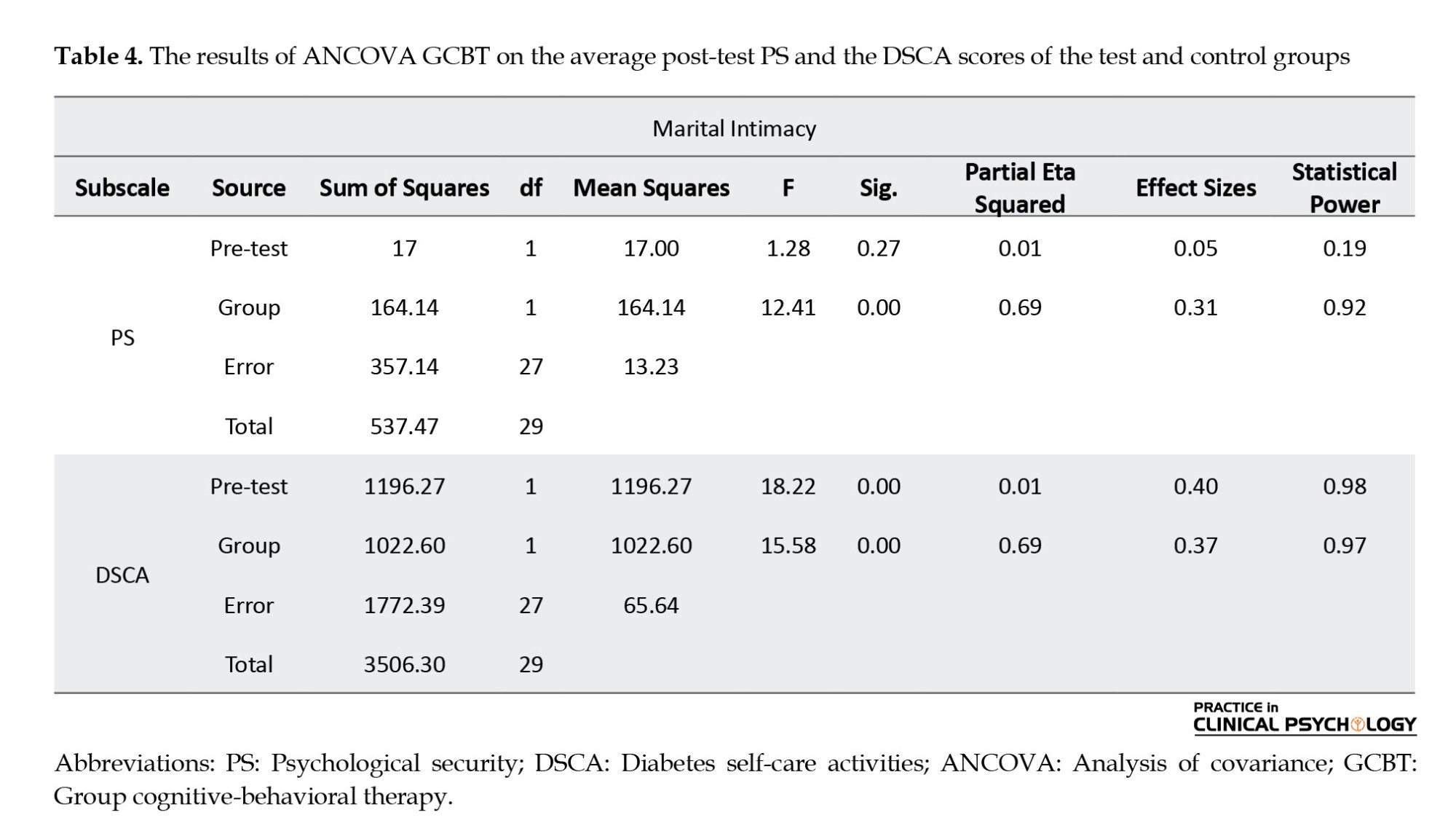
The effect size of “practical significance” was 0.31; that is, 31% of the total variance changes or individual differences in the PS and the DSCA of patients with T2DM were caused by the effect of GCBT. The statistical power for the PS and DSCA were 0.92 and 0.97, respectively, indicating the sampling volume’s adequacy. According to Table 4, There is a significant difference between the level of PS (P=0.001, F=12.41) and the DSCA (P=0.001, F=15.58) of the subjects in the test and the control groups. With 95% certainty, the null hypothesis is rejected, and the main hypothesis is confirmed. We conclude that GCBT effectively increases the PS and the DSCA of patients with T2DM.
To investigate the effect of GCBT on the components of PS and the DSCA, we used multivariate covariance analysis, where the dependent variable includes the DSCA and the components of PS: Environmental maladjustment, paranoia, self-belief, passion for life, depression, sense of bliss, social security, self-awareness, self-confidence, nervousness, disappointment, interest in life, adjustment with others, feeling of healthiness, and feeling of inferiority.
Table 4 shows the difference between the post-test of the three groups in the DSCA and PS components, indicating a significant difference between the test and the control groups. GCBT has increased the scores of self-belief, passion for life, sense of bliss, social security, self-awareness, self-confidence, interest in life, adjustment with others, and feeling of healthiness. Also, the scores of environmental maladjustments, paranoia, depression, nervousness, disappointment, and feeling of inferiority decreased in the post-test, and all the components of PS are significant (P<0.05). So, there is a significant difference between the DSCA and PS components scores in the test and control groups in the post-test. We conclude that GCBT affects the DSCA and the PS components of patients with T2DM.
Discussion
This quasi-experimental research aimed to explore the effectiveness of GCBT on the PS and DSCA in patients with T2DM. It was conducted with a pre-test -post-test design and a control group on 30 elderly female diabetic patients during the summer of 2023. The results of ANCOVA indicated that GCBT significantly increased the PS and the DSCA in patients with T2DM (P≤0.05). GCBT was effective in improving the PS and the DSCA of the patients with T2DM.
According to the results, GCBT was effective in improving and enhancing the PS of patients with T2DM (P<0.001). GCBT intervention can be introduced as a fruitful psychological intervention. It can increase psychological well-being indicators, QoL, and greater adherence to treatment recommendations. The increase in this way will help to prevent the complications of diabetes and will be an effective step towards increasing the level of mental and physical health of patients with T2DM. Previous research such as Haneda et al. (2016), Welschen (2014), Serlachius et al., (2016), Puig-Domingo et al., (2020), Delshad Noghabi et al. (2021), Nakao et al., (2021), Farimanian and Bayazi (2024) and Ramezani Rezaabad et al. (2024) have confirmed the effectiveness of GCBT on PS in their research results. Research has shown that GCBT increases PS, reduces depression symptoms, and a relative decrease in symptoms of anxiety in women with T2DM (Basiri et al., 2023). In other words, the decline in the symptoms of depression and anxiety in people with T2DM is associated with improving the PS. The results of other researchers suggest that PS in people with T2DM can be influenced by positive psychological characteristics such as life expectancy and efficient attitudes (Xu et al., 2022). Nurses can improve their PS by improving efficient and hopeful attitudes in patients with T2DM. Nurses can also help patients with T2DM, who often have cognitive errors and irrational and destructive beliefs in their lives, by informing patients of their irrational documents and beliefs. Using their knowledge and experience to help modify these misconceptions and promote patient information literacy to create rational and efficient beliefs. As a result, patients, using experiences and enhancing health information, change the misconceptions and documents that have caused anxiety and depression and thus reduce their PS.
By examining the content of the materials presented in the psychological safety management training sessions in this research, it can be assumed that using behavioral strategies and strategies such as calming and creating a sense of calm in the affected person have also reduced his psychological symptoms and distress. On the other hand, cognitive strategies such as problem-solving, recognizing cognitive errors, fighting against negative thoughts, using logical thinking, and positive self-talk may change the attitudes and cognitions of patients so that they accept their illness and rationally face its psychological consequences. By applying the skills taught, they took steps to improve themselves and control the disease more effectively. Also, GCBT training sessions familiarize patients with T2DM with how stress affects them and teach them to look at stressful situations as solvable problems. In addition, different coping methods and their effective management are shown to patients with T2DM. This makes them feel that they have more control over their surroundings, evaluate them as less threatening when dealing with such situations, and when faced with said situations, having more efficient coping skills, they can solve them more effectively and be safe from the negative psychological effects caused by ineffective coping with stressful situations. Therefore, they can have better control over the anxieties caused by the disease.
Anxiety caused by suffering from a chronic and permanent disease such as diabetes can lead to many psychological complications. Examples include depression, insomnia, anxiety, physical symptoms, and social dysfunction. Anxiety in its chronic state causes the erosion of the physical and mental reserves of the affected person by creating a state of permanent alertness in the body. This condition plays an effective role by using the mechanism of the learned helplessness effect of the diabetic person on non-compliance with the treatment. This helplessness happens because a person does not accept his diabetes in the early stages of diagnosis, and the stress caused by it due to the occurrence of psychological complications of the disease, which was mentioned, is placed between the stage of denial and acceptance of the disease. This state causes the observance of treatment points in the stage of feeling acceptance and non-observance in the stage of illness. Thus, the patients do not achieve regular control of their blood sugar, and they think it is impossible to control their blood sugar in both cases of following and not following the treatment. Therefore, these issues can be better overcome by teaching destructive thoughts to stop self-deception and skills to deal with disappointment, failure, and unfairness syndrome in meetings.
Also, GCBT effectively improved and encouraged the DSCA of patients with T2DM (P<0.001). These findings are in line with Christie et al., (2014), Serlachius et al., (2016), Puig-Domingo et al., (2020), Shegarf Nakhaei et al. (2021), and Alahyari et al. (2022). Research has shown that GCBT increases SCB, reduces depression symptoms, and has a relative decrease in symptoms of anxiety in women with T2DM. In other words, the decline in the symptoms of depression and anxiety in people with T2DM is associated with improving the DSCA (Bădescu et al., 2016). The results of some studies have shown that having sufficient motivation and information in women with vaginitis fertility will positively affect DSCA and disease recovery (Xu et al., 2022). The results of other researchers suggest that self-care behaviors in people with T2DM can be influenced by positive psychological characteristics such as life expectancy and efficient attitudes. Nurses can improve their self-care by improving efficient and hopeful attitudes in patients. Nurses can also help patients with T2DM, who often have cognitive errors and irrational and destructive beliefs in their lives, by informing patients of their irrational documents and beliefs. Using their knowledge and experience to help modify these misconceptions and promote patient information literacy to create rational and efficient beliefs. As a result, patients, using experiences and enhancing health-health information, change the misconceptions and documents that have caused anxiety and depression and thus reduce their DSCA.
One of the reasons for the effectiveness of GCBT in increasing the PS and the DSCA of patients with T2DM is that the quality of patient care skills results from one’s own beliefs, thoughts, behavior, and deeds and relates to one’s decisions and performance. GCBT, as a psychotherapeutic method, alters the destructive patterns that are effective on patients’ behavior and emotions (Hofmann et al., 2012). Nurses can emphasize the importance of acquiring cognitive information, feeling efficient, skills, and using these skills by providing GCBT training. Also, during the training, people learn fruitful behavioral methods in addition to working on negative thinking. People affected by these tutorials will find the ability to correct automatic thoughts and evaluate their evidence and the documents needed to approve and disapprove those.
Conclusion
The implementation of GCBT has led to improving PS and the DSCA in patients with T2DM. According to the obtained results, the effort to change the attitudes and negative beliefs in GCBT by patients with T2DM has led to the improvement of the psychological condition of diabetic patients. In this treatment, the attitude and mental perception of patients about their disease and its symptoms have been changed, and it can be used in psychological clinics and educational workshops to increase adherence to the treatment, the perception of the disease, and the QoL of patients with T2DM.
Recommendations
It is suggested to take help from this treatment method to increase the learning of correct thinking and judgment skills about diabetes and to deal with unrealistic thoughts about this disease. Therefore, counselors and therapists can use this method to improve the PS of patients with T2DM. In addition, it is recommended that planners design programs based on this research to improve the PS of patients with T2DM.
Implications for family therapy/practice
Clinical counselors and therapists of diabetes centers and clinics can use the GCBT approach in their therapy groups and training classes to improve the basic PS, not to be discouraged, and to continue the treatment and, as a result, increase the physical health of patients with T2DM.
Research limitations
Because this manuscript was extracted from the thesis and involved financial and time limitations for the implementation of the thesis, it was not possible to carry out a follow-up. The reason for choosing female patients was the limitation in sampling men, considering that this research was related to a student’s thesis. Also, it was impossible to increase the sample due to the limitations of the thesis or this research. However, it is mentioned in the limitations section, and it is suggested that the sample size be increased in other future research studies. Another limitation of this research was the potential biases associated with self-reported data. In our application to clinical intervention, we examined the effects of participant demographics on response bias before and after participation, and bias is lower in the Post-test than in the Pre-test. Any shift in metric from before to after an intervention is caused by the intervention itself and may lead to underestimates of program effects.
Direction for future research and recommendations
It is hoped that the results of this research can be a basis for further study in the PS of patients to help improve and treat patients with T2DM as much as possible. This research is suggested to be repeated with larger and diverse samples, long-term follow-ups, and studies to investigate these interventions’ mediating factors and variables. It is also recommended that experts design a special PS program for patients with T2DM, and the official integration of this training in diabetes treatment-care programs should be considered by experts and institutions active in this field.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Torbat-e-Jam Branch, the Islamic Azad University, Torbat-e-Jam, Iran (Code: IR.IAU.TJ.REC.1402.093).The study was performed in accordance with relevant guidelines and regulations.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization and supervision: Sima Farimanian and Mohammad Hossein Bayazi; Methodology: Mohammad Hossein Bayazi; Investigation and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers must thank the patients and those who helped them conduct this research.
References
Old age is an important part of human life and can be considered the final stage of human development and growth. Older people are more exposed to incurable diseases than other groups because their immune system is weakened, and they do not have the physical and mental strength to deal with diseases. One of the diseases observed in the older population is diabetes (Frey et al., 2018). Diabetes is considered a lifestyle and metabolic disorder, the management of which is regarded as one of the necessities of the psychological science of this century. The number of diabetic patients from 200 million in 2000 will reach 592 million in 2035, with the highest prevalence in developing countries, including the Middle East (World Health Organization [WHO], 2000). The spread of the prevalence of type II diabetes mellitus (T2DM) (90% of diabetic patients) has made the disease an epidemic issue (Yazdi et al., 2020). T2DM is caused by the inability of the body to produce or use insulin (Zhang et al., 2010) and is related to aging, obesity, glucose metabolism disorder, and physical inactivity. Usually, T2DM is associated with many long-term complications (Oyewole et al., 2023). T2DM is one of the chronic diseases that increases the possibility of mental disorders due to physical problems. Therefore, psychological interventions can probably create positive changes in the psychological activity indicators. Despite the expenses spent for the prevention and control of diabetes, the number of people suffering from it increases every day, which seems to be a weak point for patients with T2DM.
On the other hand, despite having enough information about self-care (nutrition, injecting insulin, exercise, etc.), patients with T2DM cannot take proper care of themselves. Not taking care of yourself, like any behavior, can be affected by the way of thinking, and the way of teaching philosophy can be a good way to change thinking. During the last decades, the psychological aspects of diabetes have attracted the attention of many experts because diabetes is considered one of the most demanding chronic diseases in terms of emotional and behavioral aspects (Bryan et al., 2017). While patient motivation plays an essential role in the management of diabetes, people with poor psychological health lack enough motivation and emotional strength to manage their diabetes. Psychosocial adjustment is a factor and, at the same time, an important outcome of diabetes care, both in terms of quality of life (QoL) and therapeutic effects (Snoek & Skinner, 2006). Social and psychological factors affect the QoL and often play a role in determining the outcome of dealing with a chronic disease, especially in the care of diabetes, which largely depends on the psychosocial factors of the person to manage this disease and achieve proper control.
Type 2 diabetes control involves implementing a multi-faceted self-care program that usually includes blood sugar measurement, diet, exercise, drug treatment, body weight control, and foot care. Such diabetes self-care activities (DSCA) may be laborious and often require fundamental lifestyle changes. So many patients with T2DM do not fully comply with medical and treatment recommendations despite knowing the complications of the disease, and as a result, the possibility of developing complications related to diabetes increases. Patients with T2DM face many physical problems and emotional disorders in the process of life. Therefore, emotional disturbances associated with the disease seem inevitable, and there is a likelihood of depression (Collins et al., 2008), anxiety (Li et al., 2008), stress, and depression (Krishna, 2018). This condition increases the blood sugar level of patients with T2DM and reduces effective DSCA (Morris, 2011).
One of the variables that seems to be effective in patients with T2DM is DSCA (Puig-Domingo et al., 2020). DSCA is a key concept in health promotion and includes decisions and activities that a person uses to adapt to a health problem or improve their health. DSCA refers to self-care activities, including taking medication appropriately, monitoring health fluctuations, and maintaining a healthy lifestyle (Forbes & While, 2009). One of the most important DSCA activities of patients with T2DM is to follow a healthy and balanced diet, follow up on drug treatments, monitor glucose levels to regulate diet and activity levels, and prescribe treatment (Jordan et al., 2010). DSCA is significant because diabetes is the sixth cause of death in the world and causes four million deaths in the world every year. Considering the effect of DSCA activities in determining blood sugar levels and the results of diabetes (Ricci-Cabello et al., 2014), the most critical factor behind the death of patients with T2DM can be considered as not performing DSCA activities (Christie et al., 2014). Designing and evaluating educational programs based on providing information, creating motivation, and teaching behavioral skills in the field of health-enhancing DSCA will increase patients’ adherence to DSCA and create a feeling of recovery and satisfaction with disease control (Tayefi et al., 2015; Saffariantoosi & Khaleghi, 2024).
Medication adherence in patients with T2DM in primary health clinics is poor, which causes concern as nonadherence can worsen the disease. However, changing the frailty index’s lifestyle, nutrition, physical activity, and cognitive training can reduce the complications. Research shows that T2DM increases the risk of cognitive impairment and depression, as well as increases the body’s metabolic compensation (Valenzuela et al., 2018) and reduces medication adherence. In addition, nonadherence to medical care in patients with T2DM is related to the hospitalization rate. Adherence to medical recommendations is associated with a significant reduction in hospitalization of patients and a tendency to visit less (Delevry et al., 2020). Continuous and extensive efforts in determining the current health standards, including focusing on physical and mental health and ending the continuous stress of the disease, are widely followed theoretically and empirically (Wise & Hersh, 2012), emphasizing the need to implement effective psychological interventions.
Along with medical treatments, it is necessary to control this disease and its related complications. In the meantime, one of the variables related to the existence that affects the function of older people and their satisfaction with life is the feeling of security (Montazerolhodjah et al., 2018). In this research, the researcher tries to measure the effect of GCBT training on PS variables in patients with T2DM. The occurrence of emotional, physical, and sexual injuries in childhood is one of the factors that can institutionalize a sense of insecurity and being at risk in the memory and unconsciousness of people.
Another variable that seems to be effective in patients with T2DM is psychological security (PS), which can also be called mental security or a sense of inner security (Wang et al., 2019). It is the smoothest platform for the growth of mental creativity and innovation (Xu et al., 2022; Zhang et al., 2010; Wang et al., 2019). PS is the feeling of satisfying one’s current needs (Maslow, 1942). The feeling of PS is considered the most effective way to encourage people to think and try to achieve growth and progress at different personal, family, professional, and social levels (Toobert & Glasgow, 1994; Kumar et al., 2024). This concept refers to an environment understood as “an impersonal and non-threatening environment.” Patients with T2DM suffer from depression, despair, and feelings of inferiority more than other people. Satisfying the need for security healthily and desirably throughout life can provide the basis for achieving other needs such as self-esteem, loving and being loved, and self-actualization. However, the effectiveness of a distinctive therapy depends on medication adherence. Medication adherence in patients with T2DM in primary health clinics is poor, which is a cause for concern because medication nonadherence can worsen the disease (Sun et al., 2023).
There are many treatments to adapt to the PS and DSCA of older patients with T2DM; one of these therapies is mindfulness. This approach places less emphasis on changing the content of thoughts and focuses more on changing attention, awareness, and communication with thoughts. It puts a lot of emphasis on accepting thoughts instead of changing them and emphasizes that we understand thoughts as thoughts, not as a reflection of reality. Another new treatment is self-management-based therapy. Also, there is acceptance and commitment therapy (ACT). Increasing psychological flexibility is considered the primary assumption of the mechanism of change in ACT and increasing mindfulness dimensions, which plays an essential role in the possible effects of the intervention. In this regard, Eilenberg et al. (2016) and Bonacquisti et al. (2017) declared that ACT is effective in treating anxiety and mood disorders.
Much evidence shows the effectiveness of group cognitive-behavioral therapy (GCBT) on PS, DSCA, and other health-related benefits (Samadzadeh et al., 2018). This therapy is based on the solid cooperation between the patient and the therapist. CBT-based interventions allow the patient to respond wisely instead of an immediate and ill-considered response to things. Therefore, by providing a platform for deep attention to the experiences of the disease and accepting the emotions and suffering caused by it, it intervenes. For this reason, conscientious people have a higher ability in efficiency and problem-solving than others (Emanuel et al., 2010). Based on the research, as soon as the patients reach mental security, they can achieve good results in relative recovery from their illnesses and, as a result, get a better view of their QoL and future. This outcome is also true in older people. Previous research has shown that GCBT is effective for a variety of mental problems (e.g. psychological symptoms), physical conditions (e.g. irritable bowel syndrome and fatigue syndrome), behavioral problems (overweight and antisocial behaviors) (Nakao et al., 2021), motivating and accepting responsibility for DSCA (Toobert & Glasgow, 1994), and reducing anxiety and depression (Beltman et al., 2012). A pilot study showed that GCBT effectively improves and increases DSCA, such as blood sugar control in adolescents with T2DM (Serlachius et al., 2016). ecause previous research on PS and DSCA has primarily focused on the workplace (Probst, 2002; Hu et al., 2018), the PS and DSCA of older patients with T2DM have not received sufficient attention. Tarkhan (2011) has studied the effectiveness of short-term interpersonal group therapy on the psychological well-being and QoL of spouses of people with an addiction. Nakao et al., (2021) found the effectiveness of GCBT on mental and physical variables (such as PS and psychological distress) related to patients with T2DM. Abbas et al. (2023) declared that GCBT has a significant reduction in diabetes distress, psychological distress, PS, depressive symptoms, and health anxiety and has a significant enhancement in treatment adherence, QoL, and physical activity schedule of the patients with T2DM. Pan et al. (2023) supported the effectiveness of an internet-based GCBT program for students with psychological distress. Skoglund et al. (2024) declared that GCBT decreases statistically significantly in people with comorbid PS. GCBT is short and limited in time, but it tries to help clients develop independent self-help skills. In addition, the GCBT approach relies on questioning and discovery combined with strategy and not on convincing. In this approach, which is based on inductive methods, the patient learns to look at thoughts and beliefs as hypotheses that must be tested. Finally, this approach is educational in that GCBT techniques are considered skills that must be learned through practice and entered into the patient’s environment through homework (Welschen et al., 2014). Based on GCBT intervention, skills to evaluate irrational and negative thinking are learned, and a range of standard cognitive-behavioral coping skills are taught, which is a guide for flexibility in choosing appropriate strategies. It reduces psychological symptoms (Serlachius et al., 2016). In a pilot study, it was shown that GCBT is effective in improving and increasing PS in adolescents (Nakao et al., 2021).
Since the diagnosis of diabetes has important effects on patients’ psychological and social performance, patients must devote a lot of attention and energy to self-management of the disease (Dineen-Griffin et al., 2019). The success of patients in integrating a self-management and DSCA approach with their existing lifestyle depends on the extent to which diabetes-specific events interact with the patient’s existing beliefs, thoughts, feelings, and behaviors. Diabetes is often associated with mental problems and disorders, and unfortunately, these problems reduce the patient’s ability to self-manage the disease and perform the DSCA. Decreasing the ability of patients to control diabetes aggravates their psychological problems and causes patients to get caught in a vicious cycle. These problems may even become more severe with the psychological reactions of patients that negatively impact the experience of diabetes symptoms. Identifying effective treatments to increase PS and the DSCA to be persistent for treatment is very necessary for patients with T2DM.
In general, PS and DSCA are among the basic needs of patients with T2DM, which can facilitate their interaction with family and social environment. Although previous research has emphasized the role and importance of PS and DSCA in learning and problem-causing behaviors of diabetic patients (Nakao et al., 2021; Abbas et al., 2023; Pan et al., 2023), the related variables and explaining the effectiveness of GCBT on the PS and DSCA of patients with T2DM, have not been considered. In addition, according to the background review, few researchers have investigated the effectiveness of GCBT on PS and the DSCA. Therefore, while completing this gap, this research can provide counselors, clinical psychologists, and therapists with a suitable solution for appropriate psychological interventions in patients to expand theoretical knowledge in diabetes and the effectiveness of interventions on important variables in this field. Also, the results of this study will develop knowledge of the efficacy of GCBT on PS and the DSCA. This treatment can effectively identify rational and hopeful thought patterns and increase the perception of well-being. As a result, it will positively affect constructive PS and the DSCA. Improving PS and DSCA is one of the most important steps to help patients control and manage their disease. Therefore, this research aimed to answer whether group GCBT effectively treats PS and the DSCA in people with T2DM.
Materials and Methods
Participants and design
This quasi-experimental research explored the effectiveness of GCBT on the PS and DSCA in patients with T2DM. The study was conducted with a pre-test -post-test design and a control group of 30 older female diabetic patients during the summer of 2023. The patients were randomly assigned into two groups (test and control) of 15 subjects (Figure 1).
The test group, along with regular medical care, received GCBT for 8 weekly sessions of 1.5 hours. The control group received only regular medical care. Due to the research limitations, providing a placebo or alternative intervention in the control group was impossible. Still, in the end, the intervention related to the test group was also implemented in the control group. The intervention was a special protocol that had 8 sessions. The aim was to investigate the effectiveness of a short-term and cost-effective intervention according to the research objectives and the studied variables.
The Equation 1 was used for sampling (Sarabadani et al., 2023). According to the values of δ= 3.52 (common SD of PS and the DSCA scores), d=2.81 (the pre-test mean score differences of PS and the DSCA in the test and control groups), statistical power=0.9, and error level or α equal to 0.05, the sample size was equal to 13 people for each group. With the possibility of a sample drop in the groups, the sample size of 15 people was considered for each group.
To comply with ethical considerations, written consent was obtained from the subjects for informed participation in the research. Also, emphasis was placed on the principle of confidentiality of the participants’ information and the implementation of this training for the control group after the end of the experiment. The participants were initially numbered from 1 to 30. After matching based on demographic characteristics such as age, gender, and history of disease, they were randomly assigned to the test and control groups in odd and even pairs.
Inclusion and exclusion criteria
The inclusion criteria were as follows: A specialist doctor’s diagnosis of T2DM, having at least a diploma, being 55 years old or older, and at least 6 months had passed since the onset of the disease.
The exclusion criteria were as follows: Absence of more than two sessions, suffering from another chronic physical and mental illness, suffering from addiction or being about to divorce, having diabetes complications, and having any medical problems that prevent self-care behaviors (such as exercise and regular physical activity).
Study procedures
Demographic questionnaire
The demographic questionnaire used in this study consisted of two parts, including demographic characteristics (11 questions) and two PS and DSCA questionnaires. The first section was used to evaluate the personal information of the participants, including their birth date and educational level. Before and after the GCBT intervention, both groups were assessed in terms of PS and DSCA.
Maslow’s psychosocial security scale
Maslow, (1942) created the PS questionnaire to measure different aspects of PS. It has 62-question self-report scales and 15 subscales. Its scoring is done with “yes” and “no” options. Correct answers are given a score of 0, and incorrect answers are provided 1. Achieving a high score (62 points) indicates a person’s high PS, and a low score indicates low PS. Bowen et al. (2010) reported that Cronbach’s α coefficient was 0.92. Also, the reliability of this questionnaire was obtained through the Cronbach α of 0.74.
The summary of DSCA measure
The 12-item summary of DSCA measure was introduced by Toobert & Glasgow, (1994). A full score is 7; if it is not done on any day of the week, a score of 0 is awarded. To determine the level of desirability of the self-care situation, in addition to the average score scale, the range of scores obtained was from 0 to 70. It was divided into three parts: undesirable (0-23), semi-desirable (24-47), and desirable (47-70). An overall compliance score is obtained by adding up the scores of each question. Kuwahara et al. (2004) obtained the reliability of The summary DSCA questionnaire through the Cronbach α of 0.76, and its content validity was satisfactory. To determine the diagnostic validity, the questionnaire was administered to 40 diabetic patients and 40 healthy people, and the independent t test showed that the difference between the two groups is significant and the test has a suitable diagnostic validity. The questionnaire was conducted in 2 states with a time interval of one week to obtain retest reliability, and the findings indicated that the questionnaire has a relatively high and suitable retest. Also, the validation studies showed a correlation higher than 0.89 between questions and 4 areas (Ryff et al., 2002).
Research method
The participants (30 elderly female patients with T2MD) were initially numbered from 1 to 30. After matching based on demographic characteristics such as age, gender, and history of disease, they were randomly assigned to the test (intervention) and the control groups. Figure 1 shows no missing data during the implementation phase; all subjects completed the experimental process. Then, a pre-test was performed (PS and DSCA measures). The method of conducting the research was that after the necessary coordination with the officials of the Fariman Health Diabetes Center, written consent was obtained from the sample to participate in the study after stating the purpose of the research. The questionnaires were mainly completed by the participants and, in some cases, by the patient with the help of her companion. Based on the clinical handbook of couple therapy, the test group received GCBT for 8 weekly sessions of 2 hours with GCBT (Baucom et al., 2015). The control group was placed on the waiting list and received only regular medical care during this period. A senior clinical expert held the sessions. The GCBT program was performed for three months (August-September 2023). All patients replied to the scales before (pre-test ) and immediately after the intervention (post-test).
GCBT intervention plan
The patient’s PS and DSCA programs (the amount of time for sports activities, blood sugar monitoring, diet compliance, and foot care) were announced through a written self-report by the patient’s relatives who lived with or cared for her (feminine). It should be noted that the researcher completed the questionnaires in the form of a structured interview with the participants in 15-20 minutes. The details of the intervention in the test group are described in Table 1.
Data analysis
The data were described by descriptive statistics (Mean±SD) and analyzed by inferential statistics (analysis of covariance analysis). SPSS software, version 24 used for the statistical analysis.
Results
Descriptive findings
The participants of this research were 30 older female patients with T2DM. The Mean±SD of the age of the samples was 58.14±23.47 years. They were in the age range of 55 to 67 years. The highest frequency is related to the age of 55-59, and the lowest frequency is related to the age of 59-67. The subjects were randomly divided into two equal groups; these two groups were matched in terms of age. Table 2 shows the variables’ Mean±SD in the pre-test and post-test stages. As seen, the mean of the test group increased compared to the control group in PS.
Analysis of covariance
The presuppositions of covariance analysis were evaluated before analyzing the data by covariance analysis. The Kolmogorov-Smirnov (K-S) test results on PS variables were not significant for any of the variables, indicating that the assumption of the data normality test is established at a level of <0.05 (Table 2).
Also, Levene’s test for equality of variances results were not significant, indicating that the individual group covariance matrices are equal (homogeneous across groups) and that the assumption of equal variance is valid (Table 2). According to the test for homogeneity of variance, the test and control groups are not significant for the PS and the DSCA components (Table 2). Therefore, the variances of the test and the control groups are equal.
The results of the test of homogeneity of regression slopes of the research variables have shown that the F value of the interaction for the sameness of the regression line slope for the PS (F=3.72) and the DSCA (F=2.88) variables are at a significant level of 0.142 and 0.063, respectively, which are insignificant. In other words, the homogeneity of regression slopes is accepted.
Therefore, to investigate the effect of GCBT on increasing the PS and the DSCA of patients with T2DM, the ANCOVA test was used with the control of the pre-test effect (Table 3). As can be seen, the independent variable was effective on the dependent variables. In other words, the test and control groups significantly differ in the PS and the DSCA variables (P<0.0001). Also, by controlling the pre-test effect and calculating according to the F coefficient, a significant difference is seen between the adjusted averages of PS and the DSCA scores according to group membership “test and control” in the post-test stage (P<0.0001). Therefore, the GCBT method had a greater effect on the PS and DSCA of patients with T2DM in the test group participants.
The effect size of “practical significance” was 0.31; that is, 31% of the total variance changes or individual differences in the PS and the DSCA of patients with T2DM were caused by the effect of GCBT. The statistical power for the PS and DSCA were 0.92 and 0.97, respectively, indicating the sampling volume’s adequacy. According to Table 4, There is a significant difference between the level of PS (P=0.001, F=12.41) and the DSCA (P=0.001, F=15.58) of the subjects in the test and the control groups. With 95% certainty, the null hypothesis is rejected, and the main hypothesis is confirmed. We conclude that GCBT effectively increases the PS and the DSCA of patients with T2DM.
To investigate the effect of GCBT on the components of PS and the DSCA, we used multivariate covariance analysis, where the dependent variable includes the DSCA and the components of PS: Environmental maladjustment, paranoia, self-belief, passion for life, depression, sense of bliss, social security, self-awareness, self-confidence, nervousness, disappointment, interest in life, adjustment with others, feeling of healthiness, and feeling of inferiority.
Table 4 shows the difference between the post-test of the three groups in the DSCA and PS components, indicating a significant difference between the test and the control groups. GCBT has increased the scores of self-belief, passion for life, sense of bliss, social security, self-awareness, self-confidence, interest in life, adjustment with others, and feeling of healthiness. Also, the scores of environmental maladjustments, paranoia, depression, nervousness, disappointment, and feeling of inferiority decreased in the post-test, and all the components of PS are significant (P<0.05). So, there is a significant difference between the DSCA and PS components scores in the test and control groups in the post-test. We conclude that GCBT affects the DSCA and the PS components of patients with T2DM.
Discussion
This quasi-experimental research aimed to explore the effectiveness of GCBT on the PS and DSCA in patients with T2DM. It was conducted with a pre-test -post-test design and a control group on 30 elderly female diabetic patients during the summer of 2023. The results of ANCOVA indicated that GCBT significantly increased the PS and the DSCA in patients with T2DM (P≤0.05). GCBT was effective in improving the PS and the DSCA of the patients with T2DM.
According to the results, GCBT was effective in improving and enhancing the PS of patients with T2DM (P<0.001). GCBT intervention can be introduced as a fruitful psychological intervention. It can increase psychological well-being indicators, QoL, and greater adherence to treatment recommendations. The increase in this way will help to prevent the complications of diabetes and will be an effective step towards increasing the level of mental and physical health of patients with T2DM. Previous research such as Haneda et al. (2016), Welschen (2014), Serlachius et al., (2016), Puig-Domingo et al., (2020), Delshad Noghabi et al. (2021), Nakao et al., (2021), Farimanian and Bayazi (2024) and Ramezani Rezaabad et al. (2024) have confirmed the effectiveness of GCBT on PS in their research results. Research has shown that GCBT increases PS, reduces depression symptoms, and a relative decrease in symptoms of anxiety in women with T2DM (Basiri et al., 2023). In other words, the decline in the symptoms of depression and anxiety in people with T2DM is associated with improving the PS. The results of other researchers suggest that PS in people with T2DM can be influenced by positive psychological characteristics such as life expectancy and efficient attitudes (Xu et al., 2022). Nurses can improve their PS by improving efficient and hopeful attitudes in patients with T2DM. Nurses can also help patients with T2DM, who often have cognitive errors and irrational and destructive beliefs in their lives, by informing patients of their irrational documents and beliefs. Using their knowledge and experience to help modify these misconceptions and promote patient information literacy to create rational and efficient beliefs. As a result, patients, using experiences and enhancing health information, change the misconceptions and documents that have caused anxiety and depression and thus reduce their PS.
By examining the content of the materials presented in the psychological safety management training sessions in this research, it can be assumed that using behavioral strategies and strategies such as calming and creating a sense of calm in the affected person have also reduced his psychological symptoms and distress. On the other hand, cognitive strategies such as problem-solving, recognizing cognitive errors, fighting against negative thoughts, using logical thinking, and positive self-talk may change the attitudes and cognitions of patients so that they accept their illness and rationally face its psychological consequences. By applying the skills taught, they took steps to improve themselves and control the disease more effectively. Also, GCBT training sessions familiarize patients with T2DM with how stress affects them and teach them to look at stressful situations as solvable problems. In addition, different coping methods and their effective management are shown to patients with T2DM. This makes them feel that they have more control over their surroundings, evaluate them as less threatening when dealing with such situations, and when faced with said situations, having more efficient coping skills, they can solve them more effectively and be safe from the negative psychological effects caused by ineffective coping with stressful situations. Therefore, they can have better control over the anxieties caused by the disease.
Anxiety caused by suffering from a chronic and permanent disease such as diabetes can lead to many psychological complications. Examples include depression, insomnia, anxiety, physical symptoms, and social dysfunction. Anxiety in its chronic state causes the erosion of the physical and mental reserves of the affected person by creating a state of permanent alertness in the body. This condition plays an effective role by using the mechanism of the learned helplessness effect of the diabetic person on non-compliance with the treatment. This helplessness happens because a person does not accept his diabetes in the early stages of diagnosis, and the stress caused by it due to the occurrence of psychological complications of the disease, which was mentioned, is placed between the stage of denial and acceptance of the disease. This state causes the observance of treatment points in the stage of feeling acceptance and non-observance in the stage of illness. Thus, the patients do not achieve regular control of their blood sugar, and they think it is impossible to control their blood sugar in both cases of following and not following the treatment. Therefore, these issues can be better overcome by teaching destructive thoughts to stop self-deception and skills to deal with disappointment, failure, and unfairness syndrome in meetings.
Also, GCBT effectively improved and encouraged the DSCA of patients with T2DM (P<0.001). These findings are in line with Christie et al., (2014), Serlachius et al., (2016), Puig-Domingo et al., (2020), Shegarf Nakhaei et al. (2021), and Alahyari et al. (2022). Research has shown that GCBT increases SCB, reduces depression symptoms, and has a relative decrease in symptoms of anxiety in women with T2DM. In other words, the decline in the symptoms of depression and anxiety in people with T2DM is associated with improving the DSCA (Bădescu et al., 2016). The results of some studies have shown that having sufficient motivation and information in women with vaginitis fertility will positively affect DSCA and disease recovery (Xu et al., 2022). The results of other researchers suggest that self-care behaviors in people with T2DM can be influenced by positive psychological characteristics such as life expectancy and efficient attitudes. Nurses can improve their self-care by improving efficient and hopeful attitudes in patients. Nurses can also help patients with T2DM, who often have cognitive errors and irrational and destructive beliefs in their lives, by informing patients of their irrational documents and beliefs. Using their knowledge and experience to help modify these misconceptions and promote patient information literacy to create rational and efficient beliefs. As a result, patients, using experiences and enhancing health-health information, change the misconceptions and documents that have caused anxiety and depression and thus reduce their DSCA.
One of the reasons for the effectiveness of GCBT in increasing the PS and the DSCA of patients with T2DM is that the quality of patient care skills results from one’s own beliefs, thoughts, behavior, and deeds and relates to one’s decisions and performance. GCBT, as a psychotherapeutic method, alters the destructive patterns that are effective on patients’ behavior and emotions (Hofmann et al., 2012). Nurses can emphasize the importance of acquiring cognitive information, feeling efficient, skills, and using these skills by providing GCBT training. Also, during the training, people learn fruitful behavioral methods in addition to working on negative thinking. People affected by these tutorials will find the ability to correct automatic thoughts and evaluate their evidence and the documents needed to approve and disapprove those.
Conclusion
The implementation of GCBT has led to improving PS and the DSCA in patients with T2DM. According to the obtained results, the effort to change the attitudes and negative beliefs in GCBT by patients with T2DM has led to the improvement of the psychological condition of diabetic patients. In this treatment, the attitude and mental perception of patients about their disease and its symptoms have been changed, and it can be used in psychological clinics and educational workshops to increase adherence to the treatment, the perception of the disease, and the QoL of patients with T2DM.
Recommendations
It is suggested to take help from this treatment method to increase the learning of correct thinking and judgment skills about diabetes and to deal with unrealistic thoughts about this disease. Therefore, counselors and therapists can use this method to improve the PS of patients with T2DM. In addition, it is recommended that planners design programs based on this research to improve the PS of patients with T2DM.
Implications for family therapy/practice
Clinical counselors and therapists of diabetes centers and clinics can use the GCBT approach in their therapy groups and training classes to improve the basic PS, not to be discouraged, and to continue the treatment and, as a result, increase the physical health of patients with T2DM.
Research limitations
Because this manuscript was extracted from the thesis and involved financial and time limitations for the implementation of the thesis, it was not possible to carry out a follow-up. The reason for choosing female patients was the limitation in sampling men, considering that this research was related to a student’s thesis. Also, it was impossible to increase the sample due to the limitations of the thesis or this research. However, it is mentioned in the limitations section, and it is suggested that the sample size be increased in other future research studies. Another limitation of this research was the potential biases associated with self-reported data. In our application to clinical intervention, we examined the effects of participant demographics on response bias before and after participation, and bias is lower in the Post-test than in the Pre-test. Any shift in metric from before to after an intervention is caused by the intervention itself and may lead to underestimates of program effects.
Direction for future research and recommendations
It is hoped that the results of this research can be a basis for further study in the PS of patients to help improve and treat patients with T2DM as much as possible. This research is suggested to be repeated with larger and diverse samples, long-term follow-ups, and studies to investigate these interventions’ mediating factors and variables. It is also recommended that experts design a special PS program for patients with T2DM, and the official integration of this training in diabetes treatment-care programs should be considered by experts and institutions active in this field.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Torbat-e-Jam Branch, the Islamic Azad University, Torbat-e-Jam, Iran (Code: IR.IAU.TJ.REC.1402.093).The study was performed in accordance with relevant guidelines and regulations.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization and supervision: Sima Farimanian and Mohammad Hossein Bayazi; Methodology: Mohammad Hossein Bayazi; Investigation and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers must thank the patients and those who helped them conduct this research.
References
Abbas, Q., Latif, S., Ayaz Habib, H., Shahzad, S., Sarwar, U., & Shahzadi, M., et al. (2023). Cognitive behavior therapy for diabetes distress, depression, health anxiety, quality of life and treatment adherence among patients with type-II diabetes mellitus: A randomized control trial. BMC Psychiatry, 23(1), 86. [DOI:10.1186/s12888-023-04546-w] [PMID]
Alahyari, A. Z., Bayazi, M. H., & Rajaei, A. R. (2021). The effectiveness of cognitive behavioral group intervention on depression and anxiety in patients with type II diabetes. European Review of Applied Psychology, 71(1), 100624. [DOI:10.1016/j.erap.2021.100624]
Baucom, D. H., Epstein, N. B., Kirby, J. S., & LaTaillade, J. J. (2015). Cognitive-behavioral couple therapy. In A. S. Gurman, J. L. Lebow, & D. K. Snyder (Eds.), Clinical handbook of couple therapy (pp. 23-60). New York: The Guilford Press. [Link]
Bădescu, S. V., Tătaru, C., Kobylinska, L., Georgescu, E. L., Zahiu, D. M., & Zăgrean, A. M., et al. (2016). The association between diabetes mellitus and depression. Journal of Medicine and Life, 9(2), 120-125. [PMID]
Basiri, R., Seidu, B., & Rudich, M. (2023). Exploring the interrelationships between diabetes, nutrition, anxiety, and depression: Implications for treatment and prevention strategies. Nutrients, 15(19), 4226. [DOI:10.3390/nu15194226] [PMID]
Beltman, S., & Schaeben, M. (2012). Institution-wide peer mentoring: Benefits for mentors. Student Success, 3(2), 33. [Link]
Bonacquisti, A., Cohen, M. J., & Schiller, C. E. (2017). Acceptance and commitment therapy for perinatal mood and anxiety disorders: Development of an inpatient group intervention. Archives of Women’s Mental Health, 20(5), 645–654. [DOI:10.1007/s00737-017-0735-8] [PMID]
Bowen, S., Chawla, N., & Marlatt, G.A. (2010) Mindfulness-based relapse prevention for the treatment of substance use disorders: A clinician’s guide. New York: Guilford Press. [Link]
Bryan, A. D., Jakicic, J. M., Hunter, C. M., Evans, M. E., Yanovski, S. Z., & Epstein, L. H. (2017). Behavioral and psychological phenotyping of physical activity and sedentary behavior: Implications for weight management. Obesity (Silver Spring, Md.), 25(10), 1653–1659. [DOI:10.1002/oby.21924] [PMID]
Christie, D., Thompson, R., Sawtell, M., Allen, E., Cairns, J., & Smith, F., et al. (2014). Structured, intensive education maximising engagement, motivation and long-term change for children and young people with diabetes: A cluster randomised controlled trial with integral process and economic evaluation-the CASCADE study. Health Technology Assessment (Winchester, England), 18(20), 1–202. [DOI:10.3310/hta18200] [PMID]
Collins, M. M., Corcoran, P., & Perry, I. J. (2009). Anxiety and depression symptoms in patients with diabetes. Diabetic medicine : A Journal of the British Diabetic Association, 26(2), 153–161. [DOI:10.1111/j.1464-5491.2008.02648.x] [PMID]
Delevry, D., Ho, A., & Le, Q. A. (2021). Association between processes of diabetes care and health care utilization in patients with diabetes: Evidence from a nationally representative US sample. Journal of Diabetes, 13(1), 78-88. [DOI:10.1111/1753-0407.13109] [PMID]
Delshad Noghabi, A., Bayazi, M. H., Rajaei, A., & Mohammadzadeh, F. (2021). [Effectiveness of self-management training based on group cognitive behavioral therapy on quality of life in adults with metabolic syndrome: A randomized clinical trial (Persian)]. Journal of Mazandaran University of Medical Sciences, 31(197), 81-92. [Link]
Dineen-Griffin, S., Garcia-Cardenas, V., Williams, K., & Benrimoj, S. I. (2019). Helping patients help themselves: A systematic review of self-management support strategies in primary health care practice. Plos One, 14(8), e0220116. [DOI:10.1371/journal.pone.0220116] [PMID]
Eilenberg, T., Fink, P., Jensen, J. S., Rief, W., & Frostholm, L. (2016). Acceptance and commitment group therapy (ACT-G) for health anxiety: A randomized controlled trial. Psychological Medicine, 46(1), 103-115. [DOI:10.1017/S0033291715001579] [PMID]
Emanuel, A. S., Updegraff, J. A., Kalmbach, D. A., & Ciesla, J. A. (2010). The role of mindfulness facets in affective forecasting. Personality and Individual differences, 49(7), 815-818. [DOI:10.1016/j.paid.2010.06.012]
Farimanian, S., & Bayazi, M. H. (2024). Effectiveness of group cognitive-behavioral therapy on the psychological security of patients with Type II Diabetes Mellitus. Practice in Clinical Psychology, 12(4), 345-360. [DOI:10.32598/jpcp.12.4.931.1]
Frey, A., Sell, R., Homola, G. A., Malsch, C., Kraft, P., & Gunreben, I., et al. (2018). Cognitive deficits and related brain lesions in patients with chronic heart failure. JACC: Heart Failure, 6(7), 583-592. [Link]
Forbes, A., & While, A. (2009). The nursing contribution to chronic disease management: A discussion paper. International Journal of Nursing Studies, 46(1), 120-131. [DOI:10.1016/j.ijnurstu.2008.06.010]
Haneda, M., Noda, M., Origasa, H., Noto, H., Yabe, D., & Fujita, Y., et al. (2018). Japanese clinical practice guideline for diabetes 2016. Diabetology International, 9, 1-45. [Link]
Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research, 36(5), 427–440. [DOI:10.1007/s10608-012-9476-1] [PMID]
Hu, Y., Zhu, L., Zhou, M., Li, J., Maguire, P., & Sun, H., et al. (2018). Exploring the influence of ethical leadership on voice behavior: how leader-member exchange, psychological safety and psychological empowerment influence employees’ willingness to speak out. Frontiers in Psychology, 9, 1718. [DOI:10.3389/fpsyg.2018.01718] [PMID]
Jordan, S. D., Könner, A. C., & Brüning, J. C. (2010). Sensing the fuels: glucose and lipid signaling in the CNS controlling energy homeostasis. Cellular and Molecular Life Sciences, 67, 3255-3273. [Link]
Keyes, C. L., Shmotkin, D., & Ryff, C. D. (2002). Optimizing well-being: The empirical encounter of two traditions. Journal of Personality and Social Psychology, 82(6), 1007–1022. [PMID]
Krishna, P. (2018). Depression, anxiety, and stress levels in patients with type 2 diabetes mellitus. National Journal of Physiology, Pharmacy and Pharmacology, 8(11), 1570-72. [DOI:10.5455/njppp.2018.8.0929117092018]
Kumar, V., Pavitra, K. S., & Bhattacharya, R. (2024). Creative pursuits for mental health and well-being. Indian Journal of Psychiatry, 66 (Suppl 2), S283-S303. [DOI:10.4103/indianjpsychiatry.indianjpsychiatry_781_23] [PMID]
Kuwahara, A., Nishino, Y., Ohkubo, T., Tsuji, I., Hisamichi, S., & Hosokawa, T. (2004). Reliability and validity of the Multidimensional Health Locus of Control Scale in Japan: Relationship with demographic factors and health-related behavior. The Tohoku Journal of Experimental Medicine, 203(1), 37–45. [DOI:10.1620/tjem.203.37] [PMID]
Maslow, A. H. (1942). The dynamics of psychological security-insecurity. Journal of Personality, 10(4), 331-344. [DOI:10.1111/j.1467-6494.1942.tb01911.x]
Montazerolhodjah, M., Sharifnejad, M., & Rajabi, M. (2018). [Assessment of the effect of physical components of urban spaces on sense of security from the viewpoint of the elderly (case study: Khan Square, Yazd City)(Persian)]. Journal of Iranian Architecture & Urbanism (JIAU), 9(1), 91-105. [Link]
Moss-Morris, R., McAlpine, L., Didsbury, L. P., & Spence, M. J. (2010). A randomized controlled trial of a cognitive behavioural therapy-based self-management intervention for irritable bowel syndrome in primary care. Psychological Medicine, 40(1), 85–94.[DOI:10.1017/S0033291709990195] [PMID]
Nakao, M., Shirotsuki, K., & Sugaya, N. (2021). Cognitive-behavioral therapy for management of mental health and stress-related disorders: Recent advances in techniques and technologies. BioPsychoSocial Medicine, 15(1), 16. [DOI:10.1186/s13030-021-00219-w] [PMID]
Oyewole, O. O., Ale, A. O., Ogunlana, M. O., & Gurayah, T. (2023). Burden of disability in type 2 diabetes mellitus and the moderating effects of physical activity. World Journal of clinical Cases, 11(14), 3128–3139. [DOI:10.12998/wjcc.v11.i14.3128] [PMID]
Pan, J. Y., Carlbring, P., & Lu, L. (2022). A therapist-guided internet-based cognitive behavioral therapy program for Hong Kong university students with psychological distress: A study protocol for a randomized controlled trial. Internet Interventions, 31, 100600. [DOI:10.1016/j.invent.2022.100600] [PMID]
Probst, T. M. (2002). The impact of job insecurity on employee work attitudes, job adaptation, and organizational withdrawal behaviors. In: Brett JM, Drasgow, F, editors. The psychology of work: Theoretically based empirical research (pp. 141-168). New York: Psychology Press. [Link]
Puig-Domingo, M., Marazuela, M., Giustina, A. (2020). COVID-19 and endocrine diseases. A statement from the European Society of Endocrinology. Endocrine, 68(1), 2-5. [DOI:10.1007/s12020-020-02294-5] [PMID]
Ramezani Rezaabad, M., Bighonah, M., Morghzari, M. & Taleghani, A. (2022). Evaluation of the effectiveness of a combined cognitive-behavioral approach and mindfulness on learned helplessness and regulation of cognitive emotion and blood pressure in patients with coronary heart disease. Journal of Modern Psychological Researches, 17(66), 159-167. [DOI:10.22034/jmpr.2022.15286]
Ricci-Cabello, I., Ruiz-Pérez, I., Rojas-García, A., Pastor, G., Rodríguez-Barranco, M., & Gonçalves, D. C. (2014). Characteristics and effectiveness of diabetes self-management educational programs targeted to racial/ethnic minority groups: A systematic review, meta-analysis and meta-regression. BMC Endocrine Disorders, 14(60), 1-13. [Link]
Saffariantoosi, K., & Khaleghi, M. R. (2024). The mediating role of organizational citizenship behavior in the relationship between career self-efficacy and career success among construction project managers in Mashhad. Current Psychology, 43, 23971–23984. [DOI:10.1007/s12144-024-06127-w]
Samadzadeh, A., Salehi, M., Banijamali, S. S., & Ahadi, H. (2018). [Comparison of the effectiveness of cognitive behavioral therapy with mindfulness training on psychological well-being in patients with type 2 diabetes (Persian)]. Journal of Psychological Science, 17(68), 491-499. [Link]
Sarabadani, A., Hassanzadeh, R., & Emadian, S. O. (2023). [Comparison of the effectiveness of cognitive therapy based on mindfulness and life therapy on mental well-being and psychological security in women with generalized anxiety disorder: A quasi-experimental study (Persian)]. Journal of Rafsanjan University of Medical Sciences, 21(12), 1249-1266. [DOI:10.52547/jrums.21.12.1249]
Serlachius, A. S., Scratch, S. E., Northam, E. A., Frydenberg, E., Lee, K. J., & Cameron, F. J. (2016). A randomized controlled trial of cognitive behavior therapy to improve glycaemic control and psychosocial well-being in adolescents with type 1 diabetes. Journal of Health Psychology, 21(6), 1157-1169. [DOI:10.1177/1359105314547940] [PMID]
Shegarf Nakhaei, M. R., Akbari Oryani, T., Bayazi, M. H., Shomoossi, N., & Hoseini, B. L. (2021). Influence of cognitive behavioral therapy on psychological well-being and Ego-resiliency in type 2 diabetes patients in Sabzevar. Iranian Journal of Diabetes and Obesity, 13(2), 88-94. [DOI:10.18502/ijdo.v13i2.6477]
Skoglund, H., Sivertsen, B., Kallestad, H., & Vedaa, Ø. (2024). Digital cognitive behavioral therapy for insomnia for people with comorbid psychological distress: A large scale randomized controlled trial. Sleep Medicine, 121, 241–250. [DOI:10.1016/j.sleep.2024.06.026] [PMID]
Snoek, F. J. & Skinner, T. C. (2006). “Psychological aspects of diabetes management”. Medicine, 34(2), 61-63. [DOI:10.1383/medc.2006.34.2.61]
Sun, J., Hu, W., Ye, S., Deng, D., & Chen, M. (2023). The description and prediction of incidence, prevalence, mortality, disability-adjusted life years cases, and corresponding age-standardized rates for global diabetes. Journal of Epidemiology and Global Health, 13(3), 566-576. [DOI:10.1007/s44197-023-00138-9] [PMID]
Tayefi, B., Sohrabi, M. R., & Kasaeian, A. (2015). Patients' satisfaction with the diabetes control and prevention program in Tehran, Iran: A cross sectional study. Journal of Research in Health Sciences, 15(4), 239-243. [Link]
Tarkhan, M. (2011). [The effectiveness of group interpersonal therapy on psychological well-being and life quality of addicted individual wives (Persian)]. Journal of Educational Psychology, 2(1), 23-36. [Link]
Toobert, D. J., Hampson, S. E., & Glasgow, R. E. (2000). The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care, 23(7), 943–950. [DOI:10.2337/diacare.23.7.943] [PMID]
Valenzuela, M. J., Münzenmayer, B., Osorio, T., Arancibia, M., & Madrid, E. (2018). [Association between depressive symptoms and metabolic control in patients with type 2 diabetes mellitus: A cross-sectional study (Spanish)]. Revista medica de Chile, 146(12), 1415–1421. [DOI:10.4067/s0034-98872018001201415] [PMID]
World Health Organization (WHO). (2000). Obesity: preventing and managing the global epidemic: Report of a WHO consultation. Geneva: World Health Organization. [Link]
Wang, J., Long, R., Chen, H., & Li, Q. (2019). Measuring the psychological security of urban residents: Construction and validation of a new scale. Frontiers in Psychology, 10, 2423. [DOI:10.3389/fpsyg.2019.02423] [PMID]
Welschen, L. M., van Oppen, P., Bot, S. D., Kostense, P. J., Dekker, J. M., & Nijpels, G. (2013). Effects of a cognitive behavioral treatment in patients with type 2 diabetes when added to managed care; a randomised controlled trial. Journal of Behavioral Medicine, 36(6), 556-566. [DOI:10.1007/s10865-012-9451-z] [PMID]
Wise, E. H., Hersh, M. A., & Gibson, C. M. (2012). Ethics, self-care and well-being for psychologists: Reenvisioning the stress-distress continuum. Professional Psychology: Research and Practice, 43(5), 487–494. [DOI:10.1037/a0029446]
Xu, Z., Wang, H., & Suntrayuth, S. (2022). Organizational climate, innovation orientation, and innovative work behavior: The mediating role of psychological safety and intrinsic motivation. Discrete Dynamics in Nature and Society, 2022, 1-10. [DOI:10.1155/2022/9067136]
Type of Study: Original Research Article |
Subject:
Cognitive behavioral
Received: 2024/12/23 | Accepted: 2025/02/15 | Published: 2025/04/1
Received: 2024/12/23 | Accepted: 2025/02/15 | Published: 2025/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |