Volume 12, Issue 2 (Spring 2024)
PCP 2024, 12(2): 179-188 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghazaei M, Abbas Zadeh F. Investigating the Relationship Between Sluggish Cognitive Tempo and Quality of Life With Controlling Anxiety, Depression, and Attention Deficit Hyperactivity Disorder Symptoms in Iranian College Students. PCP 2024; 12 (2) :179-188
URL: http://jpcp.uswr.ac.ir/article-1-911-en.html
URL: http://jpcp.uswr.ac.ir/article-1-911-en.html
1- Department of Psychology, Faculty of Humanities, Sajjad University, Mashhad, Iran. , ma.ghazayi@yahoo.com
2- Department of Psychology, Shandiz Institute of Higher Education, Mashhad, Iran.
2- Department of Psychology, Shandiz Institute of Higher Education, Mashhad, Iran.
Keywords: Attention deficit disorder with hyperactivity, Anxiety, Sluggish cognitive tempo, Depression, Quality of life (QoL)
Full-Text [PDF 602 kb]
(970 Downloads)
| Abstract (HTML) (3110 Views)
Full-Text: (657 Views)
Introduction
Sluggish cognitive tempo (SCT) in children and adults is characterized by various problems, such as mental fogginess, confusion, sluggishness, drowsiness, confusion, hypoactivity, staring, and daydreaming (Flannery et al., 2014). Barkley (2012) reported high SCT symptoms in 5.8% of all adults. Recent studies regard SCT as an essential psychological and psychiatric construct affecting different aspects of a person’s life (Barkley, 2013; Barkley, 2014). It was previously thought that SCT was associated with attention deficit disorder (ADD) (Marshall et al., 2014); however, it has recently been considered a separate condition that is usually associated with ADD or attention deficit disorder with hyperactivity disorder (ADHD). Barkley (2013) suggested that SCT is present in people without ADHD; accordingly, 40% to 50% of people who had significant symp-toms of SCT lacked apparent symptoms of ADHD (Barkley, 2013).
Subjective belief in mental and physical health and well-being is known as the quality of life (QoL) (CDC, 2009). Combs et al. (2014) concluded that SCT is correlated with poor physical, mental, and total QoL. According to Barkley (2012), SCT can affect different domains of life even more than ADHD (e.g. social life, job, and self-care). Becker & Langberg (2013) found that SCT symptoms have a negative social impact as well as low academic achievement in college students, even after controlling for demographic variables and ADHD symptoms. SCT is correlated with self-reported problems in executive functioning (self-control, problem-solving, self-organization, time management, self-regulation of emotion, and self-motivation in daily life) (Barkley, 2012; Wood et al., 2017)
In addition, some studies have shown a strong correlation between SCT and disorders such as depression and anxiety (Becker et al., 2014; Kamradt et al., 2018). Symptoms of depression and anxiety are frequently comorbid with SCT (Barkley, 2013). Function impairment in several domains, including health, job performance, and social relationships, is a common occurrence in depressive and anxiety disorders (Brenes, 2007); therefore, Bernes (2007) concluded that anxiety and depression symptoms harm all dimensions of QoL. Also, previous research has shown that QoL in people with ADHD is low (Able et al., 2007; Das et al., 2012; Lensing et al., 2013). Considering the close relationship between disorders such as depression and anxiety and core symptoms of ADHD (hyperactivity, inattention, and impulsivity) with SCT and the impact of all these disorders on QoL, the research question is to what extent SCT as a separate construct is associated with QoL (Becker & Langberg, 2013).
Despite many studies on the consequences of SCT, there has been no observed research on the effect of SCT on QoL after controlling for ADHD symptoms (hyperactivity, inattention, and impulsivity), anxiety, and depression in the Iranian population. Furthermore, published research in Iran about the consequences of SCT on QoL in adults is scarce; therefore, this study investigates whether SCT affects QoL and whether this effect will persist after controlling for ADHD symptoms, depression, and anxiety in Iranian college students. The research hypotheses are as follows:
1. SCT is negatively correlated to the QoL;
2. SCT is still negatively correlated to the QoL if ADHD symptoms are controlled;
3. SCT is still negatively correlated to the QoL if depression symptoms are controlled;
4. SCT is still negatively correlated to the QoL if anxiety symptoms are controlled;
5. SCT is still negatively correlated to the QoL if ADHD, depression, and anxiety symptoms are controlled.
Materials and Methods
Study participants and procedures
This descriptive correlational study was conducted on college students in Mashhad City, Iran. The participants were 279 students selected by the convenience sampling method from September 2020 to February 2021. In regression correlation research, considering at least 15 and 50 subjects for each predictive variable can be a reasonable estimate (Beshlideh, 2012). Therefore, considering four predictive variables in the present study, the number of 279 participants is sufficient. Sajjad University and Shandiz Institute of Higher Education were selected for sampling. During the COVID-19 pandemic, classes in Iranian colleges were not held face-to-face; therefore, students and teachers used to form groups in online applications, such as Telegram and WhatsApp, to communicate and transfer information. An electronic link to the questionnaires was created with the Porsline site to conduct the research. The electronic link to the questionnaires was sent to these college groups on Telegram and WhatsApp. In the electronic link, the aim of the study was briefly explained, and students were asked to answer the questions. By viewing the questionnaire link in their virtual study group, the students responded to its questions if they agreed. In addition, the age range of 18 to 40 years was considered the criteria for entering this study. If the students wanted to know the evaluation results, they could enter their e-mail address at the end of the questionnaire. In the middle of the questionnaire, a question measured the attention and correctness of the participants’ answers. The question was as follows: “I have traveled to space in the last year.” Participants were excluded from the sample if they answered this question positively. A total of 16 participants were excluded because of positive answers to this question. In addition, the report of the diagnosis of a psychiatric disorder or the use of psychiatric drugs was the exclusion criteria. Meanwhile, 5 participants were excluded because of the use of psychiatric drugs. The final sample was 279 participants.
Study instruments
Barkley adult ADHD rating scale-iV (BAARS-IV)
The Barkley adult ADHD rating scale-IV (BAARS-IV) (Barkley, 2011) has 27 items that include the diagnostic and statistical manual of mental disorders diagnostic criteria for ADHD. The participants answered each item based on a 4-point scale (1=not at all, 2=sometimes, 3=often, and 4=very often). Nine items measure attention deficit, three items for impulsivity, six for hyperactivity, and nine for SCT. Inattention, hyperactivity, and impulsivity symptoms were used to calculate ADHD symptom scores. Nine SCT symptoms were used to calculate the SCT score. The total score of ADHD symptoms can be between 18 and 72, and the total score of SCT symptoms can be between 9 and 36. Subjects who score above 54 on the 18 ADHD questions are individuals who have symptoms of ADHD. The onset of symptoms before the age of 12 years and functional impairment in at least two settings (school, home, work, and social relationships) are needed for diagnosis (Barkley, 2012). Barkley, (2011) reported high internal consistency for inattention (α=0.90), hyperactive-impulsive (α=0.80), and SCT (α=0.90). The correlation of the score of this scale with the scores of a collateral reporter is in the range of 0.59 to 0.76; hence, its validity is appropriate (Barkley, 2011). This questionnaire has been translated into Persian. In the Iranian population, convergent validity was appropriate, and its reliability using internal consistency was 0.71 for inattention, 0.72 for hyperactive symptoms, 0.73 for impulsive symptoms, and 0.77 for SCT (Ghazaei et al., 2012). In the current study, the Cronbach α for ADHD and SCT was 0.74 and 0.79, respectively.
Depression, anxiety, and stress scale
The depression, anxiety, and stress scale (DASS) (Lovibond & Lovibond, 1995) is a self-reported instrument. DASS measures negative emotions of stress, depression, and anxiety. A total of 14 questions are assigned for each subscale. The questions are scored based on a 4-point scale from 0 (does not apply to me at all) to 3 (extremely applies to me). The sum of scores in each subscale can be from 0 to 42. We used the subscales of anxiety and depression. The Cronbach α for the depression, anxiety, and stress subscales has been reported in the range of 0.89 to 0.97 (Zlomke, 2009). The correlation between the DASS and other scales of depression and anxiety is appropriate (Lovibond & Lovibond, 1995). This questionnaire has been translated into Persian. In an Iranian study, the convergence validity of the DASS was confirmed by a high correlation with the Beck depression inventory and Beck anxiety inventory, and its reliability using the Cronbach α coefficient was 0.90 for anxiety and 0.93 for depression (Asghari et al., 2008). In the current study, the Cronbach α for depression and anxiety was 0.83 and 0.8, respectively.
36-item short-form health survey
The 36-item short-form health survey (SF-36) measures QoL and functional deficits resulting from an illness (Ware & Sherbourne, 1992). SF-36 includes two dimensions as follows: the physical dimension with 21 questions and the mental dimension with 15 questions. The SF-36 mental part assesses the QoL during the last 4 weeks in the following four subscales: limitations in daily activities because of emotional problems, vitality (energy and fatigue), limitations in daily activities because of social problems, and mental health. In addition, the SF-36 physical part assesses the QoL during the last 4 weeks in four subscales, namely physical functioning, physical role, pain, and general health. Each question is scored from 0 to 100, and the total score in each subscale is obtained from the average sum of the scores of the questions related to that subscale. Therefore, the total score and subscales can vary from 0 to 100. Higher scores indicate the perceived or functioning QoL. The internal consistency for the subscales ranged from 0.74 to 0.86 based on the Cronbach α method. The SF-36 is widely used and is considered a valid and reliable instrument (McHorney et al., 1994). This questionnaire has been used in more than fifty countries worldwide and has been translated into Persian. Many studies have confirmed its validity and reliability (Montazeri et al., 2006). In the current study, the Cronbach α for mental, physical, and total QoL was 0.72, 0.79, and 0.76, respectively.
Data analysis
The SPSS software, version 24, was used for data analysis. Descriptive statistics were used to obtain the variables Means±SD. Pearson’s correlation coefficient was used to calculate the correlation between the variables. Finally, hierarchical regression analysis was used to examine the hypotheses. It should be noted that all statistical tests were calculated at a confidence level of 95% (P<0.05).
Results
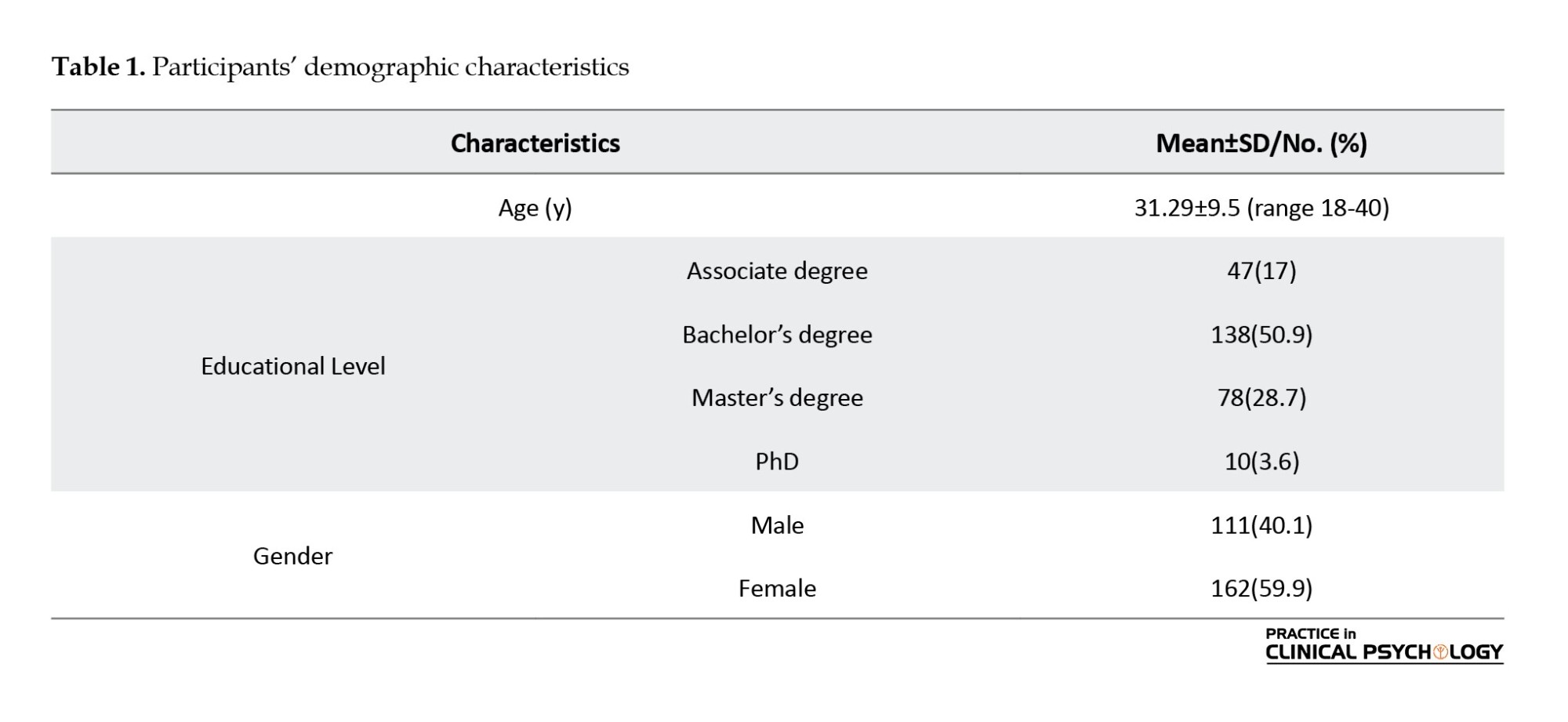
Table 1 presents the participants’ demographic characteristics. The average age of the participants was 31.29 years. Meanwhile, 40.1% of the participants were male, and 59.9% were female.
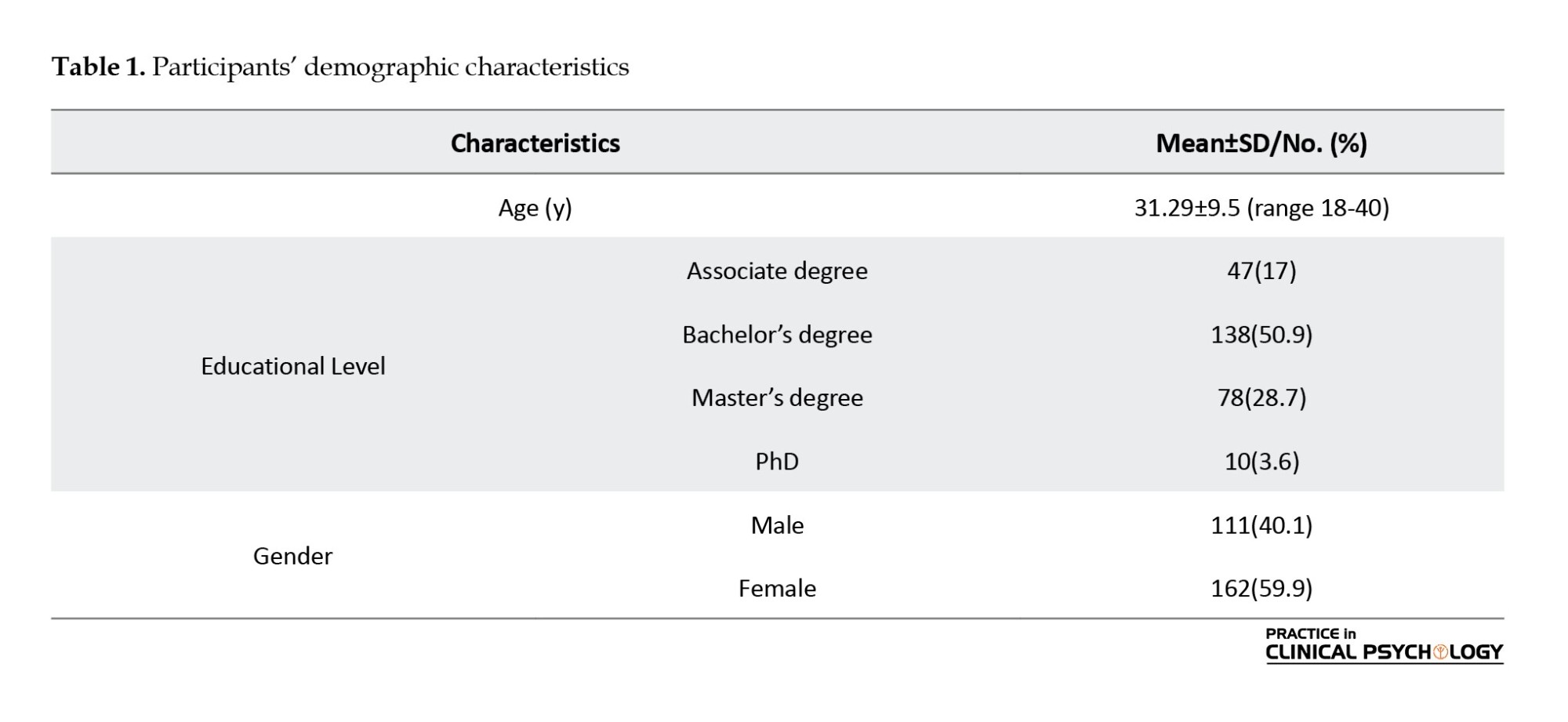
The result of multivariate analysis of variance and then of analysis of variance showed that SCT, ADHD, depression, and anxiety did not differ significantly between men and women; however, the QoL was considerably higher in women compared to men. Furthermore, the result of the multivariate variance analysis showed that SCT, ADHD, depression, anxiety, and QoL did not differ significantly between various levels of education. Also, 6 participants were excluded due to scores of three standard deviations above the mean in SCT and ADHD. Table 2 shows descriptive statistics of the research variables.
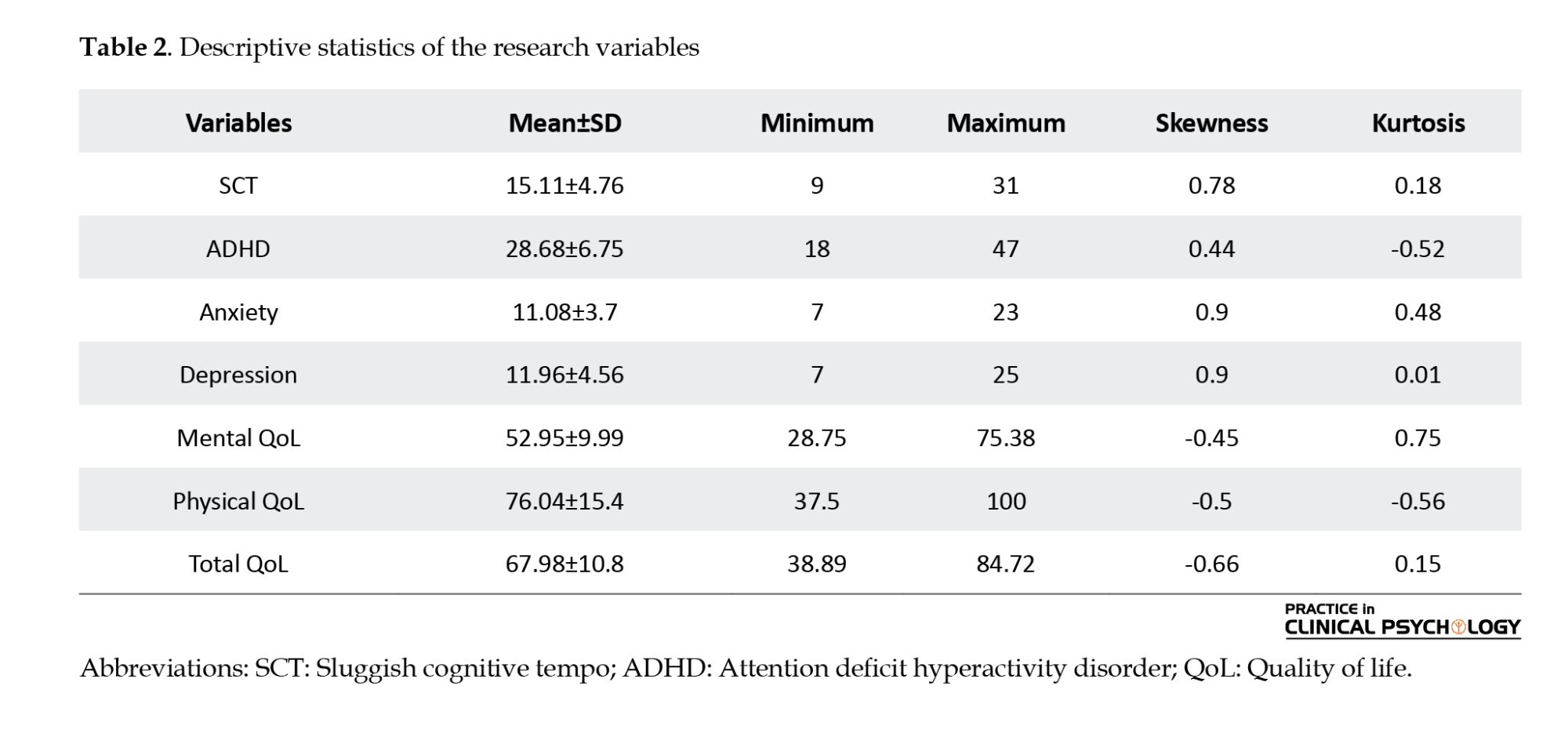
According to Table 2, the skewness and kurtosis were between -1 and +1; therefore, the variables are normal and suitable for parametric tests. We conducted a correlation analysis to examine the association among all the variables, and the correlation matrix is shown in Table 3.
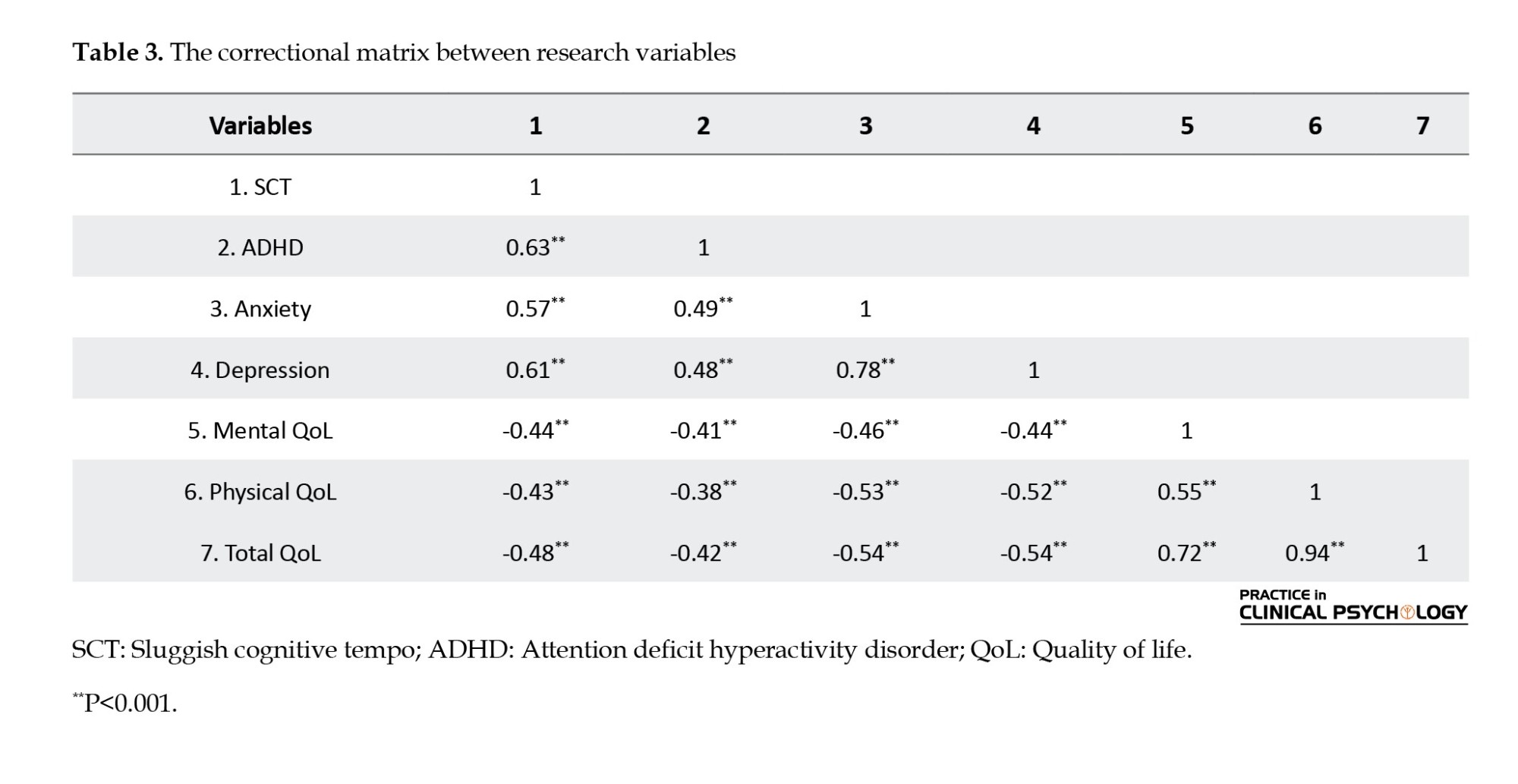
According to Table 3, SCT was positively related to anxiety, depression, and ADHD (P<0.001). QoL was negatively associated with SCT, anxiety, depression, and ADHD (P<0.001).
Hierarchical regression analysis was used to investigate the research hypotheses and answer whether SCT is still related to the QoL if ADHD, depression, and anxiety are controlled. In this method, we first enter the control variables, i.e. depression, anxiety, and ADHD symptoms, into the regression equation and then add the SCT. Table 4 shows the results of hierarchical regression for predicting QoL based on SCT after controlling for the ADHD Symptoms variable.
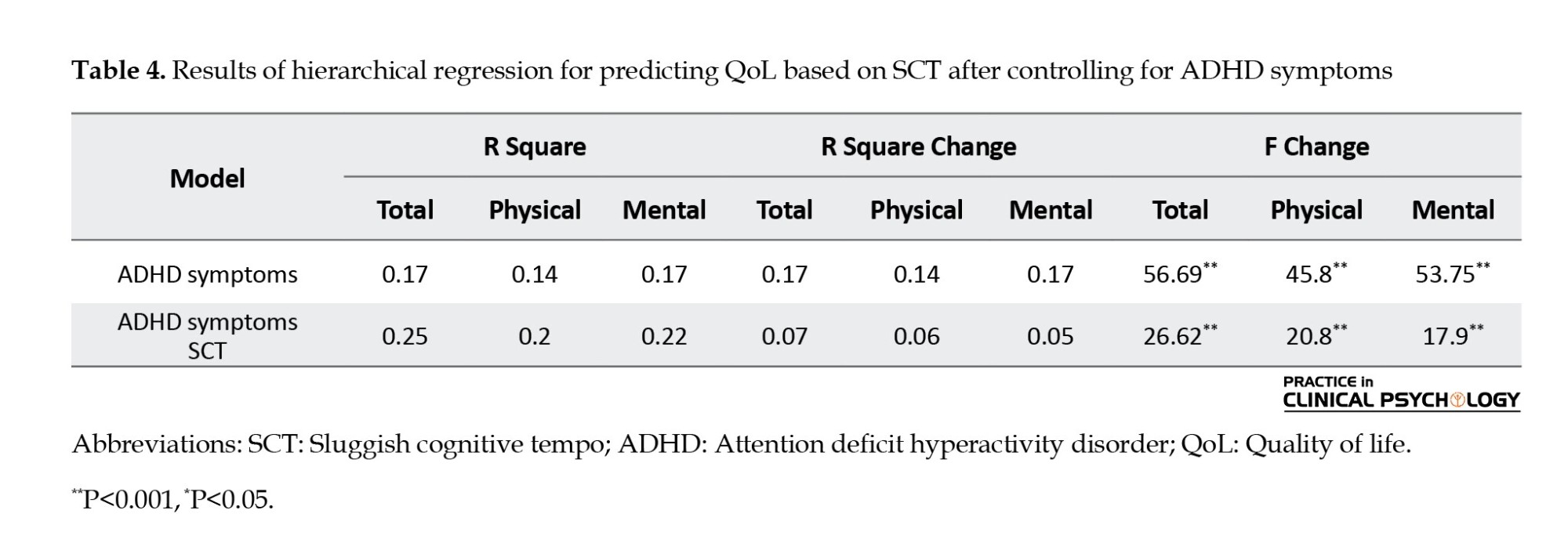
Table 4 shows that ADHD symptoms account for 17% of the variance of the total QoL, 14% of the physical dimension, and 17% of the mental dimension. The SCT and ADHD variables account for 25% of the variance of the total QoL, 20% of the variance of the physical dimension, and 22% of the variance of the mental dimension. R Square change was 7% for total QoL (F change=26.62, P<0.0001), 6% for the physical dimension of QoL (F change=20.8, P<0.0001), and 5% for the mental dimension of QoL (F change=17.9, P<0.0001), after SCT entry, which is significant. In other words, SCT, after controlling ADHD, can still account for a significant percentage of the total QoL and mental and physical dimensions of QoL. Table 5 shows the results of hierarchical regression for predicting QoL based on SCT after controlling for the depression variable.
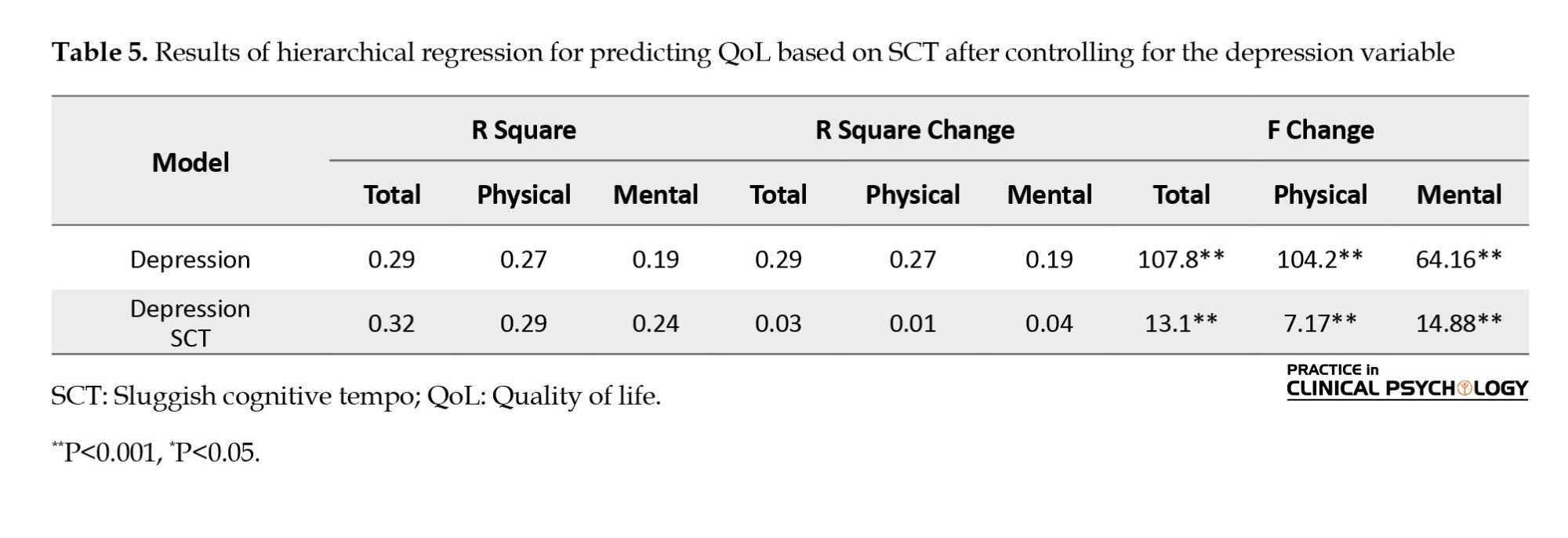
Table 5 shows that depression accounts for 29% of the variance of the total QoL, 27% of the physical dimension, and 19% of the variance of the mental dimension. The SCT and depression variables account for 32% of the variance of the total QoL, 29% of the variance of the physical dimension, and 24% of the variance of the mental dimension. R Square change was 3% for total QoL (F change=13.1, P<0.0001), 1% for the physical dimension of QoL (F change=7.1, P<0.0001), and 4% for the mental dimension of QoL (F change=14.88, P<0.0001), after SCT entry, which is significant. In other words, SCT, after controlling depression, can still account for a significant percentage of the total QoL, physical and mental dimensions of QoL. Table 6 shows the results of hierarchical regression for predicting QoL based on SCT after controlling for the anxiety variable.
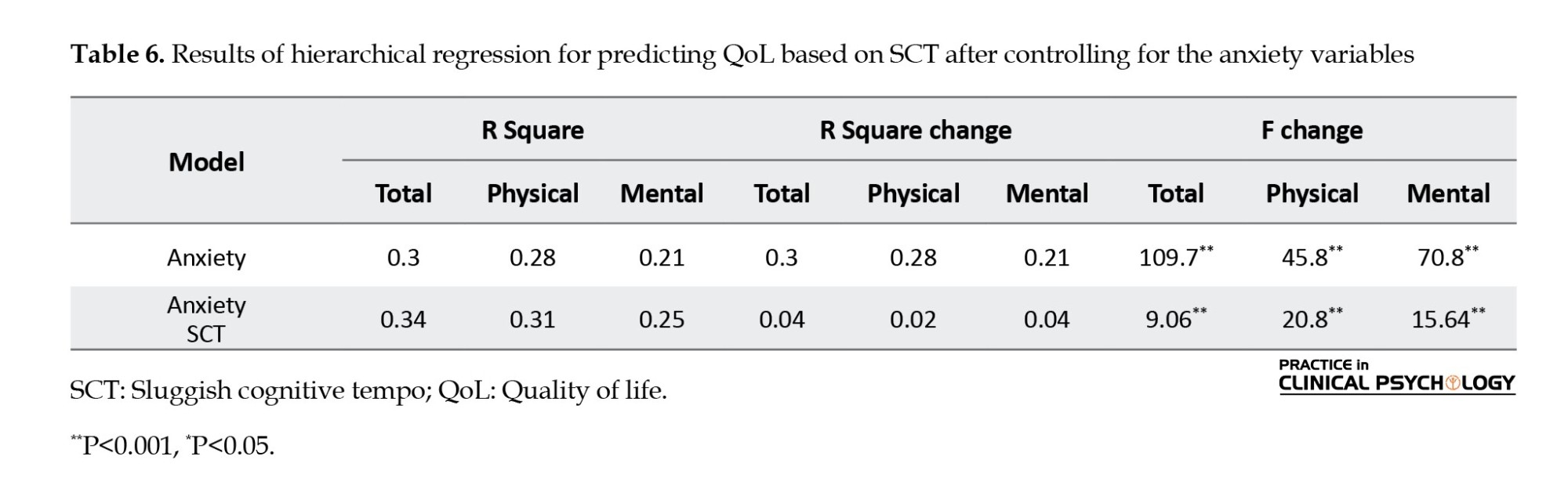
Table 6 shows that anxiety accounts for 30% of the variance of the total QoL, 28% of the physical dimension, and 21% of the variance of the mental dimension. The SCT and anxiety variables account for 34% of the variance of the total QoL, 31% of the variance of the physical dimension, and 25% of the variance of the mental dimension. R Square change was 4% for total QoL (F change=9.06, P<0.0001), 2% for the physical dimension of QoL (F change=20.8, P<0.0001), and 4% for the mental dimension of QoL (F change=15.64, P<0.0001), after SCT entry, which is significant. In other words, SCT, after controlling anxiety, can still account for a significant percentage of the total QoL and physical and mental dimensions of QoL. Table 7 shows the results of hierarchical regression for predicting QoL based on SCT after controlling for the depression, anxiety & ADHD symptoms variable.
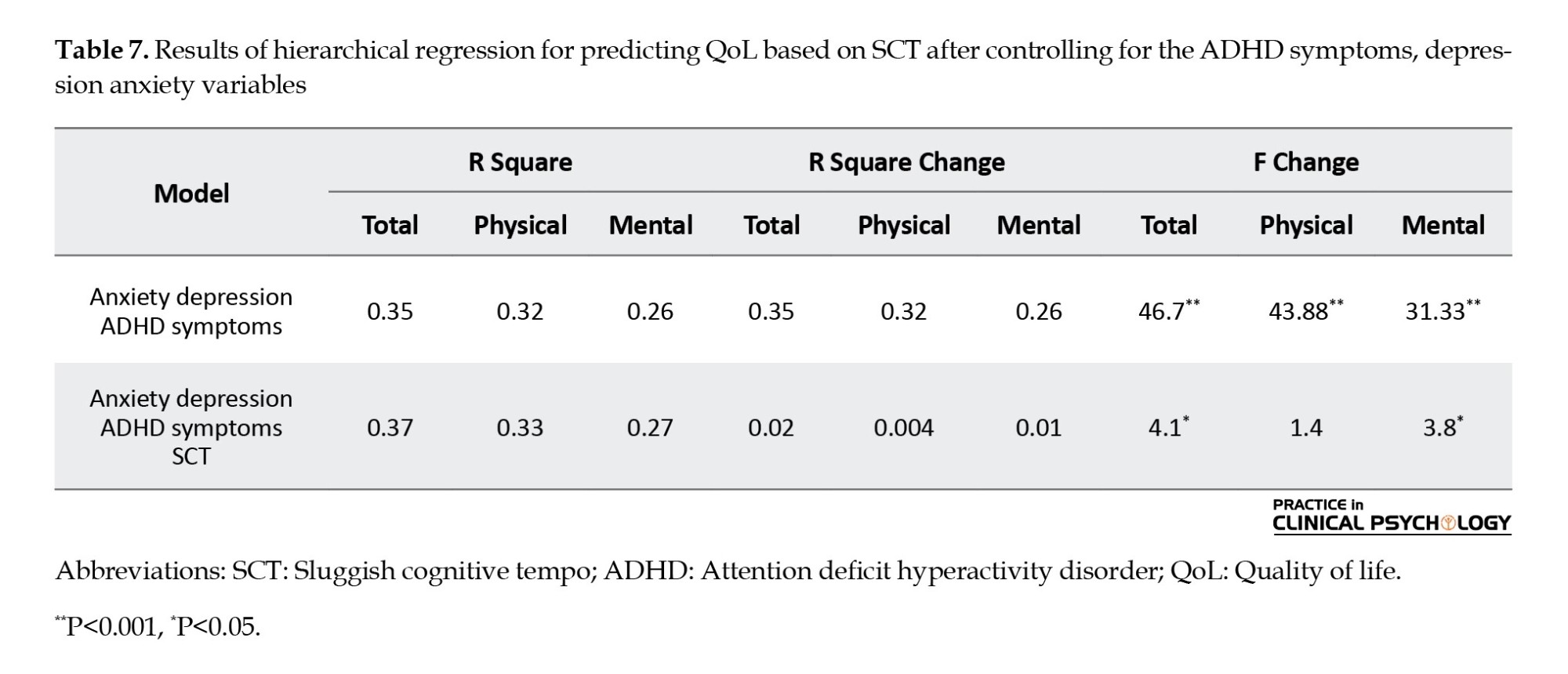
The results from Table 7 showed that ADHD symptoms, depression, and anxiety account for 35% of the variance of the total QoL, 32% of the variance of the physical dimension, and 26% of the variance of the mental dimension. The SCT, ADHD symptoms, depression, and anxiety variables account for 37% of the variance of the total QoL, 33% of the variance of the physical dimension, and 27% of the variance of the mental dimension. After the SCT entry, R square change was 2% for total QoL (F change=4.1, P=0.031), 0.4% for the physical dimension of QoL (F change=1.4, P=0.09), and 1% for the mental dimension of QoL (F change=3.8, P=0.02). In other words, SCT, after controlling ADHD, depression, and anxiety, can still account for a significant percentage of the total QoL and mental dimensions of QoL. However, SCT, after controlling depression, cannot make a meaningful change in the physical dimension of QoL.
Discussion
This study aimed to investigate whether SCT affects the QoL and whether this effect will persist after controlling for depression, ADHD, and anxiety symptoms. The results showed depression, anxiety, ADHD, and SCT symptoms are correlated to poor QoL in Mashhad college students. Hierarchical regression analysis was used to answer whether SCT can still be correlated with the lower QoL after controlling depression, anxiety, and ADHD. The results of hierarchical regression analysis showed that SCT is negatively correlated with the total QoL and mental dimensions of QoL after controlling anxiety, depression, and ADHD symptoms both individually and together. However, SCT, after controlling three variables of depression, anxiety, and ADHD, could not account for a significant variance in the physical dimension of QoL. However, after controlling the variables individually, SCT can still create a significant variance in this dimension.
Limited studies have addressed the relationship between SCT and QoL, and current research showed that SCT is negatively related to lower physical, mental, and total QoL. SCT is multidimensional and includes cognitive components (e.g. fantasy and confusion) and behavioral components (such as slow motion and slowness). Therefore, SCT can reduce the QoL in the physical dimension by reducing energy levels, reducing the ability to work and perform daily activities, and reducing sleep quality. In addition, impairment in occupational and academic performance is observed due to SCT symptoms (Barkley, 2012). Given the impact of SCT on these areas, SCT also reduces the mental dimension of QoL and creates negative emotions (Barkley, 2014; Combs et al., 2014). Furthermore, SCT reduces the mental dimension of QoL by creating social problems (Becker & Lungberg, 2013; Flannery et al., 2016).
Furthermore, current research showed that SCT is negatively correlated with the total QoL and mental dimensions of QoL after controlling ADHD symptoms. A study similar to the current study reported that even after controlling for ADHD symptoms and internalizing disorder, SCT was correlated with impaired social functioning and adjustment problems in adults (Flannery et al., 2017). Another study showed that after statistically controlling for symptoms of ADHD, oppositional defiant disorder, generalized anxiety disorder, intelligence, and major depressive disorder, SCT was still associated with avoidance and impaired social functioning (Burns et al., 2013). Thus, although SCT symptoms are related closely to The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition in attention, the current study suggests that SCT symptoms may represent a separable symptom dimension that is distinct from the inattentive and combined types of ADHD (Mayes et al., 2022). Some studies have shown that SCT can cause different problems than ADHD. The inattentive type of ADHD is more correlated to time management. In contrast, the combined type of ADHD is related to self-control, and SCT is correlated with self-organization and problem-solving (Gody et al., 2023). Gody et al., (2023) showed that SCT symptoms are more associated with executive dysfunctions than the combined type of ADHD. Also, the daydreamy-sleepy feature of SCT, one of the most critical differences between SCT and ADHD, can reduce the QoL because the person lacks the necessary energy to perform daily and social activities (Barkley, 2012). Another study found that five SCT symptoms (losing the train of thought, being easily confused, seeming drowsy, slow thinking, and slow-moving) show convergent and discriminant validity (Burns et al., 2013).
The current study showed that SCT is negatively associated with the total QoL and mental dimensions of QoL after controlling anxiety and depression. Combs et al. (2014) showed that even when demographic variables, anxiety, and mood disorder are controlled, SCT symptoms play an essential role in the QoL of adults. Also, other studies concluded that SCT is distinct from depression and anxiety (Becker et al., 2014; Burns et al., 2013). Smith et al. (2019) also found that despite the strong correlation of SCT with depression and anxiety, SCT remains distinct.
Finally, the current study showed that SCT, after controlling three variables of depression, anxiety, and ADHD, could not account for a significant variance in the physical dimension of QoL. Wood et al. (2020) reported that SCT symptoms do not have a significant relationship with function impairment after controlling for psychological disorders (depression, anxiety, and ADHD) and lifestyle variables (substance abuse, sleep problems). The questionnaire they used to assess performance measured mostly physical dimensions, such as vehicle ability and accident history. They concluded SCT symptoms can represent a lifestyle that does not cause severe problems for college students. These students had accepted SCT as a personality trait and had found ways to adapt despite having these symptoms (Wood et al., 2020).
Conclusion
SCT is associated with low QoL among Iranian college students, and this relationship remains present after controlling for depression, anxiety, and ADHD. In addition, the results of this research emphasize the importance of considering QoL in prospective research and SCT intervention.
Study limitations
The current study had several limitations. First, the correlational nature of the results limits inferences on causality, and longitudinal studies on SCT and its impact on QoL are needed. Our data was collected from Mashhad college students, and we should be careful in generalizing the results. The present study used self-report scales, which may affect the results. In addition, the study relied on a non-clinical community sample, using continuous ADHD, depression, and anxiety traits as predictors instead of actual ADHD, depression, and anxiety diagnoses. In addition, due to the spread of the COVID-19 virus, it was difficult to reach students in person, and for this reason, electronic questionnaires were used, which can affect the validity of the results. Results from this study point toward the need for added research with larger samples that can examine the longitudinal consequences of SCT on QoL. The relationship between SCT and different performance domains should be considered in future research.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The purpose of the study and the steps of the research implementation were informed to the participants. They were assured about the confidentiality of the information and the possibility of leaving the study at any moment. In addition, they were informed by e-mail if they wanted to know the evaluation results.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants in this study.
Reference
Able, S. L., Johnston, J. A., Adler, L. A., & Swindle, R. W. (2007).Functional and psychosocial impairment in adults with undiagnosed ADHD. Psychological Medicine, 37(1), 97-107. [DOI:10.1017/S0033291706008713] [PMID]
Asghari Moghadam, M. A., Saed, F., Dibaj Nia, P., & Zanganeh, J. (2008). [A preliminary study on the validity and reliability of the Depression, anxiety and stress in nonclinical samples (DASS) (Persian)]. Scientific-Research Journal of Shahed University (Daneshvar), 15(31), 23-38. [Link]
Barkley, R. A. (2011). Barkley Adult ADHD Rating Scale-IV (BAARS-IV). New York City: The Guilford Press. [Link]
Barkley, R. A. (2012). Distinguishing sluggish cognitive tempo from attention-deficit/hyperactivity disorder in adults. Journal of Abnormal Psychology, 121(4), 978-990. [DOI:10.1037/a0023961] [PMID]
Barkley, R. A. (2013). Distinguishing sluggish cognitive tempo from ADHD in children and adolescents: executive functioning, impairment, and comorbidity. Journal of Clinical Child & Adolescent Psychology, 42(2), 161-173. [DOI:10.1080/15374416.2012.734259] [PMID]
Barkley, R. A. (2014). Sluggish cognitive tempo (concentration deficit disorder?): Current status, future directions, and a plea to change the name. Journal of Abnormal Child Psychology, 42(1), 117-125. [DOI:10.1007/s10802-013-9824-y] [PMID]
Barkley, R. A. (2014). Concentration deficit disorder (sluggish cognitive tempo). Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment, 81-115. Guilford Publications. [Link]
Becker, S. P. (2014). Sluggish cognitive tempo and peer functioning in school-aged children: A six-month longitudinal study. Psychiatry Research, 217(1-2), 72-78. [DOI:10.1016/j.psychres.2014.02.007] [PMID]
Becker, S. P., & Langberg, J. M. (2013). Sluggish cognitive tempo among young adolescents with ADHD: Relations to mental health, academic, and social functioning. Journal of Attention Disorders, 17(8), 681-689. [DOI:10.1177/1087054711435411] [PMID]
Becker, S. P., Langberg, J. M., Luebbe, A. M., Dvorsky, M. R., & Flannery, A. J. (2014). Sluggish cognitive tempo is associated with academic functioning and internalizing symptoms in college students with and without attention‐deficit/hyperactivity disorder. Journal of Clinical Psychology, 70(4), 388-403. [DOI:10.1002/jclp.22046] [PMID]
Beshlideh, K. (2012). [Research methods and statistical analysis of research using SPSS and AMOS (Persian). Ahvaz: shahid Chamran University Publications; 2012. [Link]
Brenes, G. A. (2007). Anxiety, depression, and quality of life in primary care patients. Primary Care Companion to the Journal of Clinical Psychiatry, 9(6), 437–443. [DOI:10.4088/PCC.v09n0606] [PMID]
Burns, G. L., Servera, M., Bernad, M.delM., Carrillo, J. M., & Cardo, E. (2013). Distinctions between sluggish cognitive tempo, ADHD-IN, and depression symptom dimensions in Spanish first-grade children. Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 42(6), 796–808. [DOI:10.1080/15374416.2013.838771] [PMID]
Combs, M. A., Canu, W. H., Fulks, J. J. B., & Nieman, D. C. (2014). Impact of sluggish cognitive tempo and attention-deficit/hyperactivity disorder symptoms on adults’ quality of life. Applied Research in Quality of Life, 9(4), 981-995. [DOI:10.1007/s11482-013-9281-3]
Das, D., Cherbuin, N., Butterworth, P., Anstey, K. J., & Easteal, S. (2012). A population-based study of attention deficit/hyperactivity disorder symptoms and associated impairment in middle-aged adults. PloS One, 7(2), e31500. [DOI:10.1371/journal.pone.0031500] [PMID]
Flannery, A. J., Becker, S. P., & Luebbe, A. M. (2016). Does emotion dysregulation mediate the association between sluggish cognitive tempo and college students’ social impairment? Journal of Attention Disorders, 20(9), 802-812. [DOI:10.1177/1087054714527794] [PMID]
Flannery, A. J., Luebbe, A. M., & Becker, S. P. (2017). Sluggish cognitive tempo is associated with poorer study skills, more executive functioning deficits, and greater impairment in college students. Journal of Clinical Psychology, 73(9), 1091-1113. [DOI:10.1002/jclp.22406] [PMID]
Ghazaei, M., Hamid, N., & Mehrabizadeh Honarmand, M. (2012). [The effect of cognitive-behavioural therapy on attention deficit hyperactivity disorder and its symptoms in university students (Persian)]. Journal of Psychological Achievements, 19(2), 63-80. [Link]
Godoy, V. P., Serpa, A. L. O., Fonseca, R. P., & Malloy-Diniz, L. F. (2023). Executive functions contribute to the differences between ADHD and Sluggish Cognitive Tempo (SCT) in adults. Journal of Attention Disorders, 27(6), 623-634. [DOI:10.1177/10870547231153948] [PMID]
Kamradt, J. M., Momany, A. M., & Nikolas, M. A. (2018). Sluggish cognitive tempo symptoms contribute to heterogeneity in adult attention-deficit hyperactivity disorder. Journal of Psychopathology and Behavioral Assessment, 40(2), 206-223. [DOI:10.1007/s10862-017-9631-9] [PMID]
Lensing, M. B., Zeiner, P., Sandvik, L., & Opjordsmoen, S. (2013). Adults with ADHD: Use and misuse of stimulant medication as reported by patients and their primary care physicians. Attention Deficit and Hyperactivity Disorders, 5(4), 369-376. [DOI:10.1007/s12402-013-0116-8] [PMID]
Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335-343. [DOI:10.1016/0005-7967(94)00075-U] [PMID]
Marshall, S. A., Evans, S. W., Eiraldi, R. B., Becker, S. P., & Power, T. J. (2014). Social and academic impairment in youth with ADHD, predominately inattentive type and sluggish cognitive tempo. Journal of Abnormal Child Psychology, 42(1), 77-90. [DOI:10.1007/s10802-013-9758-4] [PMID]
Mayes, S. D., Becker, S. P., Calhoun, S. L., & Waschbusch, D. A. (2023). Comparison of the cognitive disengagement and hypoactivity components of sluggish cognitive tempo in autism, ADHD, and population-based samples of children. Research on Child and Adolescent Psychopathology, 51(1), 47-54. [DOI:10.1007/s10802-022-00969-3] [PMID]
McHorney, C. A., Ware, J. E., Jr, Lu, J. F., & Sherbourne, C. D. (1994). The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care, 32(1), 40–66.[DOI:10.1097/00005650-199401000-00004] [PMID]
Montazeri A, Goshtasebi A, Vahdaninia M.S. [The short form health survey (SF-36): Translation and validation study of the Iranian version (Persian)]. Payesh 2006; 5 (1):49-56. [Link]
Smith, Z. R., Eadeh, H. M., Breaux, R. P., & Langberg, J. M. (2019). Sleepy, sluggish, worried, or down? The distinction between self-reported sluggish cognitive tempo, daytime sleepiness, and internalizing symptoms in youth with attention-deficit/hyperactivity disorder. Psychological Assessment, 31(3), 365–375. [DOI:10.1037/pas0000671] [PMID]
Ware, J. E., Jr, & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30(6), 473–483. [DOI:10.1097/00005650-199206000-00002] [PMID]
Wood, W. L. M., Potts, H. E., Lewandowski, L. J., & Lovett, B. J. (2017). Sluggish cognitive tempo and speed of performance. Journal of Attention Disorders, 21(8), 684-690. [DOI:10.1177/1087054716666322] [PMID]
Wood, W. L., Lewandowski, L. J., Lovett, B. J., & Antshel, K. (2020). Sluggish cognitive tempo and impairment: The role of lifestyle factors. Psychology in the Schools, 57(7), 1171-1188. [DOI:10.1002/pits.22378]
Zlomke, K. R. (2009). Psychometric properties of internet administered versions of Penn state worry questionnaire (PSWQ) and depression, anxiety, and stress scale (DASS). Computers in Human Behavior, 25(4), 841-843. [DOI:10.1016/j.chb.2008.06.003]
Sluggish cognitive tempo (SCT) in children and adults is characterized by various problems, such as mental fogginess, confusion, sluggishness, drowsiness, confusion, hypoactivity, staring, and daydreaming (Flannery et al., 2014). Barkley (2012) reported high SCT symptoms in 5.8% of all adults. Recent studies regard SCT as an essential psychological and psychiatric construct affecting different aspects of a person’s life (Barkley, 2013; Barkley, 2014). It was previously thought that SCT was associated with attention deficit disorder (ADD) (Marshall et al., 2014); however, it has recently been considered a separate condition that is usually associated with ADD or attention deficit disorder with hyperactivity disorder (ADHD). Barkley (2013) suggested that SCT is present in people without ADHD; accordingly, 40% to 50% of people who had significant symp-toms of SCT lacked apparent symptoms of ADHD (Barkley, 2013).
Subjective belief in mental and physical health and well-being is known as the quality of life (QoL) (CDC, 2009). Combs et al. (2014) concluded that SCT is correlated with poor physical, mental, and total QoL. According to Barkley (2012), SCT can affect different domains of life even more than ADHD (e.g. social life, job, and self-care). Becker & Langberg (2013) found that SCT symptoms have a negative social impact as well as low academic achievement in college students, even after controlling for demographic variables and ADHD symptoms. SCT is correlated with self-reported problems in executive functioning (self-control, problem-solving, self-organization, time management, self-regulation of emotion, and self-motivation in daily life) (Barkley, 2012; Wood et al., 2017)
In addition, some studies have shown a strong correlation between SCT and disorders such as depression and anxiety (Becker et al., 2014; Kamradt et al., 2018). Symptoms of depression and anxiety are frequently comorbid with SCT (Barkley, 2013). Function impairment in several domains, including health, job performance, and social relationships, is a common occurrence in depressive and anxiety disorders (Brenes, 2007); therefore, Bernes (2007) concluded that anxiety and depression symptoms harm all dimensions of QoL. Also, previous research has shown that QoL in people with ADHD is low (Able et al., 2007; Das et al., 2012; Lensing et al., 2013). Considering the close relationship between disorders such as depression and anxiety and core symptoms of ADHD (hyperactivity, inattention, and impulsivity) with SCT and the impact of all these disorders on QoL, the research question is to what extent SCT as a separate construct is associated with QoL (Becker & Langberg, 2013).
Despite many studies on the consequences of SCT, there has been no observed research on the effect of SCT on QoL after controlling for ADHD symptoms (hyperactivity, inattention, and impulsivity), anxiety, and depression in the Iranian population. Furthermore, published research in Iran about the consequences of SCT on QoL in adults is scarce; therefore, this study investigates whether SCT affects QoL and whether this effect will persist after controlling for ADHD symptoms, depression, and anxiety in Iranian college students. The research hypotheses are as follows:
1. SCT is negatively correlated to the QoL;
2. SCT is still negatively correlated to the QoL if ADHD symptoms are controlled;
3. SCT is still negatively correlated to the QoL if depression symptoms are controlled;
4. SCT is still negatively correlated to the QoL if anxiety symptoms are controlled;
5. SCT is still negatively correlated to the QoL if ADHD, depression, and anxiety symptoms are controlled.
Materials and Methods
Study participants and procedures
This descriptive correlational study was conducted on college students in Mashhad City, Iran. The participants were 279 students selected by the convenience sampling method from September 2020 to February 2021. In regression correlation research, considering at least 15 and 50 subjects for each predictive variable can be a reasonable estimate (Beshlideh, 2012). Therefore, considering four predictive variables in the present study, the number of 279 participants is sufficient. Sajjad University and Shandiz Institute of Higher Education were selected for sampling. During the COVID-19 pandemic, classes in Iranian colleges were not held face-to-face; therefore, students and teachers used to form groups in online applications, such as Telegram and WhatsApp, to communicate and transfer information. An electronic link to the questionnaires was created with the Porsline site to conduct the research. The electronic link to the questionnaires was sent to these college groups on Telegram and WhatsApp. In the electronic link, the aim of the study was briefly explained, and students were asked to answer the questions. By viewing the questionnaire link in their virtual study group, the students responded to its questions if they agreed. In addition, the age range of 18 to 40 years was considered the criteria for entering this study. If the students wanted to know the evaluation results, they could enter their e-mail address at the end of the questionnaire. In the middle of the questionnaire, a question measured the attention and correctness of the participants’ answers. The question was as follows: “I have traveled to space in the last year.” Participants were excluded from the sample if they answered this question positively. A total of 16 participants were excluded because of positive answers to this question. In addition, the report of the diagnosis of a psychiatric disorder or the use of psychiatric drugs was the exclusion criteria. Meanwhile, 5 participants were excluded because of the use of psychiatric drugs. The final sample was 279 participants.
Study instruments
Barkley adult ADHD rating scale-iV (BAARS-IV)
The Barkley adult ADHD rating scale-IV (BAARS-IV) (Barkley, 2011) has 27 items that include the diagnostic and statistical manual of mental disorders diagnostic criteria for ADHD. The participants answered each item based on a 4-point scale (1=not at all, 2=sometimes, 3=often, and 4=very often). Nine items measure attention deficit, three items for impulsivity, six for hyperactivity, and nine for SCT. Inattention, hyperactivity, and impulsivity symptoms were used to calculate ADHD symptom scores. Nine SCT symptoms were used to calculate the SCT score. The total score of ADHD symptoms can be between 18 and 72, and the total score of SCT symptoms can be between 9 and 36. Subjects who score above 54 on the 18 ADHD questions are individuals who have symptoms of ADHD. The onset of symptoms before the age of 12 years and functional impairment in at least two settings (school, home, work, and social relationships) are needed for diagnosis (Barkley, 2012). Barkley, (2011) reported high internal consistency for inattention (α=0.90), hyperactive-impulsive (α=0.80), and SCT (α=0.90). The correlation of the score of this scale with the scores of a collateral reporter is in the range of 0.59 to 0.76; hence, its validity is appropriate (Barkley, 2011). This questionnaire has been translated into Persian. In the Iranian population, convergent validity was appropriate, and its reliability using internal consistency was 0.71 for inattention, 0.72 for hyperactive symptoms, 0.73 for impulsive symptoms, and 0.77 for SCT (Ghazaei et al., 2012). In the current study, the Cronbach α for ADHD and SCT was 0.74 and 0.79, respectively.
Depression, anxiety, and stress scale
The depression, anxiety, and stress scale (DASS) (Lovibond & Lovibond, 1995) is a self-reported instrument. DASS measures negative emotions of stress, depression, and anxiety. A total of 14 questions are assigned for each subscale. The questions are scored based on a 4-point scale from 0 (does not apply to me at all) to 3 (extremely applies to me). The sum of scores in each subscale can be from 0 to 42. We used the subscales of anxiety and depression. The Cronbach α for the depression, anxiety, and stress subscales has been reported in the range of 0.89 to 0.97 (Zlomke, 2009). The correlation between the DASS and other scales of depression and anxiety is appropriate (Lovibond & Lovibond, 1995). This questionnaire has been translated into Persian. In an Iranian study, the convergence validity of the DASS was confirmed by a high correlation with the Beck depression inventory and Beck anxiety inventory, and its reliability using the Cronbach α coefficient was 0.90 for anxiety and 0.93 for depression (Asghari et al., 2008). In the current study, the Cronbach α for depression and anxiety was 0.83 and 0.8, respectively.
36-item short-form health survey
The 36-item short-form health survey (SF-36) measures QoL and functional deficits resulting from an illness (Ware & Sherbourne, 1992). SF-36 includes two dimensions as follows: the physical dimension with 21 questions and the mental dimension with 15 questions. The SF-36 mental part assesses the QoL during the last 4 weeks in the following four subscales: limitations in daily activities because of emotional problems, vitality (energy and fatigue), limitations in daily activities because of social problems, and mental health. In addition, the SF-36 physical part assesses the QoL during the last 4 weeks in four subscales, namely physical functioning, physical role, pain, and general health. Each question is scored from 0 to 100, and the total score in each subscale is obtained from the average sum of the scores of the questions related to that subscale. Therefore, the total score and subscales can vary from 0 to 100. Higher scores indicate the perceived or functioning QoL. The internal consistency for the subscales ranged from 0.74 to 0.86 based on the Cronbach α method. The SF-36 is widely used and is considered a valid and reliable instrument (McHorney et al., 1994). This questionnaire has been used in more than fifty countries worldwide and has been translated into Persian. Many studies have confirmed its validity and reliability (Montazeri et al., 2006). In the current study, the Cronbach α for mental, physical, and total QoL was 0.72, 0.79, and 0.76, respectively.
Data analysis
The SPSS software, version 24, was used for data analysis. Descriptive statistics were used to obtain the variables Means±SD. Pearson’s correlation coefficient was used to calculate the correlation between the variables. Finally, hierarchical regression analysis was used to examine the hypotheses. It should be noted that all statistical tests were calculated at a confidence level of 95% (P<0.05).
Results
Table 1 presents the participants’ demographic characteristics. The average age of the participants was 31.29 years. Meanwhile, 40.1% of the participants were male, and 59.9% were female.
The result of multivariate analysis of variance and then of analysis of variance showed that SCT, ADHD, depression, and anxiety did not differ significantly between men and women; however, the QoL was considerably higher in women compared to men. Furthermore, the result of the multivariate variance analysis showed that SCT, ADHD, depression, anxiety, and QoL did not differ significantly between various levels of education. Also, 6 participants were excluded due to scores of three standard deviations above the mean in SCT and ADHD. Table 2 shows descriptive statistics of the research variables.
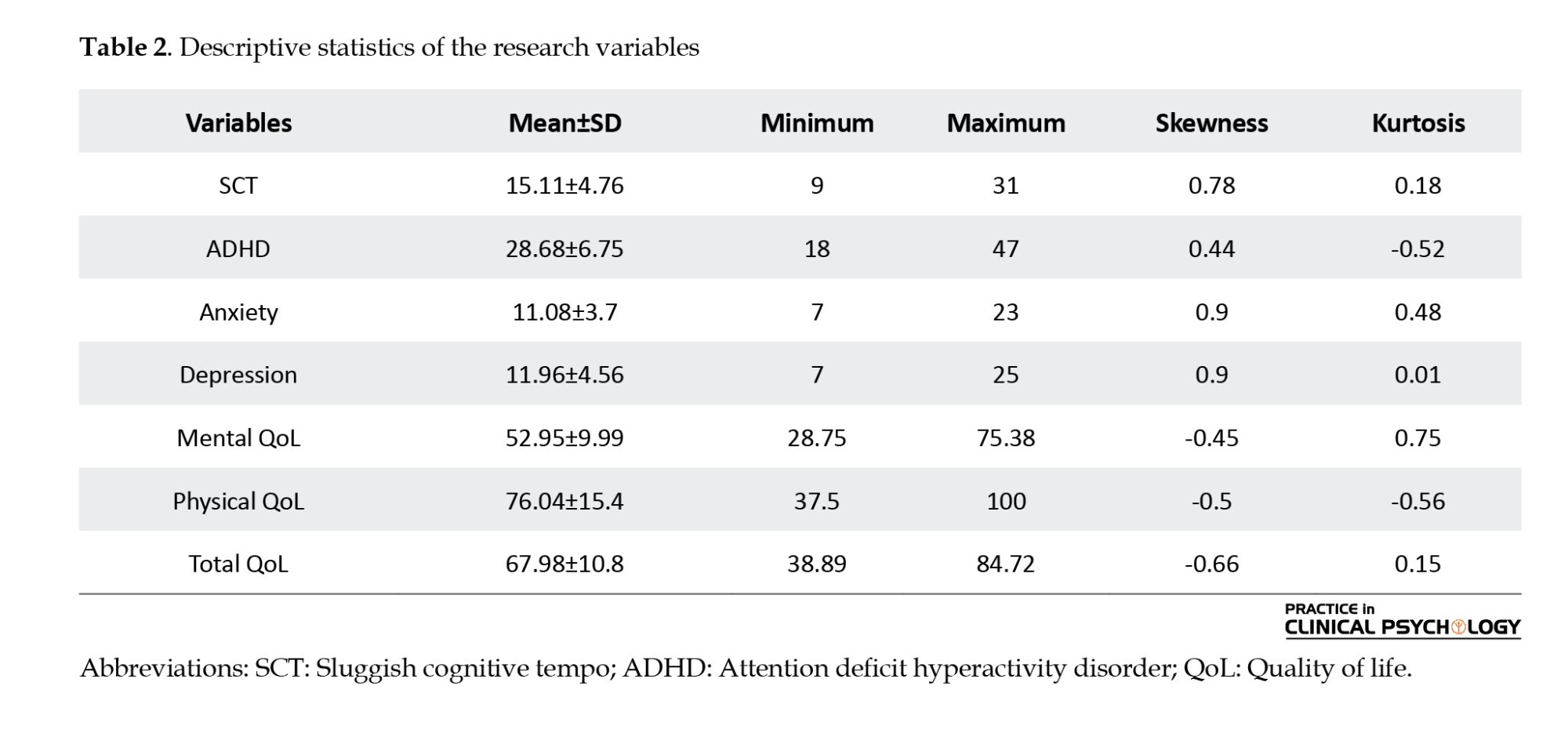
According to Table 2, the skewness and kurtosis were between -1 and +1; therefore, the variables are normal and suitable for parametric tests. We conducted a correlation analysis to examine the association among all the variables, and the correlation matrix is shown in Table 3.
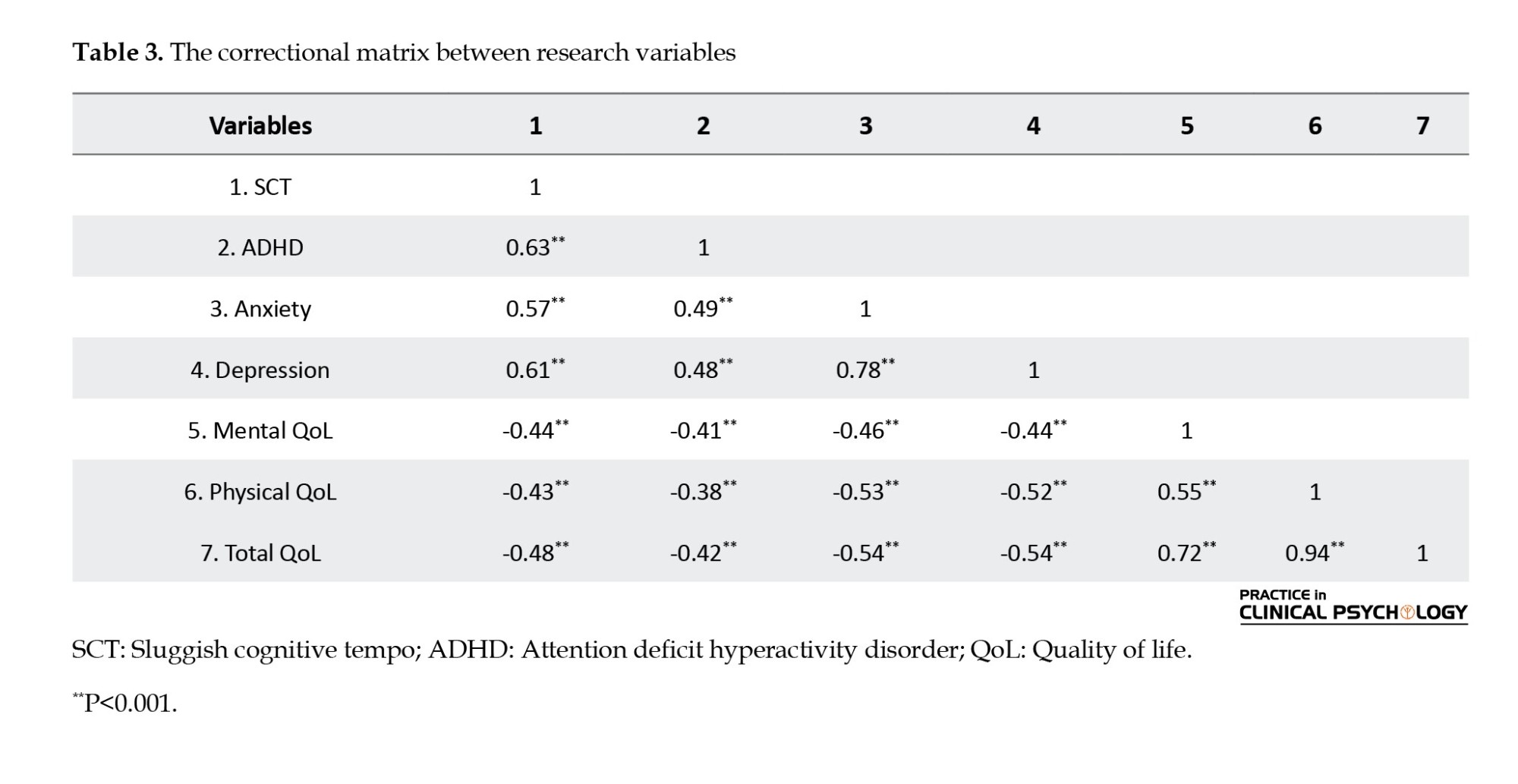
According to Table 3, SCT was positively related to anxiety, depression, and ADHD (P<0.001). QoL was negatively associated with SCT, anxiety, depression, and ADHD (P<0.001).
Hierarchical regression analysis was used to investigate the research hypotheses and answer whether SCT is still related to the QoL if ADHD, depression, and anxiety are controlled. In this method, we first enter the control variables, i.e. depression, anxiety, and ADHD symptoms, into the regression equation and then add the SCT. Table 4 shows the results of hierarchical regression for predicting QoL based on SCT after controlling for the ADHD Symptoms variable.
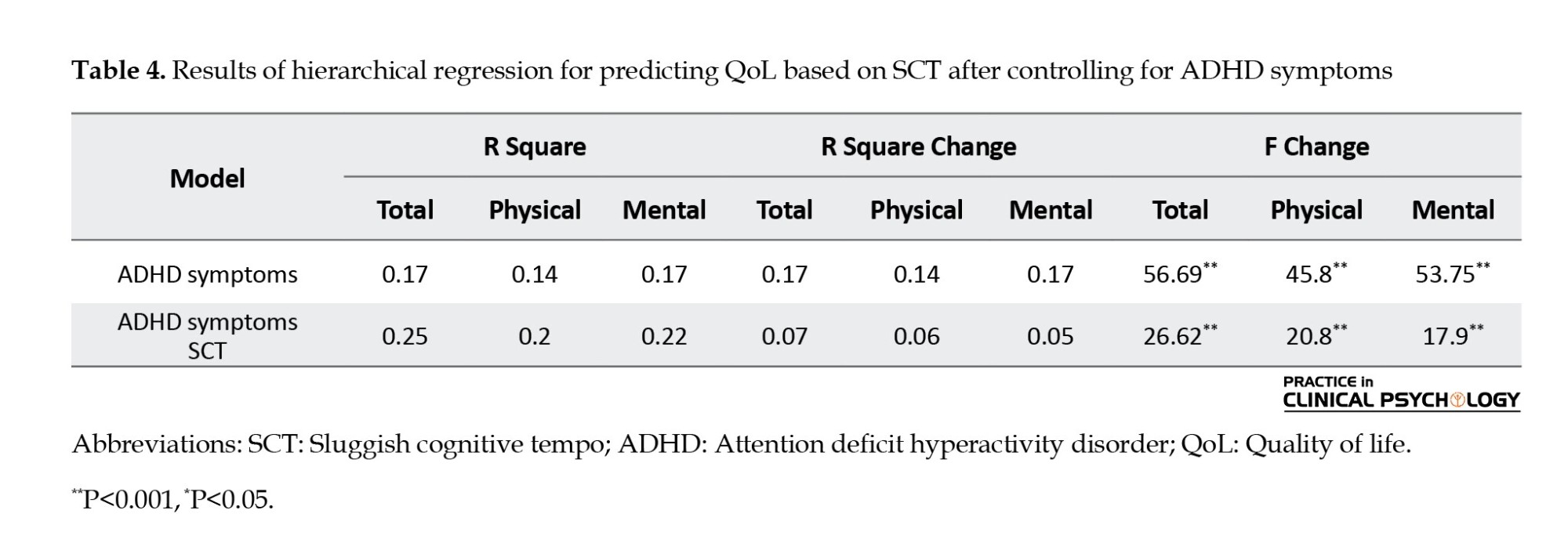
Table 4 shows that ADHD symptoms account for 17% of the variance of the total QoL, 14% of the physical dimension, and 17% of the mental dimension. The SCT and ADHD variables account for 25% of the variance of the total QoL, 20% of the variance of the physical dimension, and 22% of the variance of the mental dimension. R Square change was 7% for total QoL (F change=26.62, P<0.0001), 6% for the physical dimension of QoL (F change=20.8, P<0.0001), and 5% for the mental dimension of QoL (F change=17.9, P<0.0001), after SCT entry, which is significant. In other words, SCT, after controlling ADHD, can still account for a significant percentage of the total QoL and mental and physical dimensions of QoL. Table 5 shows the results of hierarchical regression for predicting QoL based on SCT after controlling for the depression variable.
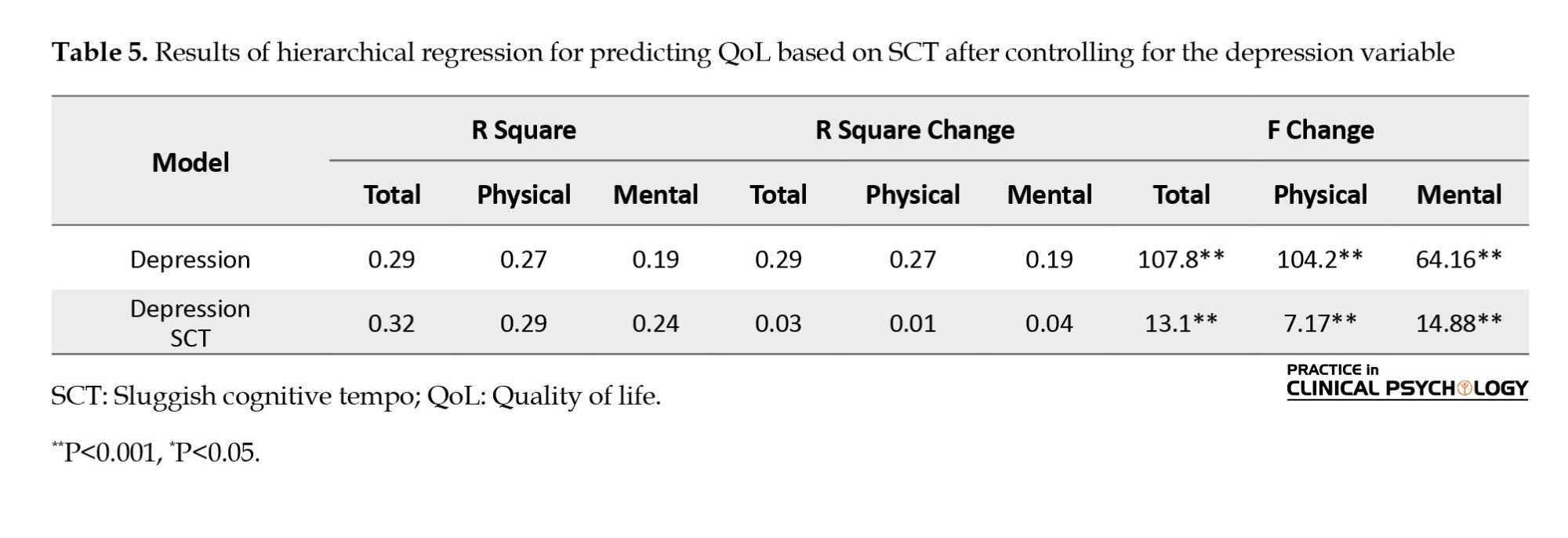
Table 5 shows that depression accounts for 29% of the variance of the total QoL, 27% of the physical dimension, and 19% of the variance of the mental dimension. The SCT and depression variables account for 32% of the variance of the total QoL, 29% of the variance of the physical dimension, and 24% of the variance of the mental dimension. R Square change was 3% for total QoL (F change=13.1, P<0.0001), 1% for the physical dimension of QoL (F change=7.1, P<0.0001), and 4% for the mental dimension of QoL (F change=14.88, P<0.0001), after SCT entry, which is significant. In other words, SCT, after controlling depression, can still account for a significant percentage of the total QoL, physical and mental dimensions of QoL. Table 6 shows the results of hierarchical regression for predicting QoL based on SCT after controlling for the anxiety variable.
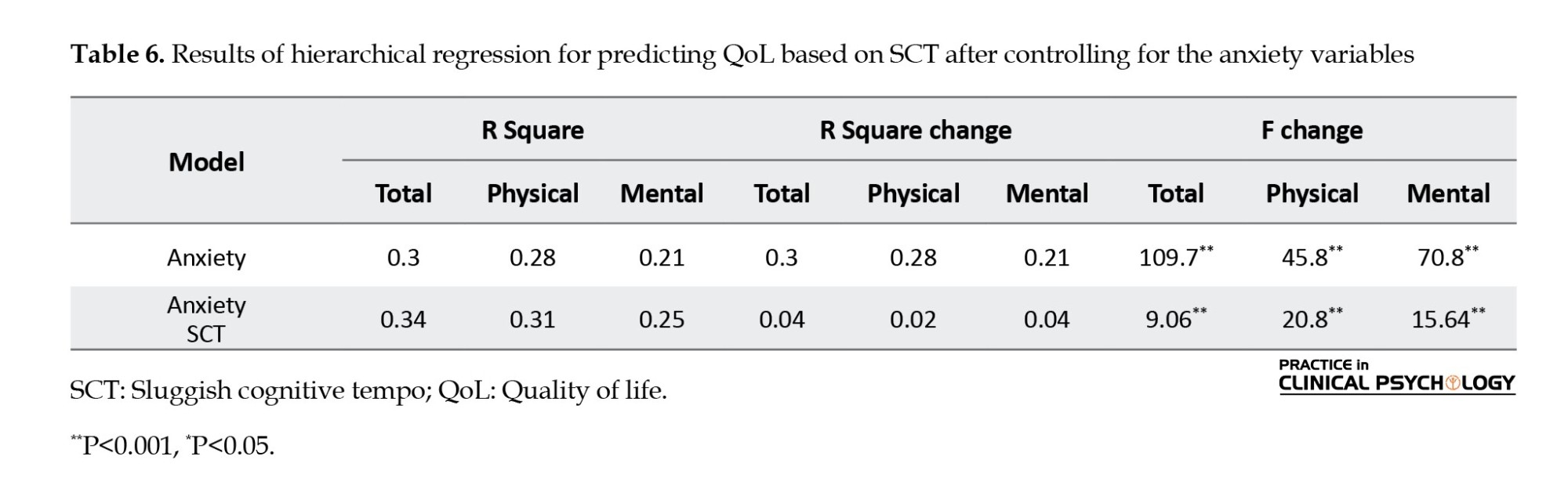
Table 6 shows that anxiety accounts for 30% of the variance of the total QoL, 28% of the physical dimension, and 21% of the variance of the mental dimension. The SCT and anxiety variables account for 34% of the variance of the total QoL, 31% of the variance of the physical dimension, and 25% of the variance of the mental dimension. R Square change was 4% for total QoL (F change=9.06, P<0.0001), 2% for the physical dimension of QoL (F change=20.8, P<0.0001), and 4% for the mental dimension of QoL (F change=15.64, P<0.0001), after SCT entry, which is significant. In other words, SCT, after controlling anxiety, can still account for a significant percentage of the total QoL and physical and mental dimensions of QoL. Table 7 shows the results of hierarchical regression for predicting QoL based on SCT after controlling for the depression, anxiety & ADHD symptoms variable.
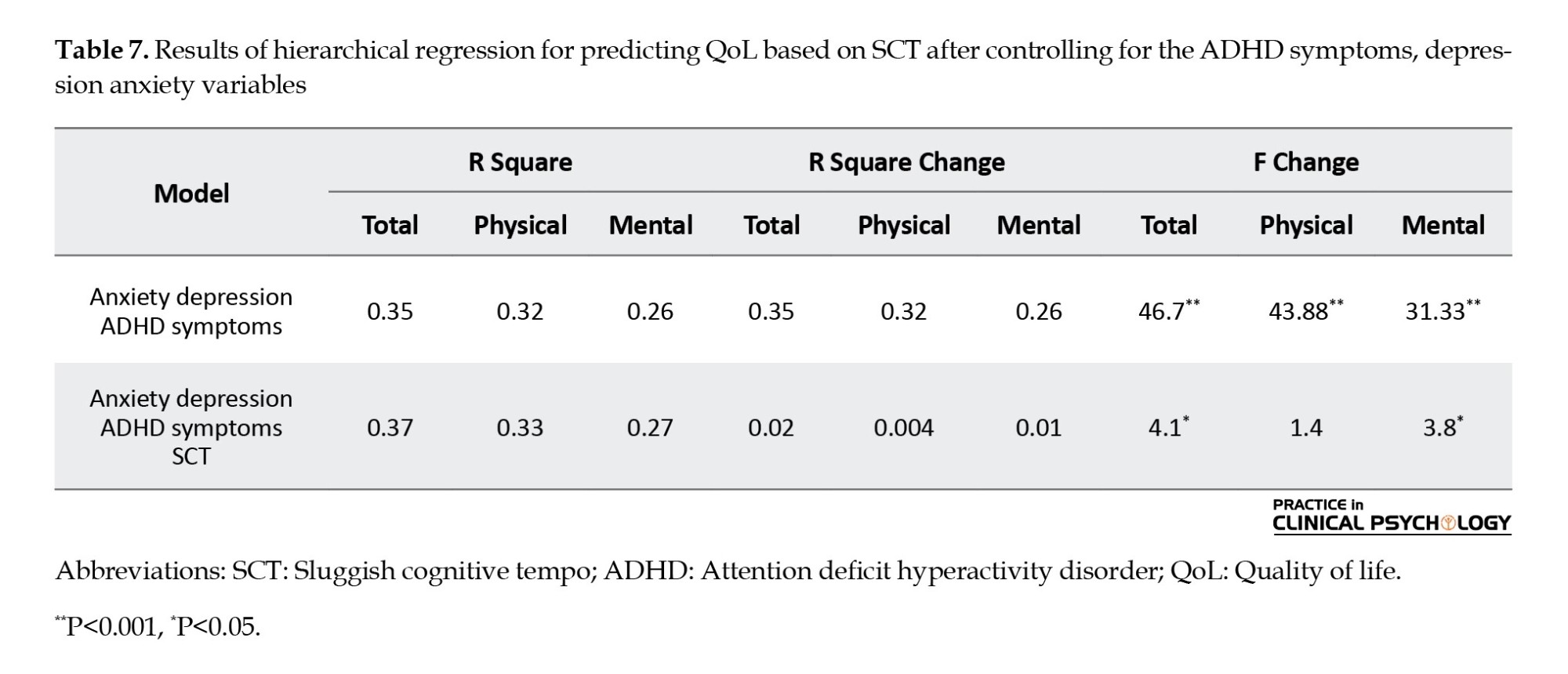
The results from Table 7 showed that ADHD symptoms, depression, and anxiety account for 35% of the variance of the total QoL, 32% of the variance of the physical dimension, and 26% of the variance of the mental dimension. The SCT, ADHD symptoms, depression, and anxiety variables account for 37% of the variance of the total QoL, 33% of the variance of the physical dimension, and 27% of the variance of the mental dimension. After the SCT entry, R square change was 2% for total QoL (F change=4.1, P=0.031), 0.4% for the physical dimension of QoL (F change=1.4, P=0.09), and 1% for the mental dimension of QoL (F change=3.8, P=0.02). In other words, SCT, after controlling ADHD, depression, and anxiety, can still account for a significant percentage of the total QoL and mental dimensions of QoL. However, SCT, after controlling depression, cannot make a meaningful change in the physical dimension of QoL.
Discussion
This study aimed to investigate whether SCT affects the QoL and whether this effect will persist after controlling for depression, ADHD, and anxiety symptoms. The results showed depression, anxiety, ADHD, and SCT symptoms are correlated to poor QoL in Mashhad college students. Hierarchical regression analysis was used to answer whether SCT can still be correlated with the lower QoL after controlling depression, anxiety, and ADHD. The results of hierarchical regression analysis showed that SCT is negatively correlated with the total QoL and mental dimensions of QoL after controlling anxiety, depression, and ADHD symptoms both individually and together. However, SCT, after controlling three variables of depression, anxiety, and ADHD, could not account for a significant variance in the physical dimension of QoL. However, after controlling the variables individually, SCT can still create a significant variance in this dimension.
Limited studies have addressed the relationship between SCT and QoL, and current research showed that SCT is negatively related to lower physical, mental, and total QoL. SCT is multidimensional and includes cognitive components (e.g. fantasy and confusion) and behavioral components (such as slow motion and slowness). Therefore, SCT can reduce the QoL in the physical dimension by reducing energy levels, reducing the ability to work and perform daily activities, and reducing sleep quality. In addition, impairment in occupational and academic performance is observed due to SCT symptoms (Barkley, 2012). Given the impact of SCT on these areas, SCT also reduces the mental dimension of QoL and creates negative emotions (Barkley, 2014; Combs et al., 2014). Furthermore, SCT reduces the mental dimension of QoL by creating social problems (Becker & Lungberg, 2013; Flannery et al., 2016).
Furthermore, current research showed that SCT is negatively correlated with the total QoL and mental dimensions of QoL after controlling ADHD symptoms. A study similar to the current study reported that even after controlling for ADHD symptoms and internalizing disorder, SCT was correlated with impaired social functioning and adjustment problems in adults (Flannery et al., 2017). Another study showed that after statistically controlling for symptoms of ADHD, oppositional defiant disorder, generalized anxiety disorder, intelligence, and major depressive disorder, SCT was still associated with avoidance and impaired social functioning (Burns et al., 2013). Thus, although SCT symptoms are related closely to The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition in attention, the current study suggests that SCT symptoms may represent a separable symptom dimension that is distinct from the inattentive and combined types of ADHD (Mayes et al., 2022). Some studies have shown that SCT can cause different problems than ADHD. The inattentive type of ADHD is more correlated to time management. In contrast, the combined type of ADHD is related to self-control, and SCT is correlated with self-organization and problem-solving (Gody et al., 2023). Gody et al., (2023) showed that SCT symptoms are more associated with executive dysfunctions than the combined type of ADHD. Also, the daydreamy-sleepy feature of SCT, one of the most critical differences between SCT and ADHD, can reduce the QoL because the person lacks the necessary energy to perform daily and social activities (Barkley, 2012). Another study found that five SCT symptoms (losing the train of thought, being easily confused, seeming drowsy, slow thinking, and slow-moving) show convergent and discriminant validity (Burns et al., 2013).
The current study showed that SCT is negatively associated with the total QoL and mental dimensions of QoL after controlling anxiety and depression. Combs et al. (2014) showed that even when demographic variables, anxiety, and mood disorder are controlled, SCT symptoms play an essential role in the QoL of adults. Also, other studies concluded that SCT is distinct from depression and anxiety (Becker et al., 2014; Burns et al., 2013). Smith et al. (2019) also found that despite the strong correlation of SCT with depression and anxiety, SCT remains distinct.
Finally, the current study showed that SCT, after controlling three variables of depression, anxiety, and ADHD, could not account for a significant variance in the physical dimension of QoL. Wood et al. (2020) reported that SCT symptoms do not have a significant relationship with function impairment after controlling for psychological disorders (depression, anxiety, and ADHD) and lifestyle variables (substance abuse, sleep problems). The questionnaire they used to assess performance measured mostly physical dimensions, such as vehicle ability and accident history. They concluded SCT symptoms can represent a lifestyle that does not cause severe problems for college students. These students had accepted SCT as a personality trait and had found ways to adapt despite having these symptoms (Wood et al., 2020).
Conclusion
SCT is associated with low QoL among Iranian college students, and this relationship remains present after controlling for depression, anxiety, and ADHD. In addition, the results of this research emphasize the importance of considering QoL in prospective research and SCT intervention.
Study limitations
The current study had several limitations. First, the correlational nature of the results limits inferences on causality, and longitudinal studies on SCT and its impact on QoL are needed. Our data was collected from Mashhad college students, and we should be careful in generalizing the results. The present study used self-report scales, which may affect the results. In addition, the study relied on a non-clinical community sample, using continuous ADHD, depression, and anxiety traits as predictors instead of actual ADHD, depression, and anxiety diagnoses. In addition, due to the spread of the COVID-19 virus, it was difficult to reach students in person, and for this reason, electronic questionnaires were used, which can affect the validity of the results. Results from this study point toward the need for added research with larger samples that can examine the longitudinal consequences of SCT on QoL. The relationship between SCT and different performance domains should be considered in future research.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The purpose of the study and the steps of the research implementation were informed to the participants. They were assured about the confidentiality of the information and the possibility of leaving the study at any moment. In addition, they were informed by e-mail if they wanted to know the evaluation results.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors would like to thank all participants in this study.
Reference
Able, S. L., Johnston, J. A., Adler, L. A., & Swindle, R. W. (2007).Functional and psychosocial impairment in adults with undiagnosed ADHD. Psychological Medicine, 37(1), 97-107. [DOI:10.1017/S0033291706008713] [PMID]
Asghari Moghadam, M. A., Saed, F., Dibaj Nia, P., & Zanganeh, J. (2008). [A preliminary study on the validity and reliability of the Depression, anxiety and stress in nonclinical samples (DASS) (Persian)]. Scientific-Research Journal of Shahed University (Daneshvar), 15(31), 23-38. [Link]
Barkley, R. A. (2011). Barkley Adult ADHD Rating Scale-IV (BAARS-IV). New York City: The Guilford Press. [Link]
Barkley, R. A. (2012). Distinguishing sluggish cognitive tempo from attention-deficit/hyperactivity disorder in adults. Journal of Abnormal Psychology, 121(4), 978-990. [DOI:10.1037/a0023961] [PMID]
Barkley, R. A. (2013). Distinguishing sluggish cognitive tempo from ADHD in children and adolescents: executive functioning, impairment, and comorbidity. Journal of Clinical Child & Adolescent Psychology, 42(2), 161-173. [DOI:10.1080/15374416.2012.734259] [PMID]
Barkley, R. A. (2014). Sluggish cognitive tempo (concentration deficit disorder?): Current status, future directions, and a plea to change the name. Journal of Abnormal Child Psychology, 42(1), 117-125. [DOI:10.1007/s10802-013-9824-y] [PMID]
Barkley, R. A. (2014). Concentration deficit disorder (sluggish cognitive tempo). Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment, 81-115. Guilford Publications. [Link]
Becker, S. P. (2014). Sluggish cognitive tempo and peer functioning in school-aged children: A six-month longitudinal study. Psychiatry Research, 217(1-2), 72-78. [DOI:10.1016/j.psychres.2014.02.007] [PMID]
Becker, S. P., & Langberg, J. M. (2013). Sluggish cognitive tempo among young adolescents with ADHD: Relations to mental health, academic, and social functioning. Journal of Attention Disorders, 17(8), 681-689. [DOI:10.1177/1087054711435411] [PMID]
Becker, S. P., Langberg, J. M., Luebbe, A. M., Dvorsky, M. R., & Flannery, A. J. (2014). Sluggish cognitive tempo is associated with academic functioning and internalizing symptoms in college students with and without attention‐deficit/hyperactivity disorder. Journal of Clinical Psychology, 70(4), 388-403. [DOI:10.1002/jclp.22046] [PMID]
Beshlideh, K. (2012). [Research methods and statistical analysis of research using SPSS and AMOS (Persian). Ahvaz: shahid Chamran University Publications; 2012. [Link]
Brenes, G. A. (2007). Anxiety, depression, and quality of life in primary care patients. Primary Care Companion to the Journal of Clinical Psychiatry, 9(6), 437–443. [DOI:10.4088/PCC.v09n0606] [PMID]
Burns, G. L., Servera, M., Bernad, M.delM., Carrillo, J. M., & Cardo, E. (2013). Distinctions between sluggish cognitive tempo, ADHD-IN, and depression symptom dimensions in Spanish first-grade children. Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 42(6), 796–808. [DOI:10.1080/15374416.2013.838771] [PMID]
Combs, M. A., Canu, W. H., Fulks, J. J. B., & Nieman, D. C. (2014). Impact of sluggish cognitive tempo and attention-deficit/hyperactivity disorder symptoms on adults’ quality of life. Applied Research in Quality of Life, 9(4), 981-995. [DOI:10.1007/s11482-013-9281-3]
Das, D., Cherbuin, N., Butterworth, P., Anstey, K. J., & Easteal, S. (2012). A population-based study of attention deficit/hyperactivity disorder symptoms and associated impairment in middle-aged adults. PloS One, 7(2), e31500. [DOI:10.1371/journal.pone.0031500] [PMID]
Flannery, A. J., Becker, S. P., & Luebbe, A. M. (2016). Does emotion dysregulation mediate the association between sluggish cognitive tempo and college students’ social impairment? Journal of Attention Disorders, 20(9), 802-812. [DOI:10.1177/1087054714527794] [PMID]
Flannery, A. J., Luebbe, A. M., & Becker, S. P. (2017). Sluggish cognitive tempo is associated with poorer study skills, more executive functioning deficits, and greater impairment in college students. Journal of Clinical Psychology, 73(9), 1091-1113. [DOI:10.1002/jclp.22406] [PMID]
Ghazaei, M., Hamid, N., & Mehrabizadeh Honarmand, M. (2012). [The effect of cognitive-behavioural therapy on attention deficit hyperactivity disorder and its symptoms in university students (Persian)]. Journal of Psychological Achievements, 19(2), 63-80. [Link]
Godoy, V. P., Serpa, A. L. O., Fonseca, R. P., & Malloy-Diniz, L. F. (2023). Executive functions contribute to the differences between ADHD and Sluggish Cognitive Tempo (SCT) in adults. Journal of Attention Disorders, 27(6), 623-634. [DOI:10.1177/10870547231153948] [PMID]
Kamradt, J. M., Momany, A. M., & Nikolas, M. A. (2018). Sluggish cognitive tempo symptoms contribute to heterogeneity in adult attention-deficit hyperactivity disorder. Journal of Psychopathology and Behavioral Assessment, 40(2), 206-223. [DOI:10.1007/s10862-017-9631-9] [PMID]
Lensing, M. B., Zeiner, P., Sandvik, L., & Opjordsmoen, S. (2013). Adults with ADHD: Use and misuse of stimulant medication as reported by patients and their primary care physicians. Attention Deficit and Hyperactivity Disorders, 5(4), 369-376. [DOI:10.1007/s12402-013-0116-8] [PMID]
Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335-343. [DOI:10.1016/0005-7967(94)00075-U] [PMID]
Marshall, S. A., Evans, S. W., Eiraldi, R. B., Becker, S. P., & Power, T. J. (2014). Social and academic impairment in youth with ADHD, predominately inattentive type and sluggish cognitive tempo. Journal of Abnormal Child Psychology, 42(1), 77-90. [DOI:10.1007/s10802-013-9758-4] [PMID]
Mayes, S. D., Becker, S. P., Calhoun, S. L., & Waschbusch, D. A. (2023). Comparison of the cognitive disengagement and hypoactivity components of sluggish cognitive tempo in autism, ADHD, and population-based samples of children. Research on Child and Adolescent Psychopathology, 51(1), 47-54. [DOI:10.1007/s10802-022-00969-3] [PMID]
McHorney, C. A., Ware, J. E., Jr, Lu, J. F., & Sherbourne, C. D. (1994). The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care, 32(1), 40–66.[DOI:10.1097/00005650-199401000-00004] [PMID]
Montazeri A, Goshtasebi A, Vahdaninia M.S. [The short form health survey (SF-36): Translation and validation study of the Iranian version (Persian)]. Payesh 2006; 5 (1):49-56. [Link]
Smith, Z. R., Eadeh, H. M., Breaux, R. P., & Langberg, J. M. (2019). Sleepy, sluggish, worried, or down? The distinction between self-reported sluggish cognitive tempo, daytime sleepiness, and internalizing symptoms in youth with attention-deficit/hyperactivity disorder. Psychological Assessment, 31(3), 365–375. [DOI:10.1037/pas0000671] [PMID]
Ware, J. E., Jr, & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care, 30(6), 473–483. [DOI:10.1097/00005650-199206000-00002] [PMID]
Wood, W. L. M., Potts, H. E., Lewandowski, L. J., & Lovett, B. J. (2017). Sluggish cognitive tempo and speed of performance. Journal of Attention Disorders, 21(8), 684-690. [DOI:10.1177/1087054716666322] [PMID]
Wood, W. L., Lewandowski, L. J., Lovett, B. J., & Antshel, K. (2020). Sluggish cognitive tempo and impairment: The role of lifestyle factors. Psychology in the Schools, 57(7), 1171-1188. [DOI:10.1002/pits.22378]
Zlomke, K. R. (2009). Psychometric properties of internet administered versions of Penn state worry questionnaire (PSWQ) and depression, anxiety, and stress scale (DASS). Computers in Human Behavior, 25(4), 841-843. [DOI:10.1016/j.chb.2008.06.003]
Type of Study: Original Research Article |
Subject:
Psychiatry
Received: 2023/09/4 | Accepted: 2024/01/15 | Published: 2024/04/1
Received: 2023/09/4 | Accepted: 2024/01/15 | Published: 2024/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








