Volume 12, Issue 4 (Autumn 2024)
PCP 2024, 12(4): 383-396 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sharafi S E, Shegarf Nakhaei M, Taj A. A Case Report of a Patient With Extreme Anorexia Nervosa and Hyper Prolactinoma: Complaints and Treatment. PCP 2024; 12 (4) :383-396
URL: http://jpcp.uswr.ac.ir/article-1-941-en.html
URL: http://jpcp.uswr.ac.ir/article-1-941-en.html
1- Psychosomatic Research Center, Imam Khomeini Hospital, Tehran University of Medical Sciences, Tehran, Iran.
2- Psychosomatic Research Center, Imam Khomeini Hospital, Tehran University of Medical Sciences, Tehran, Iran. ,rezashegarf@yahoo.com
3- Non-Communicable Diseases Research Center, Sabzevar University of Medical Sciences, Sabzevar. Iran.
2- Psychosomatic Research Center, Imam Khomeini Hospital, Tehran University of Medical Sciences, Tehran, Iran. ,
3- Non-Communicable Diseases Research Center, Sabzevar University of Medical Sciences, Sabzevar. Iran.
Keywords: Anorexia nervosa (AN), Eating disorder, Prevention, Management, Treatment, Hyper prolactinoma
Full-Text [PDF 624 kb]
(659 Downloads)
| Abstract (HTML) (1723 Views)
Full-Text: (731 Views)
Introduction
Anorexia nervosa (AN), first described by Sir William Withey Gull in 1968 (Crumby et al., 2024), is a severe psychiatric disorder, in which an individual abstains from keeping their weight at a minimum proportionate to their height and age; accordingly, they start to suffer from severe weight loss and disturbed physical and psychosocial functioning (Berends et al., 2012). Long starvation periods lead to adaptive changes in most physiologic systems. Some cases manage to lose weight by restricting their diet while others resort to behaviors, such as binging, vomiting, and use of laxatives (the binge-eating and purging type) (Salvato et al., 2024).
AN was previously diagnosed and reported in Western countries but its prevalence is on the rise in other countries (Demarque et al., 2015). Reports suggest that its prevalence ascends the cross-cultural borders. Although there are cultural differences between traditional and Western communities, several factors increase the prevalence of the disorder in non-Western countries, exposure to modern trade experiences in the West, globalization effects via facilitated cross-continental voyages, and use of social media (Qadan, 2009).
People with anorexia often have a strong fear of gaining weight and may think they are overweight, even when they are thin. To prevent weight gain or continue to lose weight, people with anorexia often limit the amount or type of food they eat. They place a high value on controlling their weight and shape and use extreme efforts that can greatly harm their lives. Anorexia, like other eating disorders, can take over people’s lives and be very hard to overcome. Because it is related to changes in the brain, anorexia behaviors are not choices, and the illness is not about food or looking a certain way. With proven treatment, people with anorexia can return to a healthy weight, develop more balanced eating habits, and reverse some of anorexia’s serious medical and mental health complications (Holtom-Viesel et al., 2014).
In a Middle Eastern country like Iran, the prevalence of AN among female high school students in Tehran City, the capital of Iran, in 2000 was reported as 0.09% (Nobakht, 2000). In 2015, its prevalence among adolescents in Northeast Iran was 1.2% (Rauof et al., 2015). Comparably, its prevalence in the West ranges from 1.2% to 2.2% (Jagielska, 2017). Therefore, while unexpected from an Eastern community, the Iranian community appears much like the Western communities as far as the prevalence of AN is concerned. However, the disorder is less recognized in Iran and the health system is less prepared for screening and timely diagnosis of AN. Therefore, we decided to report a severe case of AN who was admitted and hospitalized in the largest educational hospital in Tehran City.
Materials and Methods
A single, educated master of industrial engineering 32-year-old female patient was admitted with a locked knee, weakness, and lethargy, and hospitalized in the hematology ward due to electrolyte and hematological complications. She was then referred to the psychiatric service due to her extremely low weight.
She completely refused her admission to the psychosomatic ward but accepted starting her treatment after assurance and the doctor’s promise to request a medical consultation for her musculoskeletal problems. She appeared highly guarded in providing a medical history. However, successive interview attempts gradually brought more information about her. She revealed that symptoms began 10 years ago following her father’s disease (who suffered a hematologic complication involving his spleen and used warfarin. From then on, she abstained from eating with her family members and decreased her food intake to a minimum; for instance, she ate 2-3 spoons for lunch and dinner; she recently ate only one meal during the day. She has avoided cooked food for the past 1-2 year and adopted a vegetarian diet only, including half a courgetti, one tomato, and one cucumber. She believes that her father suffered from overeating, and blames others for eating. Neither intentional vomiting nor periodical overeating was reported. During the past two years, her weight has dropped from 51 kg to 36 kg; it minimized to 24 kg due to strict restrictions on food intake. She stated that she could not get up without help but could walk independently. Despite her height (160 cm) and body mass index (BMI) (9.37), she expressed her satisfaction with her weight.
Her history showed no psychotic and mood signs, self-harm, and suicide. She reported normal sleeping patterns, no smoking, nor using alcohol but reported both symmetry obsessions and compulsion to over-wash things, exacerbated during the past year. She was worried about her physical health and frequently had complete blood count (CBC) tests every three months.
In psychiatric examination, she pretends to be normal and avoids discussing her weight and nutrition. Her mood is described as mostly normal but occasionally irritable. She is worried about her health and accepts her compulsion to repeatedly wash the house yard, take frequent showers, longer stay in the toilet, and obsession with ordering things, such as the perfect folding of her clothes. Aggravated obsession has been reported since the last year. She is neither psychotic nor suicidal. Her consciousness, orientation, and cognitive status are normal.
Digestive problems and malignancy were rejected, and the diagnostic and statistical manual of mental disorders, fifth edition (DSM-5) diagnostic criteria led us to extreme AN (restricting type) diagnosis. Upon admission, the patient avoided her prescribed regimen meals, abundantly drank tea and liquid, ate ample fruit, stored and neatly piled up edibles from other patients in her locker, showed distress to eat in front of others, and got agonized upon nutrition plan control by the doctor or medical personnel. However, these behaviors started to fade away during her stay in the ward.
Laboratory test results
Electrolyte levels were measured at the beginning and periods. Upon nephrology consultation, treatment was initiated with potassium chloride (KCl) 15% due to mild hypokalemia. Also, oral Calcium + D was prescribed. After diet prescription and the likelihood of hypophosphatemia, successive measurements revealed no drop in phosphate level. Table 1 presents changes in electrolyte levels.

Tables 2 and 3 present the results of CBC tests, blood indexes, iron, reserves, and peripheral blood smear (PBS).

Hematological consultation was requested due to anemia and leukopenia, and two units of packed cells were injected due to a drop in hemoglobin levels. Figure 1 shows subsequent changes after injection.

Regarding bicytopenia and PBS, myeloid dysplasia with malnutrition was observed and medical prescriptions included daily injection of B12 100 mg up to 7 days and then weekly, daily B6 tablets 400 mg, daily B1 300 mg, daily folic acid 5 mg, and daily multivitamin.

Table 4 presents an evaluation of vitamins at the beginning and one month after the treatment.

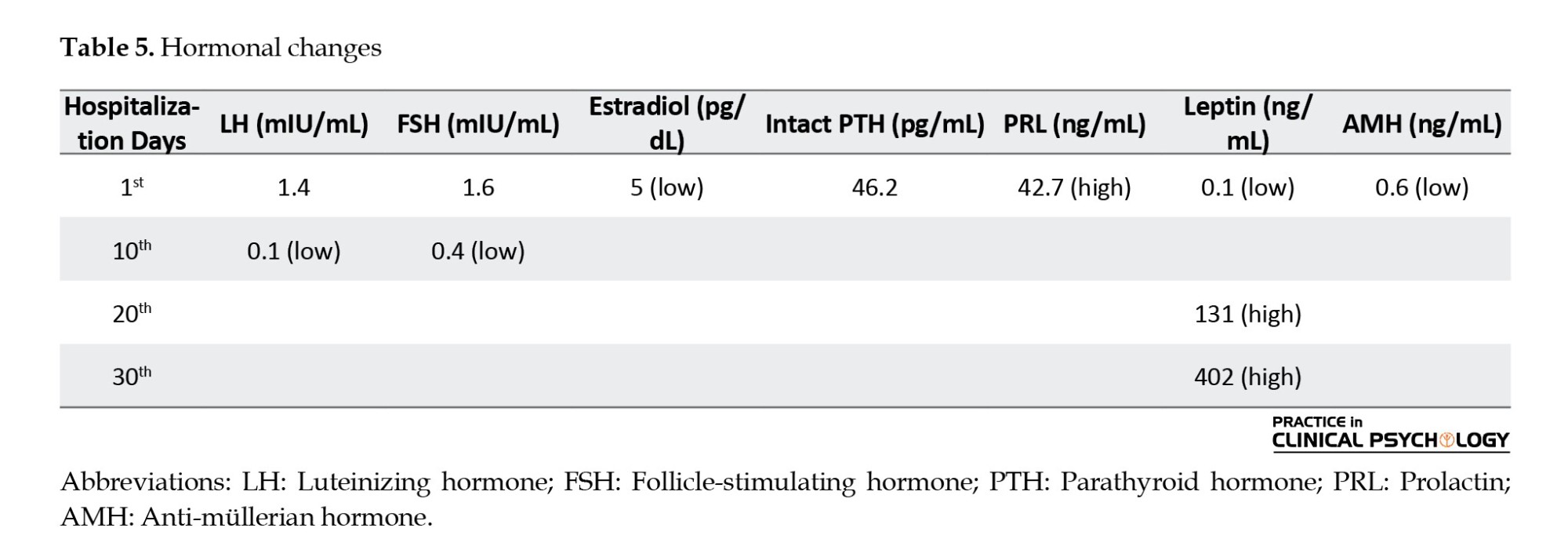
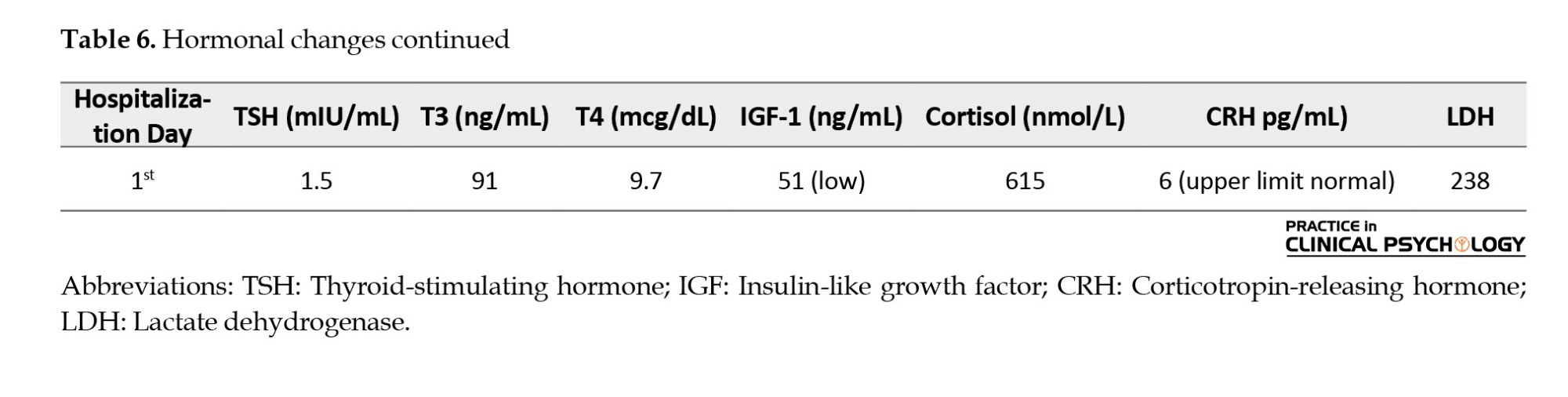
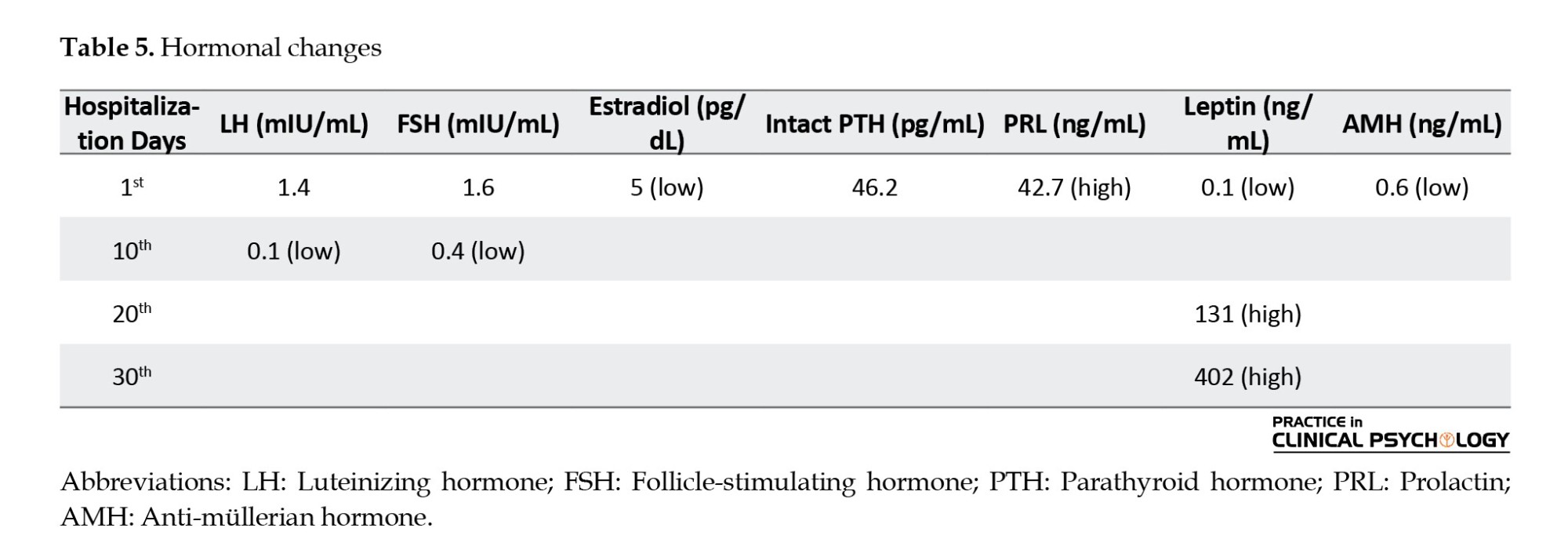
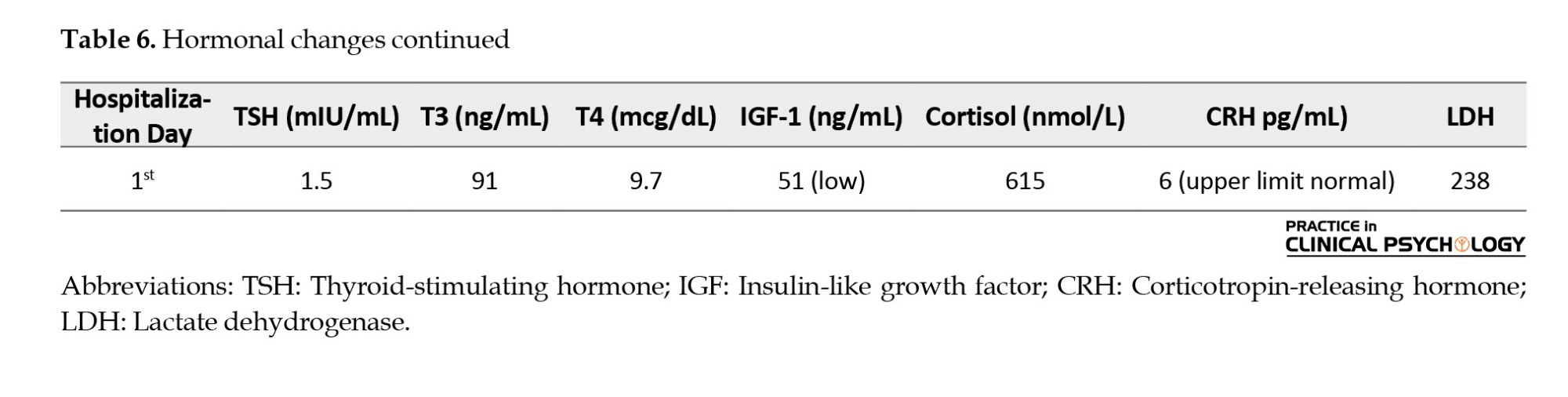
Endocrine consultation was requested due to the patient’s amenorrhea and high prolactin level. The results of hormonal tests (Tables 5 and 6) showed that sex hormones and gonadotropin were low. Successive tests also revealed that prolactin levels were high; insulin-like growth factor-1 (IGF-1), leptin, and anti-Müllerian hormone were low; corticotropin-releasing hormone (CRH) was at the highest normal level; however, parathormone, thyroid hormones, and cortisol were normal.
Dual x-ray absorptiometry (DXA) bone densitometry using LEXXOS densitometer revealed a lower density score than the score expected for her age (lumbar region Z score was -4.1). Based on her amenorrhea, osteoporosis, and hormonal test results, she was prescribed to take estradiol conjugated 0.625 from day 1 to day 25 of menstruation as well as medroxyprogesterone 10 mg from day 16 to day 25 of menstruation. In addition, a D3 injection every two weeks and daily calcium+D oral were also prescribed.
Therapeutic measures
Following hyperprolactinemia, a magnetic resonance imaging (MRI) of the brain without contrast was requested to examine hypophysis, which reported a lesion of 7.5 mm to the right of the hypophysis and mild bulge in the right with some mild deviation of hypophysis stem to the left, contributing to pituitary microadenoma diagnosis. Accordingly, a weekly oral tablet of cabergoline 0.5 was initiated for hyperprolactinemia and pituitary microadenoma. Pelvic and abdominal ultrasound imaging were normal. Computed tomography (CT) scan of the area did not render anything abnormal. Electrocardiogram (EKG) at the beginning of treatment was normal, QTc=430 ms; successive EKS also were normal. Kidney and liver functions were normal, too.
The next goal was to correct the diet and weight gain. Due to her initial low weight and avoidance of oral intake, she was given a daily venous feed of amino acid 5% and intralipid 500-700 Kcal. After the patient started to cooperate, 6 oral daily meals containing 500-700 Kcal, including peptiamine three times a day, drug administration and food intake were carefully supervised, and the patient was forbidden to go to the toilet two hours after each meal to prevent the likelihood of intentional vomiting.
Based on the patient’s chief complaint (i.e. musculoskeletal problems, such as inability to get up and sit, and locked knee), sports medicine consultation was requested. Despite the patient’s initial resistance to treatment, acceptance of supportive psychotherapy was suggested by active listening and empathy with the patient’s medical problems. After medical communication to enhance her motivation, we presented psycho-education on the diagnosis and complications of her disease and the likelihood of more serious complications in the future, if left untreated.
A psychotropic medication used at the beginning was olanzapine with a primary dose of 2.5 mg each night, which resulted in her lessened resistance to treatment and irritability and enhanced cooperation; with the patient’s acceptance, the dosage gradually increased to 7.5 mg daily for the first week, and 10 mg daily for the second week. During the second month of hospitalization and due to the patient’s obsessive-compulsive disorder signs, sertraline 12.5 mg was started; the dosage gradually increased to 25 mg daily. The patient’s weight gradually increased from 24 kg to 17.5 kg during her 45-day hospitalization. Considering her height (160 cm), Table 7 and Figure 2 show her BMI changes during the treatment.


Considering the stability of medical status and electrolyte disorders at the very beginning of treatment, mood improvement, dietary behaviors, the patient’s relatively appropriate cooperation with the therapists, improvement in the patient’s attitude towards her disease and its complications, concerns about the COVID-19 contagion, the patient’s and her family’s stress on continuing the rest of treatment at home, she was discharged with BMI=10.74, and the rest of the treatments were left to be followed up as outpatients.
Discussion
The patient’s problem started at the age of 22 years with signs of retarded menstruation and puberty at an earlier age. Studies also show most patients are young and adolescent cases, the period of life in which they encounter stressors of puberty, socializing, and starting independent lives (Gonidakis et al., 2014, Cuspidi et al., 2024). Lock believes that adolescence is the beginning of major brain development; therefore, anorexia and subsequent complications cause serious damage to this process (Hurst et al., 2015). This disorder mainly affects women, although it may be observed in men and other age periods (Berends et al., 2012).
Etiology and diagnosis
In this case, her avoidance of feeding was not due to fear of fatphobia, rather she abstained from food for the fear of a disease that her father suffered from and she felt it was due to overeating. Some researchers believe that the clinical presentations of this disorder in non-Western ethnicities, such as Caucasians are different from those observed in Europe and North America. For instance, they contend that fatphobia may not be the main reason for AN in the East and those other causes, such as digestive, and diseases can be the reason to avoid eating food. In 2013, a 14-year-old boy was reported whose food abstinence was due to digestive problems after eating fried and packaged food (Paul et al., 2013). Another study reported 70 Chinese patients with AN, 595 of whom did not have fatphobia; rather, they stated other reasons, such as gastrointestinal problems as the main reason to avoid food (Dani et al., 2024). Probably, it is due to such reports that persistent behavior that interferes with weight gain is added to criterion B in the diagnostic and statistical manual of mental disorders, fifth edition (DSM-5) (Demarque et al., 2015). The patient’s BMI (9.37) represented an extreme form of AN, which urgently required her hospitalization to control her medical complications (Cass et al., 2020).
Etiology
Biological, psychological, and sociocultural factors play a role in causing symptoms of AN, but environmental factors have been the focus of researchers’ attention (Phillipou et al., 2019). Biologically, the prevalence rate in the immediate family members of the patient is 10 times that of the normal population (Cass et al., 2020). In this patient, family history was negative but traces of anxiety and obsessive disorders seemed likely in her mother. Today, scholars consider family dysfunction not as an etiologic factor but as a perpetuating factor for symptoms of AN (Martini et al., 2024). Regarding the onset of the disorder in early adolescence, psychological, social, and biological factors of adolescence can appear as one possible etiological factor of the disorder (Martini et al., 2024), which was witnessed in the patient we described as delayed menstruation and hyperprolactinemia at puberty. Also, co-morbidities of obsessive-compulsive disorder, major depressive disorder, and various anxiety disorders are in perspective (Wonderlich et al., 2024), which appears as uncontrolled washing, and frequent CBC check-ups.
Electrolyte disorders
Hyponatremia is likely to occur in AN, which results from the patient’s desire to drink liquids to show a false feeling of weight gain. Other causes may include kidney failure to excrete enough water and, quite rarely, syndrome of inappropriate antidiuretic hormone (SIADH) (Cass et al., 2020). However, the most common electrolyte disorders of AN are hypokalemia. The patients’ intake of magnesium is remarkably low, and hypomagnesemia occurs either before or during re-feeding. Hypomagnesemia is often caused by hydration through venous saline infusion and magnesium elimination; it may occur simultaneously with hypokalemia and it becomes necessary to measure magnesium levels in the blood in case of resistant hypokalemia. Also, hypocalcemia may occur both in hunger and re-feeding, which may be caused by giving phosphate to patients during refeeding. It may be due to hypomagnesemia (Winston, 2012). Fortunately, in this case, the only electrolyte disorder we encountered was hypokalemia, which was successfully controlled early in the treatment, and no other disorder was observed at the initial or later stages of refeeding.
Cardiopulmonary disorders
Patients with the restricting type of AN suffer from recurring cardiopulmonary disorders. Mitral valve prolapses due to cardiac atrophy occur in 25% of cases, which manifest as palpitation, vertigo, and dyspnea. The most common arrhythmia is sinus bradycardia, which is caused mainly by increased vague tone due to malnutrition. Systolic blood pressure is normally under 100 mm Hg. Cardiac sudden death occurs due to prolonged QT interval, caused by medical and electrolyte disorders. Low cardiac output occurs in response to myocardial atrophy due to malnutrition. In addition, weak respiratory muscles and diaphragm weakness have a role in patients’ dyspnea (Cass et al., 2020). In the present case, no problem was observed in the cardiologic consultation, and ECG, heartbeats and blood pressure were normal.
Endocrine disorders
Multiple endocrine changes occur in patients with the restricting type of AN to adapt to the energy intake of the body (Cass et al., 2020). The level of hormone regulating the appetite alters in such a way that leptin decreases and ghrelin increases. The function of leptin is to regulate energy homeostasis and food intake in proportion with the body weight so that its secretion increases with fat and weight gain in a normal person; leptin directly inhibits the appetite-stimulating effects of neuropeptide Y, resulting in declined appetite. A significant reduction of lipids and leptin in the blood is observed in patients with AN. Genome-wide association studies have determined high-risk genome spots of AN incidence related to leptin dysregulation; thus, it may function as a potential biomarker in screening AN (Kim et al., 2020). Secreted predominantly from the stomach, ghrelin is a peptide with profound or exogenic properties and stimulates the growth hormone. Researchers believe that it is a brain-gut peptide and has a role in regulating body energy. Several studies have been conducted on the effects of ghrelin in AN patients; these studies have reported higher levels of ghrelin in these patients than in normal persons. It increases the secretion of prolactin, adrenocorticotropic hormone (ACTH), and cortisol (Salvato et al., 2024). Prolactin serum levels in AN patients varied from normal, to mildly increased, and increased, but no relationship was observed between low body weight and prolactin levels (Wonderlich et al., 2024). In this case, the leptin level was very low 0.1 ng/mL (the normal range is 2.5-21.8 ng/mL); also, hyperprolactinemia was observed and reported in the context of pituitary microadenoma. It seems that further investigation is required to find a relationship between AN and prolactin levels in the blood as either a disorder or a biomarker of the disorder. Probably, we face various biological types of AN, in some of which increased prolactin levels are observed (Jagielska, 2017).
Normal menses show increased bone density and the relationship is independent of the patient’s weight change. It suggests the role of hypogonadism in lowered bone density (Salvato et al., 2024). In earlier studies, 17.6% to 88% of patients with AN had low vitamin D levels but their intact parathyroid hormone (PTH) was relatively normal. As indicated in Table 5, in our patient, the parathormone level was 46.2, which is normal. In research by Lenherr-Taube et al., almost one-third of adolescents with AN had normal PTH levels; and they concluded that PTH may be age-dependent (Lenherr-Taube et al., 2020).
Increased levels of growth hormone in the blood, reduced IGF-1, and resistance to the effects of growth hormone are visible in AN patients, which may be attributable to the role of this hormone in lipolysis (Crumby et al., 2024). In our patient, the blood levels of IGF-1 were lower than the normal values. Hypogonadotropic hypogonadism (low luteinizing hormone [LH], follicle-stimulating hormone [FSH], and estradiol) and amenorrhea due to hypothalamus-pituitary axis dysfunction occur in 85% of patients (Cass et al., 2020). In our patient, low luteinizing hormone [LH], follicle-stimulating hormone (FSH) and estradiol were reported.
Patients with AN are affected with more infertility and more labor complications than the normal population. Normally, fertility is negatively correlated with age. Some diseases lead to the early reduction of follicle count, termed the early reduction of ovarian reserve. Anti-Müllerian hormone (AMH) is produced by granulosa cells from the small follicles in a woman’s ovaries and is used as a marker of oocyte quantity. It reaches its maximum in women’s third decade of life and is not measurable after menopause. Its low level may show reduced response of ovaries to stimuli and lowers the likelihood of pregnancy. AMH is higher than normal in patients with AN (4.7 vs 3.2 ng/mL) and in 19.6% of patients with AN, AMH levels are higher than the normal range (>6.78). Therefore, AMH levels are either normal or increased in AN patients; and its reduction means early reduction of ovarian reserve and should not be attributed solely to malnutrition (Pitts et al., 2020). As indicated in Table 5, the AMH level in our patient was 0.6 ng/mL, below the normal range.
Hypoglycemia is common. Hypercholesterolemia is also common but its significance in predisposing the patient to cardiovascular diseases is unknown. Increased salivary amylase production is a cause of the patient’s latent vomiting but normal amylase does not reject vomiting. In our patient, the amylase level was normal.
Hypercarotenemia leads to the alteration of orange skin color, which is not to be mistaken with icterus. Its etiology is unknown and may be attributable to the overuse of vegetables and fruit in some cases (Winston, 2012). In the present case, her yellowish skin color gradually decreased upon admission due to the weight loss.
Deficiency of micronutrients
Most patients with AN tend to lower their intake of micronutrients, including zinc, copper, vitamin C, riboflavin, and vitamin B2. Thiamin deficiency occurs in 38% of cases; due to its importance in carbohydrate metabolism, its deficiency is associated with cognitive defects. Also, taste changes and neuropsychiatric symptoms appear following zinc deficiency (Winston, 2012). In the case of our patient, despite her aggravated condition, blood levels of folic acid, vitamin B12, and D3 were in the normal range (Table 3), which may account for the patient’s tendency to use sufficient amounts of salts and vitamins despite her abstinence from high-calorie foods.
Gastrointestinal complications
In 50% of AN patients, gastrointestinal complications occur in the form of satiety, early or feeling full, abdominal distension, pain, and nausea. Nasopharyngeal muscle weakness causes dysphagia, coughing while eating, and aspiration. Gastroparesis is a barrier against refeeding because it brings about early satiety. Delayed colon discharge and constipation affect two-thirds of patients (Cass et al., 2020). Similarly, our patient also reported feeling full at the beginning of refeeding; she often complained of constipation from the early days of hospitalization but further examination revealed that she had no serious complaints of defecation and stool consistency; rather, frequency of defecation was low due to poor nutrition, but tended to improve through improved nutritional status.
In 50% of patients, increased level of aminotransferase enzymes from the liver is evidenced throughout refeeding. Type 1 occurs due to hepatic ischemia and hypoperfusion, hepatocyte autophagy, and glutathione synthetase deficiency, which tend to be cured by feeding. However, type 2 is a result of steatohepatitis and requires a lowered intake of fat and carbohydrates (Winston, 2012). In our patient, test results indicated no increase in the levels of these enzymes.
Albumin levels in these patients are usually normal even in patients with severe malnutrition. If hyperalbuminemia occurs, it may be due to factors other than malnutrition, such as infection, and bears a bad prognosis (Winston, 2012). In our patient, the albumin level was normal.
Neurological complications
Both the central and peripheral nervous systems are affected by AN. The white and grey matter are affected in central nervous system (CNS), leading to cognitive disorders that may persist even after treatment. Also, thalamus dysfunction results in thermal dysregulation and hypothermia, as well as smelling and taste disturbance. Also, neuropraxia (i.e. focal demyelination without damage to nerve continuity) develops as a result of damage to subcutaneous peripheral nerves, which occasionally causes foot drop and local hand weakness; but these peripheral complications are reversible (Cass et al., 2020). In the present patient, no evidence of cognitive disorders was found. Upon neurologic examination, no serious pathologic finding was found except weakness of the lower limbs and her inability to get up. Her brain’s MRI reveals no significant result except pituitary microadenoma.
Hematological complications
The prevalence of anemia, thrombocytopenia, and leukopenia in AN patients is 16.4%, 7.4%, and 50.5%, respectively. As can be seen, low white blood cell (WBC) is more prevalent than other complications. Replacement of saccharides with bone marrow lipids results in gelatinous marrow transformation that is due to low blood cells. The severity of bone marrow damage and hypoplasia of all three blood cells is associated with reduced body weight. Thus, regarding our patient’s low BMI, it is not odd if her WBC and red blood cell (RBC) counts were low. Anemia can appear as microcytosis and macrocytosis, while the development of the latter is higher. Despite leukopenia, the overall rate of infection was not high (Walsh et al., 2020). Refeeding and weight gain can improve bone marrow status and blood cell counts. In our patient, the leukocyte counts gradually started to increase by refeeding, although severe anemia necessitated blood transfusion.
As Table 2 indicates, the platelets in our patient reached 433 on the eighth day, and 512 on the 14th day; after that, it gradually dropped and returned to normal. In AN patients, both thrombocytosis and thrombocytopenia are observed, although neither hemorrhage nor abnormal thrombosis is evidenced. In a study conducted by Sabel et al, 2013, out of 53 AN patients, 34% showed thrombosis, half of whom had thrombocytosis during hospitalization. In patients with high platelets, the maximum platelet level was 549 which occurred on the 13th day; those who experienced thrombocytosis during hospitalization experienced it on the 21st day on average. Sabel et al believed that, in the early stages of refeeding, thrombocytosis originated from bone marrow reconstruction, which is likely to improve in due time (Sabel et al, 2013).
Renal function
Urea and creatinine levels in patients with AN due to low intake of protein and muscle loss are at a minimum level than normal. Therefore, the highest levels of urea and creatinine denote dehydration (Winston, 2012).
Medical interventions
Treatment of AN is an interdisciplinary matter entailing the cooperation of various medical specialties. Treatment aims include treating medical problems, diet modifications, normalizing the patient’s body weight, correcting the patient’s overvalued attitudes toward body weight, body shape, and feed and finally, treating the associated psychiatric disorders (Sadock et al., 2015). The primary focus should be on stabilizing the medical conditions particularly, on fluid and electrolyte balance of the body, and then on weight gain and altering patients’ eating habits (Berends et al., 2012).
In these patients, the beginning of feeding is associated with the risk of refeeding syndrome. Five life-threatening complications of this syndrome include rhabdomyolysis, heart failure, respiratory failure, hemolysis, and convulsion (Cass et al., 2020). It also causes electrolyte disorder/disturbance, both hyper and hypoglycemia, acute reduction of thiamine and fluid, and electrolyte imbalance; therefore, replacement of thiamine and monitoring sugar and electrolytes are essential (Winston, 2012). Hypophosphatemia, hypokalemia, and hypomagnesemia occur in refeeding. The highest risk factor for developing this syndrome is low BMI; the lower the BMI, the higher the development of the refeeding syndrome (Cass et al., 2020).
Some recommend the beginning of the diet with 1500-1800 Kcal/day to be sustained for a few days and suggest increasing it after stabilization of the patient’s medical status by X100 Kcal every other day, ultimately reading 3500-4000 Kcal/day (Sadock et al., 2015). In conservative methods, to prevent the refeeding syndrome, the beginning rate is calculated by 10 Kcal per 1 k of body weight and it is added to 200-400 Kcal every 2-4 days; hence, weight gain of 3-4 pounds per week is acceptable (Cass et al., 2020).
In our patient (BMI=9.37), the risk of refeeding syndrome was assessed as high, and a more conservative method (feeding with fewer calories) was started. It is necessary to check daily amounts of phosphate and other electrolytes in the first 7-14 days. Hypophosphatemia occurs at the early phase of feeding and anabolism due to the use of phosphate and the construction of adenosine triphosphate. Also, hypokalemia and hypomagnesemia occur at early feeding stages due to increased cellular absorption of the electrolyte (Cass et al., 2020). Fortunately, in our patient, after correcting her minor hypokalemia, electrolytes remained normal up to the end. Regarding the patient’s early gastroparesis saturation, we included six meals, three main meals, and three low-volume meals in between in her diet.
In these patients, a lack of micronutrients, including thiamin, other types of vitamins B, and C, zinc, and copper are observed (Winston, 2012). Thus, medications containing these elements were prescribed for the present patient. Meanwhile, treatment with estrogen and progesterone was considered due to lowered bone density, amenorrhea, and lack of sex hormones in the present patient. Also, cabergoline was started due to hyperprolactinemia.
Patients with AN try to burn calories through excessive physical activity, but most medical interventions restrict such activities. However, exercises help improve patients’ muscle atrophy, bone density, quality of life, and mood. However, endurance training can help improve patients’ muscle atrophy, bone density, quality of life, and mood. Thus, we included light workouts, including stretching exercises for the present patient (Hughes et al., 2019).
Various medications, such as antidepressants, antipsychotics, and mood stabilizers, such as risperidone, aripiprazole, and fluoxetine have been used in the treatment of AN. The logic behind the use of all these drugs is their effects on the serotonergic system, which is conceived to play a role in the primary pathophysiology of AN. A meta-analysis by Sidar et al. has determined the efficacy of olanzapine on the treatment of this disorder and patients’ weight gain; its dosage above 5 mg showed higher efficacy levels. However, in patients with AN, care must be taken to control complications, such as neuroleptic malignant syndrome (NMS), hypoglycemia, and heart block (Sidar et al., 2020). In this patient, olanzapine was used for medical therapy, applied from the beginning together with supportive psychotherapy and psychoeducation to enhance weight gain and the patient’s cooperation.
The use of anti-depressant selective serotonin reuptake inhibitors (SSRIs) is not recommended except for comorbidity (Sadock et al., 2015), and this patient, it was started after initial weight gain due to the comorbidity of AN with obsessive disorder. Bupropion is not used due to its convulsive effect. No evidence of the beneficial effects of tricyclic antidepressants (TCA) and monoamine oxidase inhibitors (MAOI) is found (Sidar et al., 2020).
Studies with the highest efficiency are mostly associated with cognitive behavioral therapy, although several studies have also shown similar efficiency of interpersonal and psychoanalysis focal studies. In adolescents, the highest frequency and efficiency of studies are reported with family-based therapy. In cognitive behavioral therapy, after effective communication and motivation, changes are observed after 20-40 sessions within four therapy stages. In the first stage, correcting the patient’s eating habits is in perspective. In the second stage, re-assessing and rewarding the patient for positive changes are done together with examining the underlying causes of unchanged behaviors. In the third or the main stage of treatment, the overvalued thoughts about body weight and shape are corrected. Throughout this stage, if perfectionism, low self-confidence, and disturbed interpersonal relationships are diagnosed to underlie the overvalued thoughts about body weight and shape, the therapy sessions will focus on correcting them. In the last stage, measures are taken to prevent the relapse of the disorder (Elwyn et al., 2020).
Prognosis
Complete recovery in 30% to 60% of cases, residual recovery in 20%, and unremitting recovery in 20% have been reported (Cass et al., 2020). The highest mortality and relapse of psychiatric disorders occur in AN patients, and long-term recovery occurs in less than 50% of patients (Phillipou et al., 2019) so that 30% to 50% of hospitalized patients successfully treated will still experience relapse of the disorder. Its relapse is particularly common in the first two years after treatment (Berends et al., 2012). The rate of mortality (5%) is higher than any psychiatric disorder. Suicide in these patients becomes more likely, and the cause of death in these patients is wither medical side-effects of suicide. Most medical side effects relapse after weight gain while only two complications are irreversible, low bone density and cognitive disorder (Cass et al., 2020).
Conclusion
In sum, three points are considered in this case. First, despite the patient’s extreme weight loss, her abstinence from eating did not originate in her perceived body image; rather, she was highly obsessed with an overeating complication the way afflicted her father; this may signal clinicians not to rely on such misconceptions for diagnosis necessarily. Second, the relationship between AN with hyperprolactinoma and pituitary microadenoma is observed; such a relationship may shape a line of research for the psychopathology of AN by the categorization of the disorder into with or without hyperprolactinemia. Third, regarding the patient’s refeeding, low-calorie intake was considered according to the latest guidelines, which prevented relevant complications and caused the patient’s optimal compliance with treatment.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, supervision and data collection:: Mohammadreza Shegafr Nakhaei; Methodology: Sayedeh Elham Sharafi; Investigation and writing: All authors; Data analysis: Sayedeh Ekham Sharafi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the officials of Imam Khomeini Hospital who helped in conducting this research
References
Anorexia nervosa (AN), first described by Sir William Withey Gull in 1968 (Crumby et al., 2024), is a severe psychiatric disorder, in which an individual abstains from keeping their weight at a minimum proportionate to their height and age; accordingly, they start to suffer from severe weight loss and disturbed physical and psychosocial functioning (Berends et al., 2012). Long starvation periods lead to adaptive changes in most physiologic systems. Some cases manage to lose weight by restricting their diet while others resort to behaviors, such as binging, vomiting, and use of laxatives (the binge-eating and purging type) (Salvato et al., 2024).
AN was previously diagnosed and reported in Western countries but its prevalence is on the rise in other countries (Demarque et al., 2015). Reports suggest that its prevalence ascends the cross-cultural borders. Although there are cultural differences between traditional and Western communities, several factors increase the prevalence of the disorder in non-Western countries, exposure to modern trade experiences in the West, globalization effects via facilitated cross-continental voyages, and use of social media (Qadan, 2009).
People with anorexia often have a strong fear of gaining weight and may think they are overweight, even when they are thin. To prevent weight gain or continue to lose weight, people with anorexia often limit the amount or type of food they eat. They place a high value on controlling their weight and shape and use extreme efforts that can greatly harm their lives. Anorexia, like other eating disorders, can take over people’s lives and be very hard to overcome. Because it is related to changes in the brain, anorexia behaviors are not choices, and the illness is not about food or looking a certain way. With proven treatment, people with anorexia can return to a healthy weight, develop more balanced eating habits, and reverse some of anorexia’s serious medical and mental health complications (Holtom-Viesel et al., 2014).
In a Middle Eastern country like Iran, the prevalence of AN among female high school students in Tehran City, the capital of Iran, in 2000 was reported as 0.09% (Nobakht, 2000). In 2015, its prevalence among adolescents in Northeast Iran was 1.2% (Rauof et al., 2015). Comparably, its prevalence in the West ranges from 1.2% to 2.2% (Jagielska, 2017). Therefore, while unexpected from an Eastern community, the Iranian community appears much like the Western communities as far as the prevalence of AN is concerned. However, the disorder is less recognized in Iran and the health system is less prepared for screening and timely diagnosis of AN. Therefore, we decided to report a severe case of AN who was admitted and hospitalized in the largest educational hospital in Tehran City.
Materials and Methods
A single, educated master of industrial engineering 32-year-old female patient was admitted with a locked knee, weakness, and lethargy, and hospitalized in the hematology ward due to electrolyte and hematological complications. She was then referred to the psychiatric service due to her extremely low weight.
She completely refused her admission to the psychosomatic ward but accepted starting her treatment after assurance and the doctor’s promise to request a medical consultation for her musculoskeletal problems. She appeared highly guarded in providing a medical history. However, successive interview attempts gradually brought more information about her. She revealed that symptoms began 10 years ago following her father’s disease (who suffered a hematologic complication involving his spleen and used warfarin. From then on, she abstained from eating with her family members and decreased her food intake to a minimum; for instance, she ate 2-3 spoons for lunch and dinner; she recently ate only one meal during the day. She has avoided cooked food for the past 1-2 year and adopted a vegetarian diet only, including half a courgetti, one tomato, and one cucumber. She believes that her father suffered from overeating, and blames others for eating. Neither intentional vomiting nor periodical overeating was reported. During the past two years, her weight has dropped from 51 kg to 36 kg; it minimized to 24 kg due to strict restrictions on food intake. She stated that she could not get up without help but could walk independently. Despite her height (160 cm) and body mass index (BMI) (9.37), she expressed her satisfaction with her weight.
Her history showed no psychotic and mood signs, self-harm, and suicide. She reported normal sleeping patterns, no smoking, nor using alcohol but reported both symmetry obsessions and compulsion to over-wash things, exacerbated during the past year. She was worried about her physical health and frequently had complete blood count (CBC) tests every three months.
In psychiatric examination, she pretends to be normal and avoids discussing her weight and nutrition. Her mood is described as mostly normal but occasionally irritable. She is worried about her health and accepts her compulsion to repeatedly wash the house yard, take frequent showers, longer stay in the toilet, and obsession with ordering things, such as the perfect folding of her clothes. Aggravated obsession has been reported since the last year. She is neither psychotic nor suicidal. Her consciousness, orientation, and cognitive status are normal.
Digestive problems and malignancy were rejected, and the diagnostic and statistical manual of mental disorders, fifth edition (DSM-5) diagnostic criteria led us to extreme AN (restricting type) diagnosis. Upon admission, the patient avoided her prescribed regimen meals, abundantly drank tea and liquid, ate ample fruit, stored and neatly piled up edibles from other patients in her locker, showed distress to eat in front of others, and got agonized upon nutrition plan control by the doctor or medical personnel. However, these behaviors started to fade away during her stay in the ward.
Laboratory test results
Electrolyte levels were measured at the beginning and periods. Upon nephrology consultation, treatment was initiated with potassium chloride (KCl) 15% due to mild hypokalemia. Also, oral Calcium + D was prescribed. After diet prescription and the likelihood of hypophosphatemia, successive measurements revealed no drop in phosphate level. Table 1 presents changes in electrolyte levels.

Tables 2 and 3 present the results of CBC tests, blood indexes, iron, reserves, and peripheral blood smear (PBS).

Hematological consultation was requested due to anemia and leukopenia, and two units of packed cells were injected due to a drop in hemoglobin levels. Figure 1 shows subsequent changes after injection.

Regarding bicytopenia and PBS, myeloid dysplasia with malnutrition was observed and medical prescriptions included daily injection of B12 100 mg up to 7 days and then weekly, daily B6 tablets 400 mg, daily B1 300 mg, daily folic acid 5 mg, and daily multivitamin.

Table 4 presents an evaluation of vitamins at the beginning and one month after the treatment.

Endocrine consultation was requested due to the patient’s amenorrhea and high prolactin level. The results of hormonal tests (Tables 5 and 6) showed that sex hormones and gonadotropin were low. Successive tests also revealed that prolactin levels were high; insulin-like growth factor-1 (IGF-1), leptin, and anti-Müllerian hormone were low; corticotropin-releasing hormone (CRH) was at the highest normal level; however, parathormone, thyroid hormones, and cortisol were normal.
Dual x-ray absorptiometry (DXA) bone densitometry using LEXXOS densitometer revealed a lower density score than the score expected for her age (lumbar region Z score was -4.1). Based on her amenorrhea, osteoporosis, and hormonal test results, she was prescribed to take estradiol conjugated 0.625 from day 1 to day 25 of menstruation as well as medroxyprogesterone 10 mg from day 16 to day 25 of menstruation. In addition, a D3 injection every two weeks and daily calcium+D oral were also prescribed.
Therapeutic measures
Following hyperprolactinemia, a magnetic resonance imaging (MRI) of the brain without contrast was requested to examine hypophysis, which reported a lesion of 7.5 mm to the right of the hypophysis and mild bulge in the right with some mild deviation of hypophysis stem to the left, contributing to pituitary microadenoma diagnosis. Accordingly, a weekly oral tablet of cabergoline 0.5 was initiated for hyperprolactinemia and pituitary microadenoma. Pelvic and abdominal ultrasound imaging were normal. Computed tomography (CT) scan of the area did not render anything abnormal. Electrocardiogram (EKG) at the beginning of treatment was normal, QTc=430 ms; successive EKS also were normal. Kidney and liver functions were normal, too.
The next goal was to correct the diet and weight gain. Due to her initial low weight and avoidance of oral intake, she was given a daily venous feed of amino acid 5% and intralipid 500-700 Kcal. After the patient started to cooperate, 6 oral daily meals containing 500-700 Kcal, including peptiamine three times a day, drug administration and food intake were carefully supervised, and the patient was forbidden to go to the toilet two hours after each meal to prevent the likelihood of intentional vomiting.
Based on the patient’s chief complaint (i.e. musculoskeletal problems, such as inability to get up and sit, and locked knee), sports medicine consultation was requested. Despite the patient’s initial resistance to treatment, acceptance of supportive psychotherapy was suggested by active listening and empathy with the patient’s medical problems. After medical communication to enhance her motivation, we presented psycho-education on the diagnosis and complications of her disease and the likelihood of more serious complications in the future, if left untreated.
A psychotropic medication used at the beginning was olanzapine with a primary dose of 2.5 mg each night, which resulted in her lessened resistance to treatment and irritability and enhanced cooperation; with the patient’s acceptance, the dosage gradually increased to 7.5 mg daily for the first week, and 10 mg daily for the second week. During the second month of hospitalization and due to the patient’s obsessive-compulsive disorder signs, sertraline 12.5 mg was started; the dosage gradually increased to 25 mg daily. The patient’s weight gradually increased from 24 kg to 17.5 kg during her 45-day hospitalization. Considering her height (160 cm), Table 7 and Figure 2 show her BMI changes during the treatment.


Considering the stability of medical status and electrolyte disorders at the very beginning of treatment, mood improvement, dietary behaviors, the patient’s relatively appropriate cooperation with the therapists, improvement in the patient’s attitude towards her disease and its complications, concerns about the COVID-19 contagion, the patient’s and her family’s stress on continuing the rest of treatment at home, she was discharged with BMI=10.74, and the rest of the treatments were left to be followed up as outpatients.
Discussion
The patient’s problem started at the age of 22 years with signs of retarded menstruation and puberty at an earlier age. Studies also show most patients are young and adolescent cases, the period of life in which they encounter stressors of puberty, socializing, and starting independent lives (Gonidakis et al., 2014, Cuspidi et al., 2024). Lock believes that adolescence is the beginning of major brain development; therefore, anorexia and subsequent complications cause serious damage to this process (Hurst et al., 2015). This disorder mainly affects women, although it may be observed in men and other age periods (Berends et al., 2012).
Etiology and diagnosis
In this case, her avoidance of feeding was not due to fear of fatphobia, rather she abstained from food for the fear of a disease that her father suffered from and she felt it was due to overeating. Some researchers believe that the clinical presentations of this disorder in non-Western ethnicities, such as Caucasians are different from those observed in Europe and North America. For instance, they contend that fatphobia may not be the main reason for AN in the East and those other causes, such as digestive, and diseases can be the reason to avoid eating food. In 2013, a 14-year-old boy was reported whose food abstinence was due to digestive problems after eating fried and packaged food (Paul et al., 2013). Another study reported 70 Chinese patients with AN, 595 of whom did not have fatphobia; rather, they stated other reasons, such as gastrointestinal problems as the main reason to avoid food (Dani et al., 2024). Probably, it is due to such reports that persistent behavior that interferes with weight gain is added to criterion B in the diagnostic and statistical manual of mental disorders, fifth edition (DSM-5) (Demarque et al., 2015). The patient’s BMI (9.37) represented an extreme form of AN, which urgently required her hospitalization to control her medical complications (Cass et al., 2020).
Etiology
Biological, psychological, and sociocultural factors play a role in causing symptoms of AN, but environmental factors have been the focus of researchers’ attention (Phillipou et al., 2019). Biologically, the prevalence rate in the immediate family members of the patient is 10 times that of the normal population (Cass et al., 2020). In this patient, family history was negative but traces of anxiety and obsessive disorders seemed likely in her mother. Today, scholars consider family dysfunction not as an etiologic factor but as a perpetuating factor for symptoms of AN (Martini et al., 2024). Regarding the onset of the disorder in early adolescence, psychological, social, and biological factors of adolescence can appear as one possible etiological factor of the disorder (Martini et al., 2024), which was witnessed in the patient we described as delayed menstruation and hyperprolactinemia at puberty. Also, co-morbidities of obsessive-compulsive disorder, major depressive disorder, and various anxiety disorders are in perspective (Wonderlich et al., 2024), which appears as uncontrolled washing, and frequent CBC check-ups.
Electrolyte disorders
Hyponatremia is likely to occur in AN, which results from the patient’s desire to drink liquids to show a false feeling of weight gain. Other causes may include kidney failure to excrete enough water and, quite rarely, syndrome of inappropriate antidiuretic hormone (SIADH) (Cass et al., 2020). However, the most common electrolyte disorders of AN are hypokalemia. The patients’ intake of magnesium is remarkably low, and hypomagnesemia occurs either before or during re-feeding. Hypomagnesemia is often caused by hydration through venous saline infusion and magnesium elimination; it may occur simultaneously with hypokalemia and it becomes necessary to measure magnesium levels in the blood in case of resistant hypokalemia. Also, hypocalcemia may occur both in hunger and re-feeding, which may be caused by giving phosphate to patients during refeeding. It may be due to hypomagnesemia (Winston, 2012). Fortunately, in this case, the only electrolyte disorder we encountered was hypokalemia, which was successfully controlled early in the treatment, and no other disorder was observed at the initial or later stages of refeeding.
Cardiopulmonary disorders
Patients with the restricting type of AN suffer from recurring cardiopulmonary disorders. Mitral valve prolapses due to cardiac atrophy occur in 25% of cases, which manifest as palpitation, vertigo, and dyspnea. The most common arrhythmia is sinus bradycardia, which is caused mainly by increased vague tone due to malnutrition. Systolic blood pressure is normally under 100 mm Hg. Cardiac sudden death occurs due to prolonged QT interval, caused by medical and electrolyte disorders. Low cardiac output occurs in response to myocardial atrophy due to malnutrition. In addition, weak respiratory muscles and diaphragm weakness have a role in patients’ dyspnea (Cass et al., 2020). In the present case, no problem was observed in the cardiologic consultation, and ECG, heartbeats and blood pressure were normal.
Endocrine disorders
Multiple endocrine changes occur in patients with the restricting type of AN to adapt to the energy intake of the body (Cass et al., 2020). The level of hormone regulating the appetite alters in such a way that leptin decreases and ghrelin increases. The function of leptin is to regulate energy homeostasis and food intake in proportion with the body weight so that its secretion increases with fat and weight gain in a normal person; leptin directly inhibits the appetite-stimulating effects of neuropeptide Y, resulting in declined appetite. A significant reduction of lipids and leptin in the blood is observed in patients with AN. Genome-wide association studies have determined high-risk genome spots of AN incidence related to leptin dysregulation; thus, it may function as a potential biomarker in screening AN (Kim et al., 2020). Secreted predominantly from the stomach, ghrelin is a peptide with profound or exogenic properties and stimulates the growth hormone. Researchers believe that it is a brain-gut peptide and has a role in regulating body energy. Several studies have been conducted on the effects of ghrelin in AN patients; these studies have reported higher levels of ghrelin in these patients than in normal persons. It increases the secretion of prolactin, adrenocorticotropic hormone (ACTH), and cortisol (Salvato et al., 2024). Prolactin serum levels in AN patients varied from normal, to mildly increased, and increased, but no relationship was observed between low body weight and prolactin levels (Wonderlich et al., 2024). In this case, the leptin level was very low 0.1 ng/mL (the normal range is 2.5-21.8 ng/mL); also, hyperprolactinemia was observed and reported in the context of pituitary microadenoma. It seems that further investigation is required to find a relationship between AN and prolactin levels in the blood as either a disorder or a biomarker of the disorder. Probably, we face various biological types of AN, in some of which increased prolactin levels are observed (Jagielska, 2017).
Normal menses show increased bone density and the relationship is independent of the patient’s weight change. It suggests the role of hypogonadism in lowered bone density (Salvato et al., 2024). In earlier studies, 17.6% to 88% of patients with AN had low vitamin D levels but their intact parathyroid hormone (PTH) was relatively normal. As indicated in Table 5, in our patient, the parathormone level was 46.2, which is normal. In research by Lenherr-Taube et al., almost one-third of adolescents with AN had normal PTH levels; and they concluded that PTH may be age-dependent (Lenherr-Taube et al., 2020).
Increased levels of growth hormone in the blood, reduced IGF-1, and resistance to the effects of growth hormone are visible in AN patients, which may be attributable to the role of this hormone in lipolysis (Crumby et al., 2024). In our patient, the blood levels of IGF-1 were lower than the normal values. Hypogonadotropic hypogonadism (low luteinizing hormone [LH], follicle-stimulating hormone [FSH], and estradiol) and amenorrhea due to hypothalamus-pituitary axis dysfunction occur in 85% of patients (Cass et al., 2020). In our patient, low luteinizing hormone [LH], follicle-stimulating hormone (FSH) and estradiol were reported.
Patients with AN are affected with more infertility and more labor complications than the normal population. Normally, fertility is negatively correlated with age. Some diseases lead to the early reduction of follicle count, termed the early reduction of ovarian reserve. Anti-Müllerian hormone (AMH) is produced by granulosa cells from the small follicles in a woman’s ovaries and is used as a marker of oocyte quantity. It reaches its maximum in women’s third decade of life and is not measurable after menopause. Its low level may show reduced response of ovaries to stimuli and lowers the likelihood of pregnancy. AMH is higher than normal in patients with AN (4.7 vs 3.2 ng/mL) and in 19.6% of patients with AN, AMH levels are higher than the normal range (>6.78). Therefore, AMH levels are either normal or increased in AN patients; and its reduction means early reduction of ovarian reserve and should not be attributed solely to malnutrition (Pitts et al., 2020). As indicated in Table 5, the AMH level in our patient was 0.6 ng/mL, below the normal range.
Hypoglycemia is common. Hypercholesterolemia is also common but its significance in predisposing the patient to cardiovascular diseases is unknown. Increased salivary amylase production is a cause of the patient’s latent vomiting but normal amylase does not reject vomiting. In our patient, the amylase level was normal.
Hypercarotenemia leads to the alteration of orange skin color, which is not to be mistaken with icterus. Its etiology is unknown and may be attributable to the overuse of vegetables and fruit in some cases (Winston, 2012). In the present case, her yellowish skin color gradually decreased upon admission due to the weight loss.
Deficiency of micronutrients
Most patients with AN tend to lower their intake of micronutrients, including zinc, copper, vitamin C, riboflavin, and vitamin B2. Thiamin deficiency occurs in 38% of cases; due to its importance in carbohydrate metabolism, its deficiency is associated with cognitive defects. Also, taste changes and neuropsychiatric symptoms appear following zinc deficiency (Winston, 2012). In the case of our patient, despite her aggravated condition, blood levels of folic acid, vitamin B12, and D3 were in the normal range (Table 3), which may account for the patient’s tendency to use sufficient amounts of salts and vitamins despite her abstinence from high-calorie foods.
Gastrointestinal complications
In 50% of AN patients, gastrointestinal complications occur in the form of satiety, early or feeling full, abdominal distension, pain, and nausea. Nasopharyngeal muscle weakness causes dysphagia, coughing while eating, and aspiration. Gastroparesis is a barrier against refeeding because it brings about early satiety. Delayed colon discharge and constipation affect two-thirds of patients (Cass et al., 2020). Similarly, our patient also reported feeling full at the beginning of refeeding; she often complained of constipation from the early days of hospitalization but further examination revealed that she had no serious complaints of defecation and stool consistency; rather, frequency of defecation was low due to poor nutrition, but tended to improve through improved nutritional status.
In 50% of patients, increased level of aminotransferase enzymes from the liver is evidenced throughout refeeding. Type 1 occurs due to hepatic ischemia and hypoperfusion, hepatocyte autophagy, and glutathione synthetase deficiency, which tend to be cured by feeding. However, type 2 is a result of steatohepatitis and requires a lowered intake of fat and carbohydrates (Winston, 2012). In our patient, test results indicated no increase in the levels of these enzymes.
Albumin levels in these patients are usually normal even in patients with severe malnutrition. If hyperalbuminemia occurs, it may be due to factors other than malnutrition, such as infection, and bears a bad prognosis (Winston, 2012). In our patient, the albumin level was normal.
Neurological complications
Both the central and peripheral nervous systems are affected by AN. The white and grey matter are affected in central nervous system (CNS), leading to cognitive disorders that may persist even after treatment. Also, thalamus dysfunction results in thermal dysregulation and hypothermia, as well as smelling and taste disturbance. Also, neuropraxia (i.e. focal demyelination without damage to nerve continuity) develops as a result of damage to subcutaneous peripheral nerves, which occasionally causes foot drop and local hand weakness; but these peripheral complications are reversible (Cass et al., 2020). In the present patient, no evidence of cognitive disorders was found. Upon neurologic examination, no serious pathologic finding was found except weakness of the lower limbs and her inability to get up. Her brain’s MRI reveals no significant result except pituitary microadenoma.
Hematological complications
The prevalence of anemia, thrombocytopenia, and leukopenia in AN patients is 16.4%, 7.4%, and 50.5%, respectively. As can be seen, low white blood cell (WBC) is more prevalent than other complications. Replacement of saccharides with bone marrow lipids results in gelatinous marrow transformation that is due to low blood cells. The severity of bone marrow damage and hypoplasia of all three blood cells is associated with reduced body weight. Thus, regarding our patient’s low BMI, it is not odd if her WBC and red blood cell (RBC) counts were low. Anemia can appear as microcytosis and macrocytosis, while the development of the latter is higher. Despite leukopenia, the overall rate of infection was not high (Walsh et al., 2020). Refeeding and weight gain can improve bone marrow status and blood cell counts. In our patient, the leukocyte counts gradually started to increase by refeeding, although severe anemia necessitated blood transfusion.
As Table 2 indicates, the platelets in our patient reached 433 on the eighth day, and 512 on the 14th day; after that, it gradually dropped and returned to normal. In AN patients, both thrombocytosis and thrombocytopenia are observed, although neither hemorrhage nor abnormal thrombosis is evidenced. In a study conducted by Sabel et al, 2013, out of 53 AN patients, 34% showed thrombosis, half of whom had thrombocytosis during hospitalization. In patients with high platelets, the maximum platelet level was 549 which occurred on the 13th day; those who experienced thrombocytosis during hospitalization experienced it on the 21st day on average. Sabel et al believed that, in the early stages of refeeding, thrombocytosis originated from bone marrow reconstruction, which is likely to improve in due time (Sabel et al, 2013).
Renal function
Urea and creatinine levels in patients with AN due to low intake of protein and muscle loss are at a minimum level than normal. Therefore, the highest levels of urea and creatinine denote dehydration (Winston, 2012).
Medical interventions
Treatment of AN is an interdisciplinary matter entailing the cooperation of various medical specialties. Treatment aims include treating medical problems, diet modifications, normalizing the patient’s body weight, correcting the patient’s overvalued attitudes toward body weight, body shape, and feed and finally, treating the associated psychiatric disorders (Sadock et al., 2015). The primary focus should be on stabilizing the medical conditions particularly, on fluid and electrolyte balance of the body, and then on weight gain and altering patients’ eating habits (Berends et al., 2012).
In these patients, the beginning of feeding is associated with the risk of refeeding syndrome. Five life-threatening complications of this syndrome include rhabdomyolysis, heart failure, respiratory failure, hemolysis, and convulsion (Cass et al., 2020). It also causes electrolyte disorder/disturbance, both hyper and hypoglycemia, acute reduction of thiamine and fluid, and electrolyte imbalance; therefore, replacement of thiamine and monitoring sugar and electrolytes are essential (Winston, 2012). Hypophosphatemia, hypokalemia, and hypomagnesemia occur in refeeding. The highest risk factor for developing this syndrome is low BMI; the lower the BMI, the higher the development of the refeeding syndrome (Cass et al., 2020).
Some recommend the beginning of the diet with 1500-1800 Kcal/day to be sustained for a few days and suggest increasing it after stabilization of the patient’s medical status by X100 Kcal every other day, ultimately reading 3500-4000 Kcal/day (Sadock et al., 2015). In conservative methods, to prevent the refeeding syndrome, the beginning rate is calculated by 10 Kcal per 1 k of body weight and it is added to 200-400 Kcal every 2-4 days; hence, weight gain of 3-4 pounds per week is acceptable (Cass et al., 2020).
In our patient (BMI=9.37), the risk of refeeding syndrome was assessed as high, and a more conservative method (feeding with fewer calories) was started. It is necessary to check daily amounts of phosphate and other electrolytes in the first 7-14 days. Hypophosphatemia occurs at the early phase of feeding and anabolism due to the use of phosphate and the construction of adenosine triphosphate. Also, hypokalemia and hypomagnesemia occur at early feeding stages due to increased cellular absorption of the electrolyte (Cass et al., 2020). Fortunately, in our patient, after correcting her minor hypokalemia, electrolytes remained normal up to the end. Regarding the patient’s early gastroparesis saturation, we included six meals, three main meals, and three low-volume meals in between in her diet.
In these patients, a lack of micronutrients, including thiamin, other types of vitamins B, and C, zinc, and copper are observed (Winston, 2012). Thus, medications containing these elements were prescribed for the present patient. Meanwhile, treatment with estrogen and progesterone was considered due to lowered bone density, amenorrhea, and lack of sex hormones in the present patient. Also, cabergoline was started due to hyperprolactinemia.
Patients with AN try to burn calories through excessive physical activity, but most medical interventions restrict such activities. However, exercises help improve patients’ muscle atrophy, bone density, quality of life, and mood. However, endurance training can help improve patients’ muscle atrophy, bone density, quality of life, and mood. Thus, we included light workouts, including stretching exercises for the present patient (Hughes et al., 2019).
Various medications, such as antidepressants, antipsychotics, and mood stabilizers, such as risperidone, aripiprazole, and fluoxetine have been used in the treatment of AN. The logic behind the use of all these drugs is their effects on the serotonergic system, which is conceived to play a role in the primary pathophysiology of AN. A meta-analysis by Sidar et al. has determined the efficacy of olanzapine on the treatment of this disorder and patients’ weight gain; its dosage above 5 mg showed higher efficacy levels. However, in patients with AN, care must be taken to control complications, such as neuroleptic malignant syndrome (NMS), hypoglycemia, and heart block (Sidar et al., 2020). In this patient, olanzapine was used for medical therapy, applied from the beginning together with supportive psychotherapy and psychoeducation to enhance weight gain and the patient’s cooperation.
The use of anti-depressant selective serotonin reuptake inhibitors (SSRIs) is not recommended except for comorbidity (Sadock et al., 2015), and this patient, it was started after initial weight gain due to the comorbidity of AN with obsessive disorder. Bupropion is not used due to its convulsive effect. No evidence of the beneficial effects of tricyclic antidepressants (TCA) and monoamine oxidase inhibitors (MAOI) is found (Sidar et al., 2020).
Studies with the highest efficiency are mostly associated with cognitive behavioral therapy, although several studies have also shown similar efficiency of interpersonal and psychoanalysis focal studies. In adolescents, the highest frequency and efficiency of studies are reported with family-based therapy. In cognitive behavioral therapy, after effective communication and motivation, changes are observed after 20-40 sessions within four therapy stages. In the first stage, correcting the patient’s eating habits is in perspective. In the second stage, re-assessing and rewarding the patient for positive changes are done together with examining the underlying causes of unchanged behaviors. In the third or the main stage of treatment, the overvalued thoughts about body weight and shape are corrected. Throughout this stage, if perfectionism, low self-confidence, and disturbed interpersonal relationships are diagnosed to underlie the overvalued thoughts about body weight and shape, the therapy sessions will focus on correcting them. In the last stage, measures are taken to prevent the relapse of the disorder (Elwyn et al., 2020).
Prognosis
Complete recovery in 30% to 60% of cases, residual recovery in 20%, and unremitting recovery in 20% have been reported (Cass et al., 2020). The highest mortality and relapse of psychiatric disorders occur in AN patients, and long-term recovery occurs in less than 50% of patients (Phillipou et al., 2019) so that 30% to 50% of hospitalized patients successfully treated will still experience relapse of the disorder. Its relapse is particularly common in the first two years after treatment (Berends et al., 2012). The rate of mortality (5%) is higher than any psychiatric disorder. Suicide in these patients becomes more likely, and the cause of death in these patients is wither medical side-effects of suicide. Most medical side effects relapse after weight gain while only two complications are irreversible, low bone density and cognitive disorder (Cass et al., 2020).
Conclusion
In sum, three points are considered in this case. First, despite the patient’s extreme weight loss, her abstinence from eating did not originate in her perceived body image; rather, she was highly obsessed with an overeating complication the way afflicted her father; this may signal clinicians not to rely on such misconceptions for diagnosis necessarily. Second, the relationship between AN with hyperprolactinoma and pituitary microadenoma is observed; such a relationship may shape a line of research for the psychopathology of AN by the categorization of the disorder into with or without hyperprolactinemia. Third, regarding the patient’s refeeding, low-calorie intake was considered according to the latest guidelines, which prevented relevant complications and caused the patient’s optimal compliance with treatment.
Ethical Considerations
Compliance with ethical guidelines
There were no ethical considerations to be considered in this research.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, supervision and data collection:: Mohammadreza Shegafr Nakhaei; Methodology: Sayedeh Elham Sharafi; Investigation and writing: All authors; Data analysis: Sayedeh Ekham Sharafi.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank the officials of Imam Khomeini Hospital who helped in conducting this research
References
Berends, T., van Meijel, B., & van Elburg, A. (2012). The Anorexia Relapse Prevention Guidelines in practice: A case report. Perspectives in Psychiatric Care, 48(3), 149–155. [DOI:10.1111/j.1744-6163.2011.00322.x] [PMID]
Cass, K., McGuire, C., Bjork, I., Sobotka, N., Walsh, K., & Mehler, P. S. (2020). Medical complications of anorexia nervosa. Psychosomatics, 61(6), 625–631. [DOI:10.1016/j.psym.2020.06.020] [PMID]
Crumby, E., Penwell, T. E., Butler, R. M., Ortiz, A. M. L., Fitterman-Harris, H. F., & Levinson, C. A. (2024). Does response to treatment differ between anorexia nervosa and atypical anorexia nervosa? Findings from two open series trials. Journal of Affective Disorders, 365, 451–458. [DOI:10.1016/j.jad.2024.08.115] [PMID]
Dani, C., Tarchi, L., Cassioli, E., Rossi, E., Merola, G. P., & Ficola, A., et al. (2024). A transdiagnostic and diagnostic-specific approach on inflammatory biomarkers in eating disorders: A meta-analysis and systematic review. Psychiatry Research, 340, 116115. [DOI:10.1016/j.psychres.2024.116115] [PMID]
Demarque, M., Guzman, G., Morrison, E., Ahovi, J., Moro, M. R., & Blanchet-Collet, C. (2015). Anorexia nervosa in a girl of Chinese origin: Psychological, somatic and transcultural factors. Clinical Child Psychology and Psychiatry, 20(2), 276-288. [DOI:10.1177/1359104513514067] [PMID]
Elwyn, R., Williams, M., Smith, E., & Smith, S. (2024). Two identical twin pairs discordant for longstanding anorexia nervosa and OSFED: Lived experience accounts of eating disorder and recovery processes. Journal of Eating Disorders, 12(1), 127. [DOI:10.1186/s40337-024-01078-w] [PMID]
Gherbesi, E., Faggiano, A., Sala, C., Carugo, S., Grassi, G., & Cuspidi, C., et al. (2024). Myocardial mechanics in anorexia nervosa: A systematic review and meta-analysis of speckle tracking echocardiographic studies. Journal of Cardiovascular Medicine (Hagerstown, Md.), 25(10), 740–748. [DOI:10.2459/JCM.0000000000001661] [PMID]
Gonidakis, F., Georgantopoulos, G., Konstantakopoulos, G., & Varsou, E. (2014). Late onset anorexia nervosa and the role of parental family. Presentation of two cases. Eating and Weight Disorders: EWD, 19(3), 409–412. [DOI:10.1007/s40519-014-0098-3] [PMID]
Holtom-Viesel, A., & Allan, S. (2014). A systematic review of the literature on family functioning across all eating disorder diagnoses in comparison to control families. Clinical Psychology Review, 34(1), 29-43. [DOI:10.1016/j.cpr.2013.10.005] [PMID]
Hughes, K., Woodgate, D., Halford, S. J., Cowan, M., & Himmerich, H. (2019). The therapeutic effect of physical activity in a Day-Hospital patient with Anorexia nervosa. Psychiatria Danubina, 31(2), 201-203. [DOI:10.24869/psyd.2019.201] [PMID]
Hurst, K., & Zimmer-Gembeck, M. (2015). Focus on perfectionism in female adolescent anorexia nervosa. International Journal of Eating Disorders, 48(7), 936-941. [DOI:10.1002/eat.22417] [PMID]
Jagielska, G., & Kacperska, I. (2017). Outcome, comorbidity and prognosis in anorexia nervosa. Psychiatria Polska, 51(2), 205–218. [DOI:10.12740/PP/64580] [PMID]
Kim, Y., Hersch, J., Bodell, L. P., Schebendach, J., Hildebrandt, T., & Walsh, B. T., et al. (2021). The association between leptin and weight maintenance outcome in anorexia nervosa. The International Journal of Eating Disorders, 54(4), 527–534.[DOI:10.1002/eat.23407] [PMID]
Lenherr-Taube, N., Trajcevski, K., Sochett, E., & Katzman, D. K. (2020). Low PTH levels in adolescents with anorexia nervosa. Frontiers in Pediatrics, 8, 99. [DOI:10.3389/fped.2020.00099] [PMID]
Martini, M., Longo, P., Toppino, F., De Bacco, C., Preti, A., & Abbate-Daga, G., et al. (2024). The structure of motivation: Assessing readiness to change dimensions and their predictive value with the network validation of the Italian version of the Anorexia Nervosa Stages of Change Questionnarie. European Eating Disorders Review: The Journal of the Eating Disorders Association, 10.1002/erv.3133. [DOI:10.1002/erv.3133] [PMID]
Nobakht, M., & Dezhkam, M. (2000). An epidemiological study of eating disorders in Iran. The International Journal of Eating Disorders, 28(3), 265–271. [DOI:10.1002/1098-108x(200011)28:3<265::aid-eat3>3.0.co;2-l] [PMID]
Paul, P., Mehta, S., & Coffey, B. J. (2013). Anorexia nervosa in a 14-year-old second-generation hispanic adolescent boy. Journal of Child and Adolescent Psychopharmacology, 23(4), 295-299. [DOI:10.1089/cap.2013.2343] [PMID]
Phillipou, A., Musić, S., & Lee Rossell, S. (2019). A biopsychosocial proposal to progress the field of anorexia nervosa. The Australian and New Zealand journal of psychiatry, 53(12), 1145–1147.[DOI:10.1177/0004867419849487] [PMID]
Pitts, S., Dahlberg, S. E., Gallagher, J. S., Gordon, C. M., & DiVasta, A. D. (2021). is ovarian reserve impacted in anorexia nervosa? Journal of Pediatric and Adolescent Gynecology, 34(2), 196–202. [DOI:10.1016/j.jpag.2020.11.021] [PMID]
Qadan, L. (2009). Anorexia nervosa: Beyond boundaries. International Journal of Eating Disorders, 42(5), 479-481. [DOI:10.1002/eat.20641] [PMID]
Rauof, M., Ebrahimi, H., Asghari Jafarabadi, M., Malek, A., & Babapour Kheiroddin, J. (2015). Prevalence of eating disorders among adolescents in the Northwest of Iran. Iranian Red Crescent Medical Journal, 17(10), e19331. [DOI:10.5812/ircmj.19331] [PMID]
Sabel, A. L., Gaudiani, J. L., Statland, B., & Mehler, P. S. (2013). Hematological abnormalities in severe anorexia nervosa. Annals of Hematology, 92(5), 605–613. [DOI:10.1007/s00277-013-1672-x] [PMID]
Sadock, B. J., Sadock V. A., & Ruiz, S. P. (2015). Kaplan and Sadock’s synopsis of psychiatry: Behavioral sciences/clinical psychiatry. Alphen aan den Rijn: Wolters Kluwers. [Link]
Salvato, G., Sellitto, M., Crottini, F., Tarlarini, P., Tajani, M., & Basilico, S., et al. (2024). Extreme weight conditions impact on the relationship between risky decision-making and interoception. Cortex, 179, 126-142. [DOI:10.1016/j.cortex.2024.07.009] [PMID]
Sidar, Ç., & Mazlum, Ç. (2020). Olanzapine in the treatment of anorexia nervosa: A systematic review. The Egyptian Journal of Neurology, Psychiatry, and Neurosurgery, 56(60). [DOI:10.1186/s41983-020-00195-y]
Walsh, K., Blalock, D. V., & Mehler, P. S. (2020). Hematologic findings in a large sample of patients with anorexia nervosa and bulimia nervosa. American Journal of Hematology, 95(4), E98-E101. [DOI:10.1002/ajh.25732]
Winston, A. P. (2012). The clinical biochemistry of anorexia nervosa. Annals of Clinical Biochemistry, 49(2), 132-143. [DOI:10.1258/acb.2011.011185] [PMID]
Wonderlich, J. A., Dodd, D. R., Sondag, C., Jorgensen, M., Blumhardt, C., & Evanson, A. N., et al. (2024). Clinical and scientific review of severe and enduring anorexia nervosa in intensive care settings: introducing an innovative treatment paradigm. Journal of Eating Disorders, 12(1), 131. [DOI:10.1186/s40337-024-01079-9] [PMID]
Type of Study: case report |
Subject:
Approach to biological neural
Received: 2024/06/17 | Accepted: 2024/09/23 | Published: 2024/10/2
Received: 2024/06/17 | Accepted: 2024/09/23 | Published: 2024/10/2
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








