Volume 13, Issue 1 (Winter 2025)
PCP 2025, 13(1): 33-46 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ahanian Moghaddam P, Atashpour S H, Golparvar M. Comparing the Effectiveness of Combined Schema Therapy and Mindfulness With Schema Therapy and CBT on Psychological Flexibility. PCP 2025; 13 (1) :33-46
URL: http://jpcp.uswr.ac.ir/article-1-950-en.html
URL: http://jpcp.uswr.ac.ir/article-1-950-en.html
1- Department of Counseling, Faculty of Educational Sciences and Psychology, Isfahan (Khorasgan) Branch, Islamic Azad University, Isfahan, Iran.
2- Department of Counseling, Faculty of Educational Sciences and Psychology, Isfahan (Khorasgan) Branch, Islamic Azad University, Isfahan, Iran. ,hamidatashpour@gmail.com
2- Department of Counseling, Faculty of Educational Sciences and Psychology, Isfahan (Khorasgan) Branch, Islamic Azad University, Isfahan, Iran. ,
Keywords: Psychological flexibility, Schema therapy, Mindfulness, Cognitive behavioral therapy (CBT), Obsession
Full-Text [PDF 638 kb]
(1366 Downloads)
| Abstract (HTML) (3940 Views)
Full-Text: (795 Views)
Introduction
Throughout the general population, obsessive-compulsive disorder (OCD) has an estimated lifetime prevalence ranging from 2.3% to 8.3%, which is projected to increase to 15% by 2026 (Hermida-Barros et al., 2024). In recent years, extensive studies have been conducted in the etiology and treatment of psychological disorders, resulting in the identifica-tion of over 580 different treatment models. Certain disorders, such as depression, anxiety, and obsession, have higher prevalence rates and lead to more significant functional impairments. As a result, they have attracted considerable attention from researchers (Ponzini & Steinman, 2021). OCD, in particular, can significantly impact women and lead to severe functional impairments, warranting a focused approach involving screening and early diagnosis to mitigate its negative consequences (Caudek et al., 2020).
Individuals with OCD experience difficulties in various domains, including psychological flexibility (Bhatt, 2024). Consequently, OCD has garnered significant attention from re-searchers in the fields of etiology and treatment. The disorder is time-consuming for affected individuals and can impair various aspects of their lives, such as occupational func-tioning, interpersonal relationships, and academic performance. Moreover, its severity often increases over time, necessitating specialized therapeutic interventions (Leeuwerik et al., 2020).
Individuals with OCD often struggle with various aspects of executive functioning, including psychological flexibility, response inhibition, visual and verbal memory, and emotional processing (Wheaton et al., 2021). Psychological flexibility, a key component of executive functioning, refers to the ability to adapt effectively to changing demands (Darby et al., 2018). Those with high psychological flexibility can assess new problems and situations from various angles and develop with innovative alternative options and ideas. In contrast, people with lower psychological flexibility find it challenging to let go of their initial learning and tend to persist in their original beliefs, with negative consequences (Deveci et al., 2024). This rigidity hampers their ability to adapt to new circumstances and increases their vulnerability to anxiety (Hayes et al., 2004).
Individuals with OCD often experience decreased psychological flexibility. This limitation contributes to rigid and repetitive thoughts and behaviors, hindering their ability to adapt to changes (Caudek et al., 2020). Research demonstrates that people with OCD symptoms exhibit lower levels of psychological flexibility (Francazio & Felssner, 2015; Graner & Pittenger, 2017; Feinberg et al., 2015). A study conducted by Izadi et al. (2014) revealed that participants with OCD who engaged in interventions designed to enhance flexibility and reduce experiential avoidance reported fewer symptoms compared to their peers. Similarly, Den Ouden, et al. (2020) found that individuals with OCD tend to exhibit less flexibility, rely more on avoidance strategies, and display increased obsessive symptoms. Furthermore, research by Sanaei Moharrer and Mirshekari (2017) affirmed the relationship between psychological flexibility and anxiety in the development and persistence of obsessive-compulsive symptoms.
Research suggests that individuals with obsessive-compulsive symptoms exhibit lower levels of psychological flexibility (Francazio & Felssner, 2015; Gruner & Pittenger, 2017; Fineberg et al., 2015; Caudek et al., 2020). Consistent with these results, a study conducted by Izadi et al. (2014) revealed that individuals with OCD who received interventions to en-hance flexibility and reduce experiential avoidance reported fewer symptoms compared to those who did not. Den Ouden, et al. (2020) also found in a similar study that these individuals displayed lower psychological flexibility, utilized more avoidance-based coping strategies, and manifested more obsessive symptoms. Additionally, Sanaei Moharrer and Mirshe-kari (2017) affirmed the role of psychological flexibility and anxiety in the development and persistence of symptoms associated with OCD.
People with OCD often encounter obsessive symptoms and struggle with psychological flexibility, prompting counselors and researchers to explore various therapeutic approaches to help them. Recent third-wave cognitive-behavioral therapies, such as schema therapy and mindfulness-based therapy, have been specifically tailored to address the needs of individuals with OCD. Schema therapy, developed by Young et al. (2003), is an innovative and integrative therapeutic model in the realm of cognitive therapy. It has garnered significant attention as an effective treatment for various anxiety disorders, particularly OCD. Schema therapy is recommended for patients who have not responded well to traditional cog-nitive-behavioral therapy. It has a particular emphasis on the developmental roots of psychological disorders, underlying patterns in psychological and social functioning, and maladaptive cognitions and behaviors of patients. From a schema therapeutic perspective, maladaptive schemas in individuals are activated by threatening and critical life events, leading to increased emotions such as anxiety, sadness, and anger. Schema therapy primarily focuses on reducing obsessive thoughts and behaviors by addressing under-lying maladaptive schemas, rather than directly confronting individuals with their fears. Sunde et al. (2019) concluded that schema therapy effectively reduced the symptoms of OCD in patients.
In addition to schema therapy, mindfulness-based therapy has emerged as a relatively contemporary approach utilized for individuals with OCD. Mindfulness practices enable patients to acknowledge their distressing thoughts without attempting to suppress them. Moreover, mindfulness fosters the development of awareness and acceptance of both internal and external experiences without passing judgment. Specifically tailored for OCD, mindfulness training assists patients in acknowledging their thoughts, feelings, and bodily sensations without automatically reacting. This form of therapy enhances self-awareness and non-judgment, thus preventing patients from engaging in negative evalua-tions, judgments, and biases (Reis et al., 2024).
Empirical results demonstrate the efficacy of mindfulness-based therapy in decreasing rumination, perfectionism, and thought-action fusion in women diagnosed with OCD (Khadem et al., 2023). Additionally, research supports the effectiveness of mindfulness intervention in reducing symptoms, such as obsessive checking, washing, slowing/repeating, and doubting (Mardpour & Hadizadeh Kaffash, 2017). Furthermore, mindfulness-based stress reduction techniques have shown promise in reducing obses-sive-compulsive symptoms (Ghazanfari & Sepahvand, 2014). Chien et al. (2022) researched the effectiveness of mindfulness-based interventions for individuals with OCD and found that these interventions were highly effective. Similarly, Mathur et al. (2021) reported comparable results, highlighting the success of mindfulness therapy in managing stress among patients with OCD.
Mindfulness-based therapies represent a more recent generation of cognitive-behavioral treatments characterized by differing therapeutic emphases and processes while also sharing fundamental similarities with their predecessors (Abramowitz & Reuman, 2020). CBT, identified as one of the most effective interventions for OCD, instructs patients to observe their thoughts from a broader perspective and cultivate a decentered relationship with the contents of their mind (Görmezoğlu et al., 2020). This approach emphasizes the development of the freedom to understand that most thoughts are merely thoughts, not facts or realities (Huang et al., 2023), often leading to enhanced insight and an increased sense of control over their lives (Hoppen et al., 2021). In this regard, research conducted by Cervin et al. (2024) revealed that cognitive flexibility and cognitive behavioral therapy (CBT) are interconnected and substantially influence the treatment process for patients. Onaral (2021) conducted a study examining the efficacy of third-wave therapies in the treatment of OCD. The results demonstrated that two primary treatment methods, medication and cognitive behavioral therapy, are effective in managing OCD. However, the high rates of patient drop-out and the persistence of residual symptoms following CBT have led researchers to seek alternative treatment approaches. Consequently, recent developments suggest that third-wave therapies hold significant promise in addressing these challenges.
In this study, the researcher compares the effectiveness of two intervention strategies, the combination of schema therapy and mindfulness, and schema therapy paired with CBT. The objective is to gain a deeper understanding of how these different approaches influence psychological flexibility in women diagnosed with OCD.
Schema therapy focuses on identifying and modifying deep-seated dysfunctional patterns often rooted in early life experiences. In contrast, mindfulness therapy encourages individuals to engage with their thoughts and feelings non-judgmentally and accepting. CBT, a widely recognized and effective method for treating various mental health disor-ders, emphasizes altering dysfunctional thoughts and behaviors.
By contrasting these three approaches, the researcher aims to gather scientific evidence regarding the efficacy and effectiveness of each method. This study provides valuable insights into which approach, or combination thereof, can best enhance the psychological flexibility of women with OCD. Ultimately, the results may inform the development of more effective and tailored treatment strategies for this particular group of clients.
Moreover, a reciprocal relationship between cognitive flexibility and CBT has been established, indicating a significant impact on patient outcomes when these components are integrated (Cervin et al., 2024).
Indeed, by recognizing the symptoms of obsessions and compulsions, we emphasize the importance of treating individuals with this disorder to prevent them from suffering distressing symptoms throughout their lives. People with OCD often engage in frequent rumination, leading to compulsive behaviors. Furthermore, they place excessive im-portance on their thoughts, validating and perpetuating a cycle of obsessive thoughts and behaviors. While CBT is widely supported by evidence, existing methods have limitations, with limited response to conventional approaches based on CBT and serotonin reuptake inhibitors. On the other hand, schema-focused and mindfulness-based approaches aim to not only modify the course and clinical presentation of OCD but also transform the underlying functioning of the mind through cognitive training.
Research into integrated models combining schema therapy and mindfulness-based therapies, as well as the integration of schema therapy and CBT for obsessive-compulsive symptoms, is limited. Our study aims to investigate these integrated models and answer the question: Does the efficacy of integrated interventions of schema therapy and mindfulness-based therapy differ from that of schema therapy and CBT on the psychological flexibility of women with obsessive-compulsive symptoms?
Materials and Methods
The study was conducted using a quasi-experimental design with pre-test-post-test and control and follow-up groups. The participants were exclusively women diagnosed with OCD who had been referred to the Nedaye Agahayi and Zehne Poya Clinic in Tehran City during the fall and winter of 2021. Initial contact was made with counseling centers and psychotherapy clinics in District 5 of Tehran City to form the sample group. Additionally, a call for participation in group therapy was made in the same district. Interested participants messaged the word “obsession” to a provided mobile number and were subsequently contacted by the researcher. Eligible individuals underwent a clinical interview to confirm the diagnosis. The inclusion criteria included being female, having at least a middle school education, age between 20 and 45 years, and not using medication for one month before starting treatment. The exclusion criteria included having any physical or viral illnesses, neurological disorders like epilepsy, and a history of head trauma. After meeting the criteria and scoring a minimum of 16 on the Yale-Brown obsessive-compulsive scale, 60 participants were selected via convenience sampling and randomly assigned to three experimental groups of 15 participants and one control group of 15 participants.
Research tools
Yale-Brown obsessive-compulsive scale
Goodman et al. (1989) introduced a scale with two subscales in 1989: Obsessive thoughts and compulsive behaviors. The severity of symptoms is assessed for the 7 days preceding the interview, with scores ranging from 0 (indicating “no problem”) to 4 (indicating “a very severe problem”). The scale’s reliability was evaluated using Cronbach’s α, and correlation coefficients were 0.97 for obsessive thoughts, 0.96 for compulsive behaviors, and 0.98 for the total scale. The correlation of each item with the total score was used to establish the scale’s validity, resulting in a range of 0.36 to 0.77. In Iran, inter-rater reliability of 0.98, internal consistency of 0.89, and test re-test reliability of 0.84 over a two-week interval were reported (Rajeziesfahani et al., 2016). In a more recent study by Shameli et al., (2017) the scale’s reliability was assessed using Cronbach’s α, generating coefficients of 0.62 for obsessive thoughts, 0.61 for compulsive behaviors, and 0.71 for the total scale.
Acceptance and action questionnaire-iI (AAQ-II) (Bond et al., 2011)
Bond et al. developed AAQ-II to measure psychological flexibility, particularly concerning experiential avoidance and the tendency to engage in actions despite unwanted thoughts and feelings. It consists of 7 items, rated on a 7-point Likert scale (never=1, very rarely=2, rarely=3, sometimes=4, often=5, almost always=6, always=7). Higher scores on this scale indicate lower psychological flexibility and higher experiential avoidance. Bond et al. reported a test re-test reliability of 0.81 and an internal consistency of 0.84 for this questionnaire (Bond et al., 2011). In Iran, Soltani et al. (2013) also reported a Cronbach’s α coefficient of 0.89 and a test re-test reliability of 0.71 for the second edition of the AAQ.
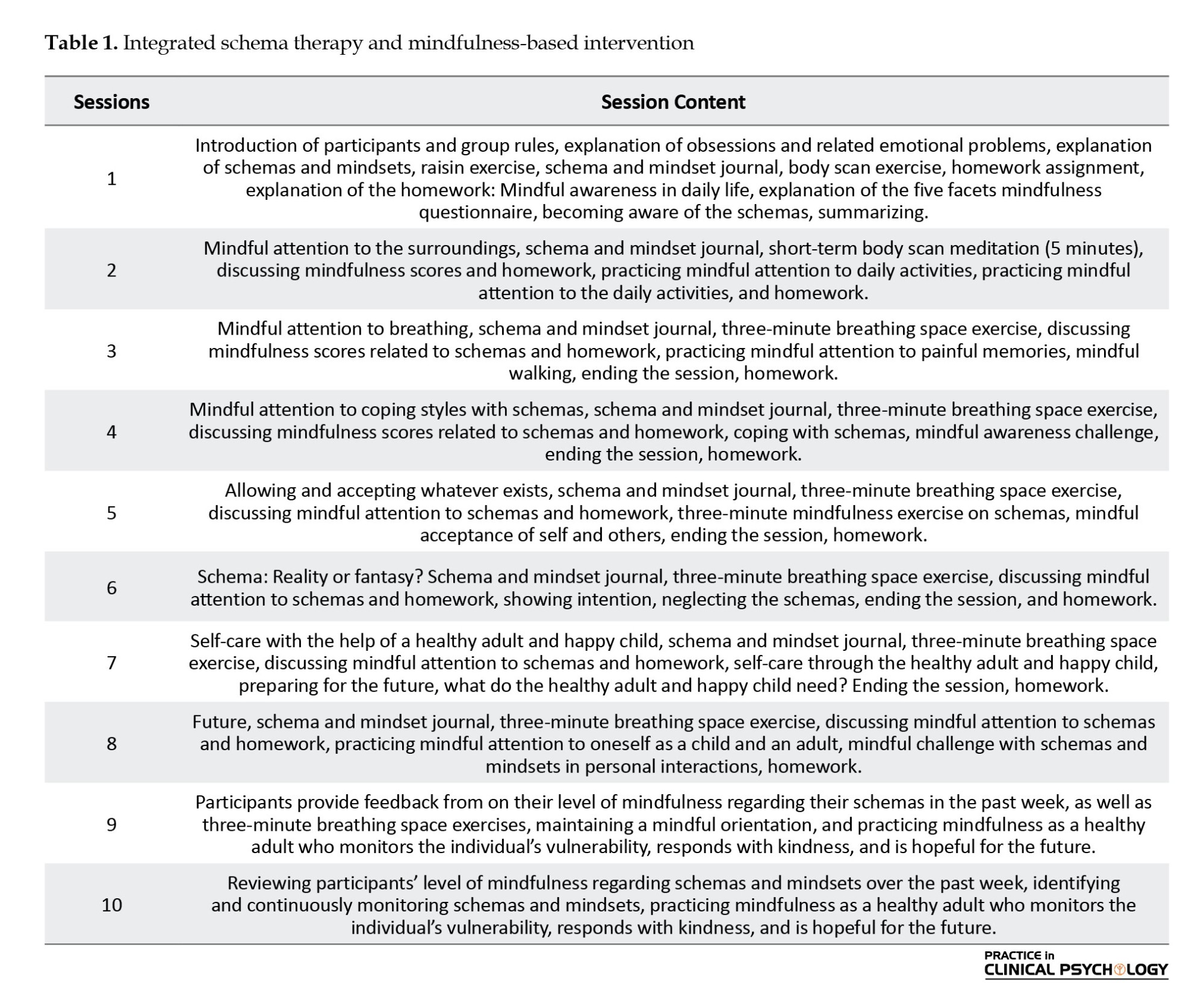
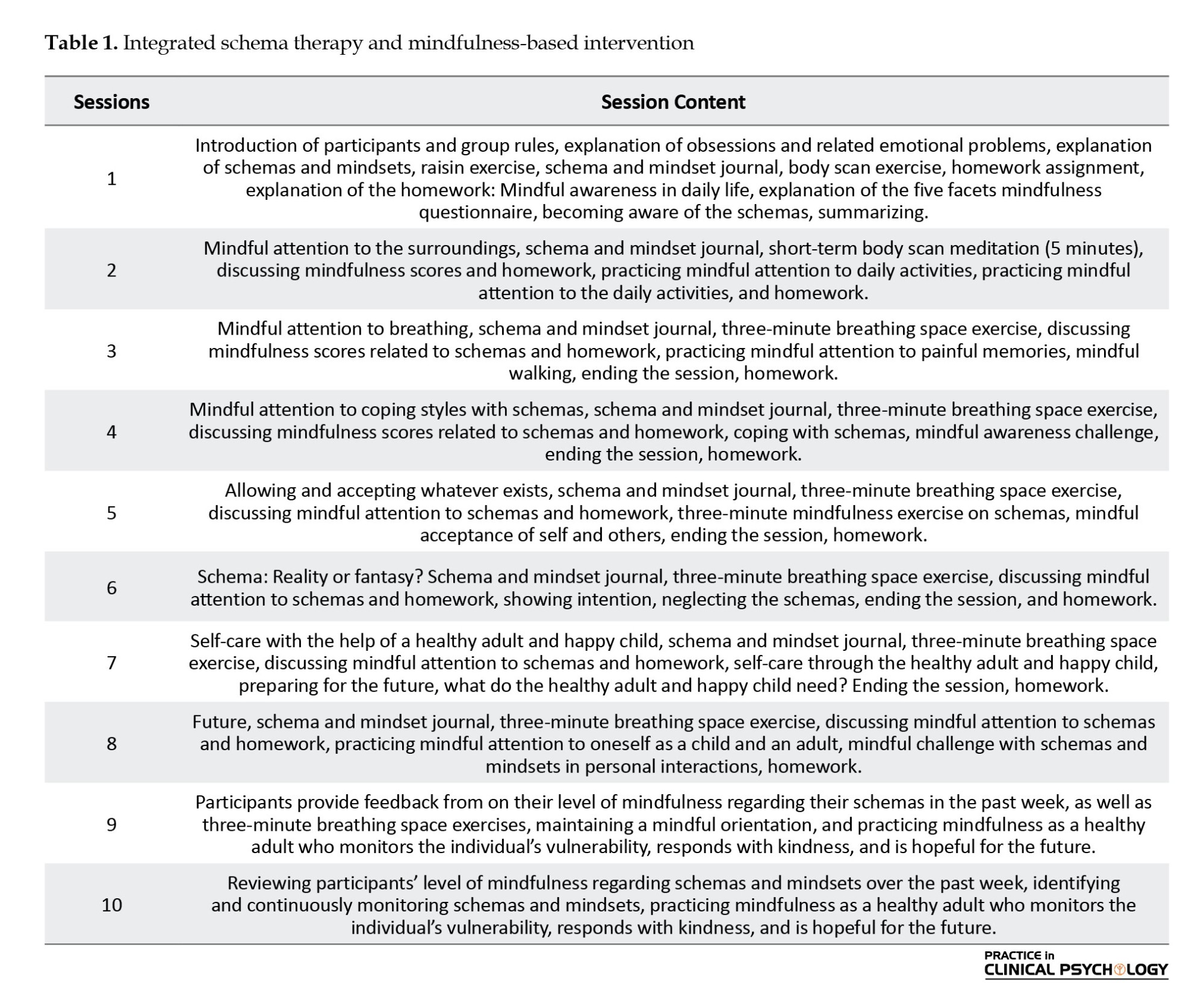
Description of the integrated schema therapy and mindfulness-based therapy intervention
The integrated model of schema-focused and mindfulness-based therapies involves the creation of a therapeutic program and package for teaching the integrated schema and mindfulness model. The researcher developed this program under the supervision of professors, utilizing theoretical and research backgrounds, as well as concepts from the schema and mindfulness approach described by Vreeswijk et al. (2014) The program was delivered over ten sessions, each lasting 90 minutes once a week. Raftar et al. (2020) confirmed the efficacy of integrated schema therapy and mindfulness-based intervention on depression, anxiety, and desperation, thus establishing its credibility for use (Table 1).
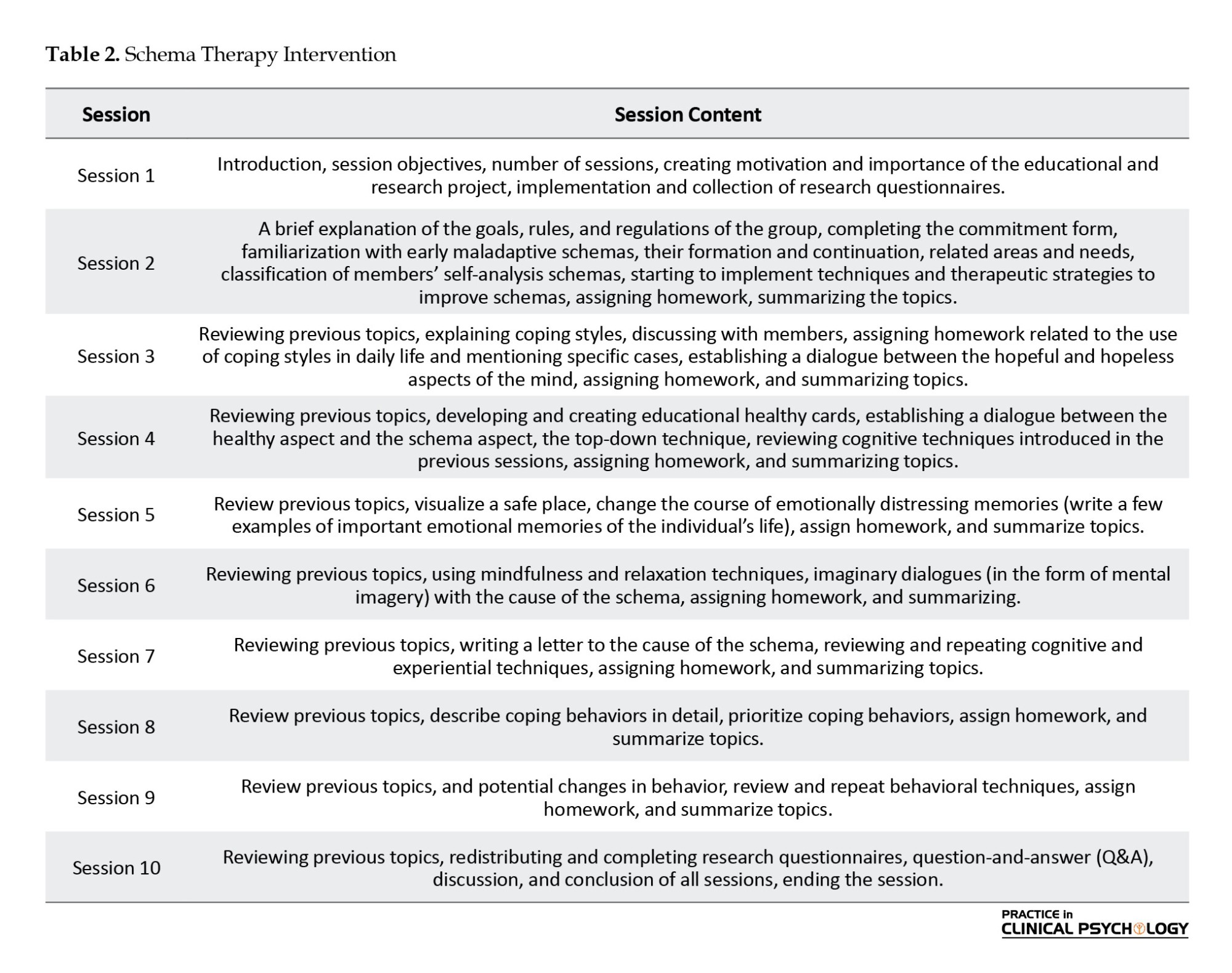
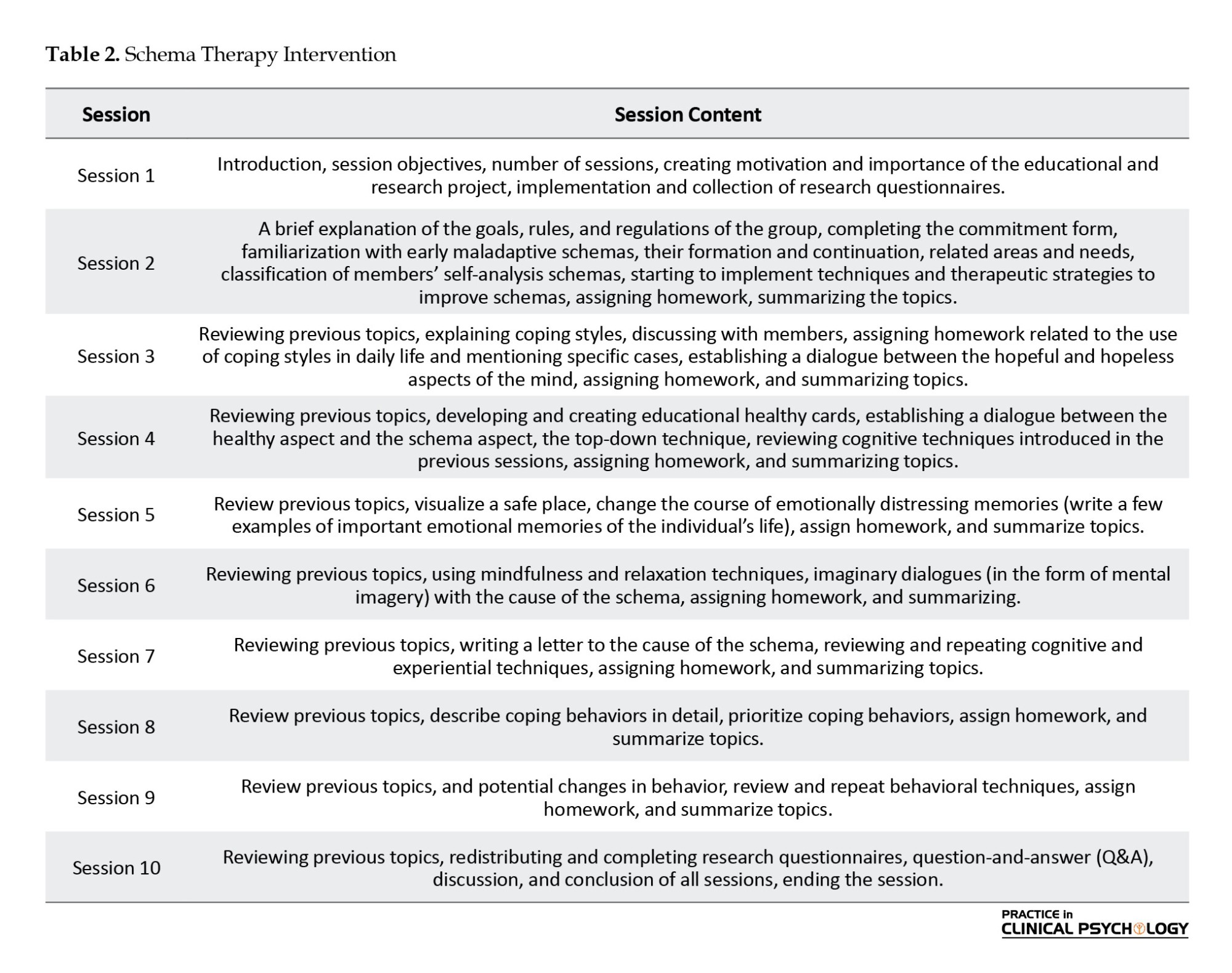
Description of schema therapy training sessions Schema therapy was implemented in a group format based on Young’s model for all participants in the experimental group during therapy sessions (Young, 1950). After conducting a pre-test in both groups, the experimental group received therapeutic intervention for ten sessions, once a week, for 90 minutes per session, while the control group did not receive any treatment. A post-test was conducted one week after the end of treatment for both the experimental and control groups. A specialist in therapeutic and counseling centers conducted this therapy. In the study conducted by Baniaadam et al. (2017), the efficacy of schema therapy in treating OCD was confirmed, thus establishing its credibility for use (Table 2).
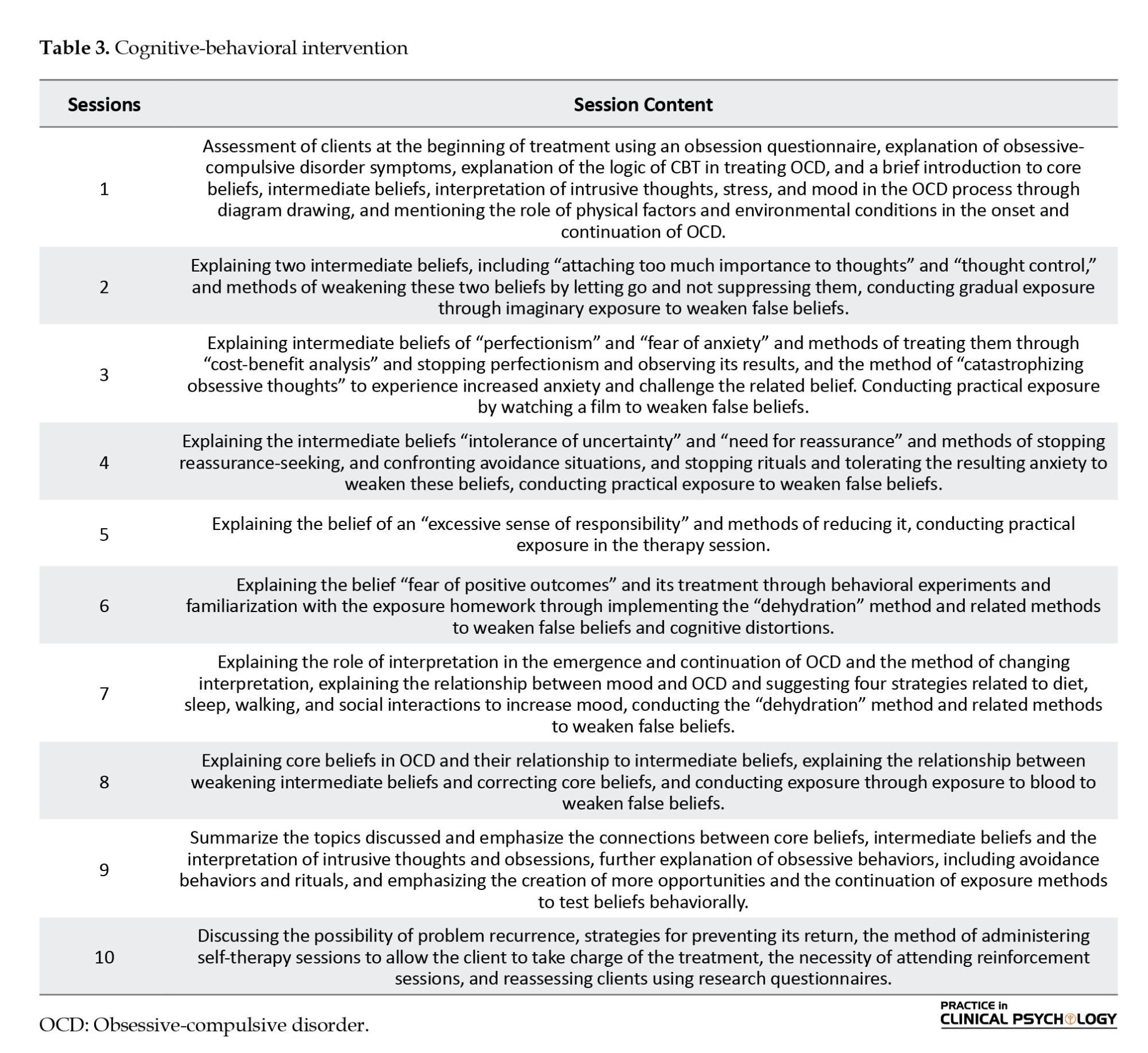
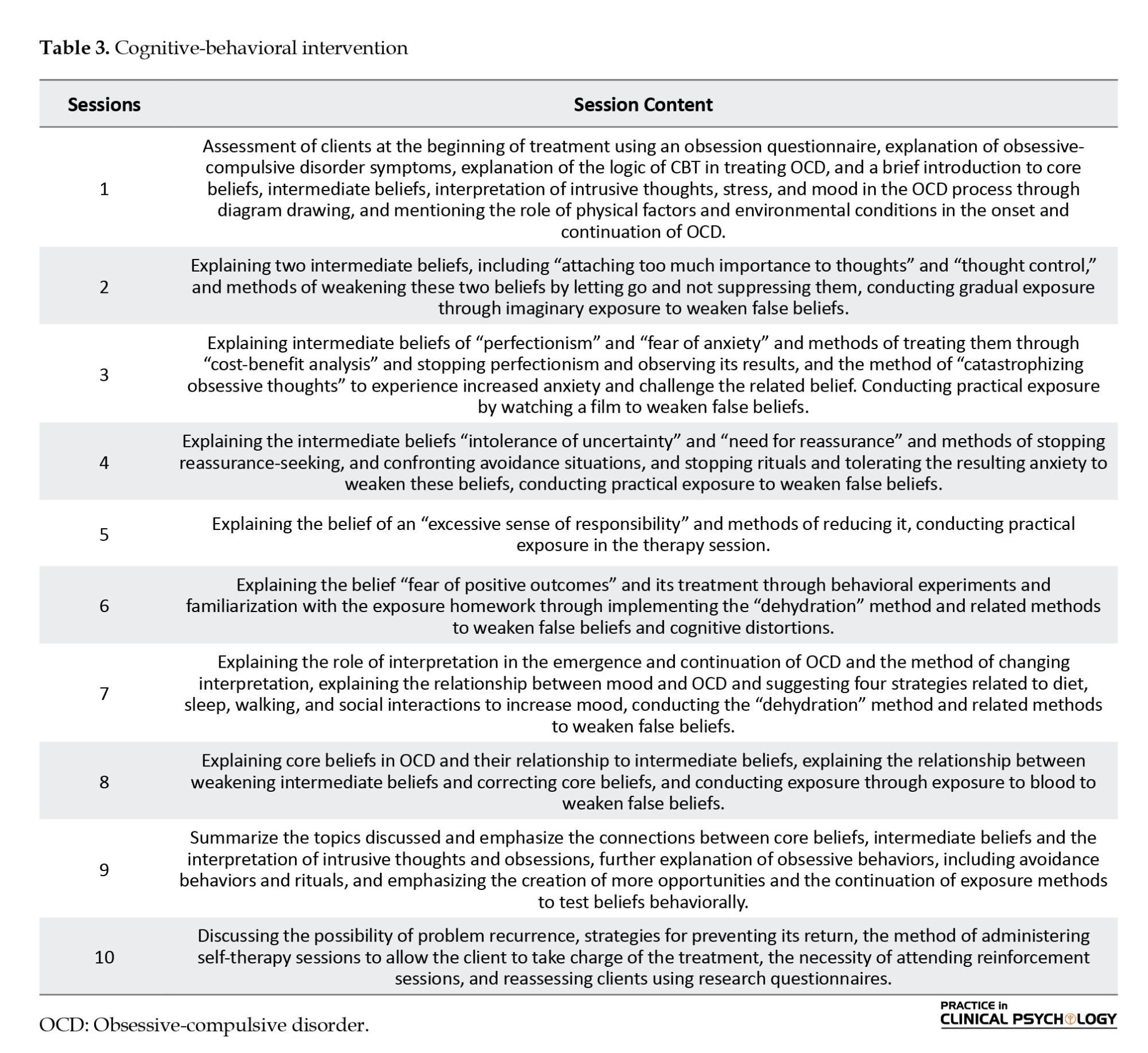
Description of CBT sessions
In this study, Meichenbaum’s protocolwas used to conduct CBT intervention, which was implemented in the experimental group once a week for 10 sessions of 90 minutes each. The validity of these sessions has been confirmed in the research of Parseh et al. (2015), Seyed Nour and Homaei (2019) and Epstein and Dattilio (2020). A repeated measures analysis of variance was used in a three-step pre-test, post-test, and follow-up design to analyze the data (Table 3).
Results
Table 4 presents descriptive statistics (Mean±SD) of psychological flexibility scores for the experimental groups (treatments based on the integrated schema therapy and mindfulness-based intervention, schema therapy, and cognitive-behavioral intervention) and the control group at the pre-test, post-test, and follow-up stages.
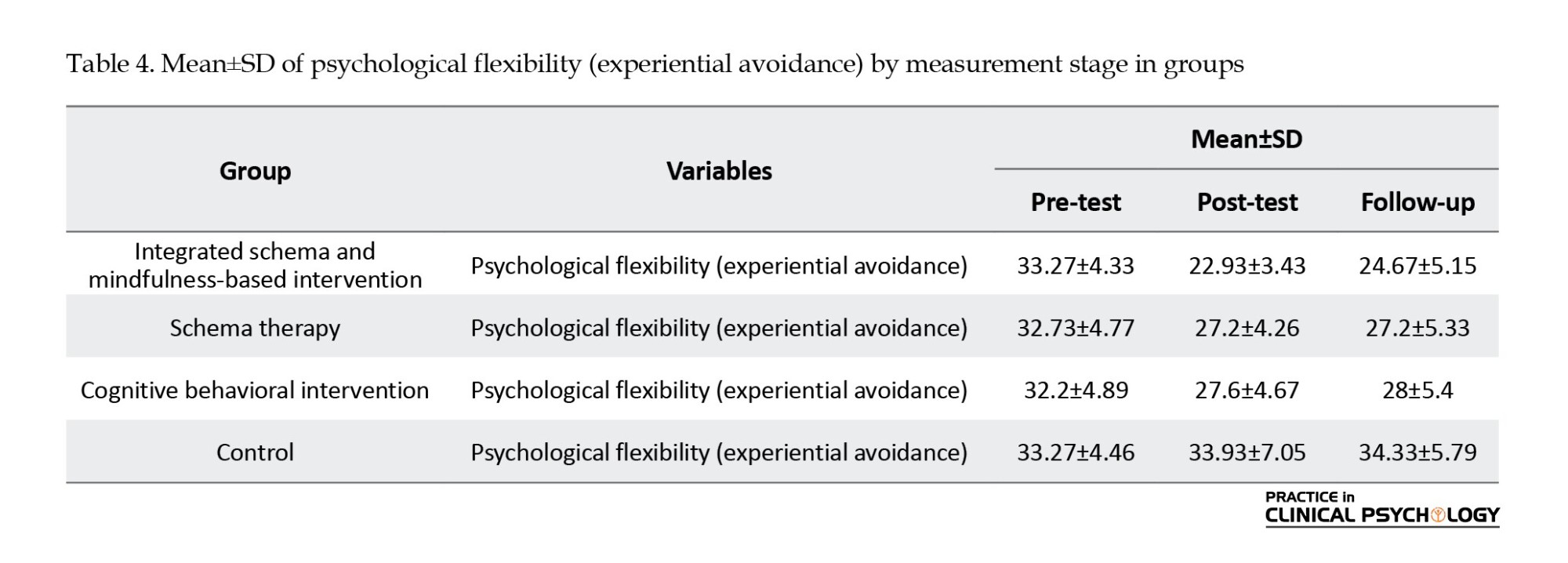
As can be seen, the mean scores for the integrated schema and mindfulness-based intervention, schema therapy, and cognitive-behavioral intervention groups decreased from the pre-test to the post-test. Based on the results presented in the Table 4, it can be concluded that the integrated schema and mindfulness-based intervention, schema therapy, and cognitive-behavioral intervention treatments decreased the psychological flexibility (experiential avoidance) among women with obsessive-compulsive symptoms.
Table 5 results indicated a significant within-subjects effect of time (pre-test, post-test, follow-up) on psychological flexibility (experiential avoidance) scores (P<0.05). Post-hoc Bonferroni tests revealed that mean psychological flexibility scores were significantly higher at post-test and follow-up than pre-test. However, no significant difference was observed between the post-test and follow-up scores, suggesting that the improved psychological flexibility observed after the intervention was maintained at the follow-up assessment.
Table 5 results indicated a significant interaction effect between time (pre-test, post-test, follow-up) and group (integrated schema therapy and mindfulness, schema therapy, cognitive-behavioral intervention, control) on psychological flexibility (experiential avoidance) scores (P<0.05). This issue suggests that the pattern of change in psychological flexibility over time differed across the four groups.
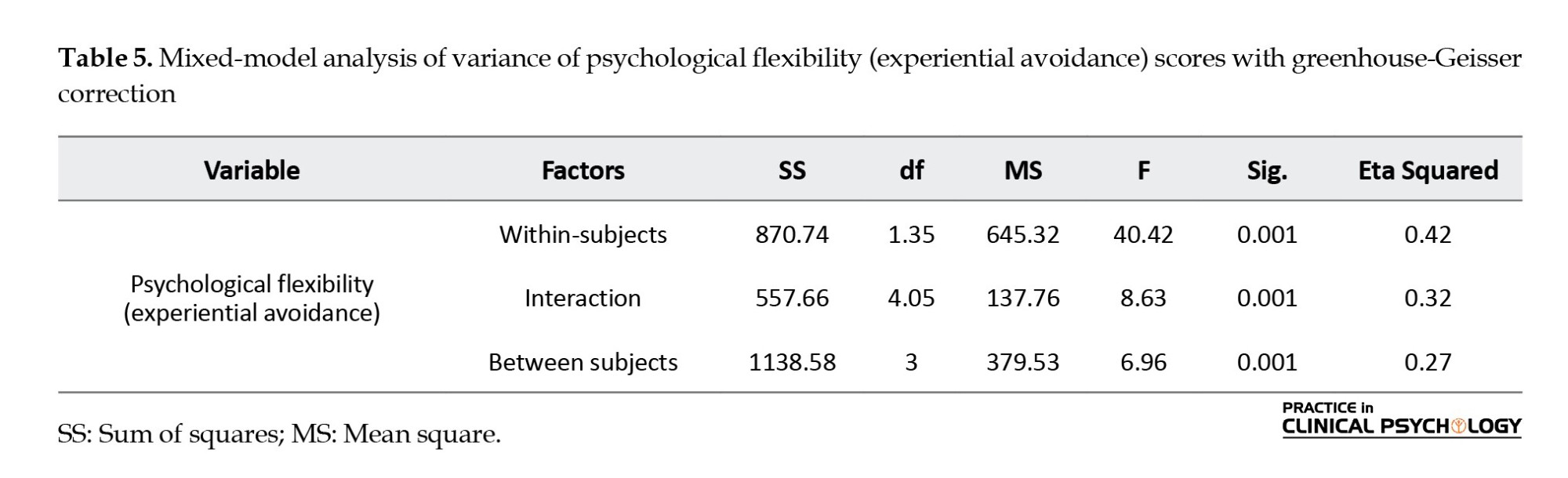
Results from Table 5 indicated a significant between-groups effect on psychological flexibility (experiential avoidance) scores (P<0.05). This issue suggests significant differences in mean psychological flexibility scores among the four intervention groups:
Integrated schema therapy and mindfulness, schema therapy, cognitive-behavioral intervention, and control. Post-hoc Tukey tests were conducted to further explore these differences. Table 6 presents the results of these tests.
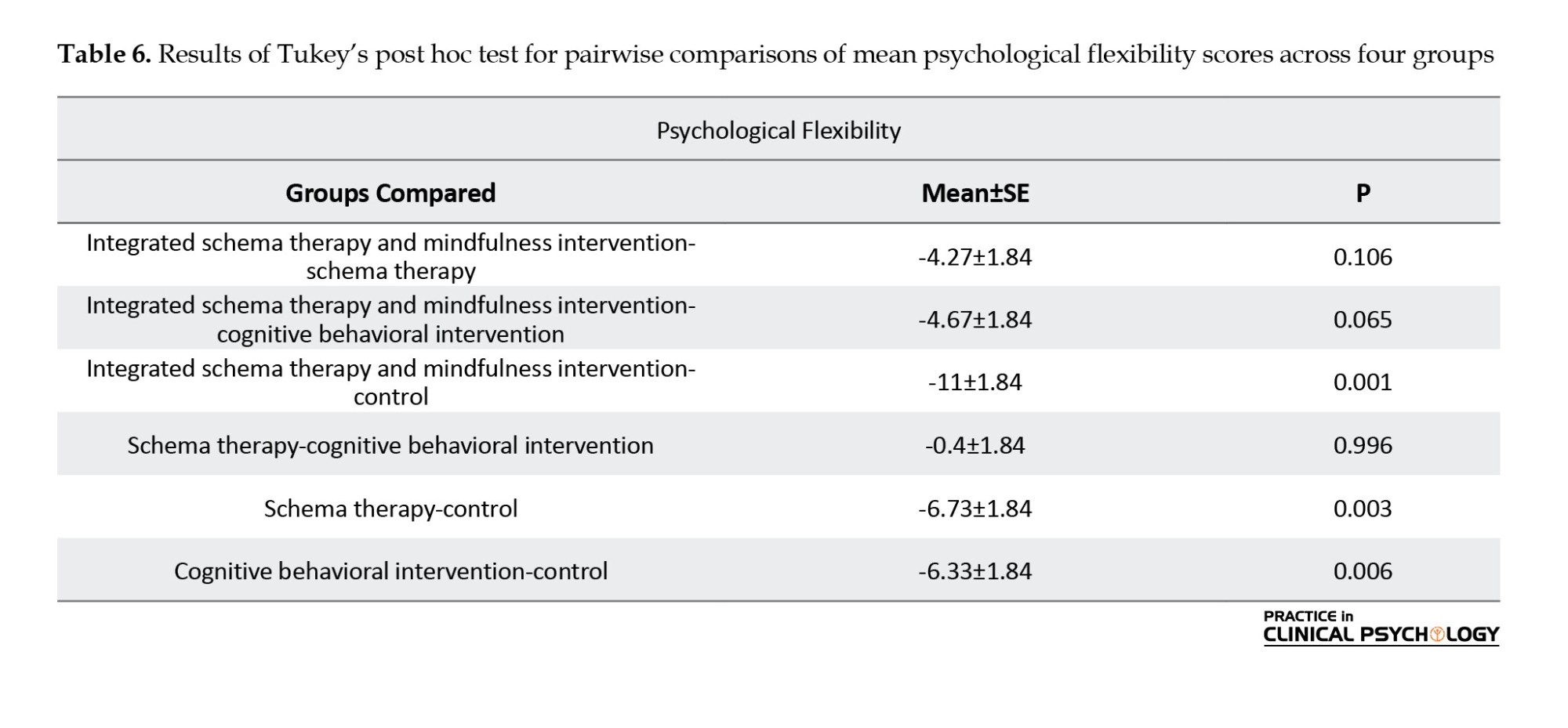
Table 6 results indicated that all interventions (integrated schema therapy and mindfulness, schema therapy, and cognitive behavioral intervention) significantly increased psychological flexibility scores compared to the control group (P<0.05). However, pairwise comparisons revealed a significant difference only between the integrated schema therapy and mindfulness group and the control group, suggesting that integrated schema therapy and mindfulness was the most effective intervention.
Discussion
The present study was conducted to compare the efficacy of integrated schema therapy and mindfulness intervention, schema therapy, and cognitive behavioral intervention on psychological flexibility in women with obsessive-compulsive symptoms. Results indicated a significant difference in mean levels of psychological flexibility (experiential avoidance) among the four groups: integrated schema therapy and mindfulness intervention, schema therapy, the control group, and cognitive behavioral intervention. Furthermore, the results indicated that the interventions (integrated schema therapy and mindfulness, schema therapy, and cognitive behavioral intervention) significantly impacted psychological flexibility scores compared to the control group. These results are consistent with previous research by Peeters et al. (2022), Mathur et al. (2021), Sunde et al. (2019) and Luppino et al. (2018).
The ultimate goal of schema therapy, as articulated in the literature, is to modify maladaptive schemas. As Beck points out, altering the structure and content of maladaptive schemas is crucial to prevent the recurrence of anxiety symptoms. Each skill-based component of schema therapy contributes to this therapeutic objective. Schema therapists believe that the therapeutic relationship is an essential component in assessing and modifying schemas but is not the primary agent of alteration; instead, it is a tool that facilitates it (Renner et al., 2018). Other influential factors in the schema modification process include cognitive, experiential-behavioral, and interpersonal strategies.
Cognitive techniques, such as challenging the validity of schemas and employing techniques, such as redefining schemas supporting evidence, engaging in internal dialogues between the healthy and schema aspects, and developing educational cards, enhance the awareness of patients with obsessive-compulsive symptoms regarding the inaccuracy of their schemas. This issue enables patients to break free from maladaptive cognitive processes and develop more effective cognitive and emotional processing, enhancing their psychological flexibility (Nasiri et al., 2022). On the other side, schema therapy-based skills support the improvement of cognitive and psychological functioning (Aslan and Türk, 2022). Consequently, participants acquire skills during treatment that enable them to disengage from ruminative thought patterns and reduce mental fatigue. Furthermore, due to the transformative nature of mindfulness techniques, research participants develop protection against future stressors, anxiety, and intrusive thoughts. These changes collectively contribute to enhance their psychological flexibility (Arslan, 2023).
Furthermore, mindfulness-based schema therapy can be explained in the following way: By increasing individuals’ awareness of the present moment through techniques, such as focusing on breath and body sensations and directing attention to the here and now, the cognitive system and information processing are influenced (Zareei et al., 2024). This issue leads to reduced rumination and maladaptive cognitions. Additionally, individuals become aware of their extraneous thoughts and are redirected toward other aspects of the present moment, such as breath, mindful walking, or environmental sounds. This process enhances psychological flexibility (Zareei et al., 2024). Furthermore, part of the problem of inflexibility and negative affect in OCD patients lies in factors, such as a lack of mindfulness in the present moment; enhancing mindfulness is a crucial step in preventing self-criticism and increasing positive affect.
Increasing attention and awareness of thoughts, emotions, and behavioral urges is a positive aspect of mindfulness (Gu et al., 2018). It leads to the alignment of adaptive behaviors and positive psychological states. This issue improves an individual’s ability to engage in solitary and social activities and increases interest in these activities (Mardpour & Hadizadeh Kaffash, 2017). These factors, in turn, can reduce OCD symptoms and increase positive emotions and psychological characteristics. In addition to schema therapy based on mindfulness, mindfulness exercises, and techniques are designed to help clients increase awareness and change challenging situations, including negative states and emotions, without automatic and habitual reactions (Mardpour & Hadizadeh Kaffash, 2017).
After receiving schema therapy based on mindfulness, individuals perceive cognitive experiences as separate entities from themselves, as transient states, and as subjects for change. Rather than exploring or avoiding these experiences cognitively or behaviorally, both of which can be painful, they accept and ultimately internalize them as other neutral or emotionally neutral cognitive experiences (Ghazanfari & Sepahvand, 2014).
On the other hand, the results of this study indicate the efficacy of CBT in increasing psychological flexibility among women with obsessive-compulsive symptoms. This result is consistent with previous research by Past et al. (2016), Tomiyama et al., (2019), Sahin et al. (2018), and Rosa-Alcazar et al. (2021). It can be argued that individuals with obsessive-compulsive symptoms often experience difficulties due to their inability to adapt to various situations to explain the efficacy of CBT in this context, leading to reduced psychological flexibility (Morris et al., 2018).
CBT aims to enhance individuals’ cognitive abilities by identifying and addressing deficits in executive functioning (Past et al., 2016). Psychological flexibility, a metacognitive concept encompassing interpersonal and intrapersonal skills, is closely linked to resilience and is considered a crucial factor in mental health (Tomiyama et al., 2019). Psychological flexibility enables individuals to adapt to situational changes, reshape mental resources, shift perspectives, and balance competing demands, needs, and life circumstances (Abramowitz & Reuman, 2020). In other words, psychological flexibility emphasizes cultivating a different relationship with one’s psychological experiences (e.g. thoughts, feelings, and bodily sensations), rather than attempting to change the content or intensity of those experiences themselves.
Individuals with high psychological flexibility strive to employ strategies that minimize harm when confronted with challenges and problems (Sahin et al., 2018). Individuals with OCD also exhibit reduced cognitive flexibility due to deficits in executive functions (Rosa-Alcazar et al., 2021). In line with this, Sahin et al. (2018) investigated cognitive flexibility in patients with OCD. In their study, 50 OCD patients and 30 panic disorder patients were included. The results indicated lower cognitive flexibility in OCD patients compared to those with panic disorder.
Conclusion
The need for significant differences between integrated schema therapy and mindfulness therapies, schema therapy, and CBT can be attributed to several factors. Each of these approaches shares the common objective of enhancing psychological flexibility. Essentially, they all work to help identify and modify thought and behavior patterns, which likely results in similar improvements in psychological flexibility scores. Moreover, minor variations in implementation methods or the characteristics of the studied samples may have contributed to the absence of significant differences in the outcomes. Additionally, the duration of treatment and frequency of sessions also influence these results, especially if these factors were consistent across all three groups. In summary, these findings indicate that while these therapies positively impacts psychological flexibility, they may also exhibit comparable efficacy in specific domains.
A major limitation of this study pertains to its external validity. Given that the study population was restricted to women with obsessive-compulsive symptoms residing in Tehran City, generalizing the results to the broader population is limited. Additionally, data collection in this study relied on self-report measures. Therefore, another limitation concerns measurement because the self-reported responses and perceptions of these subjects may not accurately reflect their actual behaviors and experiences. It is recommended that future research be expanded to examine additional disorders and that the outcomes of these studies be thoroughly evaluated. Furthermore, using interviews instead of self-report instruments is advised to enhance data collection in subsequent research efforts. Mindfulness-based schema therapy can assist women with obsessive-compulsive symptoms in acquiring skills to manage their obsessions. For instance, meditation and mindfulness practices can contribute to reduce obsessive thoughts. Cognitive-based exercises, such as identifying and challenging obsessive thoughts, can also be beneficial. Given the efficacy of this therapeutic approach, it is recommended that this treatment be implemented in existing therapeutic centers nationwide to alleviate the suffering caused by trauma and crises.
Ethical Considerations
Compliance with ethical guidelines
All procedures were approved by the Committee for Ethical Considerations in Human Experimentation of Islamic Azad University of Isfahan (Khorasgan) Branch. This study was registered by the Iranian Registry of Clinical Trials (IRCT). Parents signed written informed consent before the study, and all children orally expressed their assent.
Funding
This research received no grant from public, commercial, or non-profit funding agencies.
Authors' contributions
Conceptualization and supervision: Seyed Hamid Atashpour and Mohsen Golparvar; Methodology and analysis: Seyed Hamid Atashpour and Pouyan Ahanian Moghaddam; Data collection: Pouyan Ahanian Moghaddam; Investigation and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers thank the patients and all the people who helped them in conducting this research.
References
Throughout the general population, obsessive-compulsive disorder (OCD) has an estimated lifetime prevalence ranging from 2.3% to 8.3%, which is projected to increase to 15% by 2026 (Hermida-Barros et al., 2024). In recent years, extensive studies have been conducted in the etiology and treatment of psychological disorders, resulting in the identifica-tion of over 580 different treatment models. Certain disorders, such as depression, anxiety, and obsession, have higher prevalence rates and lead to more significant functional impairments. As a result, they have attracted considerable attention from researchers (Ponzini & Steinman, 2021). OCD, in particular, can significantly impact women and lead to severe functional impairments, warranting a focused approach involving screening and early diagnosis to mitigate its negative consequences (Caudek et al., 2020).
Individuals with OCD experience difficulties in various domains, including psychological flexibility (Bhatt, 2024). Consequently, OCD has garnered significant attention from re-searchers in the fields of etiology and treatment. The disorder is time-consuming for affected individuals and can impair various aspects of their lives, such as occupational func-tioning, interpersonal relationships, and academic performance. Moreover, its severity often increases over time, necessitating specialized therapeutic interventions (Leeuwerik et al., 2020).
Individuals with OCD often struggle with various aspects of executive functioning, including psychological flexibility, response inhibition, visual and verbal memory, and emotional processing (Wheaton et al., 2021). Psychological flexibility, a key component of executive functioning, refers to the ability to adapt effectively to changing demands (Darby et al., 2018). Those with high psychological flexibility can assess new problems and situations from various angles and develop with innovative alternative options and ideas. In contrast, people with lower psychological flexibility find it challenging to let go of their initial learning and tend to persist in their original beliefs, with negative consequences (Deveci et al., 2024). This rigidity hampers their ability to adapt to new circumstances and increases their vulnerability to anxiety (Hayes et al., 2004).
Individuals with OCD often experience decreased psychological flexibility. This limitation contributes to rigid and repetitive thoughts and behaviors, hindering their ability to adapt to changes (Caudek et al., 2020). Research demonstrates that people with OCD symptoms exhibit lower levels of psychological flexibility (Francazio & Felssner, 2015; Graner & Pittenger, 2017; Feinberg et al., 2015). A study conducted by Izadi et al. (2014) revealed that participants with OCD who engaged in interventions designed to enhance flexibility and reduce experiential avoidance reported fewer symptoms compared to their peers. Similarly, Den Ouden, et al. (2020) found that individuals with OCD tend to exhibit less flexibility, rely more on avoidance strategies, and display increased obsessive symptoms. Furthermore, research by Sanaei Moharrer and Mirshekari (2017) affirmed the relationship between psychological flexibility and anxiety in the development and persistence of obsessive-compulsive symptoms.
Research suggests that individuals with obsessive-compulsive symptoms exhibit lower levels of psychological flexibility (Francazio & Felssner, 2015; Gruner & Pittenger, 2017; Fineberg et al., 2015; Caudek et al., 2020). Consistent with these results, a study conducted by Izadi et al. (2014) revealed that individuals with OCD who received interventions to en-hance flexibility and reduce experiential avoidance reported fewer symptoms compared to those who did not. Den Ouden, et al. (2020) also found in a similar study that these individuals displayed lower psychological flexibility, utilized more avoidance-based coping strategies, and manifested more obsessive symptoms. Additionally, Sanaei Moharrer and Mirshe-kari (2017) affirmed the role of psychological flexibility and anxiety in the development and persistence of symptoms associated with OCD.
People with OCD often encounter obsessive symptoms and struggle with psychological flexibility, prompting counselors and researchers to explore various therapeutic approaches to help them. Recent third-wave cognitive-behavioral therapies, such as schema therapy and mindfulness-based therapy, have been specifically tailored to address the needs of individuals with OCD. Schema therapy, developed by Young et al. (2003), is an innovative and integrative therapeutic model in the realm of cognitive therapy. It has garnered significant attention as an effective treatment for various anxiety disorders, particularly OCD. Schema therapy is recommended for patients who have not responded well to traditional cog-nitive-behavioral therapy. It has a particular emphasis on the developmental roots of psychological disorders, underlying patterns in psychological and social functioning, and maladaptive cognitions and behaviors of patients. From a schema therapeutic perspective, maladaptive schemas in individuals are activated by threatening and critical life events, leading to increased emotions such as anxiety, sadness, and anger. Schema therapy primarily focuses on reducing obsessive thoughts and behaviors by addressing under-lying maladaptive schemas, rather than directly confronting individuals with their fears. Sunde et al. (2019) concluded that schema therapy effectively reduced the symptoms of OCD in patients.
In addition to schema therapy, mindfulness-based therapy has emerged as a relatively contemporary approach utilized for individuals with OCD. Mindfulness practices enable patients to acknowledge their distressing thoughts without attempting to suppress them. Moreover, mindfulness fosters the development of awareness and acceptance of both internal and external experiences without passing judgment. Specifically tailored for OCD, mindfulness training assists patients in acknowledging their thoughts, feelings, and bodily sensations without automatically reacting. This form of therapy enhances self-awareness and non-judgment, thus preventing patients from engaging in negative evalua-tions, judgments, and biases (Reis et al., 2024).
Empirical results demonstrate the efficacy of mindfulness-based therapy in decreasing rumination, perfectionism, and thought-action fusion in women diagnosed with OCD (Khadem et al., 2023). Additionally, research supports the effectiveness of mindfulness intervention in reducing symptoms, such as obsessive checking, washing, slowing/repeating, and doubting (Mardpour & Hadizadeh Kaffash, 2017). Furthermore, mindfulness-based stress reduction techniques have shown promise in reducing obses-sive-compulsive symptoms (Ghazanfari & Sepahvand, 2014). Chien et al. (2022) researched the effectiveness of mindfulness-based interventions for individuals with OCD and found that these interventions were highly effective. Similarly, Mathur et al. (2021) reported comparable results, highlighting the success of mindfulness therapy in managing stress among patients with OCD.
Mindfulness-based therapies represent a more recent generation of cognitive-behavioral treatments characterized by differing therapeutic emphases and processes while also sharing fundamental similarities with their predecessors (Abramowitz & Reuman, 2020). CBT, identified as one of the most effective interventions for OCD, instructs patients to observe their thoughts from a broader perspective and cultivate a decentered relationship with the contents of their mind (Görmezoğlu et al., 2020). This approach emphasizes the development of the freedom to understand that most thoughts are merely thoughts, not facts or realities (Huang et al., 2023), often leading to enhanced insight and an increased sense of control over their lives (Hoppen et al., 2021). In this regard, research conducted by Cervin et al. (2024) revealed that cognitive flexibility and cognitive behavioral therapy (CBT) are interconnected and substantially influence the treatment process for patients. Onaral (2021) conducted a study examining the efficacy of third-wave therapies in the treatment of OCD. The results demonstrated that two primary treatment methods, medication and cognitive behavioral therapy, are effective in managing OCD. However, the high rates of patient drop-out and the persistence of residual symptoms following CBT have led researchers to seek alternative treatment approaches. Consequently, recent developments suggest that third-wave therapies hold significant promise in addressing these challenges.
In this study, the researcher compares the effectiveness of two intervention strategies, the combination of schema therapy and mindfulness, and schema therapy paired with CBT. The objective is to gain a deeper understanding of how these different approaches influence psychological flexibility in women diagnosed with OCD.
Schema therapy focuses on identifying and modifying deep-seated dysfunctional patterns often rooted in early life experiences. In contrast, mindfulness therapy encourages individuals to engage with their thoughts and feelings non-judgmentally and accepting. CBT, a widely recognized and effective method for treating various mental health disor-ders, emphasizes altering dysfunctional thoughts and behaviors.
By contrasting these three approaches, the researcher aims to gather scientific evidence regarding the efficacy and effectiveness of each method. This study provides valuable insights into which approach, or combination thereof, can best enhance the psychological flexibility of women with OCD. Ultimately, the results may inform the development of more effective and tailored treatment strategies for this particular group of clients.
Moreover, a reciprocal relationship between cognitive flexibility and CBT has been established, indicating a significant impact on patient outcomes when these components are integrated (Cervin et al., 2024).
Indeed, by recognizing the symptoms of obsessions and compulsions, we emphasize the importance of treating individuals with this disorder to prevent them from suffering distressing symptoms throughout their lives. People with OCD often engage in frequent rumination, leading to compulsive behaviors. Furthermore, they place excessive im-portance on their thoughts, validating and perpetuating a cycle of obsessive thoughts and behaviors. While CBT is widely supported by evidence, existing methods have limitations, with limited response to conventional approaches based on CBT and serotonin reuptake inhibitors. On the other hand, schema-focused and mindfulness-based approaches aim to not only modify the course and clinical presentation of OCD but also transform the underlying functioning of the mind through cognitive training.
Research into integrated models combining schema therapy and mindfulness-based therapies, as well as the integration of schema therapy and CBT for obsessive-compulsive symptoms, is limited. Our study aims to investigate these integrated models and answer the question: Does the efficacy of integrated interventions of schema therapy and mindfulness-based therapy differ from that of schema therapy and CBT on the psychological flexibility of women with obsessive-compulsive symptoms?
Materials and Methods
The study was conducted using a quasi-experimental design with pre-test-post-test and control and follow-up groups. The participants were exclusively women diagnosed with OCD who had been referred to the Nedaye Agahayi and Zehne Poya Clinic in Tehran City during the fall and winter of 2021. Initial contact was made with counseling centers and psychotherapy clinics in District 5 of Tehran City to form the sample group. Additionally, a call for participation in group therapy was made in the same district. Interested participants messaged the word “obsession” to a provided mobile number and were subsequently contacted by the researcher. Eligible individuals underwent a clinical interview to confirm the diagnosis. The inclusion criteria included being female, having at least a middle school education, age between 20 and 45 years, and not using medication for one month before starting treatment. The exclusion criteria included having any physical or viral illnesses, neurological disorders like epilepsy, and a history of head trauma. After meeting the criteria and scoring a minimum of 16 on the Yale-Brown obsessive-compulsive scale, 60 participants were selected via convenience sampling and randomly assigned to three experimental groups of 15 participants and one control group of 15 participants.
Research tools
Yale-Brown obsessive-compulsive scale
Goodman et al. (1989) introduced a scale with two subscales in 1989: Obsessive thoughts and compulsive behaviors. The severity of symptoms is assessed for the 7 days preceding the interview, with scores ranging from 0 (indicating “no problem”) to 4 (indicating “a very severe problem”). The scale’s reliability was evaluated using Cronbach’s α, and correlation coefficients were 0.97 for obsessive thoughts, 0.96 for compulsive behaviors, and 0.98 for the total scale. The correlation of each item with the total score was used to establish the scale’s validity, resulting in a range of 0.36 to 0.77. In Iran, inter-rater reliability of 0.98, internal consistency of 0.89, and test re-test reliability of 0.84 over a two-week interval were reported (Rajeziesfahani et al., 2016). In a more recent study by Shameli et al., (2017) the scale’s reliability was assessed using Cronbach’s α, generating coefficients of 0.62 for obsessive thoughts, 0.61 for compulsive behaviors, and 0.71 for the total scale.
Acceptance and action questionnaire-iI (AAQ-II) (Bond et al., 2011)
Bond et al. developed AAQ-II to measure psychological flexibility, particularly concerning experiential avoidance and the tendency to engage in actions despite unwanted thoughts and feelings. It consists of 7 items, rated on a 7-point Likert scale (never=1, very rarely=2, rarely=3, sometimes=4, often=5, almost always=6, always=7). Higher scores on this scale indicate lower psychological flexibility and higher experiential avoidance. Bond et al. reported a test re-test reliability of 0.81 and an internal consistency of 0.84 for this questionnaire (Bond et al., 2011). In Iran, Soltani et al. (2013) also reported a Cronbach’s α coefficient of 0.89 and a test re-test reliability of 0.71 for the second edition of the AAQ.
Description of the integrated schema therapy and mindfulness-based therapy intervention
The integrated model of schema-focused and mindfulness-based therapies involves the creation of a therapeutic program and package for teaching the integrated schema and mindfulness model. The researcher developed this program under the supervision of professors, utilizing theoretical and research backgrounds, as well as concepts from the schema and mindfulness approach described by Vreeswijk et al. (2014) The program was delivered over ten sessions, each lasting 90 minutes once a week. Raftar et al. (2020) confirmed the efficacy of integrated schema therapy and mindfulness-based intervention on depression, anxiety, and desperation, thus establishing its credibility for use (Table 1).
Description of schema therapy training sessions Schema therapy was implemented in a group format based on Young’s model for all participants in the experimental group during therapy sessions (Young, 1950). After conducting a pre-test in both groups, the experimental group received therapeutic intervention for ten sessions, once a week, for 90 minutes per session, while the control group did not receive any treatment. A post-test was conducted one week after the end of treatment for both the experimental and control groups. A specialist in therapeutic and counseling centers conducted this therapy. In the study conducted by Baniaadam et al. (2017), the efficacy of schema therapy in treating OCD was confirmed, thus establishing its credibility for use (Table 2).
Description of CBT sessions
In this study, Meichenbaum’s protocolwas used to conduct CBT intervention, which was implemented in the experimental group once a week for 10 sessions of 90 minutes each. The validity of these sessions has been confirmed in the research of Parseh et al. (2015), Seyed Nour and Homaei (2019) and Epstein and Dattilio (2020). A repeated measures analysis of variance was used in a three-step pre-test, post-test, and follow-up design to analyze the data (Table 3).
Results
Table 4 presents descriptive statistics (Mean±SD) of psychological flexibility scores for the experimental groups (treatments based on the integrated schema therapy and mindfulness-based intervention, schema therapy, and cognitive-behavioral intervention) and the control group at the pre-test, post-test, and follow-up stages.
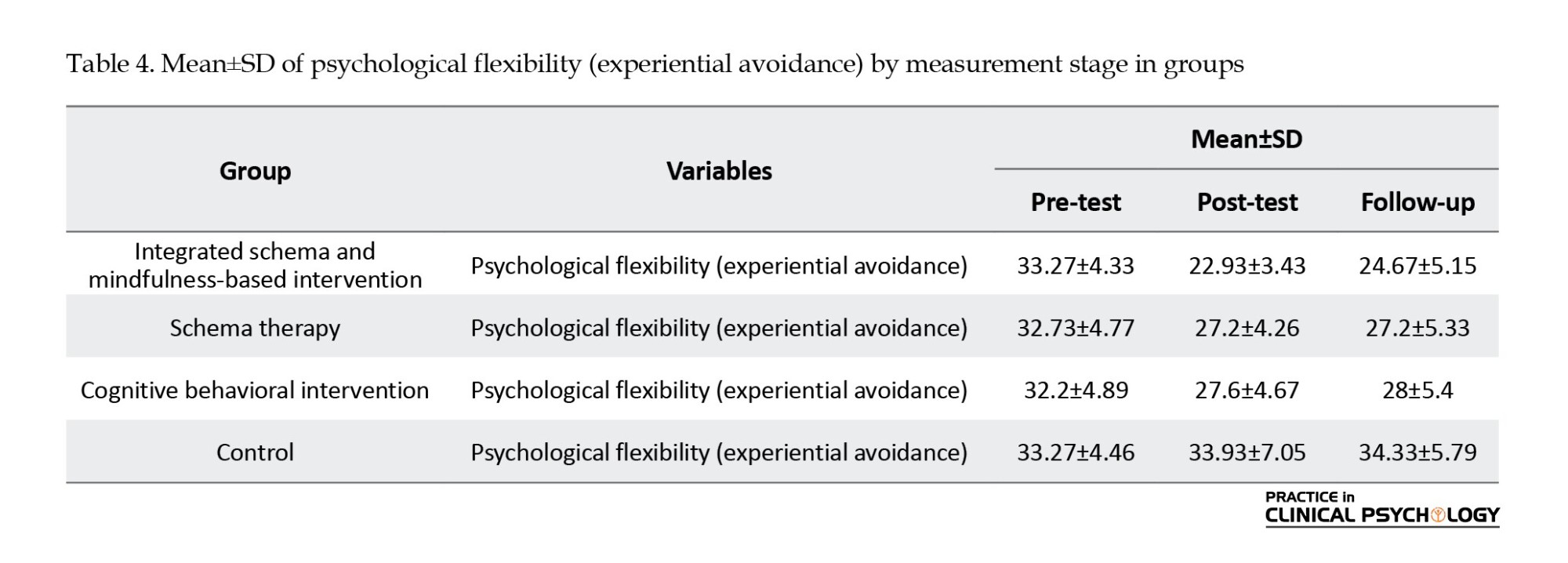
As can be seen, the mean scores for the integrated schema and mindfulness-based intervention, schema therapy, and cognitive-behavioral intervention groups decreased from the pre-test to the post-test. Based on the results presented in the Table 4, it can be concluded that the integrated schema and mindfulness-based intervention, schema therapy, and cognitive-behavioral intervention treatments decreased the psychological flexibility (experiential avoidance) among women with obsessive-compulsive symptoms.
Table 5 results indicated a significant within-subjects effect of time (pre-test, post-test, follow-up) on psychological flexibility (experiential avoidance) scores (P<0.05). Post-hoc Bonferroni tests revealed that mean psychological flexibility scores were significantly higher at post-test and follow-up than pre-test. However, no significant difference was observed between the post-test and follow-up scores, suggesting that the improved psychological flexibility observed after the intervention was maintained at the follow-up assessment.
Table 5 results indicated a significant interaction effect between time (pre-test, post-test, follow-up) and group (integrated schema therapy and mindfulness, schema therapy, cognitive-behavioral intervention, control) on psychological flexibility (experiential avoidance) scores (P<0.05). This issue suggests that the pattern of change in psychological flexibility over time differed across the four groups.
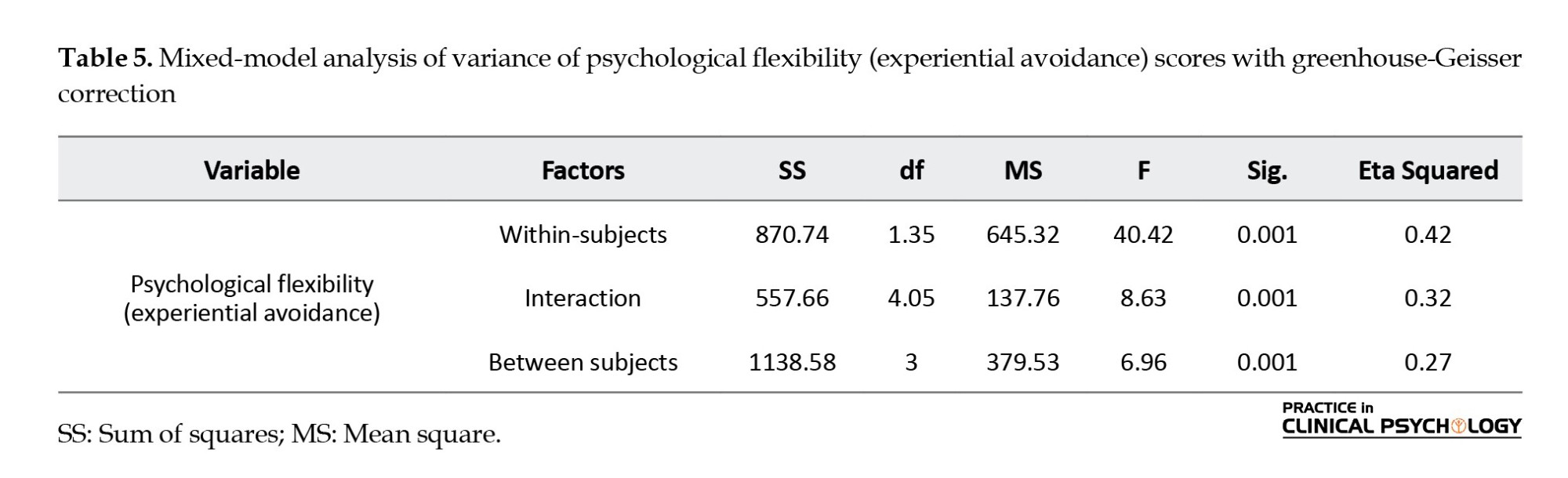
Results from Table 5 indicated a significant between-groups effect on psychological flexibility (experiential avoidance) scores (P<0.05). This issue suggests significant differences in mean psychological flexibility scores among the four intervention groups:
Integrated schema therapy and mindfulness, schema therapy, cognitive-behavioral intervention, and control. Post-hoc Tukey tests were conducted to further explore these differences. Table 6 presents the results of these tests.
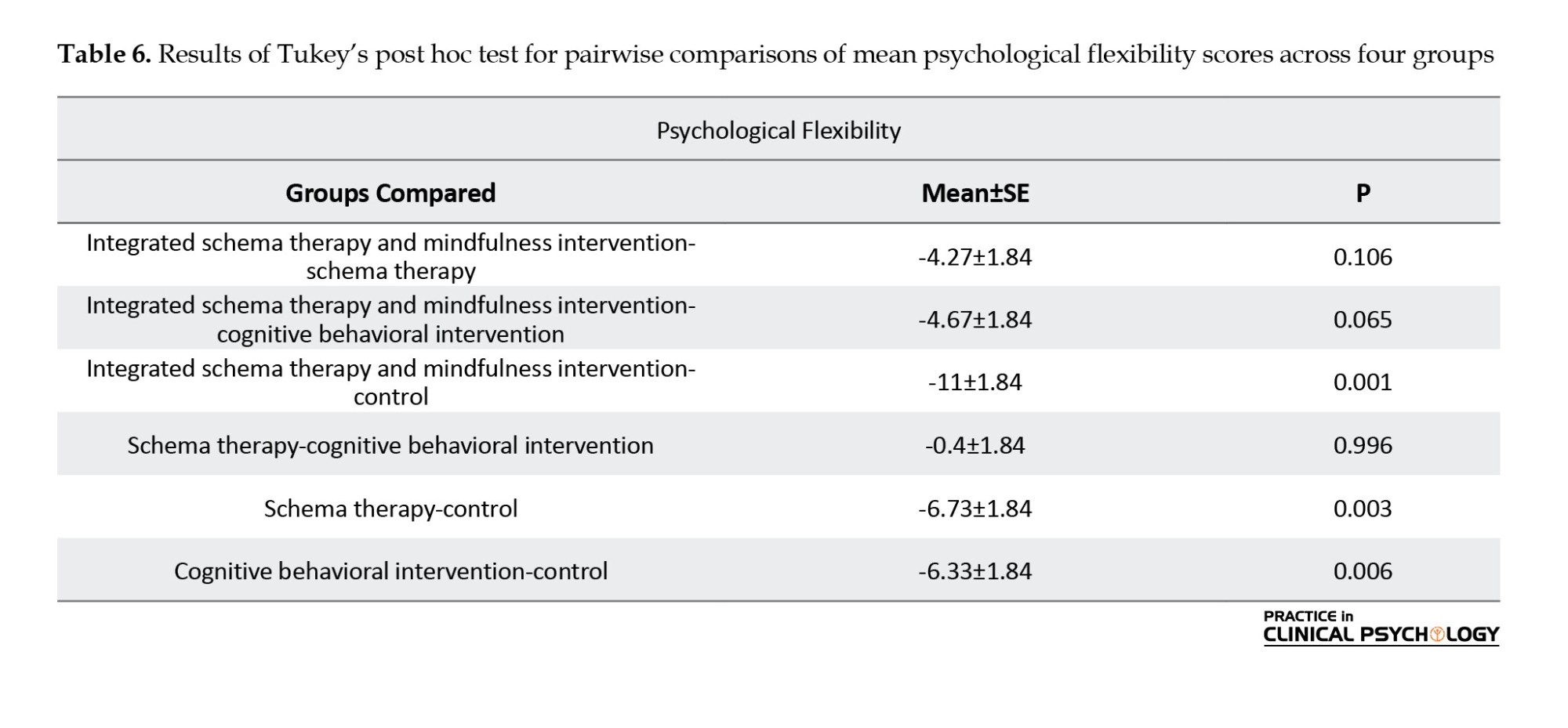
Table 6 results indicated that all interventions (integrated schema therapy and mindfulness, schema therapy, and cognitive behavioral intervention) significantly increased psychological flexibility scores compared to the control group (P<0.05). However, pairwise comparisons revealed a significant difference only between the integrated schema therapy and mindfulness group and the control group, suggesting that integrated schema therapy and mindfulness was the most effective intervention.
Discussion
The present study was conducted to compare the efficacy of integrated schema therapy and mindfulness intervention, schema therapy, and cognitive behavioral intervention on psychological flexibility in women with obsessive-compulsive symptoms. Results indicated a significant difference in mean levels of psychological flexibility (experiential avoidance) among the four groups: integrated schema therapy and mindfulness intervention, schema therapy, the control group, and cognitive behavioral intervention. Furthermore, the results indicated that the interventions (integrated schema therapy and mindfulness, schema therapy, and cognitive behavioral intervention) significantly impacted psychological flexibility scores compared to the control group. These results are consistent with previous research by Peeters et al. (2022), Mathur et al. (2021), Sunde et al. (2019) and Luppino et al. (2018).
The ultimate goal of schema therapy, as articulated in the literature, is to modify maladaptive schemas. As Beck points out, altering the structure and content of maladaptive schemas is crucial to prevent the recurrence of anxiety symptoms. Each skill-based component of schema therapy contributes to this therapeutic objective. Schema therapists believe that the therapeutic relationship is an essential component in assessing and modifying schemas but is not the primary agent of alteration; instead, it is a tool that facilitates it (Renner et al., 2018). Other influential factors in the schema modification process include cognitive, experiential-behavioral, and interpersonal strategies.
Cognitive techniques, such as challenging the validity of schemas and employing techniques, such as redefining schemas supporting evidence, engaging in internal dialogues between the healthy and schema aspects, and developing educational cards, enhance the awareness of patients with obsessive-compulsive symptoms regarding the inaccuracy of their schemas. This issue enables patients to break free from maladaptive cognitive processes and develop more effective cognitive and emotional processing, enhancing their psychological flexibility (Nasiri et al., 2022). On the other side, schema therapy-based skills support the improvement of cognitive and psychological functioning (Aslan and Türk, 2022). Consequently, participants acquire skills during treatment that enable them to disengage from ruminative thought patterns and reduce mental fatigue. Furthermore, due to the transformative nature of mindfulness techniques, research participants develop protection against future stressors, anxiety, and intrusive thoughts. These changes collectively contribute to enhance their psychological flexibility (Arslan, 2023).
Furthermore, mindfulness-based schema therapy can be explained in the following way: By increasing individuals’ awareness of the present moment through techniques, such as focusing on breath and body sensations and directing attention to the here and now, the cognitive system and information processing are influenced (Zareei et al., 2024). This issue leads to reduced rumination and maladaptive cognitions. Additionally, individuals become aware of their extraneous thoughts and are redirected toward other aspects of the present moment, such as breath, mindful walking, or environmental sounds. This process enhances psychological flexibility (Zareei et al., 2024). Furthermore, part of the problem of inflexibility and negative affect in OCD patients lies in factors, such as a lack of mindfulness in the present moment; enhancing mindfulness is a crucial step in preventing self-criticism and increasing positive affect.
Increasing attention and awareness of thoughts, emotions, and behavioral urges is a positive aspect of mindfulness (Gu et al., 2018). It leads to the alignment of adaptive behaviors and positive psychological states. This issue improves an individual’s ability to engage in solitary and social activities and increases interest in these activities (Mardpour & Hadizadeh Kaffash, 2017). These factors, in turn, can reduce OCD symptoms and increase positive emotions and psychological characteristics. In addition to schema therapy based on mindfulness, mindfulness exercises, and techniques are designed to help clients increase awareness and change challenging situations, including negative states and emotions, without automatic and habitual reactions (Mardpour & Hadizadeh Kaffash, 2017).
After receiving schema therapy based on mindfulness, individuals perceive cognitive experiences as separate entities from themselves, as transient states, and as subjects for change. Rather than exploring or avoiding these experiences cognitively or behaviorally, both of which can be painful, they accept and ultimately internalize them as other neutral or emotionally neutral cognitive experiences (Ghazanfari & Sepahvand, 2014).
On the other hand, the results of this study indicate the efficacy of CBT in increasing psychological flexibility among women with obsessive-compulsive symptoms. This result is consistent with previous research by Past et al. (2016), Tomiyama et al., (2019), Sahin et al. (2018), and Rosa-Alcazar et al. (2021). It can be argued that individuals with obsessive-compulsive symptoms often experience difficulties due to their inability to adapt to various situations to explain the efficacy of CBT in this context, leading to reduced psychological flexibility (Morris et al., 2018).
CBT aims to enhance individuals’ cognitive abilities by identifying and addressing deficits in executive functioning (Past et al., 2016). Psychological flexibility, a metacognitive concept encompassing interpersonal and intrapersonal skills, is closely linked to resilience and is considered a crucial factor in mental health (Tomiyama et al., 2019). Psychological flexibility enables individuals to adapt to situational changes, reshape mental resources, shift perspectives, and balance competing demands, needs, and life circumstances (Abramowitz & Reuman, 2020). In other words, psychological flexibility emphasizes cultivating a different relationship with one’s psychological experiences (e.g. thoughts, feelings, and bodily sensations), rather than attempting to change the content or intensity of those experiences themselves.
Individuals with high psychological flexibility strive to employ strategies that minimize harm when confronted with challenges and problems (Sahin et al., 2018). Individuals with OCD also exhibit reduced cognitive flexibility due to deficits in executive functions (Rosa-Alcazar et al., 2021). In line with this, Sahin et al. (2018) investigated cognitive flexibility in patients with OCD. In their study, 50 OCD patients and 30 panic disorder patients were included. The results indicated lower cognitive flexibility in OCD patients compared to those with panic disorder.
Conclusion
The need for significant differences between integrated schema therapy and mindfulness therapies, schema therapy, and CBT can be attributed to several factors. Each of these approaches shares the common objective of enhancing psychological flexibility. Essentially, they all work to help identify and modify thought and behavior patterns, which likely results in similar improvements in psychological flexibility scores. Moreover, minor variations in implementation methods or the characteristics of the studied samples may have contributed to the absence of significant differences in the outcomes. Additionally, the duration of treatment and frequency of sessions also influence these results, especially if these factors were consistent across all three groups. In summary, these findings indicate that while these therapies positively impacts psychological flexibility, they may also exhibit comparable efficacy in specific domains.
A major limitation of this study pertains to its external validity. Given that the study population was restricted to women with obsessive-compulsive symptoms residing in Tehran City, generalizing the results to the broader population is limited. Additionally, data collection in this study relied on self-report measures. Therefore, another limitation concerns measurement because the self-reported responses and perceptions of these subjects may not accurately reflect their actual behaviors and experiences. It is recommended that future research be expanded to examine additional disorders and that the outcomes of these studies be thoroughly evaluated. Furthermore, using interviews instead of self-report instruments is advised to enhance data collection in subsequent research efforts. Mindfulness-based schema therapy can assist women with obsessive-compulsive symptoms in acquiring skills to manage their obsessions. For instance, meditation and mindfulness practices can contribute to reduce obsessive thoughts. Cognitive-based exercises, such as identifying and challenging obsessive thoughts, can also be beneficial. Given the efficacy of this therapeutic approach, it is recommended that this treatment be implemented in existing therapeutic centers nationwide to alleviate the suffering caused by trauma and crises.
Ethical Considerations
Compliance with ethical guidelines
All procedures were approved by the Committee for Ethical Considerations in Human Experimentation of Islamic Azad University of Isfahan (Khorasgan) Branch. This study was registered by the Iranian Registry of Clinical Trials (IRCT). Parents signed written informed consent before the study, and all children orally expressed their assent.
Funding
This research received no grant from public, commercial, or non-profit funding agencies.
Authors' contributions
Conceptualization and supervision: Seyed Hamid Atashpour and Mohsen Golparvar; Methodology and analysis: Seyed Hamid Atashpour and Pouyan Ahanian Moghaddam; Data collection: Pouyan Ahanian Moghaddam; Investigation and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers thank the patients and all the people who helped them in conducting this research.
References
Abramowitz, J. S., & Reuman, L. (2020). Obsessive-compulsive disorder. In V. Zeigler-Hill & T. K. Shackelford (Eds), Encyclopedia of personality and individual differences (pp. 3304-3306 ). Cham: Springer. [DOI:10.1007/978-3-319-24612-3_919]
Arslan, G. (2023). Dysfunctional parenting and emotional problems and substance misuse: Enhancing psychological flexibility in college students. Journal of Ethnicity in Substance Abuse, 1-17. [DOI:10.1080/15332640.2023.2237930] [PMID]
Aslan, Ş., & Türk, F. (2022). [Comparison of concepts of cognitive flexibility and psychological flexibility (Turkish)]. Psikiyatride Guncel Yaklasimlar, 14(1), 119-130. [DOI:10.18863/pgy.917360]
Baniadam, L. , Makvand Hoseini, S. , & Sedaghat, M. (2017). [The efficacy of schema therapy on obsessive compulsive disorder and Marital Satisfaction on Married Women (Persian)]. Journal of Applied Psychological Research, 8(2), 131-143. [DOI:10.22059/japr.2017.68337]
Bhatt, S., Anitha, K., Chellappan, D. K., Mukherjee, D., Shilpi, S., & Suttee, A., et al. (2024). Targeting inflammatory signaling in obsessive-compulsive disorder: A promising approach. Metabolic Brain Disease, 39(2), 335-346. [DOI:10.1007/s11011-023-01314-3] [PMID]
Bond, F. W., Hayes, S. C., Baer, R. A., Carpenter, K. M., Guenole, N., & Orcutt, H. K., et al. (2011). Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42(4), 676-688. [DOI:10.1016/j.beth.2011.03.007] [PMID]
Caudek, C., Sica, C., Marchetti, I., Colpizzi, I., & Stendardi, D. (2020). Cognitive inflexibility specificity for individuals with high levels of obsessive-compulsive symptoms. Journal of Behavioral and Cognitive Therapy, 30(2), 103-113. [DOI:10.1016/j.jbct.2020.03.010]
Cervin, M., McGuire, J. F., D'Souza, J. M., De Nadai, A. S., Aspvall, K., & Goodman, W. K., et al. (2024). Efficacy and acceptability of cognitive‐behavioral therapy and serotonin reuptake inhibitors for pediatric obsessive‐compulsive disorder: A network meta‐analysis. Journal of Child Psychology and Psychiatry, 65(5), 594-609. [DOI:10.1111/jcpp.13934] [PMID]
Chien, W. T., Tse, M. K., Chan, H. Y., Cheng, H. Y., & Chen, L. (2022). Is mindfulness-based intervention an effective treatment for people with obsessive-compulsive disorder? A systematic review and meta-analysis. Journal of Obsessive-Compulsive and Related Disorders, 32, 100712. [DOI:10.1016/j.jocrd.2022.100712]
Darby, K. P., Castro, L., Wasserman, E. A., & Sloutsky, V. M. (2018). Cognitive flexibility and memory in pigeons, human children, and adults. Cognition, 177, 30-40. [DOI:10.1016/j.cognition.2018.03.015] [PMID]
Den Ouden, L., Tiego, J., Lee, R. S. C., Albertella, L., Greenwood, L. M., & Fontenelle, L., et al. (2020). The role of experiential avoidance in transdiagnostic compulsive behavior: A structural model analysis. Addictive Behaviors, 108, 106464. [DOI:10.1016/j.addbeh.2020.106464] [PMID]
Deveci, N., Uğurlu, M., Karakaş Uğurlu, G., Kabadayi Şahin, E., Erdoğan, E. Ç., & Çayköylü, A. (2024). The effects of psychological flexibility and resilience on psychopharmacological treatment response in patients with obsessive-compulsive disorder. International Clinical Psychopharmacology, 39(3), 181-186. [DOI:10.1097/YIC.0000000000000499] [PMID]
Epstein, N. B., & Dattilio, F. M. (2020). Behavioral and cognitive-behavioral approaches in systemic family therapy. In K. S. Wampler., R. B. Miller., R. B. Seedall (Eds.), The handbook of systemic family therapy (pp. 365-389). Hoboken: Wiley. [Link]
Fineberg, N. A., Day, G. A., de Koenigswarter, N., Reghunandanan, S., Kolli, S., & Jefferies-Sewell, K., et al. (2015). The neuropsychology of obsessive-compulsive personality disorder: A new analysis. CNS Spectrums, 20(5), 490-499. [DOI:10.1017/S1092852914000662] [PMID]
Francazio, S. K., & Flessner, C. A. (2015). Cognitive flexibility differentiates young adults exhibiting obsessive-compulsive behaviors from controls. Psychiatry Research, 228(2), 185-190. [DOI:10.1016/j.psychres.2015.04.038] [PMID]
Ghazanfari, F., & Sepahvand, R. (2014). [The effectiveness of Mindfulness-based Stress Reduction (MBSR) Technique in Obsessive-Compulsive Disorder Symptoms (Persian)]. Journal of Clinical Psychology and Counseling Research, 4(2), 110-121. [DOI:10.22067/ijap.v4i2.19209]
Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Fleischmann, R. L., & Hill, C. L., et al. (1989). The yale-brown obsessive compulsive scale. I. development, use, and reliability. Archives of General Psychiatry, 46(11), 1006–1011. [DOI:10.1001/archpsyc.1989.01810110048007] [PMID]
Görmezoğlu, M., Bouwens van der Vlis, T., Schruers, K., Ackermans, L., Polosan, M., & Leentjens, A. F. G. (2020). Effectiveness, timing and procedural aspects of cognitive behavioral therapy after deep brain stimulation for therapy-resistant obsessive-compulsive disorder: A systematic review. Journal of Clinical Medicine, 9(8), 2383. [DOI:10.3390/jcm9082383] [PMID]
Gruner, P., & Pittenger, C. (2017). Cognitive inflexibility in obsessive-compulsive disorder. Neuroscience, 345, 243-255. [DOI:10.1016/j.neuroscience.2016.07.030] [PMID]
Gu, Y., Xu, G., & Zhu, Y. (2018). A randomized controlled trial of mindfulness-based cognitive therapy for college students with ADHD. Journal of Attention Disorders, 22(4), 388-399. [DOI:10.1177/1087054716686183] [PMID]
Hayes, S. C., Strosahl, K., Wilson, K. G., Bissett, R. T., Pistorello, J., & Toarmino, D., et al. (2004). Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record, 54(4), 553-578. [DOI:10.1007/BF03395492]
Hermida-Barros, L., Primé-Tous, M., García-Delgar, B., Forcadell, E., Lera-Miguel, S., & de la Cruz, L. F., et al. (2024). Family accommodation in obsessive-compulsive disorder: an updated systematic review and meta-analysis. Neuroscience and Biobehavioral Reviews, 161, 105678.[DOI:10.1016/j.neubiorev.2024.105678] [PMID]
Hoppen, L. M., Kuck, N., Bürkner, P. C., Karin, E., Wootton, B. M., & Buhlmann, U. (2021). Low intensity technology-delivered cognitive behavioral therapy for obsessive-compulsive disorder: A meta-analysis. BMC Psychiatry, 21(1), 322. [DOI:10.1186/s12888-021-03272-5] [PMID]
Huang, F. F., Wang, P. C., Yang, X. Y., Luo, J., Yang, X. J., & Li, Z. J. (2023). Predicting responses to cognitive behavioral therapy in obsessive-compulsive disorder based on multilevel indices of rs-fMRI. Journal of Affective Disorders, 323, 345-353. [DOI:10.1016/j.jad.2022.11.073] [PMID]
Izadi, R., Neshatdust, H. T., Asgari, K., Abedi, M. R. (2014).[Comparison of the efficacy of acceptance and commitment therapy and cognitive-behavior therapy on symptoms of treatment of patients with obsessive-compulsive disorder (Persian)]. Journal of Research in Behavioural Sciences, 12(1), 19-33. [Link]
Khadem, S., Fakhri, M., & Emadian, S. O. (2023). The effectiveness of mindfulness-based cognitive therapy on rumination, perfectionism, and thought-action fusion in women with obsessive-compulsive disorder. Bi-monthly Journal of Adolescent and Young Adult Psychological Studies, 4(4), 1-13. [DOI:10.61838/kman.jayps.4.4.11]
Leeuwerik, T., Cavanagh, K., & Strauss, C. (2020). The association of trait mindfulness and self-compassion with obsessive-compulsive disorder symptoms: results from a large survey with treatment-seeking adults. Cognitive Therapy and Research, 44(1), 120-135. [DOI:10.1007/s10608-019-10049-4]
Luppino, O. I., Tenore, K., Mancini, F., & Basile, B. (2018). A theoretical integration of schema therapy and cognitive therapy in OCD treatment: Goals and beliefs of the obsessive mind (Part I). Psychology, 9(9), 2261. [DOI:10.4236/psych.2018.99129]
Mathur, S., Sharma, M. P., Balachander, S., Kandavel, T., & Reddy, Y. J. (2021). A randomized controlled trial of mindfulness-based cognitive therapy vs stress management training for obsessive-compulsive disorder. Journal of Affective Disorders, 282, 58-68. [DOI:10.1016/j.jad.2020.12.082] [PMID]
Mardpour, A., & Hadizadeh Kaffash, R. (2017). The effectiveness of mindfulness on reducing symptoms of obsessive-compulsive disorder. Paper presented at: International Conference on Psychology, Educational Sciences, and Behavioral Sciences. 2017 November 20; Tehran, Iran. [Link]
Morris, L., & Mansell, W. (2018). A systematic review of the relationship between rigidity/flexibility and transdiagnostic cognitive and behavioral processes that maintain psychopathology. Journal of Experimental Psychopathology, 9(3), 2043808718779431. [DOI:10.1177/2043808718779431]
Nasiri, A., Sharifi, T., Ghazanfari, A., & Chorami, M. (2022). [Comparison of the effectiveness of schema-therapy and realitytherapy on psychological flexibility and emotional self-regulation of preschool teachers (Persian)]. Quarterly of Applied Psychology, 16(4), 161-183. [DOI:10.52547/apsy.2022.224539.1203]
Onaral, G. (2021). Effectiveness of third wave therapies for treatment of obsessive-compulsive disorder: A review. Psikiyatride Güncel Yaklaşımlar, 13(2), 292-331. [Link]
Paast, N., Khosravi, Z., Memari, A. H., Shayestehfar, M., & Arbabi, M. (2016). Comparison of cognitive flexibility and planning ability in patients with obsessive-compulsive disorder, patients with obsessive-compulsive personality disorder, and healthy controls. Shanghai Archives of Psychiatry, 28(1), 28-34. [PMID]
Parseh, M., Naderi, F., & Mehrabizade Honarmand, M. (2015). [Efficacy of cognitive– behavioral family therapy on marital conflicts and sexual satisfaction in couples referred to psychological centers (Persian)]. Clinical Psychology Achievements, 1(1), 125-148. [DOI:10.22055/jacp.2015.11510]
Peeters, N., van Passel, B., & Krans, J. (2022). The effectiveness of schema therapy for patients with anxiety disorders, OCD, or PTSD: A systematic review and research agenda. The British Journal of Clinical Psychology, 61(3), 579–597. [DOI:10.1111/bjc.12324] [PMID]
Ponzini, G. T., & Steinman, S. A. (2022). A systematic review of public stigma attributes and obsessive-compulsive disorder symptom subtypes. Stigma and Health, 7(1), 14–26. [DOI:10.1037/sah0000310]
Raftar, A. M. R., Shareh, H., & Toozandehjani, H. (2020). [Effectiveness of mindfulness-based schema therapy in depression, anxiety and hopelessness of betrayed women: A randomized clinical trial (Persian)]. Journal of Neyshabur University of Medical Sciences, 8(2), 140-155. [Link]
Reis, A., Westhoff, M., Quintarelli, H., & Hofmann, S. G. (2024). Mindfulness as a therapeutic option for obsessive-compulsive disorder. Expert Review of Neurotherapeutics, 24(8), 735–741. [DOI:10.1080/14737175.2024.2365945] [PMID]
Renner, F., DeRubeis, R., Arntz, A., Peeters, F., Lobbestael, J., & Huibers, M. J. H. (2018). Exploring mechanisms of change in schema therapy for chronic depression. Journal of Behavior Therapy and Experimental Psychiatry, 58, 97-105. [DOI:10.1016/j.jbtep.2017.10.002] [PMID]
Rajeziesfahani, S., Fata, L., Hassanabadi, H., Yaghuobi, H., Zahiroddin, A., & Sadr, S., et al. (2016). [Meta-cognitive therapy in drug-resistant patients with obsessive - compulsive disorder: Case report (Persian)]. The Scientific Journal of Rehabilitation Medicine, 5(2), 40-51. [DOI:10.22037/jrm.2016.1100168]
Rosa-Alcázar, A. I., Rosa-Alcázar, Á., Martínez-Esparza, I. C., Storch, E. A., & Olivares-Olivares, P. J. (2021). Response inhibition, cognitive flexibility and working memory in obsessive-compulsive disorder, generalized anxiety disorder and social anxiety disorder. International Journal of Environmental Research and Public Health, 18(7), 3642. [DOI:10.3390/ijerph18073642] [PMID]
Şahin, H., Köşger, F., EşSizoğlu, A., & Aksaray, G. (2018). The relationship between obsessive belief level and cognitive flexibility in patients with obsessive compulsive disorder. Noro Psikiyatri Arsivi, 55(4), 376–379. [DOI:10.5152%2Fnpa.2017.21648] [PMID]
Sanagavi Moharrar, G., & Mir Shekari, H. (2019). [Evaluation of the relationship between cognitive flexibility and obsession in anxiety patients (Persian)]. Medical Journal of Mashhad University of Medical Sciences, 61(supplment1), 223-230. [DOI:10.22038/mjms.201q9.14889]
Seyed Nour, S., & Homaei, R. (2019). Effectiveness of group cognitive-behavioral therapy on the self-care behaviors. psychological wellbeing, and hope of patients with type II diabetes (persian)]. Journal of Clinical Nursing and Midwifery, 8(1), 265-275. [Link]
Shameli, A., Althoff, T., Saberi, A., & Leskovec, J. (2017). How gamification affects physical activity: Large-scale analysis of walking challenges in a mobile application. Proceedings of the International World-Wide Web Conference. International WWW Conference, 2017, 455–463. [DOI:10.1145/3041021.3054172] [PMID]
Soltani, E., Shareh, H., Bahrainian, S. A., & Farmani, A. (2013). [The mediating role of cognitive flexibility in correlation of coping styles and resilience with depression (Persian)]. Pajoohandeh Journal, 18(2), 88-96. [Link]
Sunde, T., Hummelen, B., Himle, J. A., Walseth, L. T., Vogel, P. A., & Launes, G., et al. (2019). Early maladaptive schemas impact on long-term outcome in patients treated with group behavioral therapy for obsessive-compulsive disorder. BMC Psychiatry, 19(1), 318. [DOI:10.1186/s12888-019-2285-2] [PMID]
Tomiyama, H., Nakao, T., Murayama, K., Nemoto, K., Ikari, K., & Yamada, S., et al. (2019). Dysfunction between dorsal caudate and salience network associated with impaired cognitive flexibility in obsessive-compulsive disorder: A resting-state fMRI study. NeuroImage. Clinical, 24, 102004. [DOI:10.1016/j.nicl.2019.102004] [PMID]
Vreeswijk, M. V., Broersen, J., & Schurink, G. (2014). Mindfulness and schema therapy: A practical guide. Hoboken: Wiley. [Link]
Wheaton, M. G., Ward, H. E., Silber, A., McIngvale, E., & Björgvinsson, T. (2021). How is the COVID-19 pandemic affecting individuals with obsessive-compulsive disorder (OCD) symptoms? Journal of Anxiety Disorders, 81, 102410. [DOI:10.1016/j.janxdis.2021.102410] [PMID]
Young, J. (1950). Cognitive therapy of schema-oriented personality disorders [A. Sahebi., & H. Hamidpour, Persian trans]. Tehran: Arjmand publications. [Link]
Young, J. E., Klosko, J. S., & Weishaar, M. E. (2003). Schema therapy: A practitioner’s guide. New York: Guilford Press. [Link]
Zareei, M. B., Bahrainian, S. A. M., Ahi, Q., & Mansouri, A. (2024). [Comparison of the effectiveness of cognitive therapy based on mindfulness and schema therapy on emotion regulation and distress intolerance of women with obsessivecompulsive symptoms (Persian)]. Journal of Research in Psychological Health, 17(4), 82-105. [Link]
Type of Study: Original Research Article |
Subject:
Cognitive behavioral
Received: 2024/08/16 | Accepted: 2024/11/10 | Published: 2025/01/1
Received: 2024/08/16 | Accepted: 2024/11/10 | Published: 2025/01/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |