Volume 12, Issue 4 (Autumn 2024)
PCP 2024, 12(4): 345-360 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Farimanian S, Bayazi M H. Effectiveness of Group Cognitive-behavioral Therapy on the Psychological Security of Patients With Type II Diabetes Mellitus. PCP 2024; 12 (4) :345-360
URL: http://jpcp.uswr.ac.ir/article-1-939-en.html
URL: http://jpcp.uswr.ac.ir/article-1-939-en.html
1- Department of Psychology, Faculty of Psychology, Torbat-e-Jam Branch, Islamic Azad University, Torbat-e-Jam, Iran.
2- Department of Psychology, Faculty of Psychology, Torbat-e-Jam Branch, Islamic Azad University, Torbat-e-Jam, Iran. ,drmhbayazi1@gmail.com
2- Department of Psychology, Faculty of Psychology, Torbat-e-Jam Branch, Islamic Azad University, Torbat-e-Jam, Iran. ,
Keywords: Group cognitive-behavioral therapy (GCBT), Psychological security (PS), Patients with type II diabetes (T2DM)
Full-Text [PDF 730 kb]
(571 Downloads)
| Abstract (HTML) (1715 Views)
Full-Text: (518 Views)
Introduction
Aging is a crucial part of human life and it can be considered as the final stage of human development and growth. Along with aging, a new period of the human life cycle appears, and if the necessary facilities and conditions are provided, this period can be a rebirth for humans (Kaplan & Robson, 2009). In the meantime, the elderly are more exposed to incurable diseases than other groups, because their immune system is weakened and they do not have the physical and mental strength to deal with diseases (Naghavi et al., 2017). Based on this, one of the diseases observed in the elderly population is diabetes (Frey et al., 2018). Diabetes is an endocrine disease, the management of which is considered one of the necessities of the medical science of this century (Morris et al., 2011). It has many issues and problems (Riddle & Herman, 2018). Coping with these problems and the long process of treatment always causes many crises for affected patients and their families (Blacburn et al., 2013). Approximately 90% of diabetic patients have type II diabetes mellitus (T2DM) (American Diabetes Association, 2007). T2DM is caused by the inability of the body to produce or use insulin (Zhang et al., 2008), and is related to aging, obesity, glucose metabolism disorder, and physical inactivity. Usually, T2DM is associated with many long-term complications (D’Souza et al., 2017). T2DM is one of the chronic diseases increasing the possibility of mental disorders due to physical problems (Oyewole et al., 2023; Goyal et al., 2024). Therefore, psychological interventions can probably create positive changes in the body’s immune and psychological activity indicators. Because patients with T2DM face many physical problems and emotional disorders in the process of life; Therefore, emotional disturbances associated with the disease seem inevitable (Fisher et al., 2010), and the likelihood of depression (Collins et al., 2008), anxiety (Li et al., 2008), stress and depression (Krishna, 2018). This increases the blood sugar level of patients with T2DM and reduces effective DSCA (Morris, 2011). Despite the expenses spent for the prevention and control of diabetes, the number of patients increases every day, which seems to be a weak point for patients with T2DM (Atlas, 2015).
T2DM is one of the chronic diseases increasing the possibility of mental disorders due to physical problems. On the other hand, patients with T2DM cannot take proper care of themselves. Not taking care of yourself, and the way of teaching philosophy can be a good way to change thinking. People with poor psychological health do not have enough motivation and emotional strength to manage their diabetes. Psychosocial adjustment is a factor and at the same time, a critical outcome of diabetes care, whether in therapeutic effects or quality of life (QoL) (Snoek, 2002). Psychological symptoms play a crucial role in the care of diabetes, which largely depends on the psychosocial factors of the person to manage this disease and achieve proper control.
Hereditary and family history is essential in the onset of diabetes, but the sudden onset is often related to emotional stress that upsets the vital balance in susceptible people. Effective psychological factors include those that evoke feelings of failure, loneliness, and sadness (Sadock et al., 2015). Patients with diabetes usually follow diets to control their diabetes, but when they are depressed or sad, stress and anxiety often resort to overeating and drinking, resisting insulin injections, and self-destruction causing diabetes to go out of control (Sadock et al., 2015). In other words, depression itself aggravates diabetes and thus worsens the prognosis of diabetes. The results of various studies (12-9) (Lloyd et al., 2018; Schmitt et al., 2017; Joseph & Golden, 2017) show that depression and diabetes often occur together. In various surveys, the rate of depression in patients with T2DM has been declared to be twice that of normal people. Depression in this group of patients can have a significant effect on the prognosis of diabetes and some studies (Joseph & Golden, 2017) have shown that the lack of diagnosis and treatment of depression in patients with T2DM worsens the prognosis of patients and lowers the quality of their life. It seems that depression can be related to the severity of physical and cognitive complications associated with diabetes.
The occurrence of depression with diabetes disrupts self-care behaviors, increases physical complaints, decreases QoL, increases treatment costs, and increases factors that increase the risk of death for sufferers (Bogner et al., 2007). The depression of patients with T2DM makes them unable to use their memory strategies (mental skills, semantic knowledge, and expertise) to isolate the happening events (Ossher et al., 2012). Also, due to the presence of cognitive errors in depressed people, receiving information from perceived events (surrounding environment) is not done correctly. As a result, when a person needs information received from daily events to carry out his daily tasks, it is not possible to retrieve them or it is associated with limitations (Williams et al., 2007). Although the cognitive functions of non-depressed diabetics are weaker than the healthy group, they benefit from their compensatory strategies to correctly register the information received from the happening events. Therefore, their weakness in memory performance, especially everyday memory, is covered by using compensatory strategies and they have no problems in doing their daily tasks. Research results show that CBT increases the psychological health of T2DM patients (Lipman, 2003). Also, researchers (Sabourin et al., 2011) show that psychosocial group training and treatment methods are effective in controlling diabetes and reducing the stress caused by this disease.
The use of medicine is essential in the management of T2DM. Due to poor medication adherence in patients with T2DM, it causes concern because not complying with it can lead to the worsening of the disease (Ahmad et al., 2013). Research shows that type 2 diabetes increases the risk of cognitive impairment (Meneilly et al., 2018) and depression (Tong et al., 2016), as well as increases the body’s metabolic compensation (Valenzuela et al., 2018) and reduces medication adherence. In addition, non-adherence to medical care in the care of patients with diabetes is related to the hospitalization rate. Adherence to medical recommendations was related to a remarkable decrease in hospitalization of patients and a tendency to visit less (Delevry et al., 2020). Continuous and extensive efforts in determining the current standards of health, including focusing on physical and mental health and ending the continuous stress of the disease, are widely followed theoretically and empirically (Wise & Hersh, 2012), emphasizing the need to implement effective psychological interventions. Along with medical treatments, it is necessary to control this disease and its related complications (Huges et al., 2014). In the meantime, one of the variables related to the existence that affects the function of the elderly and their satisfaction with life is the feeling of security (Montazerolhodjah et al., 2018). In this research, the researcher tries to measure the effect of group cognitive-behavioral therapy (GCBT) training on psychological security (PS) variables in patients with T2DM. The occurrence of emotional, physical, and sexual injuries in childhood is one of the factors that can institutionalize a sense of insecurity and being at risk in people’s memory and unconsciousness (Otgaar et al., 2021).
One of the variables that seem to be effective in patients with T2DM is PS. PS, which can also be called mental security or a sense of inner security (Raina & Bhan, 2013; American Psychiatric Association, 2013), is the smoothest platform for the growth of mental creativity and innovation (Steinke et al., 2016; Xu et al., 2022; Saffariantoosi & Khaleghi, 2024). The feeling of PS is one of the most obvious personality traits of creative and capable people (Maslow, 1942; Maslow et al., 1952; Zhang et al., 2010; Taormina & Sun, 2015; Wang et al., 2019; Kumar et al., 2024), and it is considered the most effective way to encourage people to think and try to achieve growth and progress at different personal, family, professional and social levels (Toobert et al., 2000). This concept refers to an environment that is understood as “an impersonal and non-threatening environment” (Hirak, 2012). Patients with T2DM suffer from depression, despair, and feelings of inferiority more than other people. Security is a divine gift and an innate human need, and it is considered one of the basic human motivations. Maslow, (1942) has proposed security as the second basic need in the pyramid of needs; in such a way that satisfying the need for security healthily and desirably throughout life can provide the basis for achieving other needs, such as self-esteem, loving and being loved, and self-actualization. However, the effectiveness of a distinctive therapy depends on medication adherence. Medication adherence in patients with T2DM in primary health clinics is poor, which is a cause for concern because not complying with it can lead to a worsening of the disease (Sun et al., 2023).
Many treatments exist to adapt to T2DM; one of these types of therapy is GCBT. It is based on the solid cooperation between the patient and the therapist. Today, evidence shows the effectiveness of CBT-based training programs on mental health, well-being, and other health-related benefits (McConville et al., 2017). CBT-based interventions allow the patient to give a wise response instead of an immediate and ill-considered response to things. Therefore, it intervenes by providing a platform for deep attention to the experiences of the disease and accepting the emotions and suffering caused by it. For this reason, conscientious people have a higher ability in efficiency and problem-solving than others (Emanuel et al., 2010). Based on the research, as soon as the patient reaches mental security, he/she can achieve good results in the field of relative recovery of her illness (Al Qudah et al., 2020) and as a result, get a better view of her QoL and future. This is also true in the elderly (Gong et al., 2012). Previous research has shown that GCBT is effective for various mental problems (e.g. psychological symptoms), physical conditions (e.g. irritable bowel syndrome and fatigue syndrome), and behavioral problems (overweight and antisocial behaviors) (Nakao et al., 2021; Surmai & Duff, 2022). Since in the previous research, most focus was on workplace PS (Probst, 2002), therefore less attention was paid to elderly patients with T2DM. Nakao et al., (2021) (found the effectiveness of GCBT on mental and physical variables (such as PS and psychological distress) related to patients with T2DM. Abbas et al. (2023) declared that GCBT has a significant reduction in diabetes distress, psychological distress, PS, depressive symptoms, and health anxiety, and has a significant enhancement in treatment adherence, QoL, and physical activity schedule of patients with T2DM. Lindhe et al. (2023) confirmed the effectiveness of GCBT for individuals experiencing psychological distress, PS, and health anxiety associated with climate change. Pan et al. (2023) achieved the effectiveness of an internet-based GCBT program for students with psychological distress. Skoglund et al. (2024) declared that GCBT has a statistically significant decrease in people with comorbid PS. GCBT is short and limited in terms of time and it tries to help clients to develop independent self-help skills. In addition, the GCBT approach relies on the process of questioning and discovery combined with strategy and not on convincing (Jesse et al., 2019). In this approach, based on inductive methods, the patient learns to look at thoughts and beliefs as hypotheses that must be tested. Finally, this approach is educational in that GCBT techniques are considered skills that must be learned through practice and entered into the patient’s environment through homework (Welschen et al., 2013). Based on GCBT intervention, skills to evaluate irrational and negative thinking are learned and a range of standard cognitive-behavioral coping skills are taught, which is a guide for flexibility in choosing strategies appropriate to the situation (Baker et al., 2016). It reduces psychological symptoms (Serlachius et al., 2016). In a pilot study, it was shown that GCBT is effective in improving and increasing PS in adolescents (Nakao et al., 2021).
Since the diagnosis of diabetes has crucial effects on the psychological and social performance of patients, patients must devote a lot of attention and energy to self-management of the disease. The success of patients in integrating a self-management approach with their existing lifestyle depends on the extent to which diabetes-specific events interact with the patient’s existing beliefs, thoughts, feelings, and behaviors. Diabetes is often associated with mental problems and disorders, and unfortunately, these problems reduce the patient’s ability to self-manage the disease. Decreasing the ability of patients to control diabetes aggravates their psychological problems and causes patients to get caught in a vicious cycle. These problems may even become more severe with the psychological reactions of patients that negatively impact the experience of diabetes symptoms. Identifying effective treatments to increase PS is essential to continue treatment for patients with T2DM. In addition, according to the background review, few researchers have investigated the effectiveness of GCBT on PS. Therefore, while completing this research gap, this research can provide counselors, clinical psychologists, and therapists with a suitable solution for appropriate psychological interventions in patients to expand theoretical knowledge in the field of diabetes and the effectiveness of interventions on crucial variables in this field. Also, the results of this study will develop knowledge of the effectiveness of GCBT on PS. This treatment can be effective in identifying rational and hopeful thought patterns and increasing the perception of well-being, and as a result, it will have a positive effect on constructive PS. One of the vital factors in the control of diabetes is PS and improving PS is one of the vital steps to help patients for better control and management of their disease. Therefore this research was conducted to answer the question of whether group GCBT is effective on PS in people with T2DM.
Materials and Methods
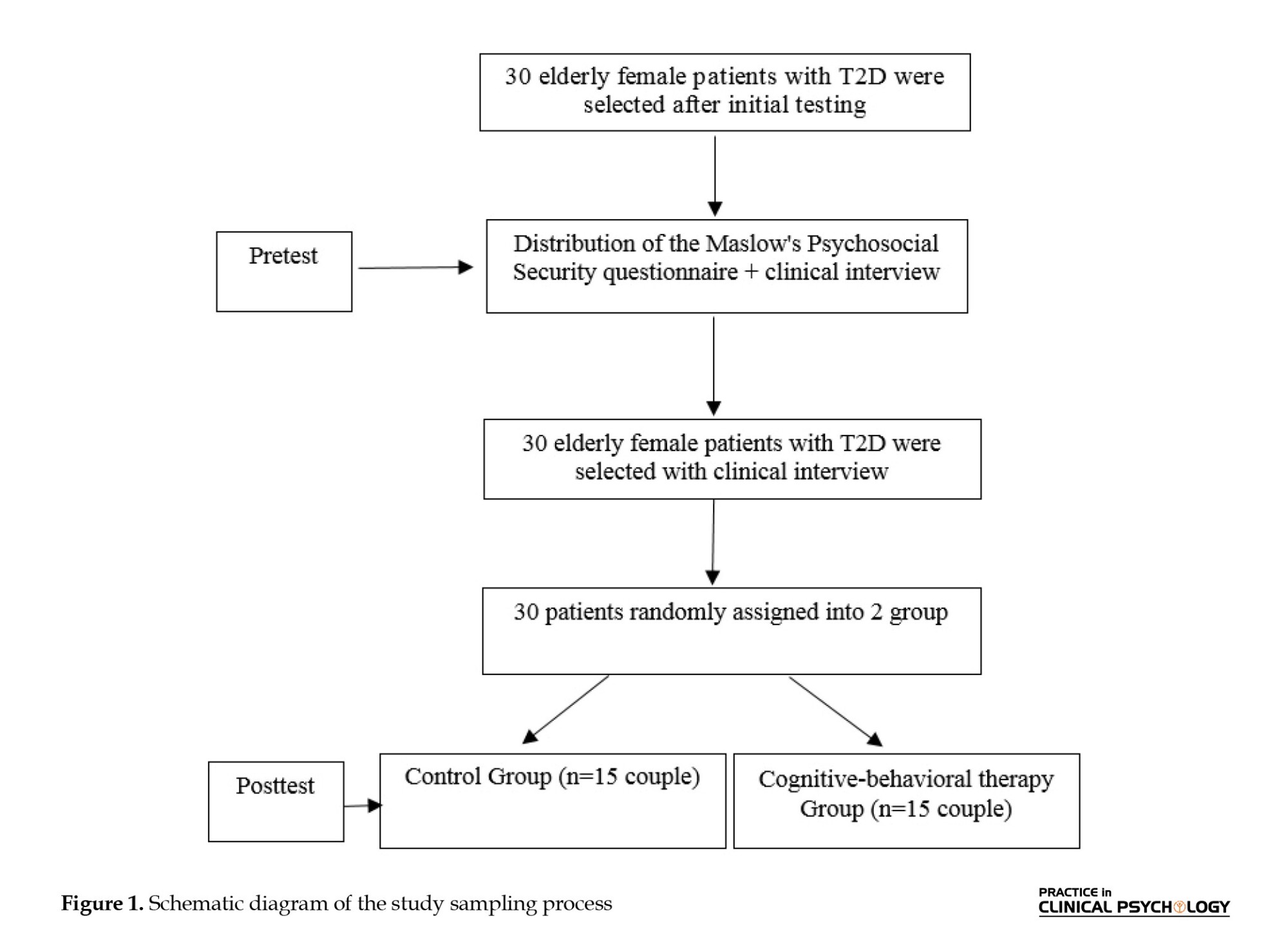
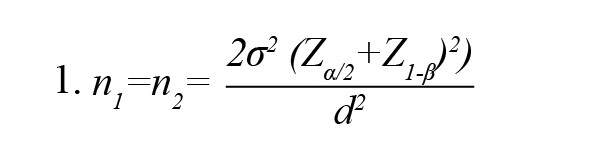
The current study was a quasi-experimental and a pre-test-post-test design with a control group. The sample included 30 elderly female patients with T2DM who visited a counseling center in Fariman City. The convenience sampling method was implemented to select subjects. The study was conducted during August-September 2023. The Equation 1 was used for sampling (Sarabadani et al., 2023). According to the values of δ=3.52 (common SD of PS score), d=2.81 (the pre-test mean score differences of PS in the test and control groups), statistical power=0.9, and error level or α equal to 0.05, the sample size was equal to 13 people for each group. With the possibility of a sample drop in the groups, the sample size of 15 people was considered for each group.
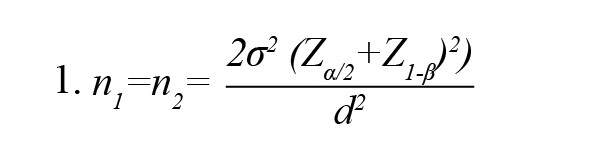
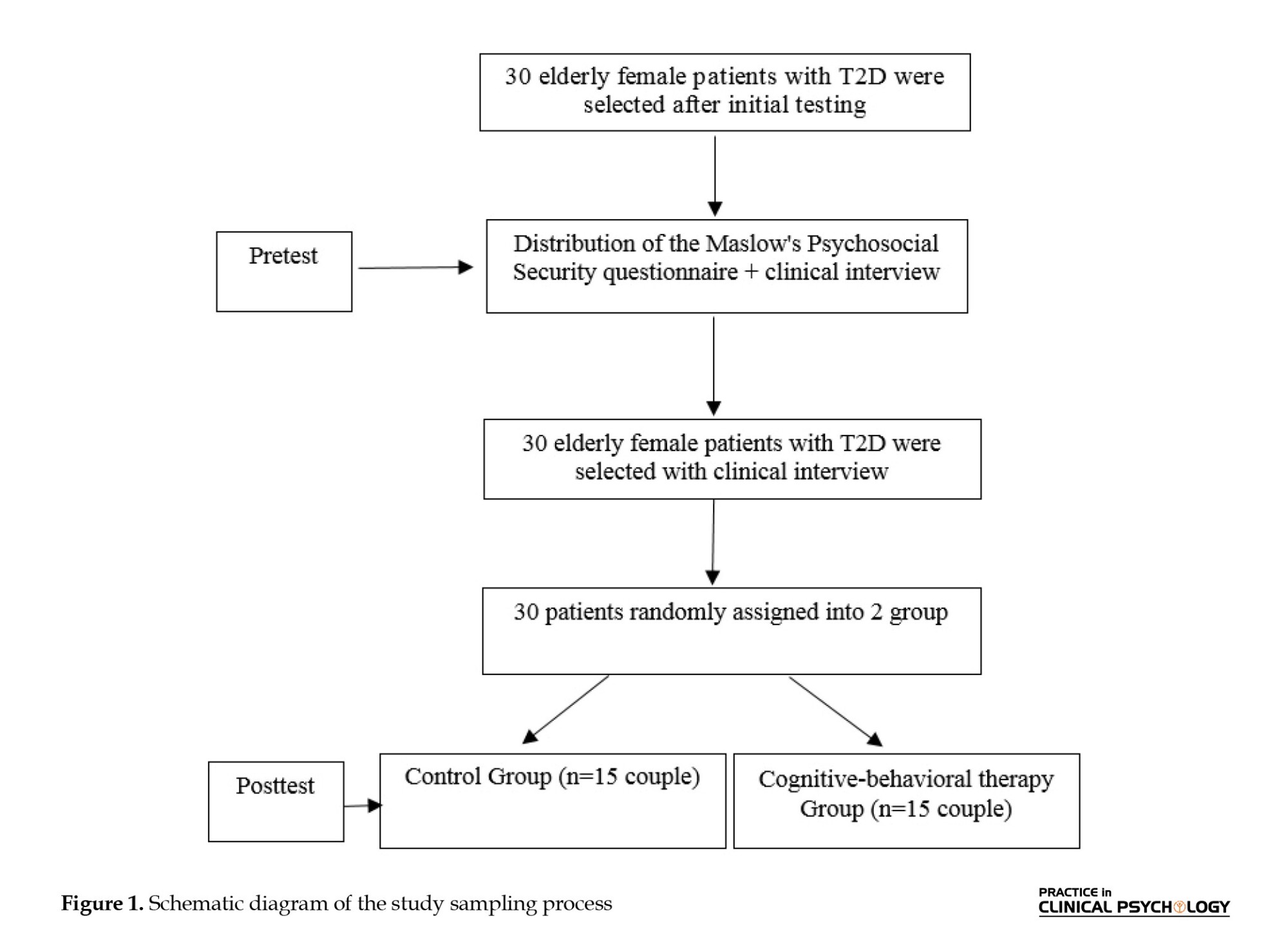
To comply with ethical considerations, written consent was obtained from the subjects for informed participation in the research. Also, it is emphasized on the principle of confidentiality of the participants’ information and the implementation of this training for the control group after the end of the experiment. The participants were initially numbered from 1 to 30. After matching based on demographic characteristics, such as age, gender, and history of disease, they were randomly assigned to the test and control groups in odd and even pairs (Figure 1).
Inclusion and exclusion criteria
The inclusion criteria included a specialist doctor’s diagnosis of T2DM, having at least a diploma, and being 55 years old or older. The exclusion criteria included the absence of more than two sessions, unwillingness to continue cooperating in the study, and acquiring an incomplete questionnaire.
Procedures
To collect data, the Maslow’s psychosocial security (PS) questionnaire (Maslow, 1942) was used:
Maslow’s PS
Maslow’s PS questionnaire was created in 1942 to measure different aspects of PS. It has 62 62-question self-report scales and 15 subscales. It includes scales, such as environmental maladjustment (1-6), paranoia (7-11), self-belief (12-16), passion for Life (21-17), depression (22-25), sense of bliss (26-30), social security (31-34), self-awareness (35-37), self-confidence (38-41), nervousness (42-44), disappointment, (45-47), interest in life (48-51), adjustment with others (52-54), feeling of healthiness (55-58), feeling of inferiority (59-62). It is scored with yes and no options. Achieving a high score on this test (62) indicates a person’s high PS and a low score indicates low PS (Maslow, 1942). Maslow reported the value of Cronbach’s α of this questionnaire as 0.66 (Maslow, 1942). Bowen et al. (2010) reported the total Cronbach’s α coefficient of 0.92. Also, Zare and Aminpour (2012) reported a Cronbach’s α coefficient of 0.64 and re-test reliability at two-week intervals of 0.81. In the current research, the validity of the questionnaire has been well evaluated and confirmed using the opinions of supervisors and advisors. Also, the reliability of Maslow’s PS questionnaire was obtained through Cronbach’s α of 0.57.
Procedure
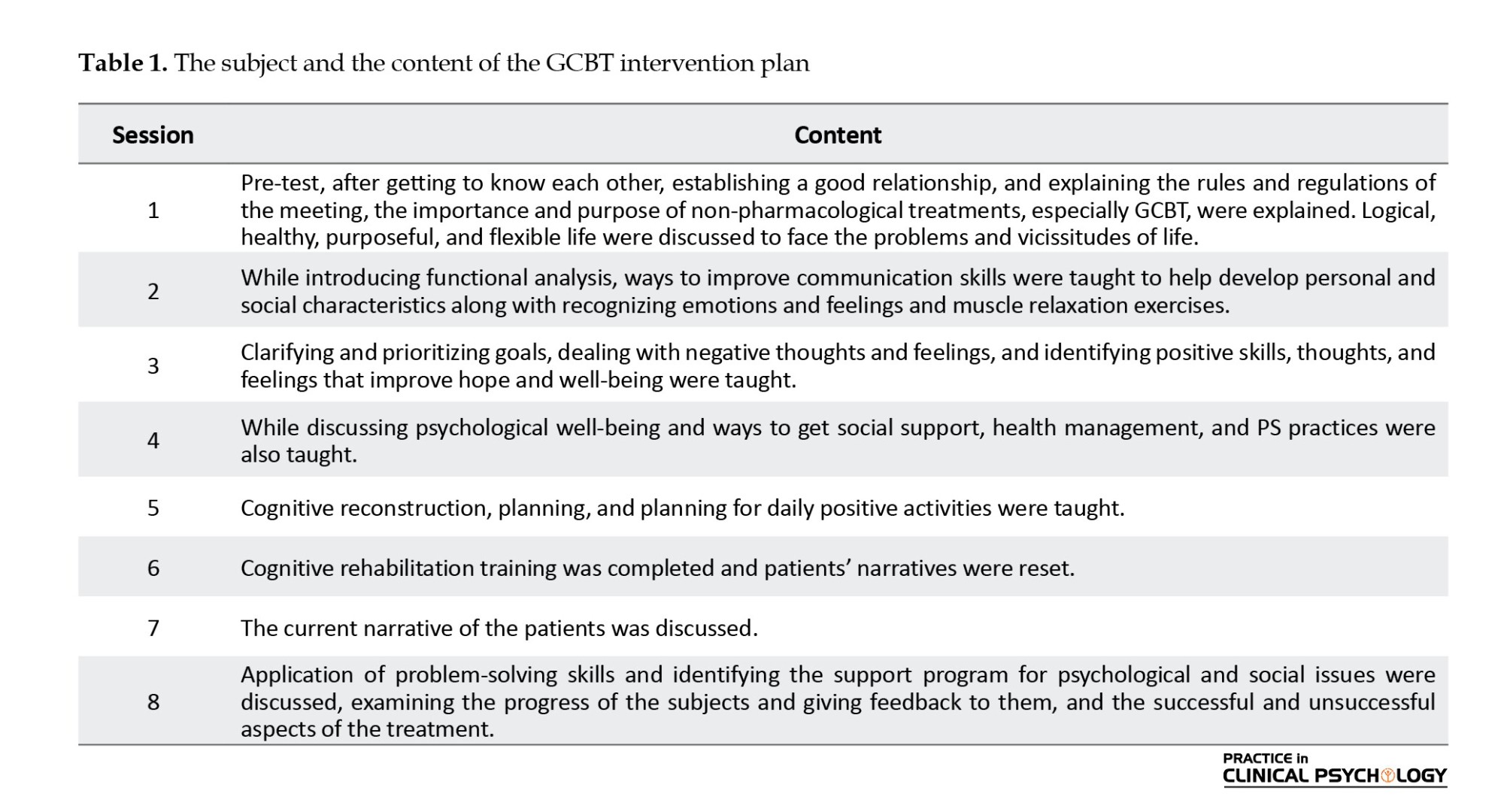
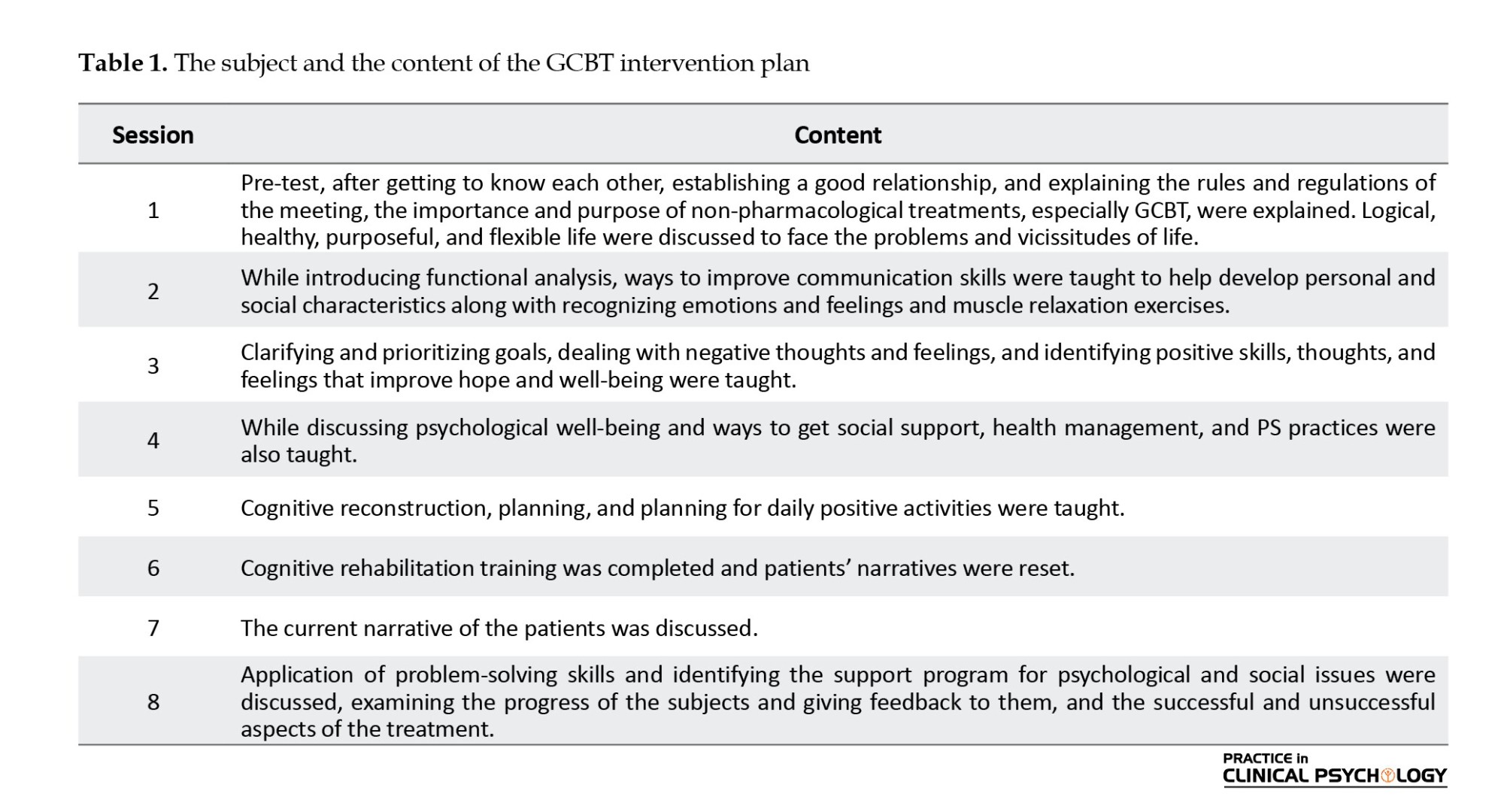
The participants were initially numbered from 1 to 30. After matching based on demographic characteristics, such as age, gender, and history of disease, they were randomly assigned to the test and control groups in odd and even pairs. The method of conducting the research was that after the necessary coordination with the officials of the Freeman Health Diabetes Center, written consent was obtained from the sample to participate in the study after stating the purpose of the study. The questionnaires were mostly completed by the participants and in some cases by the patient with the help of his companion. The test group was separately trained for 8 sessions of 120 minutes (one session per week) with GCBT based on Datiliou and Barashk’s (2006) treatment package, and the control group was placed on the waiting list. The sessions were held by a senior clinical expert. Also, in this research, an attempt was made to maintain the confidentiality of information in all stages of the research.
GCBT intervention plan
The patient’s PS programs were announced through a written self-report by the patient himself/her relatives living with him. It should be noted that the researcher completed the questionnaires in the form of a structured interview with the participants in 15-20 minutes. Table 1 presents the details of the intervention in the test group.
Data analysis
In this study, descriptive statistics (Mean±SD) and inferential statistics analyzed the data (analysis of covariance [ANCOVA]).
Results
Descriptive results
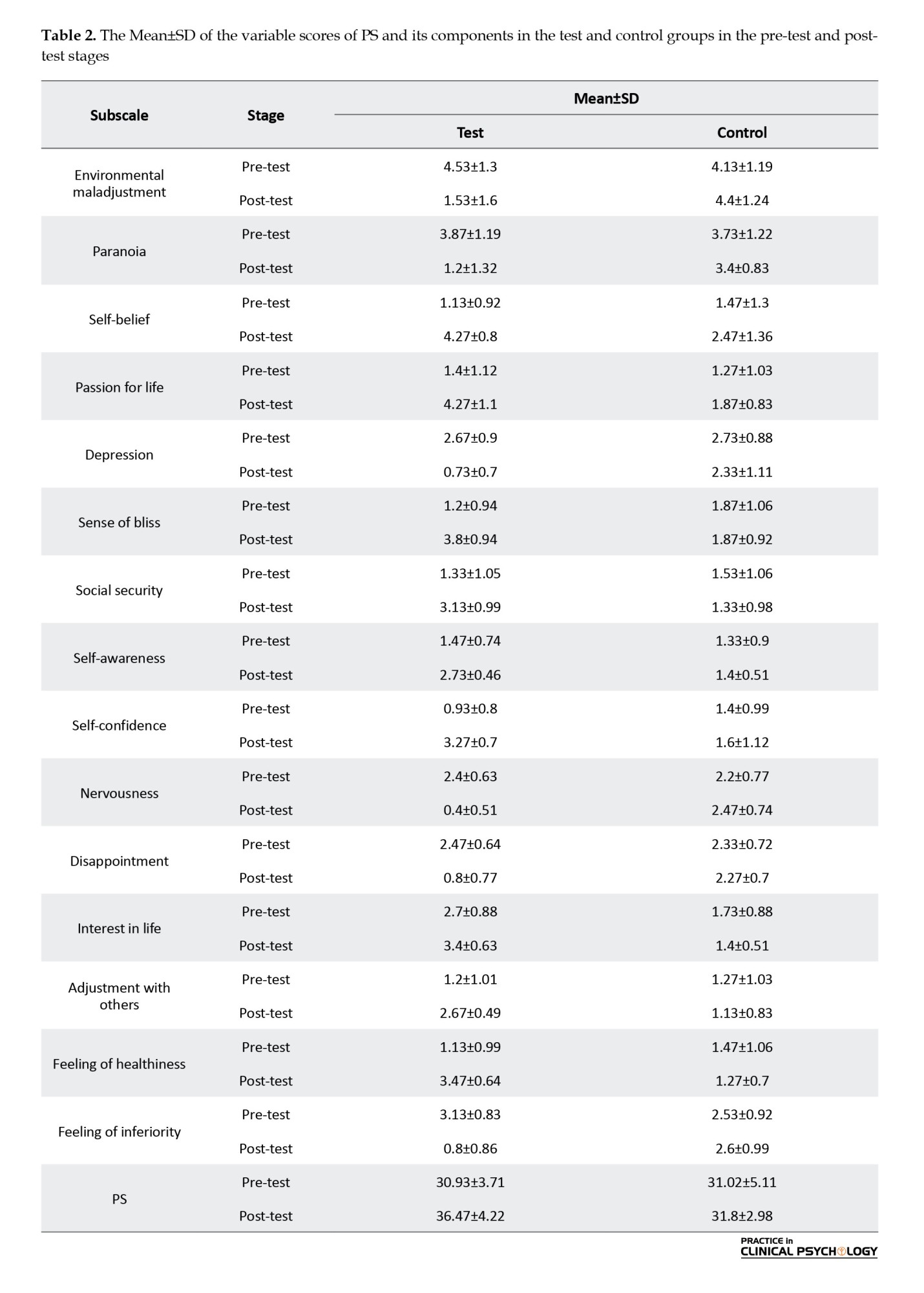
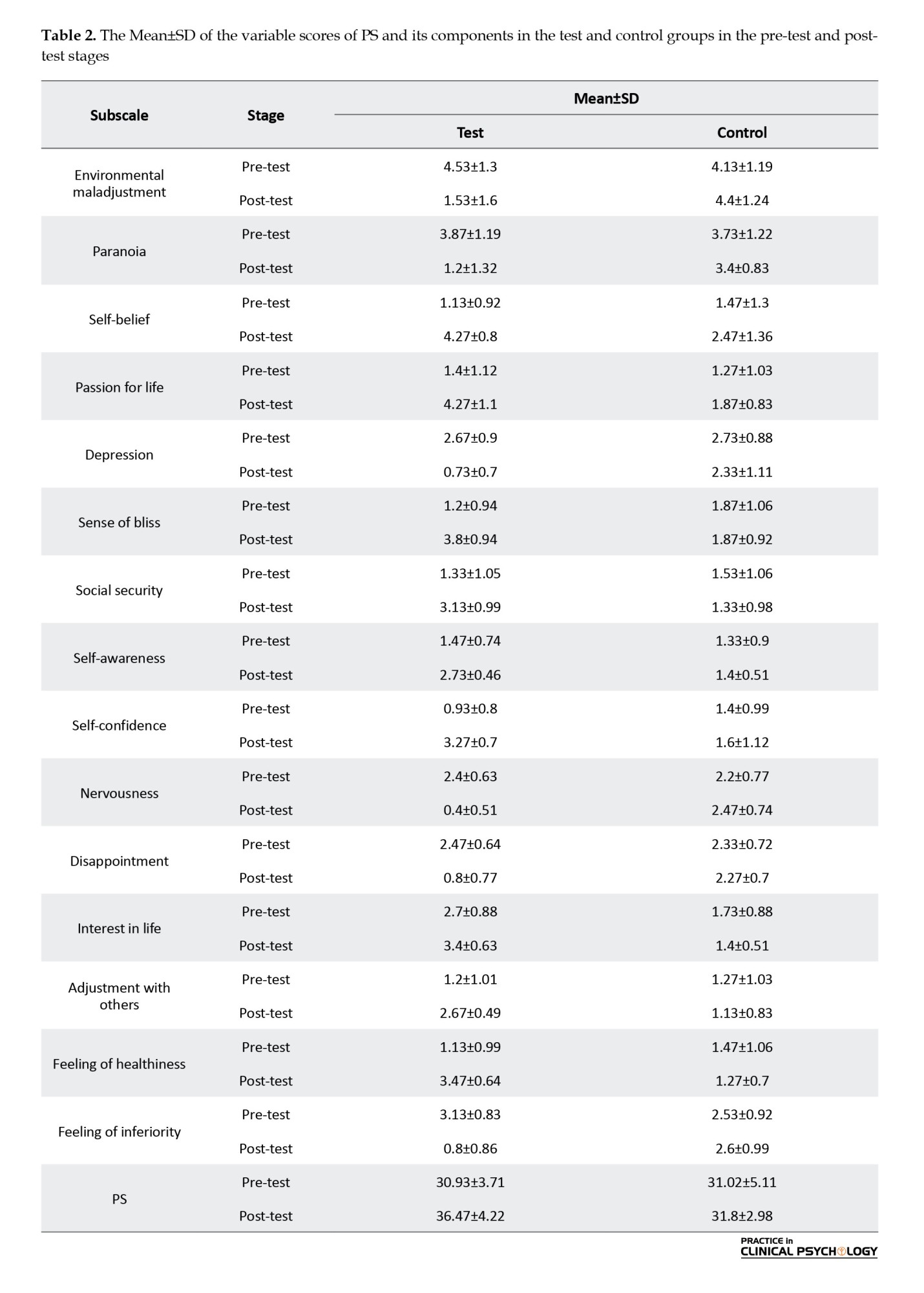
The participants of this research were 30 patients with T2DM. Demographic data that were assessed in this study included age, sex, and education. The Mean±SD of the age of the samples was 58.14±23.47 years. They were in the age range of 55 to 67 years. The highest frequency is related to the age of 55-59 years and the lowest frequency is related to the age of 59-67 years. Table 2 presents the descriptive statistics (Mean±SD) of the variables in the pre-test and post-test stages. As seen, the mean of the test group increased compared to the control group in PS.
Analysis of covariance (ANCOVA)
Before analyzing the data by ANCOVA, the presuppositions of ANCOVA were evaluated. The results of the Kolmogorov-Smirnov test on PS variables were not significant for any of the variables, indicating that the assumption of the data normality test is established (P>0.05) (Table 3).
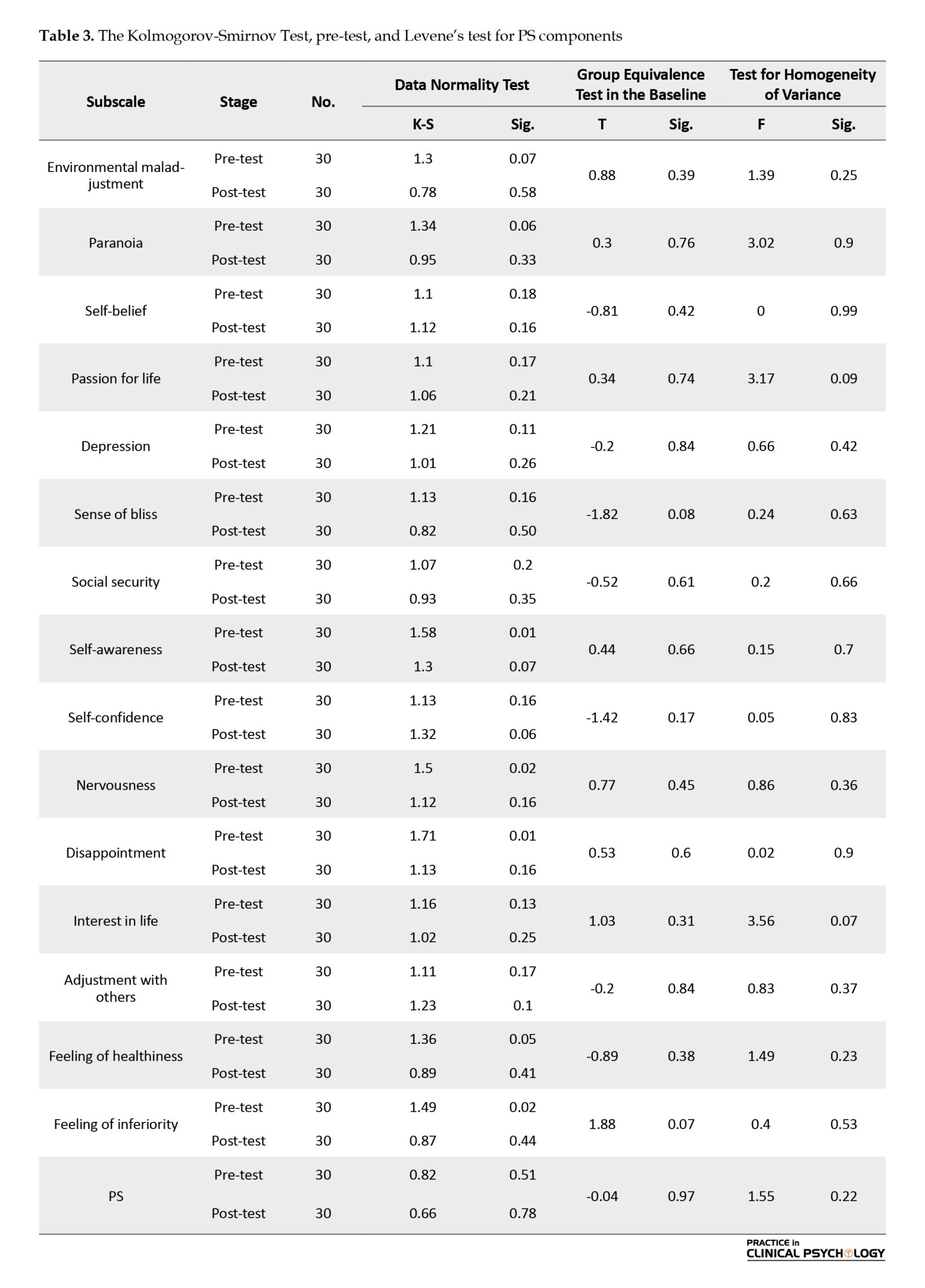
Also, the results of Levene’s test for equality of variances were not significant indicating the assumption that the individual group covariance matrices are equal (homogeneous across groups) and the assumption of equal variance is valid (Table 3). As can be seen in Table 3, the results of the test for homogeneity of variance of the test and control groups are not significant for the PS component; therefore, the variances of the test and control groups are the same.
While it is assumed that the variables in ANCOVA should show linearity in the whole data, this assumption should also be considered that the regression lines should be the same for each group in the research. The results of the test of homogeneity of regression slopes of the research variables have shown that the F value of the interaction for the sameness of the regression line slope for the PS variable (F=3.72) is at a significant level of 0.063, which is insignificant. In other words, the homogeneity of regression slopes is accepted. Table 4 presents the results of the ANCOVA test. As seen, the test results showed that the independent variable was effective on the dependent variable. In other words, the test and control groups have a significant difference in the PS variable (P<0.0001).
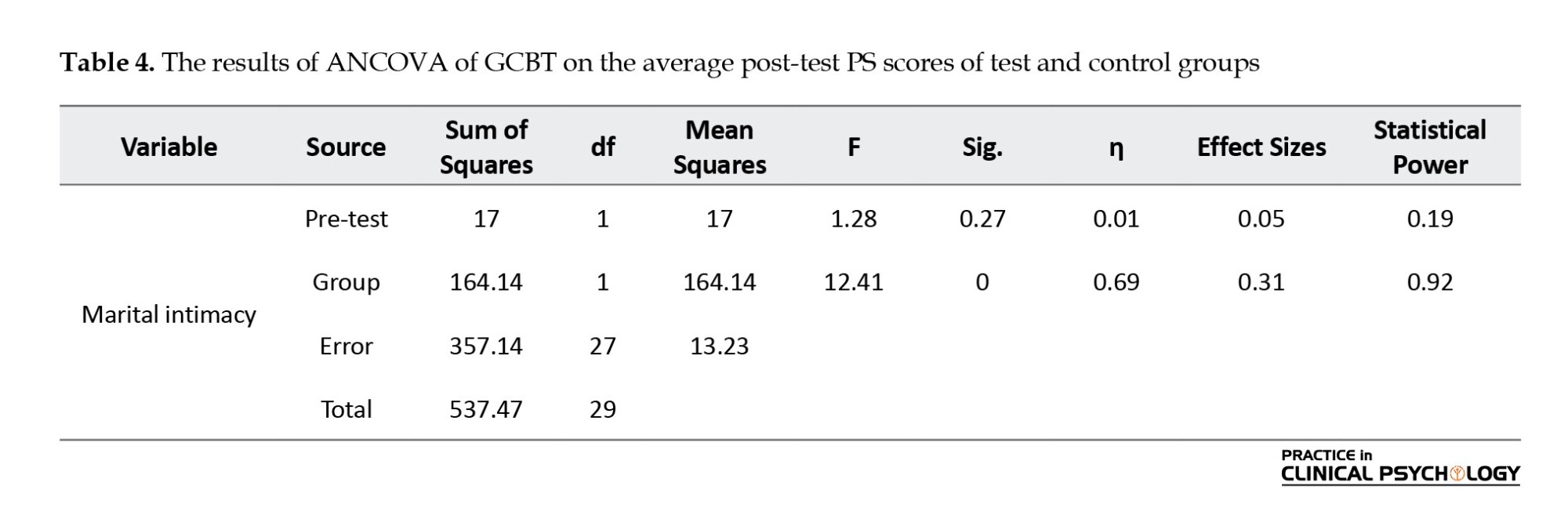
According to the results of ANCOVA by controlling the pre-test effect and calculated according to the F coefficient, a significant difference is observed between the adjusted averages of PS scores according to group membership “test and control” in the post-test stage (P<0.0001). It can be concluded that the null hypothesis was rejected and the GCBT method had a greater effect on the participants of the test group.
The effect size of “practical significance” was 0.31, that is, 31% of the total variance changes or individual differences in the PS of patients with T2DM were caused by the effect of GCBT. The statistical power was 0.92, which indicated the adequacy of the sampling volume. A significant difference is observed between the level of PS of the subjects in the test and control groups (P=0.001, F=12.41). With 95% certainty, the null hypothesis is rejected and the main hypothesis is confirmed, and we conclude that GCBT is effective in increasing the PS of patients with T2DM.
To investigate the effect of GCBT on the components of PS, we use multivariate ANCOVA, where the dependent variable includes the components of PS, environmental maladjustment, paranoia, self-belief, passion for life, depression, sense of bliss, social security, self-awareness, self-confidence, nervousness, disappointment, interest in life, adjustment with others, feeling of healthiness, and feeling of inferiority.
The results of Table 4 show the difference between the post-test of the two groups in the components of PS. GCBT has increased the scores of self-belief, passion for life, sense of bliss, social security, self-awareness, self-confidence, interest in life, adjustment with others, and feeling of healthiness. Also, the scores of environmental maladjustment, paranoia, depression, nervousness, disappointment, and feeling of inferiority decreased in the post-test and all the components of PS are significant (P<0.05). We conclude that GCBT affects the PS components of patients with T2DM.
Discussion
The present study was conducted to investigate the effects of GCBT on the PS in patients with T2DM. The results revealed that GCBT was effective in enhancing and improving the PS of patients with T2DM (P<0.001). GCBT intervention can be introduced as a fruitful psychological intervention. It can increase psychological well-being indicators and greater medical adherence to treatment recommendations. Increasing this method helps prevent the complications of diabetes and improves the psychological health of patients with T2DM. Previous research, such as Welschen (2014), Baker et al., (2016), Serlachius et al., (2016), Pillow et al. (2017), Jesse et al., (2019), Puig-Domingo et al. (2020), Nakao et al., (2021), Pericot-Valverde et al. (2018), and Kamath et al. (2022) have confirmed the effectiveness of GCBT on PS in their research results. Research has shown that GCBT increases PS, reduces depression symptoms, and decreases symptoms of anxiety in women with T2DM. In other words, declined symptoms of depression and anxiety in people with T2DM are associated with improving PS (Adams et al., 2022). The results of some studies have shown that having sufficient motivation and information in women with vaginitis fertility will have a positive effect on PS and disease recovery (Xu et al., 2020). The results of other researchers suggest that PS in people with T2DM can be influenced by positive psychological characteristics, such as life expectancy and efficient attitudes. Nurses can improve their PS by improving efficient and hopeful attitudes in patients with T2DM. Nurses can also help patients with T2DM, who often have cognitive errors, and irrational and destructive beliefs in their lives, to inform patients of their irrational documents and beliefs. Using their knowledge and experience to help modify these misconceptions and promote patient information literacy to create rational and efficient beliefs. As a result, using experiences and enhancing health information, patients modify the misconceptions and documents that cause anxiety and depression and thus reduce their PS.
By examining the content of the materials presented in the psychological safety management training sessions in this research, it can be assumed that the use of behavioral strategies and strategies, such as calming and creating a sense of calm in the affected person have also reduced the psychological symptoms and distress in him. On the other hand, cognitive strategies, such as problem-solving, recognizing cognitive errors and fighting against negative thoughts, logical thinking, and using positive self-talk have probably caused a change in the attitudes and cognitions of patients so that they accepted their illness and rationally they faced its psychological consequences and by applying the skills taught, they took steps to improve themselves and control the disease more effectively. Also, GCBT training sessions, concerning the education of immunity against stress to patients with T2DM, familiarize them with how stress affects them and teach them to look at stressful situations as solvable problems. In addition, different coping methods and their effective management are shown to patients with T2DM. This makes them feel that they have more control over their surroundings, evaluate them as less threatening when dealing with such situations, and when faced with said situations, having more efficient coping skills, they can solve them more effectively, and be safe from the negative psychological effects caused by ineffective coping with stressful situations. Therefore, they can have better control over the anxieties caused by the disease.
Anxiety caused by chronic and permanent diseases, such as diabetes can lead to many psychological complications. Examples include depression, insomnia, anxiety, physical symptoms, and social dysfunction. Anxiety in its chronic state causes the erosion of the physical and mental reserves of the affected person by creating a state of permanent alertness in the body. This plays an effective role in using the mechanism of the learned helplessness effect of the diabetic person on non-compliance with the treatment. This helplessness happens because a person does not accept his diabetes in the early stages of diagnosis and the stress caused by it between the stage of denial and acceptance of the disease due to the occurrence of psychological complications of the disease that was mentioned. This state causes the observance of treatment points in the stage of feeling acceptance and non-observance of it in the stage of illness. The result is that the person does not achieve regular control of his blood sugar, and this teaches the patient that it is not possible to control his blood sugar in both cases of following and not following the treatment; therefore, these issues can be better overcome by teaching destructive thoughts to stop self-deception, and skills to deal with disappointment, failure and unfairness syndrome in meetings.
One of the reasons for the effectiveness of GCBT in increasing the PS of patients with T2DM is that the quality of patient care skills is the result of an individual’s beliefs, thoughts, behavior, and deeds and relates to one’s decisions and performance. As a psychotherapeutic method, GCBT alters the destructive patterns affecting patients’ behavior and emotions (Hofmann et al., 2012). Nurses can emphasize the importance of acquiring cognitive information, feeling efficient, skills, and using these skills by providing GCBT training. Also during the training, people learn fruitful behavioral methods in addition to working on negative thinking. People affected by these tutorials will find the ability to correct automatic thoughts and evaluate their evidence, as well as the documents needed to approve and disapprove those (Jun & Park, 2013).
Implementing GCBT has led to the improvement of PS in patients with T2DM. According to the obtained results, it can be said that the effort to change the attitudes and core and negative beliefs in GCBT by patients with T2DM has led to the improvement of the psychological condition of diabetic patients. In this treatment, the attitude and mental perception of patients about their disease and its symptoms have been changed, and it can be used in psychological clinics and educational workshops to increase adherence to the treatment, the perception of the disease, and the QoL of patients with T2DM.
Conclusion
The GCBT could improve the PS of patients with T2DM. The effort to change the attitudes and core and negative beliefs about the disease and its symptoms in patients with T2DM by the GCBT was successful. The intervention can be used in psychological clinics and educational workshops to increase adherence to the treatment, perception of disease, and quality of life of patients with T2DM.
Recommendations
It is suggested to take help from this treatment method to increase the learning of correct thinking and judgment skills about diabetes and to deal with unrealistic thoughts about this disease. Therefore, counselors and therapists can use this method to improve the PS of patients with T2DM. In addition, it is recommended that planners design programs based on this research to improve the PS of patients with T2DM.
Implications for family therapy/practice
Counselors and therapists of diabetes centers and clinics can use the GCBT approach in their therapy groups and training classes to improve the basic PS, not to be discouraged, and to continue the treatment and as a result, increase the physical health of patients with T2DM.
Research limitations
Not using follow-up was the most remarkable limitation of this research. Also, some sample groups could not participate in the meetings due to illness or some personal problems or did not have enough effort to perform their homework. Also, failure to control the presence of mental illnesses in patients, especially hospitalized patients, was another limitation of the current research. Also, coexisting diseases can be psychological, which can affect the PS variable. This may have affected the results of the current research, which is hoped to improve in subsequent research. The questionnaire was also used in this study to collect data. Therefore, there may be a bias in the information obtained; because some participants may answer some questions with a bias to better show themselves. Also, limiting the research population to diabetic patients referred to the counseling center in Fariman City was one of the limitations of this study. Failure to control some disturbing variables, such as the economic, family, social, and educational status of the research samples, has led to a decrease in the internal validity of the research, which is expected to be improved in future research.
Future research
It is hoped that the output of this study can be a background for further research in the field of PS of patients to help improve and treat patients with T2DM as much as possible. It is suggested that this research be repeated with larger and diverse samples and with long-term follow-ups, and studies to investigate the mediating factors and variables of these interventions. It is also recommended that a special PS program be designed by experts for patients with T2DM and the official integration of this training in diabetes treatment-care programs should be considered by experts and institutions active in this field.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles are considered in this article. The participants were informed of the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them. A written consent has been obtained from the subjects. Principles of the Helsinki Convention was also observed.
Funding
The paper was extracted from the master's thesis of Sima Farimanian, approved by the Department of Health Psychology, Faculty of Psychology, Torbat-e-Jam Branch, Islamic Azad University.
Authors' contributions
Conceptualization and supervision: Sima Farimanian and Mohammad Hossein Bayazi; Methodology: Mohammad Hossein Bayazi; Investigation and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers thank the patients and all the people who helped us in conducting this research.
References
Aging is a crucial part of human life and it can be considered as the final stage of human development and growth. Along with aging, a new period of the human life cycle appears, and if the necessary facilities and conditions are provided, this period can be a rebirth for humans (Kaplan & Robson, 2009). In the meantime, the elderly are more exposed to incurable diseases than other groups, because their immune system is weakened and they do not have the physical and mental strength to deal with diseases (Naghavi et al., 2017). Based on this, one of the diseases observed in the elderly population is diabetes (Frey et al., 2018). Diabetes is an endocrine disease, the management of which is considered one of the necessities of the medical science of this century (Morris et al., 2011). It has many issues and problems (Riddle & Herman, 2018). Coping with these problems and the long process of treatment always causes many crises for affected patients and their families (Blacburn et al., 2013). Approximately 90% of diabetic patients have type II diabetes mellitus (T2DM) (American Diabetes Association, 2007). T2DM is caused by the inability of the body to produce or use insulin (Zhang et al., 2008), and is related to aging, obesity, glucose metabolism disorder, and physical inactivity. Usually, T2DM is associated with many long-term complications (D’Souza et al., 2017). T2DM is one of the chronic diseases increasing the possibility of mental disorders due to physical problems (Oyewole et al., 2023; Goyal et al., 2024). Therefore, psychological interventions can probably create positive changes in the body’s immune and psychological activity indicators. Because patients with T2DM face many physical problems and emotional disorders in the process of life; Therefore, emotional disturbances associated with the disease seem inevitable (Fisher et al., 2010), and the likelihood of depression (Collins et al., 2008), anxiety (Li et al., 2008), stress and depression (Krishna, 2018). This increases the blood sugar level of patients with T2DM and reduces effective DSCA (Morris, 2011). Despite the expenses spent for the prevention and control of diabetes, the number of patients increases every day, which seems to be a weak point for patients with T2DM (Atlas, 2015).
T2DM is one of the chronic diseases increasing the possibility of mental disorders due to physical problems. On the other hand, patients with T2DM cannot take proper care of themselves. Not taking care of yourself, and the way of teaching philosophy can be a good way to change thinking. People with poor psychological health do not have enough motivation and emotional strength to manage their diabetes. Psychosocial adjustment is a factor and at the same time, a critical outcome of diabetes care, whether in therapeutic effects or quality of life (QoL) (Snoek, 2002). Psychological symptoms play a crucial role in the care of diabetes, which largely depends on the psychosocial factors of the person to manage this disease and achieve proper control.
Hereditary and family history is essential in the onset of diabetes, but the sudden onset is often related to emotional stress that upsets the vital balance in susceptible people. Effective psychological factors include those that evoke feelings of failure, loneliness, and sadness (Sadock et al., 2015). Patients with diabetes usually follow diets to control their diabetes, but when they are depressed or sad, stress and anxiety often resort to overeating and drinking, resisting insulin injections, and self-destruction causing diabetes to go out of control (Sadock et al., 2015). In other words, depression itself aggravates diabetes and thus worsens the prognosis of diabetes. The results of various studies (12-9) (Lloyd et al., 2018; Schmitt et al., 2017; Joseph & Golden, 2017) show that depression and diabetes often occur together. In various surveys, the rate of depression in patients with T2DM has been declared to be twice that of normal people. Depression in this group of patients can have a significant effect on the prognosis of diabetes and some studies (Joseph & Golden, 2017) have shown that the lack of diagnosis and treatment of depression in patients with T2DM worsens the prognosis of patients and lowers the quality of their life. It seems that depression can be related to the severity of physical and cognitive complications associated with diabetes.
The occurrence of depression with diabetes disrupts self-care behaviors, increases physical complaints, decreases QoL, increases treatment costs, and increases factors that increase the risk of death for sufferers (Bogner et al., 2007). The depression of patients with T2DM makes them unable to use their memory strategies (mental skills, semantic knowledge, and expertise) to isolate the happening events (Ossher et al., 2012). Also, due to the presence of cognitive errors in depressed people, receiving information from perceived events (surrounding environment) is not done correctly. As a result, when a person needs information received from daily events to carry out his daily tasks, it is not possible to retrieve them or it is associated with limitations (Williams et al., 2007). Although the cognitive functions of non-depressed diabetics are weaker than the healthy group, they benefit from their compensatory strategies to correctly register the information received from the happening events. Therefore, their weakness in memory performance, especially everyday memory, is covered by using compensatory strategies and they have no problems in doing their daily tasks. Research results show that CBT increases the psychological health of T2DM patients (Lipman, 2003). Also, researchers (Sabourin et al., 2011) show that psychosocial group training and treatment methods are effective in controlling diabetes and reducing the stress caused by this disease.
The use of medicine is essential in the management of T2DM. Due to poor medication adherence in patients with T2DM, it causes concern because not complying with it can lead to the worsening of the disease (Ahmad et al., 2013). Research shows that type 2 diabetes increases the risk of cognitive impairment (Meneilly et al., 2018) and depression (Tong et al., 2016), as well as increases the body’s metabolic compensation (Valenzuela et al., 2018) and reduces medication adherence. In addition, non-adherence to medical care in the care of patients with diabetes is related to the hospitalization rate. Adherence to medical recommendations was related to a remarkable decrease in hospitalization of patients and a tendency to visit less (Delevry et al., 2020). Continuous and extensive efforts in determining the current standards of health, including focusing on physical and mental health and ending the continuous stress of the disease, are widely followed theoretically and empirically (Wise & Hersh, 2012), emphasizing the need to implement effective psychological interventions. Along with medical treatments, it is necessary to control this disease and its related complications (Huges et al., 2014). In the meantime, one of the variables related to the existence that affects the function of the elderly and their satisfaction with life is the feeling of security (Montazerolhodjah et al., 2018). In this research, the researcher tries to measure the effect of group cognitive-behavioral therapy (GCBT) training on psychological security (PS) variables in patients with T2DM. The occurrence of emotional, physical, and sexual injuries in childhood is one of the factors that can institutionalize a sense of insecurity and being at risk in people’s memory and unconsciousness (Otgaar et al., 2021).
One of the variables that seem to be effective in patients with T2DM is PS. PS, which can also be called mental security or a sense of inner security (Raina & Bhan, 2013; American Psychiatric Association, 2013), is the smoothest platform for the growth of mental creativity and innovation (Steinke et al., 2016; Xu et al., 2022; Saffariantoosi & Khaleghi, 2024). The feeling of PS is one of the most obvious personality traits of creative and capable people (Maslow, 1942; Maslow et al., 1952; Zhang et al., 2010; Taormina & Sun, 2015; Wang et al., 2019; Kumar et al., 2024), and it is considered the most effective way to encourage people to think and try to achieve growth and progress at different personal, family, professional and social levels (Toobert et al., 2000). This concept refers to an environment that is understood as “an impersonal and non-threatening environment” (Hirak, 2012). Patients with T2DM suffer from depression, despair, and feelings of inferiority more than other people. Security is a divine gift and an innate human need, and it is considered one of the basic human motivations. Maslow, (1942) has proposed security as the second basic need in the pyramid of needs; in such a way that satisfying the need for security healthily and desirably throughout life can provide the basis for achieving other needs, such as self-esteem, loving and being loved, and self-actualization. However, the effectiveness of a distinctive therapy depends on medication adherence. Medication adherence in patients with T2DM in primary health clinics is poor, which is a cause for concern because not complying with it can lead to a worsening of the disease (Sun et al., 2023).
Many treatments exist to adapt to T2DM; one of these types of therapy is GCBT. It is based on the solid cooperation between the patient and the therapist. Today, evidence shows the effectiveness of CBT-based training programs on mental health, well-being, and other health-related benefits (McConville et al., 2017). CBT-based interventions allow the patient to give a wise response instead of an immediate and ill-considered response to things. Therefore, it intervenes by providing a platform for deep attention to the experiences of the disease and accepting the emotions and suffering caused by it. For this reason, conscientious people have a higher ability in efficiency and problem-solving than others (Emanuel et al., 2010). Based on the research, as soon as the patient reaches mental security, he/she can achieve good results in the field of relative recovery of her illness (Al Qudah et al., 2020) and as a result, get a better view of her QoL and future. This is also true in the elderly (Gong et al., 2012). Previous research has shown that GCBT is effective for various mental problems (e.g. psychological symptoms), physical conditions (e.g. irritable bowel syndrome and fatigue syndrome), and behavioral problems (overweight and antisocial behaviors) (Nakao et al., 2021; Surmai & Duff, 2022). Since in the previous research, most focus was on workplace PS (Probst, 2002), therefore less attention was paid to elderly patients with T2DM. Nakao et al., (2021) (found the effectiveness of GCBT on mental and physical variables (such as PS and psychological distress) related to patients with T2DM. Abbas et al. (2023) declared that GCBT has a significant reduction in diabetes distress, psychological distress, PS, depressive symptoms, and health anxiety, and has a significant enhancement in treatment adherence, QoL, and physical activity schedule of patients with T2DM. Lindhe et al. (2023) confirmed the effectiveness of GCBT for individuals experiencing psychological distress, PS, and health anxiety associated with climate change. Pan et al. (2023) achieved the effectiveness of an internet-based GCBT program for students with psychological distress. Skoglund et al. (2024) declared that GCBT has a statistically significant decrease in people with comorbid PS. GCBT is short and limited in terms of time and it tries to help clients to develop independent self-help skills. In addition, the GCBT approach relies on the process of questioning and discovery combined with strategy and not on convincing (Jesse et al., 2019). In this approach, based on inductive methods, the patient learns to look at thoughts and beliefs as hypotheses that must be tested. Finally, this approach is educational in that GCBT techniques are considered skills that must be learned through practice and entered into the patient’s environment through homework (Welschen et al., 2013). Based on GCBT intervention, skills to evaluate irrational and negative thinking are learned and a range of standard cognitive-behavioral coping skills are taught, which is a guide for flexibility in choosing strategies appropriate to the situation (Baker et al., 2016). It reduces psychological symptoms (Serlachius et al., 2016). In a pilot study, it was shown that GCBT is effective in improving and increasing PS in adolescents (Nakao et al., 2021).
Since the diagnosis of diabetes has crucial effects on the psychological and social performance of patients, patients must devote a lot of attention and energy to self-management of the disease. The success of patients in integrating a self-management approach with their existing lifestyle depends on the extent to which diabetes-specific events interact with the patient’s existing beliefs, thoughts, feelings, and behaviors. Diabetes is often associated with mental problems and disorders, and unfortunately, these problems reduce the patient’s ability to self-manage the disease. Decreasing the ability of patients to control diabetes aggravates their psychological problems and causes patients to get caught in a vicious cycle. These problems may even become more severe with the psychological reactions of patients that negatively impact the experience of diabetes symptoms. Identifying effective treatments to increase PS is essential to continue treatment for patients with T2DM. In addition, according to the background review, few researchers have investigated the effectiveness of GCBT on PS. Therefore, while completing this research gap, this research can provide counselors, clinical psychologists, and therapists with a suitable solution for appropriate psychological interventions in patients to expand theoretical knowledge in the field of diabetes and the effectiveness of interventions on crucial variables in this field. Also, the results of this study will develop knowledge of the effectiveness of GCBT on PS. This treatment can be effective in identifying rational and hopeful thought patterns and increasing the perception of well-being, and as a result, it will have a positive effect on constructive PS. One of the vital factors in the control of diabetes is PS and improving PS is one of the vital steps to help patients for better control and management of their disease. Therefore this research was conducted to answer the question of whether group GCBT is effective on PS in people with T2DM.
Materials and Methods
The current study was a quasi-experimental and a pre-test-post-test design with a control group. The sample included 30 elderly female patients with T2DM who visited a counseling center in Fariman City. The convenience sampling method was implemented to select subjects. The study was conducted during August-September 2023. The Equation 1 was used for sampling (Sarabadani et al., 2023). According to the values of δ=3.52 (common SD of PS score), d=2.81 (the pre-test mean score differences of PS in the test and control groups), statistical power=0.9, and error level or α equal to 0.05, the sample size was equal to 13 people for each group. With the possibility of a sample drop in the groups, the sample size of 15 people was considered for each group.
To comply with ethical considerations, written consent was obtained from the subjects for informed participation in the research. Also, it is emphasized on the principle of confidentiality of the participants’ information and the implementation of this training for the control group after the end of the experiment. The participants were initially numbered from 1 to 30. After matching based on demographic characteristics, such as age, gender, and history of disease, they were randomly assigned to the test and control groups in odd and even pairs (Figure 1).
Inclusion and exclusion criteria
The inclusion criteria included a specialist doctor’s diagnosis of T2DM, having at least a diploma, and being 55 years old or older. The exclusion criteria included the absence of more than two sessions, unwillingness to continue cooperating in the study, and acquiring an incomplete questionnaire.
Procedures
To collect data, the Maslow’s psychosocial security (PS) questionnaire (Maslow, 1942) was used:
Maslow’s PS
Maslow’s PS questionnaire was created in 1942 to measure different aspects of PS. It has 62 62-question self-report scales and 15 subscales. It includes scales, such as environmental maladjustment (1-6), paranoia (7-11), self-belief (12-16), passion for Life (21-17), depression (22-25), sense of bliss (26-30), social security (31-34), self-awareness (35-37), self-confidence (38-41), nervousness (42-44), disappointment, (45-47), interest in life (48-51), adjustment with others (52-54), feeling of healthiness (55-58), feeling of inferiority (59-62). It is scored with yes and no options. Achieving a high score on this test (62) indicates a person’s high PS and a low score indicates low PS (Maslow, 1942). Maslow reported the value of Cronbach’s α of this questionnaire as 0.66 (Maslow, 1942). Bowen et al. (2010) reported the total Cronbach’s α coefficient of 0.92. Also, Zare and Aminpour (2012) reported a Cronbach’s α coefficient of 0.64 and re-test reliability at two-week intervals of 0.81. In the current research, the validity of the questionnaire has been well evaluated and confirmed using the opinions of supervisors and advisors. Also, the reliability of Maslow’s PS questionnaire was obtained through Cronbach’s α of 0.57.
Procedure
The participants were initially numbered from 1 to 30. After matching based on demographic characteristics, such as age, gender, and history of disease, they were randomly assigned to the test and control groups in odd and even pairs. The method of conducting the research was that after the necessary coordination with the officials of the Freeman Health Diabetes Center, written consent was obtained from the sample to participate in the study after stating the purpose of the study. The questionnaires were mostly completed by the participants and in some cases by the patient with the help of his companion. The test group was separately trained for 8 sessions of 120 minutes (one session per week) with GCBT based on Datiliou and Barashk’s (2006) treatment package, and the control group was placed on the waiting list. The sessions were held by a senior clinical expert. Also, in this research, an attempt was made to maintain the confidentiality of information in all stages of the research.
GCBT intervention plan
The patient’s PS programs were announced through a written self-report by the patient himself/her relatives living with him. It should be noted that the researcher completed the questionnaires in the form of a structured interview with the participants in 15-20 minutes. Table 1 presents the details of the intervention in the test group.
Data analysis
In this study, descriptive statistics (Mean±SD) and inferential statistics analyzed the data (analysis of covariance [ANCOVA]).
Results
Descriptive results
The participants of this research were 30 patients with T2DM. Demographic data that were assessed in this study included age, sex, and education. The Mean±SD of the age of the samples was 58.14±23.47 years. They were in the age range of 55 to 67 years. The highest frequency is related to the age of 55-59 years and the lowest frequency is related to the age of 59-67 years. Table 2 presents the descriptive statistics (Mean±SD) of the variables in the pre-test and post-test stages. As seen, the mean of the test group increased compared to the control group in PS.
Analysis of covariance (ANCOVA)
Before analyzing the data by ANCOVA, the presuppositions of ANCOVA were evaluated. The results of the Kolmogorov-Smirnov test on PS variables were not significant for any of the variables, indicating that the assumption of the data normality test is established (P>0.05) (Table 3).
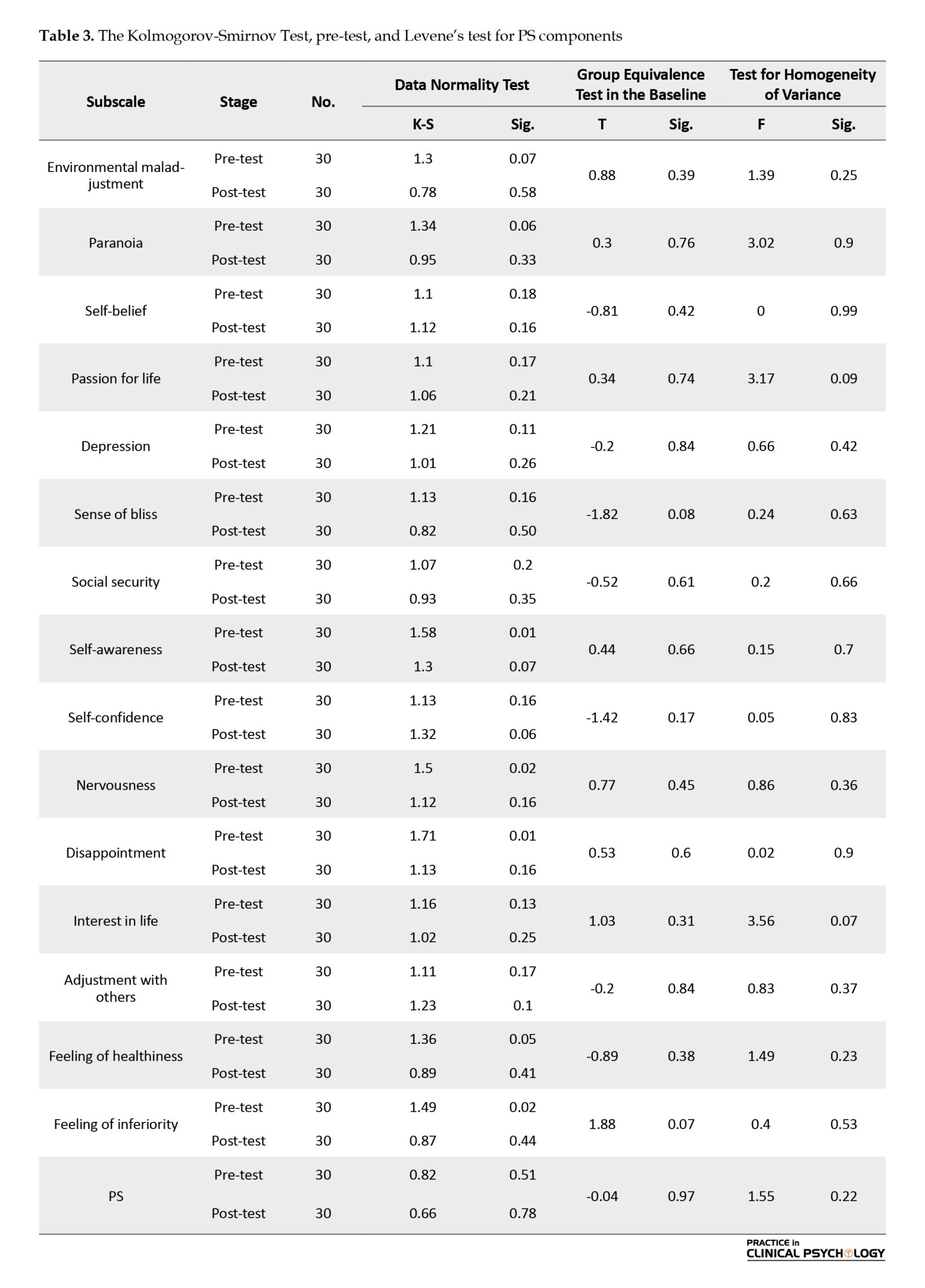
Also, the results of Levene’s test for equality of variances were not significant indicating the assumption that the individual group covariance matrices are equal (homogeneous across groups) and the assumption of equal variance is valid (Table 3). As can be seen in Table 3, the results of the test for homogeneity of variance of the test and control groups are not significant for the PS component; therefore, the variances of the test and control groups are the same.
While it is assumed that the variables in ANCOVA should show linearity in the whole data, this assumption should also be considered that the regression lines should be the same for each group in the research. The results of the test of homogeneity of regression slopes of the research variables have shown that the F value of the interaction for the sameness of the regression line slope for the PS variable (F=3.72) is at a significant level of 0.063, which is insignificant. In other words, the homogeneity of regression slopes is accepted. Table 4 presents the results of the ANCOVA test. As seen, the test results showed that the independent variable was effective on the dependent variable. In other words, the test and control groups have a significant difference in the PS variable (P<0.0001).
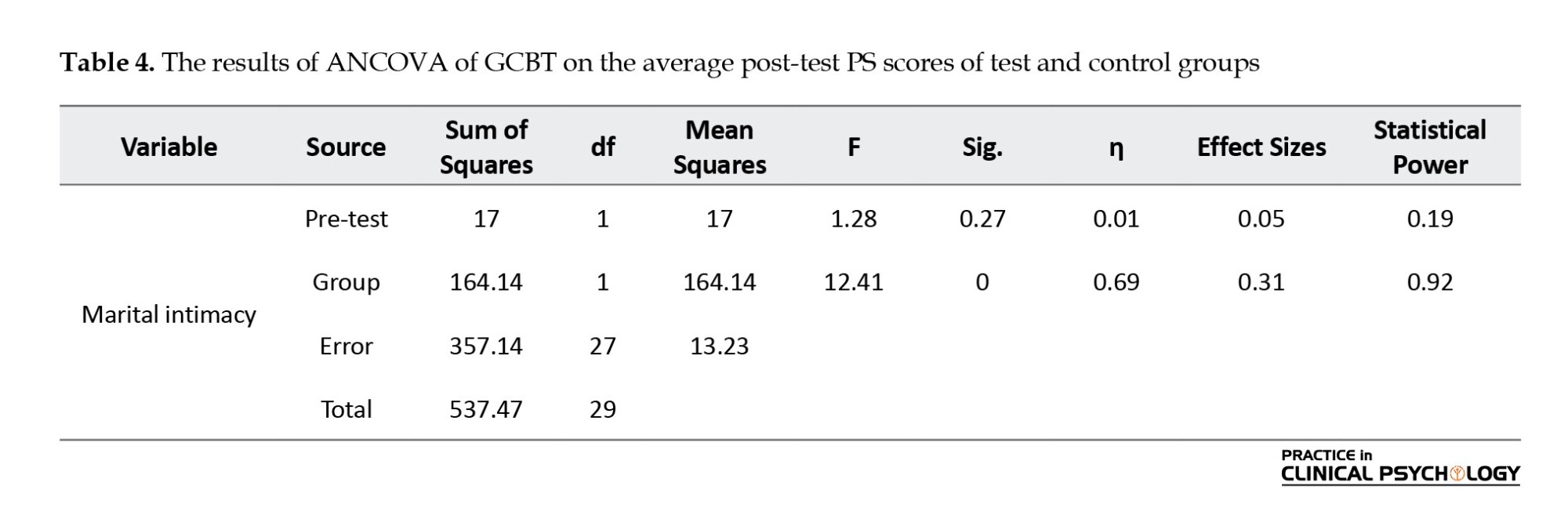
According to the results of ANCOVA by controlling the pre-test effect and calculated according to the F coefficient, a significant difference is observed between the adjusted averages of PS scores according to group membership “test and control” in the post-test stage (P<0.0001). It can be concluded that the null hypothesis was rejected and the GCBT method had a greater effect on the participants of the test group.
The effect size of “practical significance” was 0.31, that is, 31% of the total variance changes or individual differences in the PS of patients with T2DM were caused by the effect of GCBT. The statistical power was 0.92, which indicated the adequacy of the sampling volume. A significant difference is observed between the level of PS of the subjects in the test and control groups (P=0.001, F=12.41). With 95% certainty, the null hypothesis is rejected and the main hypothesis is confirmed, and we conclude that GCBT is effective in increasing the PS of patients with T2DM.
To investigate the effect of GCBT on the components of PS, we use multivariate ANCOVA, where the dependent variable includes the components of PS, environmental maladjustment, paranoia, self-belief, passion for life, depression, sense of bliss, social security, self-awareness, self-confidence, nervousness, disappointment, interest in life, adjustment with others, feeling of healthiness, and feeling of inferiority.
The results of Table 4 show the difference between the post-test of the two groups in the components of PS. GCBT has increased the scores of self-belief, passion for life, sense of bliss, social security, self-awareness, self-confidence, interest in life, adjustment with others, and feeling of healthiness. Also, the scores of environmental maladjustment, paranoia, depression, nervousness, disappointment, and feeling of inferiority decreased in the post-test and all the components of PS are significant (P<0.05). We conclude that GCBT affects the PS components of patients with T2DM.
Discussion
The present study was conducted to investigate the effects of GCBT on the PS in patients with T2DM. The results revealed that GCBT was effective in enhancing and improving the PS of patients with T2DM (P<0.001). GCBT intervention can be introduced as a fruitful psychological intervention. It can increase psychological well-being indicators and greater medical adherence to treatment recommendations. Increasing this method helps prevent the complications of diabetes and improves the psychological health of patients with T2DM. Previous research, such as Welschen (2014), Baker et al., (2016), Serlachius et al., (2016), Pillow et al. (2017), Jesse et al., (2019), Puig-Domingo et al. (2020), Nakao et al., (2021), Pericot-Valverde et al. (2018), and Kamath et al. (2022) have confirmed the effectiveness of GCBT on PS in their research results. Research has shown that GCBT increases PS, reduces depression symptoms, and decreases symptoms of anxiety in women with T2DM. In other words, declined symptoms of depression and anxiety in people with T2DM are associated with improving PS (Adams et al., 2022). The results of some studies have shown that having sufficient motivation and information in women with vaginitis fertility will have a positive effect on PS and disease recovery (Xu et al., 2020). The results of other researchers suggest that PS in people with T2DM can be influenced by positive psychological characteristics, such as life expectancy and efficient attitudes. Nurses can improve their PS by improving efficient and hopeful attitudes in patients with T2DM. Nurses can also help patients with T2DM, who often have cognitive errors, and irrational and destructive beliefs in their lives, to inform patients of their irrational documents and beliefs. Using their knowledge and experience to help modify these misconceptions and promote patient information literacy to create rational and efficient beliefs. As a result, using experiences and enhancing health information, patients modify the misconceptions and documents that cause anxiety and depression and thus reduce their PS.
By examining the content of the materials presented in the psychological safety management training sessions in this research, it can be assumed that the use of behavioral strategies and strategies, such as calming and creating a sense of calm in the affected person have also reduced the psychological symptoms and distress in him. On the other hand, cognitive strategies, such as problem-solving, recognizing cognitive errors and fighting against negative thoughts, logical thinking, and using positive self-talk have probably caused a change in the attitudes and cognitions of patients so that they accepted their illness and rationally they faced its psychological consequences and by applying the skills taught, they took steps to improve themselves and control the disease more effectively. Also, GCBT training sessions, concerning the education of immunity against stress to patients with T2DM, familiarize them with how stress affects them and teach them to look at stressful situations as solvable problems. In addition, different coping methods and their effective management are shown to patients with T2DM. This makes them feel that they have more control over their surroundings, evaluate them as less threatening when dealing with such situations, and when faced with said situations, having more efficient coping skills, they can solve them more effectively, and be safe from the negative psychological effects caused by ineffective coping with stressful situations. Therefore, they can have better control over the anxieties caused by the disease.
Anxiety caused by chronic and permanent diseases, such as diabetes can lead to many psychological complications. Examples include depression, insomnia, anxiety, physical symptoms, and social dysfunction. Anxiety in its chronic state causes the erosion of the physical and mental reserves of the affected person by creating a state of permanent alertness in the body. This plays an effective role in using the mechanism of the learned helplessness effect of the diabetic person on non-compliance with the treatment. This helplessness happens because a person does not accept his diabetes in the early stages of diagnosis and the stress caused by it between the stage of denial and acceptance of the disease due to the occurrence of psychological complications of the disease that was mentioned. This state causes the observance of treatment points in the stage of feeling acceptance and non-observance of it in the stage of illness. The result is that the person does not achieve regular control of his blood sugar, and this teaches the patient that it is not possible to control his blood sugar in both cases of following and not following the treatment; therefore, these issues can be better overcome by teaching destructive thoughts to stop self-deception, and skills to deal with disappointment, failure and unfairness syndrome in meetings.
One of the reasons for the effectiveness of GCBT in increasing the PS of patients with T2DM is that the quality of patient care skills is the result of an individual’s beliefs, thoughts, behavior, and deeds and relates to one’s decisions and performance. As a psychotherapeutic method, GCBT alters the destructive patterns affecting patients’ behavior and emotions (Hofmann et al., 2012). Nurses can emphasize the importance of acquiring cognitive information, feeling efficient, skills, and using these skills by providing GCBT training. Also during the training, people learn fruitful behavioral methods in addition to working on negative thinking. People affected by these tutorials will find the ability to correct automatic thoughts and evaluate their evidence, as well as the documents needed to approve and disapprove those (Jun & Park, 2013).
Implementing GCBT has led to the improvement of PS in patients with T2DM. According to the obtained results, it can be said that the effort to change the attitudes and core and negative beliefs in GCBT by patients with T2DM has led to the improvement of the psychological condition of diabetic patients. In this treatment, the attitude and mental perception of patients about their disease and its symptoms have been changed, and it can be used in psychological clinics and educational workshops to increase adherence to the treatment, the perception of the disease, and the QoL of patients with T2DM.
Conclusion
The GCBT could improve the PS of patients with T2DM. The effort to change the attitudes and core and negative beliefs about the disease and its symptoms in patients with T2DM by the GCBT was successful. The intervention can be used in psychological clinics and educational workshops to increase adherence to the treatment, perception of disease, and quality of life of patients with T2DM.
Recommendations
It is suggested to take help from this treatment method to increase the learning of correct thinking and judgment skills about diabetes and to deal with unrealistic thoughts about this disease. Therefore, counselors and therapists can use this method to improve the PS of patients with T2DM. In addition, it is recommended that planners design programs based on this research to improve the PS of patients with T2DM.
Implications for family therapy/practice
Counselors and therapists of diabetes centers and clinics can use the GCBT approach in their therapy groups and training classes to improve the basic PS, not to be discouraged, and to continue the treatment and as a result, increase the physical health of patients with T2DM.
Research limitations
Not using follow-up was the most remarkable limitation of this research. Also, some sample groups could not participate in the meetings due to illness or some personal problems or did not have enough effort to perform their homework. Also, failure to control the presence of mental illnesses in patients, especially hospitalized patients, was another limitation of the current research. Also, coexisting diseases can be psychological, which can affect the PS variable. This may have affected the results of the current research, which is hoped to improve in subsequent research. The questionnaire was also used in this study to collect data. Therefore, there may be a bias in the information obtained; because some participants may answer some questions with a bias to better show themselves. Also, limiting the research population to diabetic patients referred to the counseling center in Fariman City was one of the limitations of this study. Failure to control some disturbing variables, such as the economic, family, social, and educational status of the research samples, has led to a decrease in the internal validity of the research, which is expected to be improved in future research.
Future research
It is hoped that the output of this study can be a background for further research in the field of PS of patients to help improve and treat patients with T2DM as much as possible. It is suggested that this research be repeated with larger and diverse samples and with long-term follow-ups, and studies to investigate the mediating factors and variables of these interventions. It is also recommended that a special PS program be designed by experts for patients with T2DM and the official integration of this training in diabetes treatment-care programs should be considered by experts and institutions active in this field.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles are considered in this article. The participants were informed of the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them. A written consent has been obtained from the subjects. Principles of the Helsinki Convention was also observed.
Funding
The paper was extracted from the master's thesis of Sima Farimanian, approved by the Department of Health Psychology, Faculty of Psychology, Torbat-e-Jam Branch, Islamic Azad University.
Authors' contributions
Conceptualization and supervision: Sima Farimanian and Mohammad Hossein Bayazi; Methodology: Mohammad Hossein Bayazi; Investigation and writing: All authors.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The researchers thank the patients and all the people who helped us in conducting this research.
References
Abbas, Q., Latif, S., Ayaz Habib, H., Shahzad, S., Sarwar, U., & Shahzadi, M., et al. (2023). Cognitive behavior therapy for diabetes distress, depression, health anxiety, quality of life and treatment adherence among patients with type-II diabetes mellitus: A randomized control trial. BMC Psychiatry, 23(1), 86. [DOI:10.1186/s12888-023-04546-w] [PMID]
Adams, R. N., Athinarayanan, S. J., McKenzie, A. L., Hallberg, S. J., McCarter, J. P., & Phinney, S. D., et al. (2022). Depressive symptoms improve over 2 years of type 2 diabetes treatment via a digital continuous remote care intervention focused on carbohydrate restriction. Journal of Behavioral Medicine, 45(3), 416-427. [DOI:10.1007/s10865-021-00272-4] [PMID]
Ahmad, N. S., Ramli, A., Islahudin, F., & Paraidathathu, T. (2013). Medication adherence in patients with type 2 diabetes mellitus treated at primary health clinics in Malaysia. Patient Preference and Adherence, 7, 525-530. [DOI:10.2147/PPA.S44698] [PMID]
Al Qudah, M. F., Al-Barashdi, H. S., Hassan, E. M. A. H., Albursan, I. S., Heilat, M. Q., & Bakhiet, S. F. A., et al. (2020). Psychological security, psychological loneliness, and age as the predictors of cyber-bullying among university students. Community Mental Health Journal, 56(3), 393–403. [DOI:10.1007/s10597-019-00455-z] [PMID]
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders, Fifth Edition. Washington, DC: American Psychiatric Association. [DOI:10.1176/appi.books.9780890425596]
Baker, A. L., Hides, L., Kelly, P. J., Kay-Lambkin, F., Nasstasia, Y., & Birchwood, M. (2016). Motivational interviewing and GCBT to improve health and wellbeing. In Innovations and Future Directions in the Behavioral and Cognitive Therapies (pp. 171-175). Australia: Australian Academic Press. [Link]
Blackburn, D. F., Swidrovich, J., & Lemstra, M. (2013). Non-adherence in type 2 diabetes: practical considerations for interpreting the literature. Patient Preference and Adherence, 7, 183–189. [DOI:10.2147/PPA.S30613] [PMID]
Bogner, H. R., Morales, K. H., Post, E. P., & Bruce, M. L. (2007). Diabetes, depression, and death: A randomized controlled trial of a depression treatment program for older adults based in primary care (PROSPECT). Diabetes Care, 30(12), 3005-3010. [DOI:10.2337/dc07-0974] [PMID]
Bowen, S., Chawla, N., & Marlatt, G. A. (2010). Mindfulness-based relapse prevention for the treatment of substance use disorders: A clinician’s guide. New York: Guilford Press. [Link]
Collins, M., Corcoran, P., & Perry, I. (2008). Anxiety and depression symptoms in patients with diabetes. Diabetic Medicine, 26(2), 153-161. [DOI:10.1111/j.1464-5491.2008.02648.x]
Datiliou, F., & Barashk, B. (2006). [Cognitive behavioral therapy of couples (Persian)]. Advances in Cognitive Sciences, 8 (3), 80-71. [Link]
Delevry, D., Ho, A., & Le, Q. A. (2021). Association between processes of diabetes care and health care utilization in patients with diabetes: Evidence from a nationally representative US sample. Journal of Diabetes, 13(1), 78-88. [DOI:10.1111/1753-0407.13109] [PMID]
D’'Souza, M. S., Karkada, S. N., Parahoo, K., Venkatesaperumal, R., Achora, S., & Cayaban, A. R. R. (2017). Self-efficacy and self-care behaviors among adults with type 2 diabetes. Applied Nursing Research, 36, 25-32. [DOI:10.1016/j.apnr.2017.05.004] [PMID]
Edmondson, A. (1999). Psychological safety and learning behavior in work teams. Administrative Science Quarterly, 44(2), 350-383. [DOI:10.2307/2666999]
Fisher, L., Glasgow, R. E., & Strycker, L. A. (2010). The relationship between diabetes distress and clinical depression with glycemic control among patients with type 2 diabetes. Diabetes Care, 33(5), 1034–1036. [DOI:10.2337/dc09-2175] [PMID]
Frey, L., Gravestock, I., Pichierri, G., Steurer, J., & Burgstaller, J. M. (2019). Serious adverse events in patients with target-oriented blood pressure management: A systematic review. Journal of Hypertension, 37(11), 2135–2144. [PMID]
Goyal, R., Singhal, M., & Jialal, I. (2023). Type 2 Diabetes. In StatPearls. StatPearls Publishing. [PMID]
Gong, Y., Cheung, S. Y., Wang, M., & Huang, J. C. (2012). Unfolding the proactive process for creativity: Integration of the employee proactivity, information exchange, and psychological safety perspectives. Journal of Management, 38(5), 1611-1633. [DOI:10.1177/0149206310380250]
Hirak, R., Peng, A. C., Carmeli, A., & Schaubroeck, J. M. (2012). Linking leader inclusiveness to work unit performance: The importance of psychological safety and learning from failures. The Leadership Quarterly, 23(1), 107-117. [DOI:10.1016/j.leaqua.2011.11.009]
Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research, 36(5), 427–440. [DOI:10.1007/s10608-012-9476-1] [PMID]
Huges, A. E., Berg, C. A., & Wiebe, D. J. (2012). Emotional processing and self-control in Adolescents with Type 1 Diabetes. Journal of Pediatric Psychology, 37(8), 925-934. [DOI:10.1093/jpepsy/jss062] [PMID]
Jesse, C. D., Creedy, D. K., & Anderson, D. J. (2019). Effectiveness of psychological interventions for women with type 2 diabetes who are overweight or obese: A systematic review protocol. JBI Database of Systematic Reviews and Implementation Reports, 17(3), 281–289. [DOI:10.11124/JBISRIR-2017-003589] [PMID]
Joseph, J. J., & Golden, S. H. (2017). Cortisol dysregulation: The bidirectional link between stress, depression, and type 2 diabetes mellitus. Annals of the New York Academy of Sciences, 1391(1), 20-34. [DOI:10.1111/nyas.13217] [PMID]
Jun, H. J., & Park, M. K. (2013). Cognitive behavioral therapy for tinnitus: Evidence and efficacy. Korean Journal of Audiology, 17(3), 101-104. [DOI:10.7874/kja.2013.17.3.101] [PMID]
Kamath, T., Abdulraouf, A., Burris, S. J., Langlieb, J., Gazestani, V., & Nadaf, N. M., et al. (2022). Single-cell genomic profiling of human dopamine neurons identifies a population that selectively degenerates in Parkinson’s disease. Nature Neuroscience, 25(5), 588-595. [PMID]
Kaplan, H. S., & Robson, A. J. (2009). We age because we grow. Proceedings. Biological sciences, 276(1663), 1837–1844.[DOI:10.1098/rspb.2008.1831] [PMID]
Krishna, P. (2018). Depression, anxiety, and stress levels in patients with type 2 diabetes mellitus. National Journal of Physiology, Pharmacy and Pharmacology, 8(11), 1570-1572. [DOI:10.5455/njppp.2018.8.0929117092018]
Kumar, V., Pavitra, K. S., & Bhattacharya, R. (2024). Creative pursuits for mental health and well-being. Indian Journal of Psychiatry, 66 (Suppl 2), S283-S303. [DOI:10.4103/indianjpsychiatry.indianjpsychiatry_781_23] [PMID]
Li, C., Barker, L., Ford, E. S., Zhang, X., Strine, T. W., & Mokdad, A. H. (2008). Diabetes and anxiety in US adults: Findings from the 2006 Behavioral Risk Factor Surveillance System. Diabetic Medicine, 25(7), 878-881. [DOI:10.1111/j.1464-5491.2008.02477.x] [PMID]
Lindhe, N., Bengtsson, A., Byggeth, E., Engström, J., Lundin, M., & Ludvigsson, M., et al. (2023). Tailored internet-delivered cognitive behavioral therapy for individuals experiencing psychological distress associated with climate change: A pilot randomized controlled trial. Behaviour Research and Therapy, 171, 104438. [DOI:10.1016/j.brat.2023.104438] [PMID]
Lloyd, C. E., Nouwen, A., Sartorius, N., Ahmed, H. U., Alvarez, A., & Bahendeka, S., et al. (2018). Prevalence and correlates of depressive disorders in people with Type 2 diabetes: Results from the International Prevalence and Treatment of Diabetes and Depression (INTERPRET‐DD) study, a collaborative study carried out in 14 countries. Diabetic Medicine, 35(6), 760-769. [DOI:10.1111/dme.13611] [PMID]
Maslow, A. H. (1942). The dynamics of psychological security-insecurity. Journal of Personality, 10(4), 331-344. [DOI:10.1111/j.1467-6494.1942.tb01911.x]
Maslow, A. H., Birsh, E., Honigmann, I., McGrath, F., Plason, A., & Stein, M. (1952). Manual for the Security-Insecurity Inventory. California: Stanford University Press. [Link]
McConville, J., McAleer, R., & Hahne, A. (2017). Mindfulness training for health profession students-the effect of mindfulness training on psychological well-being, learning and clinical performance of health professional students: A systematic review of randomized and non-randomized controlled trials. Explore, 13(1), 26-45. [DOI:10.1016/j.explore.2016.10.002] [PMID]
Meneilly, G. S., Berard, L. D., Cheng, A. Y., Lin, P. J., MacCallum, L., & Tsuyuki, R. T., et al. (2018). Insights into the current management of older adults with type 2 diabetes in the Ontario primary care setting. Canadian Journal of Diabetes, 42(1), 23-30. [DOI:10.1016/j.jcjd.2017.03.003] [PMID]
Montazerolhodjah, M., Sharifnejad, M., & Rajabi, M. (2018). [Assessment of the effect of physical components of urban spaces on sense of security from the viewpoint of the elderly (case study: Khan Square, Yazd City) (Persian)]. Iranian Architecture and Urbanism, 9(15), 91-105. [Link]
Moss-Morris, R., McAlpine, L., Didsbury, L. P., & Spence, M. J. (2010). A randomized controlled Trial of a cognitive behavior therapy-based self-management intervention for irritable bowel syndrome in primary. Care Psychology Medicine, 40(5), 85- 94. [DOI:10.1017/S0033291709990195] [PMID]
GBD 2016 Causes of Death Collaborators. (2017). Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet, 390(10100), 1151-1210. [DOI:10.1016/S0140-6736(17)32152-9] [PMID]
Nakao, M., Shirotsuki, K., & Sugaya, N. (2021). Cognitive-behavioral therapy for management of mental health and stress-related disorders: Recent advances in techniques and technologies. BioPsychoSocial Medicine, 15(1), 16. [DOI:10.1186/s13030-021-00219-w] [PMID]
Ossher, L., Flegal, K. E., & Lustig, C. (2013). Everyday memory errors in older adults. Neuropsychology, Development, and Cognition. Section B, Aging, Neuropsychology and Cognition, 20(2), 220–242. [DOI:10.1080/13825585.2012.690365] [PMID]
Otgaar, H., Howe, M. L., Dodier, O., Lilienfeld, S. O., Loftus, E. F., & Lynn, S. J., et al. (2021). Belief in unconscious repressed memory persists. Perspectives on Psychological Science, 16(2), 454-460. [DOI:10.1177/1745691621990628] [PMID]
Oyewole, O. O., Ale, A. O., Ogunlana, M. O., & Gurayah, T. (2023). Burden of disability in type 2 diabetes mellitus and the moderating effects of physical activity. World Journal of Clinical Cases, 11(14), 3128-3139. [DOI:10.12998/wjcc.v11.i14.3128] [PMID]
Pan, J. Y., Carlbring, P., & Lu, L. (2023). A therapist-guided internet-based cognitive behavioral therapy program for Hong Kong university students with psychological distress: A study protocol for a randomized controlled trial. Internet Interventions, 31, 100600. [DOI:10.1016/j.invent.2022.100600] [PMID]
Pericot-Valverde, I., Elliott, R. J., Miller, M. E., Tidey, J. W., & Gaalema, D. E. (2018). Posttraumatic stress disorder and tobacco use: A systematic review and meta-analysis. Addictive Behaviors, 84, 238–247. [PMID]
Pillow, D., Hale, W. J., Crabtree, M. A., & Hinojosa, T. L., (2017). Exploring the relations between self-monitoring, authenticity, and well-being. Personality and Individual Differences, 116 (1), 393-398. [DOI:10.1016/j.paid.2017.04.060]
Probst, T. M. (2002). The impact of job insecurity on employee work attitudes, job adaptation, and organizational withdrawal behaviors. In J. M. Brett & F. Drasgow (Eds.), The psychology of work: Theoretically based empirical research (pp. 141–168). Mahwah: Lawrence Erlbaum Associates Publishers. [Link]
Puig-Domingo, M., Marazuela, M., & Giustina, A. (2020). COVID-19 and endocrine diseases. A statement from the European Society of Endocrinology. Endocrine, 68(1), 2-5. [DOI:10.1007/s12020-020-02294-5] [PMID]
Raina, S., & Bhan, K. S. (2013). A study of security-insecurity feelings among adolescents in relation to sex, family system and ordinal position. International Journal of Educational Planning and Administration, 3(1), 51-60. [Link]
Riddle, M. C., & Herman, W. H. (2018). The cost of diabetes care -an elephant in the room. Diabetes Care, 41(5), 929 -932. [DOI:10.2337/dci18-0012] [PMID]
Sabourin, B. C., Vallis, T. M., & RPsych, S. C. (2011). Development and pilot-testing of a brief psychosocial group intervention protocol for type 2 diabetes self-management. Canadian Journal of Diabetes, 35(3), 287-294. [DOI:10.1016/S1499-2671(11)53013-8]
Sadock, B. J., Sadock, V. A., & Ruiz, P. (2015). Kaplan and Shaddock’s synopsis of psychiatry: Behavioral science/clinical psychiatry. New York: Wolters Kluwer. [Link]
Saffariantoosi, K., & Khaleghi, M. R. (2024). The mediating role of organizational citizenship behavior in the relationship between career self-efficacy and career success among construction project managers in Mashhad. Current Psychology, 43, 23971–23984. [DOI:10.1007/s12144-024-06127-w]
Sarabadani, A., Hassanzadeh, R., & Emadian, S. O. (2023). [Comparison of the effectiveness of cognitive therapy based on mindfulness and life therapy on mental well-being and psychological security in women with generalized anxiety disorder: A quasi-experimental study (Persian)]. Journal of Rafsanjan University of Medical Sciences, 21(12), 1249-1266. [DOI:10.52547/jrums.21.12.1249]
Schmitt, A., Reimer, A., Hermanns, N., Kulzer, B., Ehrmann, D., & Krichbaum, M., et al. (2017). Depression is linked to hyperglycemia via suboptimal diabetes self-management: A cross-sectional mediation analysis. Journal of Psychosomatic Research, 94, 17-23. [DOI:10.1016/j.jpsychores.2016.12.015] [PMID]
Serlachius, A. S., Scratch, S. E., Northam, E. A., Frydenberg, E., Lee, K. J., & Cameron, F. J. (2016). A randomized controlled trial of cognitive behavior therapy to improve glycaemic control and psychosocial well-being in adolescents with type 1 diabetes. Journal of Health Psychology, 21(6), 1157-1169. [DOI:10.1177/1359105314547940] [PMID]
Skoglund, H., Sivertsen, B., Kallestad, H., & Vedaa, Ø. (2024).Digital cognitive behavioral therapy for insomnia for people with comorbid psychological distress: A large scale randomized controlled trial. Sleep Medicine, 121, 241–250. [DOI:10.1016/j.sleep.2024.06.026] [PMID]
Snoek, F. J. (2002). Psychological aspects of diabetes management". Medicine, 30(1), 14-15. [DOI:10.1383/medc.30.1.14.28265]
Steinke, J. A., Fletcher, L., Niu, Q., & Tetrick, L. E. (2016). Creativity and innovation in cyber security work. In S. J. Zaccaro, R. S. Dalal, L. E. Tetrick, & J. A. Steinke (Eds.), Psychosocial dynamics of cyber security (pp. 111-134). London: Routledge/Taylor & Francis Group. [Link]
Sun, J., Hu, W., Ye, S., Deng, D., & Chen, M. (2023). The description and prediction of incidence, prevalence, mortality, disability-adjusted life years cases, and corresponding age-Standardized rates for global diabetes. Journal of Epidemiology and Global Health, 13(3), 566-576. [DOI:10.1007/s44197-023-00138-9] [PMID]
Surmai, M., & Duff, E. (2022). Cognitive behavioural therapy: A strategy to address pandemic-induced anxiety. The Journal for Nurse Practitioners, 18(1), 36-39. [DOI:10.1016/j.nurpra.2021.10.013] [PMID]
Taormina, R. J., & Sun, R. (2015). Antecedents and outcomes of psychological insecurity and interpersonal trust among Chinese people. Psychological Thought, 8(2), 173–188. [Link]
Tong, A., Wang, X., Li, F., Xu, F., Li, Q., & Zhang, F. Risk of depressive symptoms associated with impaired glucose metabolism, newly diagnosed diabetes, and previously diagnosed diabetes: A meta-analysis of prospective cohort studies. Acta Diabetologica, 53(4), 589-598. [DOI:10.1007/s00592-016-0845-1][PMID]
Toobert, D. J., Hampson, S. E., & Glasgow, R. E. (2000). The summary of diabetes self-care activities measure. Diabetes Care, 23(7), 943- 950. [DOI:10.2337/diacare.23.7.943] [PMID]
Valenzuela, M. J., Münzenmayer, B., Osorio, T., Arancibia, M., & Madrid, E. (2018). [Association between depressive symptoms and metabolic control in patients with type 2 diabetes mellitus: a cross-sectional study (Spanish)]. Revista Medica de Chile, 146(12), 1415–1421. [DOI:10.4067/s0034-98872018001201415] [PMID]
Zhang, C. X., Chen, Y. M., & Chen, W. Q. (2008). Association of psychosocial factors with anxiety and depressive symptoms in Chinese patients with type 2 diabetes. Diabetes Research and Clinical Practice, 79(3), 523-530. [DOI:10.1016/j.diabres.2007.10.014] [PMID]
Zhang, Y., Fang, Y., Wei, K. K., & Chen, H. (2010). Exploring the role of psychological safety in promoting the intention to continue sharing knowledge in virtual communities. International Journal of Information Management, 30(5), 425-436. [DOI:10.1016/j.ijinfomgt.2010.02.003]
Xu, J., Bian, G., Zheng, M., Lu, G., Chan, W. Y., & Li, W., et al. (2020). Fertility factors affect the vaginal microbiome in women of reproductive age. American Journal of Reproductive Immunology, 83(4), e13220. [DOI:10.1111/aji.13220] [PMID]
Xu, Z., Wang, H., & Suntrayuth, S. (2022). Organizational climate, innovation orientation, and innovative work behavior: The mediating role of psychological safety and intrinsic motivation. Discrete Dynamics in Nature and Society, 1-10. [DOI:10.1155/2022/9067136]
Wang, J., Long, R., Chen, H., & Li, Q. (2019). Measuring the psychological security of urban residents: Construction and validation of a new scale. Frontiers in Psychology, 10, 2423. [PMID]
Welschen, L. M., van Oppen, P., Bot, S. D., Kostense, P. J., Dekker, J. M., & Nijpels, G. (2013). Effects of a cognitive behavioral treatment in patients with type 2 diabetes when added to managed care; A randomised controlled trial. Journal of Behavioral Medicine, 36(6), 556-566. [DOI:10.1007/s10865-012-9451-z] [PMID]
Type of Study: Original Research Article |
Subject:
Cognitive behavioral
Received: 2024/05/27 | Accepted: 2024/07/23 | Published: 2024/10/2
Received: 2024/05/27 | Accepted: 2024/07/23 | Published: 2024/10/2
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |