Volume 12, Issue 2 (Spring 2024)
PCP 2024, 12(2): 153-164 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mostafazadeh P, Sotoudehasl N, Ghorbani R. Comparing the Effectiveness of Acceptance and Commitment Therapy and Metacognitive Therapy on Psychological Well-being in Women With Generalized Anxiety Disorder. PCP 2024; 12 (2) :153-164
URL: http://jpcp.uswr.ac.ir/article-1-907-en.html
URL: http://jpcp.uswr.ac.ir/article-1-907-en.html
1- Department of Psychology, Faculty of Humanity, Semnan Branch, Islamic Azad University, Semnan, Iran.
2- Department of Psychology, Faculty of Humanity, Semnan Branch, Islamic Azad University, Semnan, Iran. ,sotodeh1@yahoo.com
3- Social Determinants of Health Research Center, Semnan University of Medical Sciences, Semnan, Iran.
2- Department of Psychology, Faculty of Humanity, Semnan Branch, Islamic Azad University, Semnan, Iran. ,
3- Social Determinants of Health Research Center, Semnan University of Medical Sciences, Semnan, Iran.
Keywords: Acceptance and commitment therapy, Metacognitive therapy, Psychological well-being, Women, Generalized anxiety disorder
Full-Text [PDF 728 kb]
(823 Downloads)
| Abstract (HTML) (2264 Views)
Full-Text: (682 Views)
Introduction
Generalized anxiety disorder (GAD) is a common disorder associated with a chronic course and significantly reduced quality of life (Haseth et al., 2019). This disorder, as outlined in The diagnostic and statistical manual of mental disorders, fifth edition, refers to an excessive and prolonged state of anxiety regarding various events and activities that persists for a minimum of six months and significantly hampers the individual’s ability to function properly. Managing and controlling anxiety is particularly challenging in this disorder (LeardMann et al., 2021; Luo et al., 2019). Anxiety is a fear of uncertainty that a person cannot interpret but experiences unpleasant sensations related to physical stimulation (Wroblewski et al., 2023). Accordingly, the person experiencing this feeling does not know the cause of the anxiety (Li et al., 2020). GAD is a common type of anxiety disorder with a prevalence rate of 5.2% in individuals aged 18–64 years (Chaturvedi et al., 2019). Regardless of likelihood, GAD continuously predicts future irrational or exaggerated negative events (LaFreniere et al., 2020)
Previous research showed each indicator of psychological well-being had strong associations with generalized anxiety (Faraci et al., 2022). In addition, research findings indicated that concern was inversely correlated with psychological well-being (PWB) and tended to be positively linked with symptoms of anxiety, even after accounting for other variables (Iani et al., 2019). The results suggested that fostering a sense of purpose in life and the autonomy dimension of PWB could potentially prevent GAD while strengthening the positive relationship with others dimension of PWB that might contribute to generalized anxiety based on the fear of anxiety. Hence, the dimensions of PWB may be beneficial in a primary prevention setting (Takebayashi et al., 2018). A prior study demonstrated that individuals with GAD who paid less attention to their emotions and moods showed higher levels of PWB, aligning with previous research that found reduced attention to feelings predicted better mental health and positive mood (Iani et al., 2019). Furthermore, it was found that PWB acted as a protective factor in the connection between cognitive vulnerabilities and symptoms of generalized anxiety; thus, anxiety symptoms would not escalate in individuals with high cognitive vulnerability if PWB was high (Takebayashi et al., 2018).
Although researchers have shown that various therapeutic approaches can be effective in the treatment of GAD, the discussion of having empirical support and different types of psychotherapies in the treatment of this disorder have always faced challenges. Acceptance and commitment therapy (ACT) help these individuals develop personal strengths, optimal functioning, and well-being (Mani et al., 2019). A recent study conducted by Hossein Nazari et al (2022) suggests that well-being therapy and ACT have the potential to alleviate death anxiety in older adults. Implementing ACT involves encouraging participants to enhance their dedication to leading healthier and more fulfilling lives. This approach also uses behavioral strategies to cope with negative thoughts and emotions. Consequently, ACT can improve psychological well-being and reduce rumination (Mikaeili, 2022). The outcomes of a prior investigation further support the effectiveness of ACT in diminishing behavioral inhibition and cognitive behavioral avoidance in women afflicted with GAD. Moreover, the use of this cost-effective and straightforward therapeutic approach can serve as a foundation for promoting psychological well-being, managing excitement, and establishing healthy interpersonal relationships (Eqharari et al., 2019; Sharif Ara et al., 2023).
The treatment approach discussed here is a psychological intervention incorporating behavioral and modern evolutionary principles. It employs techniques like mindfulness, acceptance, and commitment to enhance psychological flexibility. The fundamental principles of this approach are as follows: 1) Acknowledging and embracing pain or other unpleasant events and thoughts without attempting to control them; 2) Engaging in actions that align with one’s values and committing to them as meaningful objectives while not disregarding unfamiliar experiences (Montazernia et al., 2021). The integration of verbal and cognitive processes with non-verbal elements contributes to the effectiveness of this treatment. It involves exercises that expose individuals to their fears, linguistic metaphors, and mindfulness practices (Abdollahi et al., 2020). ACT, which is a form of a mindfulness intervention, employs metaphors and proverbs to assist clients in enhancing their lives through increased awareness, acceptance, and present-moment focus instead of engaging in internal conflicts and avoiding internal experiences, such as thoughts, memories, and emotions (Azkhosh et al., 2016).
There have been various studies indicating that exposure techniques lead to significant reductions in GAD symptoms (Weisman & Rodebaugh, 2018). The existing evidence suggests that metacognitive therapy (MCT) is effective in treating anxiety and related disorders (McEvoy, 2019; Normann & Morina, 2018). As an alternative to CBT, MCT specifically focuses on modifying cognitive processes rather than the content of thoughts (Wells, 1995). The foundation of MCT lies in the self-regulatory executive function (S-REF) model (Wells & Matthews, 1996), which suggests that psychological disorders arise from a common set of processes referred to as the cognitive attentional syndrome (CAS). CAS entails persistent negative thinking patterns (rumination and worry), inflexible attention and threat monitoring, and maladaptive behavioral strategies that perpetuate negative thought patterns (Strand et al., 2023). According to the metacognitive model of GAD, individuals’ thoughts and beliefs about worry (known as metacognitive beliefs) play a significant role in developing and maintaining the disorder (Haseth et al., 2019).
From a metacognitive perspective, meta-worry can result in avoidance behaviors, such as situational avoidance, seeking reassurance, distraction, and efforts to control anxious thoughts. When these attempts fail, it further reinforces the individual’s belief in the uncontrollability of worry (Köcher et al., 2021). A recent systematic review and meta-analysis conducted by Normann & Morina, 2018 focused on MCT for anxiety and depression. Their findings significantly improved the pre- to post-treatment effect size when comparing MCT to waitlist controls. Previous research has also explored the effectiveness of group MCT for individuals with GAD. The results demonstrated large effect sizes in the reduction of anxiety, depression, and comorbid measures, as well as improvements in metacognitive beliefs and maladaptive coping strategies (Callesen et al., 2019; Haseth et al., 2019).
According to the mentioned studies, there is a shortage of research regarding the lack of comparison between these treatments. Therefore, this research can be considered innovative from this perspective. Additionally, given the significance of anxiety and its profound impact on various aspects of life and mental well-being, there is a necessity for such studies. However, to establish definitive conclusions, further trials with a larger number of participants are required. The current findings indicate that MCT may be more effective than other psychotherapy forms, including ACT. To comprehend the characteristics, rationale, and underlying concepts of these two approaches, an examination of their impact on individuals can be undertaken. Individuals with anxiety who do not respond well to conventional treatments and exhibit low mental and social well-being along with a poor quality of life might benefit from these therapies. This study assesses and compares the impact of ACT and MCT on women diagnosed with GAD. The researchers evaluate how these therapies influence the psychological well-being of women.
Materials and Methods
Study design and participants
The current study has an applied purpose, utilizes a semi-experimental research method, and follows a pre-test-post-test design with a control group and a two-month follow-up phase. The statistical population for this study comprises women living in Tehran City, Iran, who have GAD. The research was conducted in Tehran, Iran, during the summer and autumn of 2022. Due to the unavailability of statistics and information on all individuals with GAD syndrome in Tehran, a non-random and purposeful sampling process was employed. Only individuals who met the criteria for GAD based on the questionnaire and diagnostic interview were included. The sample size consisted of 36 patients with GAD who agreed to participate in the research (n=12 women in each group). The sample size was determined using G*Power software, with a significance level of 0.05, test power of 0.90, and effect size of 1.42 (Mohammadi et al., 2021). Meanwhile, 60 individuals were initially selected as the sample to account for potential dropouts. Following the sample selection, the participants were randomly divided into three groups, with two experimental groups assigned to each intervention and one control group (n=17 for each group). All treatment and control groups were matched in terms of all the criteria for participating in the sessions.
To participate in the research, the individuals had to meet certain requirements. These requirements included not taking any psychiatric medications, not having specific physical issues or personality disorders, not having a history of hospitalization or psychological treatment, having between 18 to 60 years of age, not having a clinical diagnosis of GAD, having a basic level of education in reading and writing, and providing informed consent. On the other hand, there are also criteria for exclusion from the research. These include having the co-occurring disorders mentioned in the entry criteria, participating in simultaneous counseling or other forms of psychotherapy, having a severe physical or mental disorder (such as a substance use disorder, personality disorders, psychosis, or symptoms like delusions, hallucinations, or lack of awareness of time and place) that would prevent intervention, receiving drug therapy, or having three consecutive sessions without attendance.
Study procedure
Once the necessary permissions were obtained to carry out the research, communication was initiated through social media platforms and with cultural and artistic centers in Tehran municipality (specifically the library) and three psychological clinics in the city, covering regions 2, 3, and 4. Subsequently, negotiations were held with the management and officials of these centers, and permission was secured to collaborate and conduct sampling within the target community of women suffering from GAD syndrome. The individuals who scored below the cut-off line on the questionnaire were contacted individually for further evaluation and to determine their eligibility for participation in the research. A clinical interview for GAD was conducted during a telephone meeting, where individuals were assessed based on specific entry and exit criteria. Those who met the criteria and expressed their willingness were invited to take part in the research.
In addition, these individuals received the necessary information regarding the study’s overall goals, advantages, disadvantages, research process, and duration. This ensured that they could make an informed decision about their participation. A total of 60 individuals were chosen for the investigation. Following the research design and using random assignment, the participants were divided into two groups: The control group (n=17) and the experimental group (n=17). Subsequently, a pre-test was administered, and all participants completed a series of questionnaires. The participants also completed a written consent form to indicate their willingness to participate in the research alongside the pre-test.
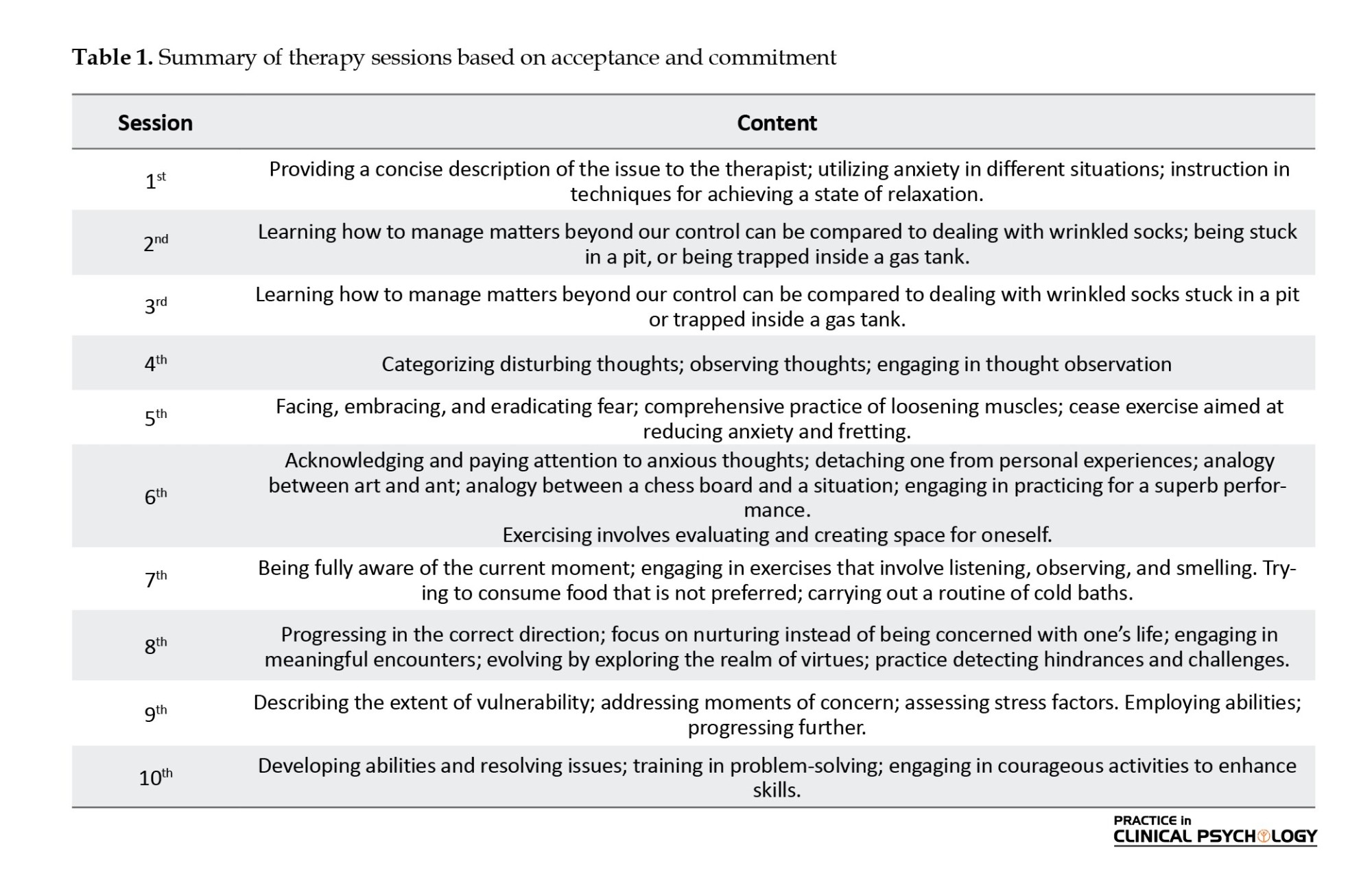
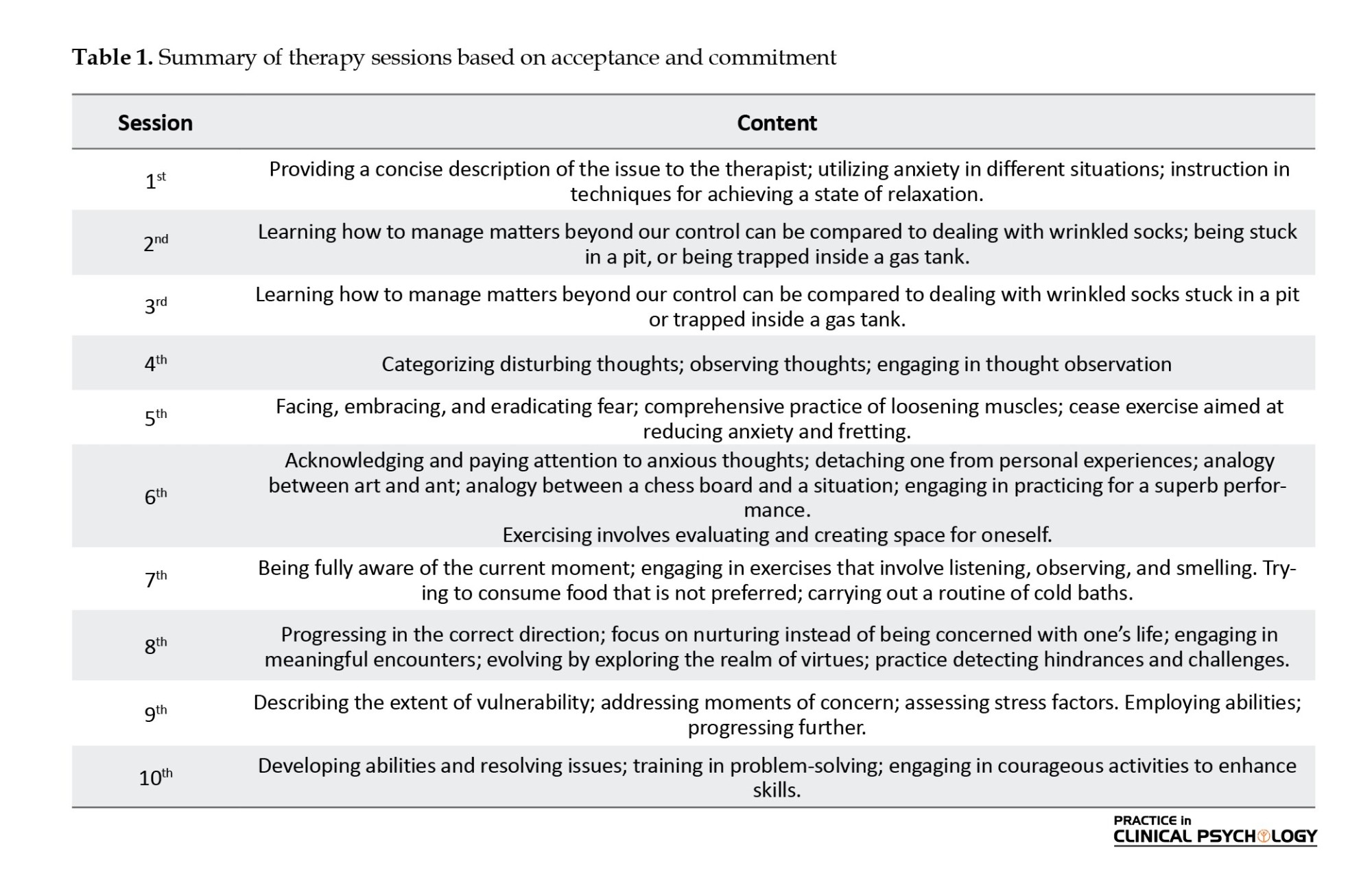
In the next step, individuals from the first experimental group (Table 1) underwent a 10-session therapy program based on ACT, as outlined by Hayes et al. (2012).
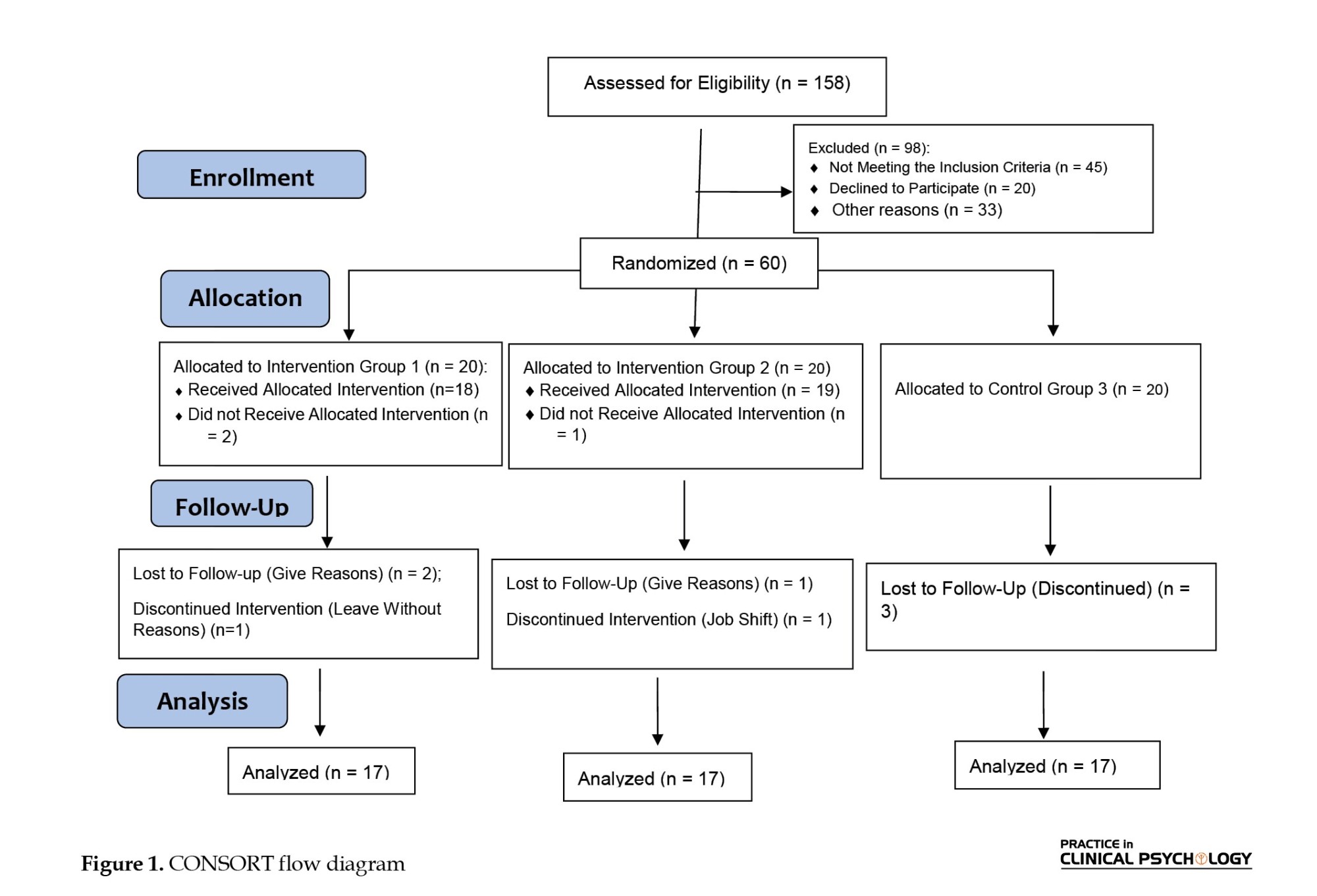
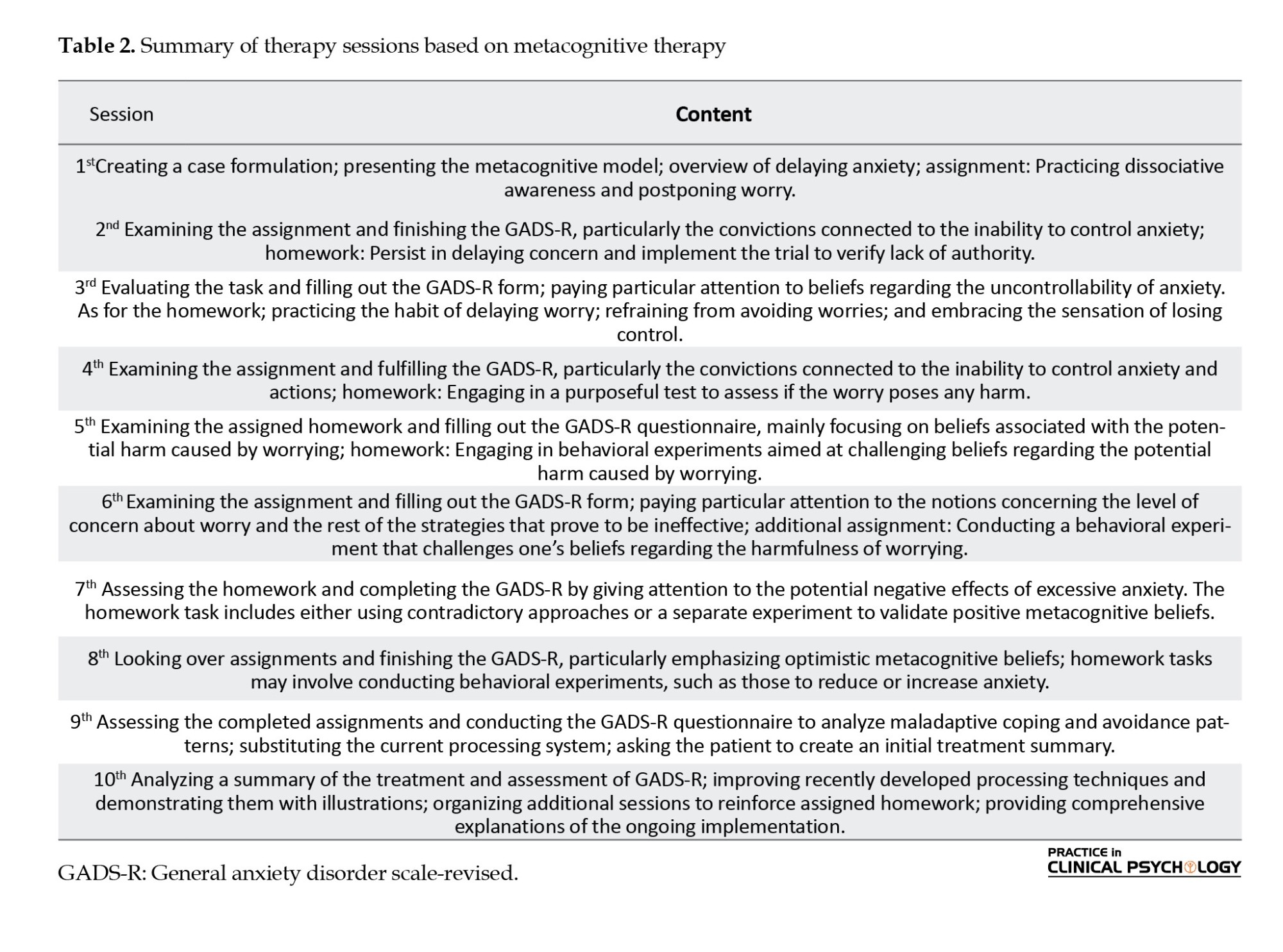
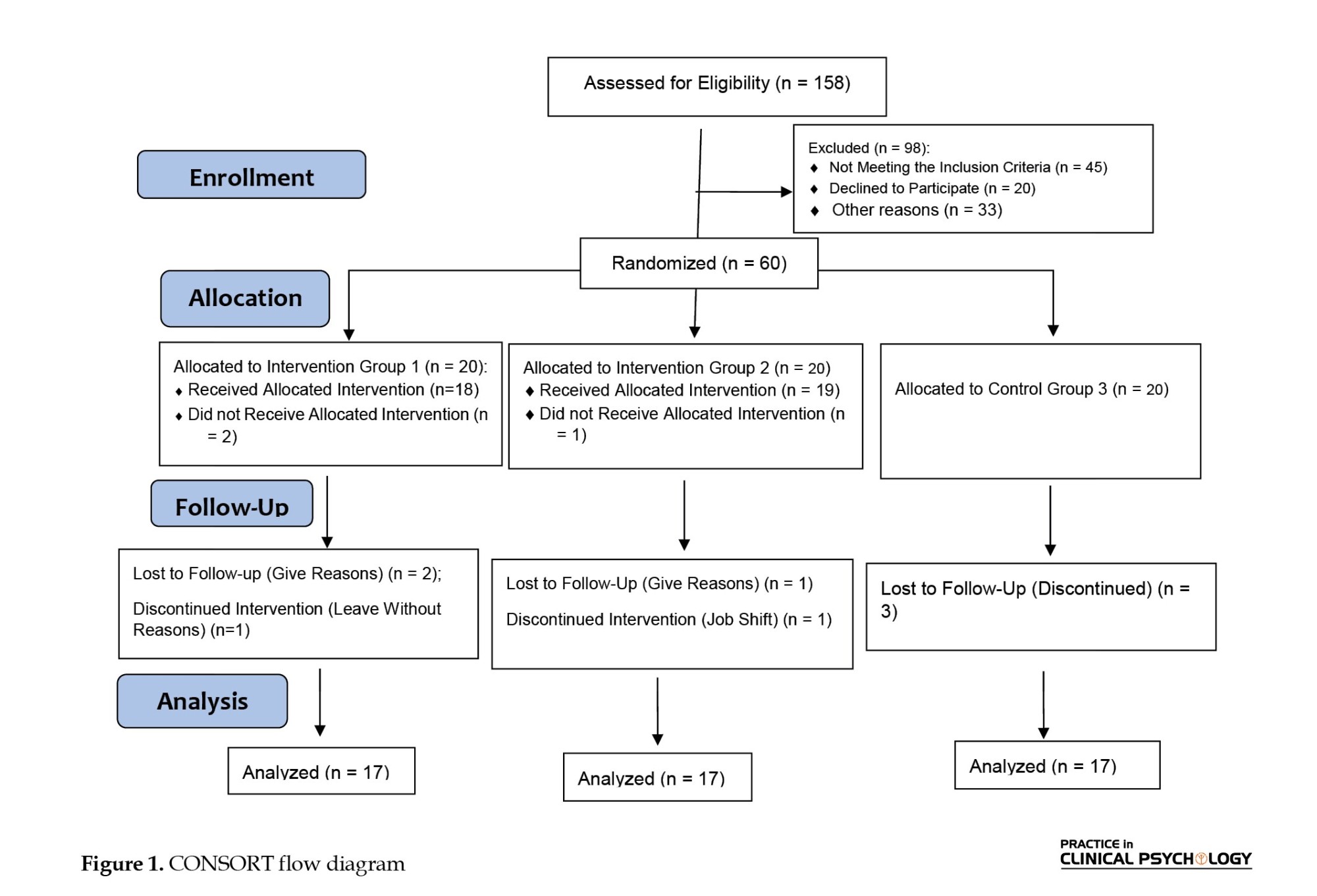
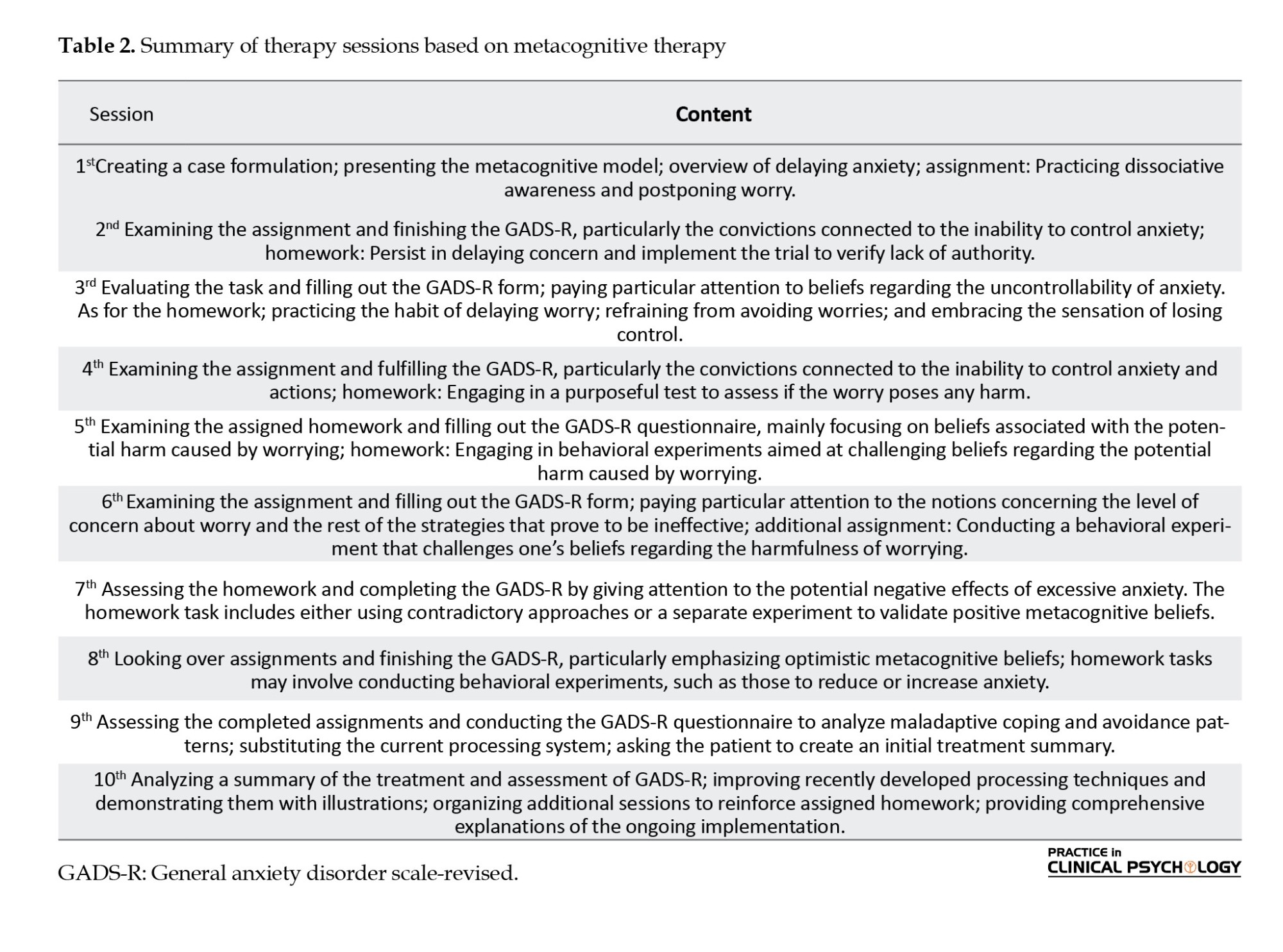
For the second experimental group, a 10-session program of MCT (developed by Wells in 2010) was implemented individually (Table 2). The control group had regular contact with the tester but received no specific active treatment. These therapy sessions took place at the Taliee Clinical Psychology Center and were administered by a PhD candidate in psychology. After the final counseling session, a post-test was conducted for all experimental and control group participants. Additionally, a follow-up phase occurred two months later. To uphold ethical principles, individuals in the control group who desired professional assistance received GAD treatment after completing the study. Figure 1 displays the consolidated standards of reporting trials flow diagram.
Research instruments were used to evaluate all participants during the pre-test and post-test stages.
Research instruments
Research-made demographic questionnaire
A researcher-made demographic was used to determine the participant’s age, education, occupation, and marital status.
Generalized anxiety disorder short scale
The scale developed by Spitzer et al. (2006) consists of 7 primary questions and 1 additional question to assess the level of impairment in various aspects of the individual’s life, including social, family, and occupational functioning. Each item was scored using a Likert scale with 4 options ranging from never to almost every day. The seven main questions of the generalized anxiety scale evaluate the mental state and difficulties experienced by the respondent over the past two weeks. Each question is assigned a score from 0 to 3, resulting in a total score range of 0 to 21. Regarding internal consistency, the Iranian scale version demonstrated good reliability with a Cronbach α value of 0.876 (Omani-Samani et al., 2018).
Ryff scales of psychological well-being
The researchers utilized the 42-item version of the Ryff scales of psychological well-being to measure psychological well-being. This index is widely used and focuses on eudaimonic well-being, encompassing various aspects, such as autonomy, environmental mastery, personal growth, positive relationships, purpose in life, and self-acceptance. An example item from this scale is as follows: “I feel a sense of purpose and direction in my life.” Ryff’s measure possesses factorial validity, high internal consistency, and high criterion-related validity. In a previous study, the Persian version of this measure achieved a Cronbach α of 0.89 (Aghababaei et al., 2016), while the short 18-item version obtained the same α value (Varaee et al., 2018). In the present study, the Persian versions of these scales exhibited Cronbach α values that ranged from 0.57 to 0.81. The survey packages used for data collection contained the Persian adaptations of the measures above and were administered to various classroom groups. The participants provided informed consent before answering demographic questions and completing the measures described earlier.
All procedures adhered to the ethical guidelines of the respective institution for research involving human subjects.
Statistical analyses
An analysis of variance of the repeated measure with a within-group effect was utilized to examine the impact of acceptance and commitment treatments and MCT on the scores of psychological well-being components in the pre-test, post-test, and follow-up periods. Initially, the hypothesis of the homogeneity of the variables was assessed to investigate the mean difference between the mean components of psychological well-being in the three groups at the three treatment stages. The normality of the data was tested using the Shapiro-Wilk test, and the significance threshold for each research variable was found to be above 0.05, indicating that parametric tests can be employed. Additionally, the Levene test was conducted to verify the equality of variance in groups, assuming all variables’ variances are equal (P>0.05). The obtained data were subjected to statistical analysis using the SPSS software, version 25, at a 0.05 significance level.
Results
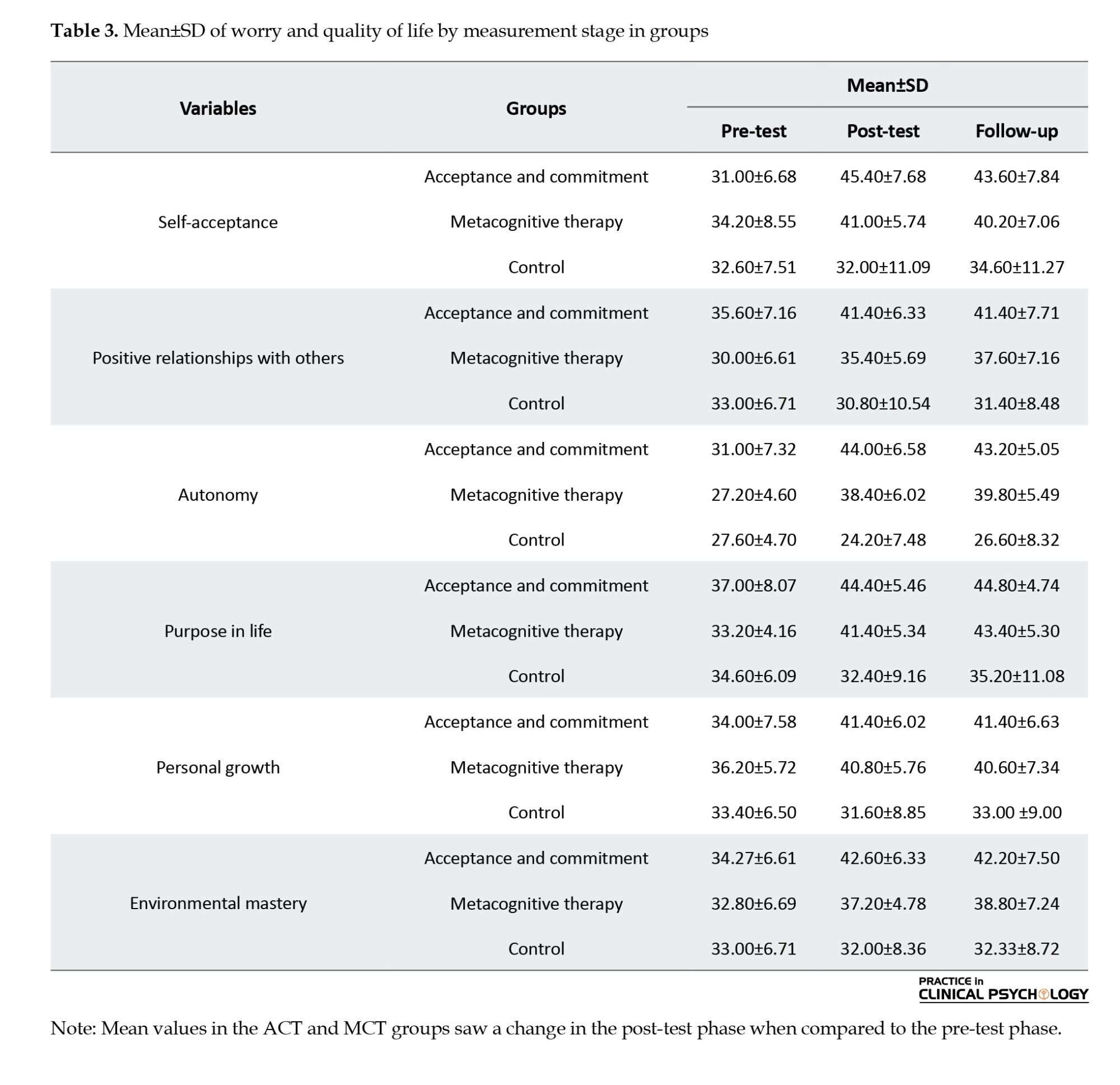
The Mean±SD of the age of women with GAD was 44.23±5.32. Demographic variables of women with this disorder are presented in Table 3. The results of the Kruskal–Wallis showed no significant difference in the age (P=0.78) and education level (P=0.57) of the three groups.
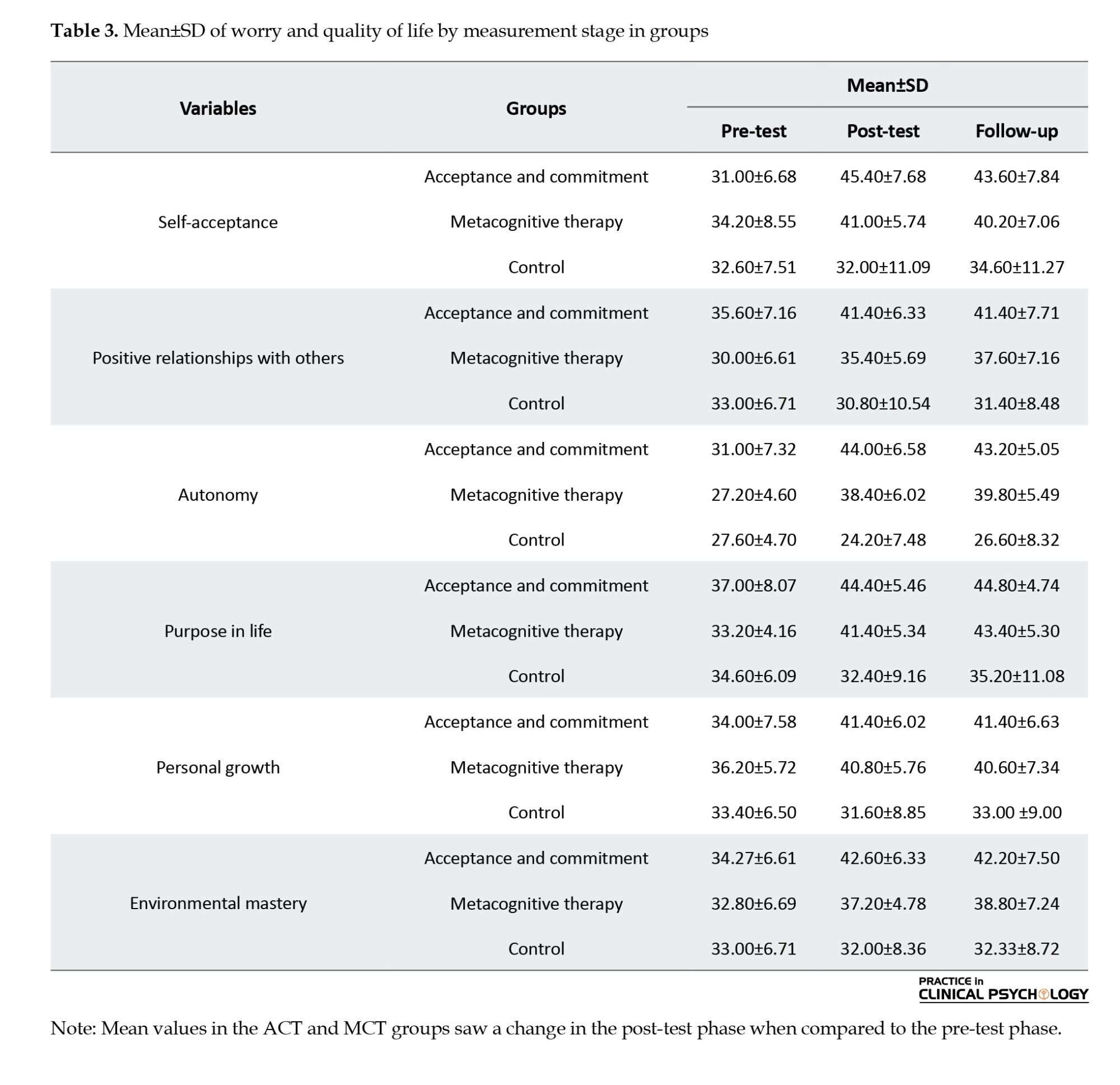
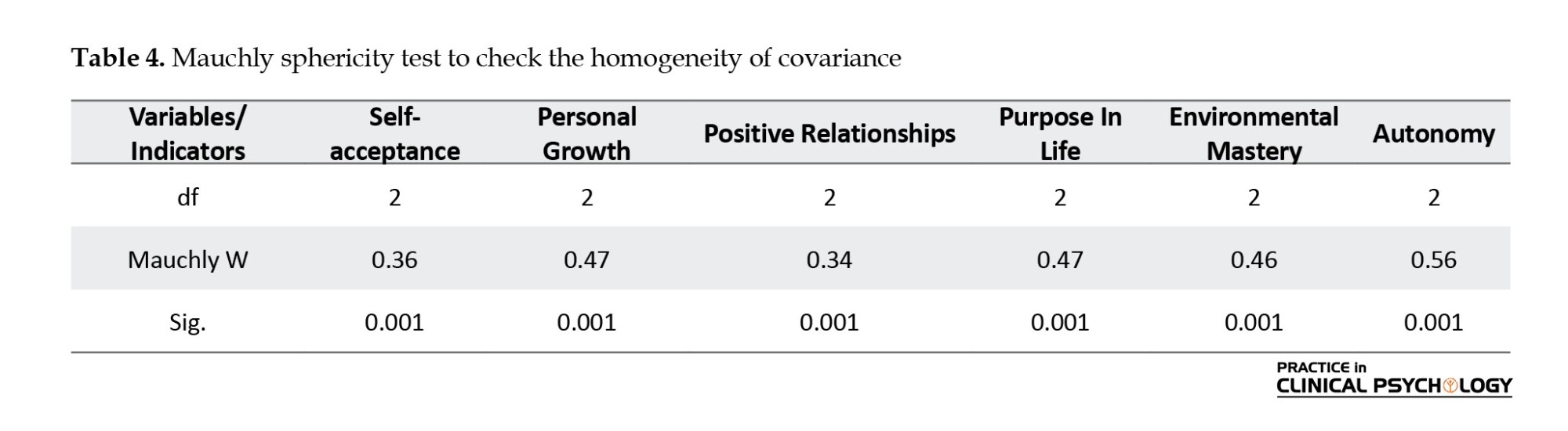
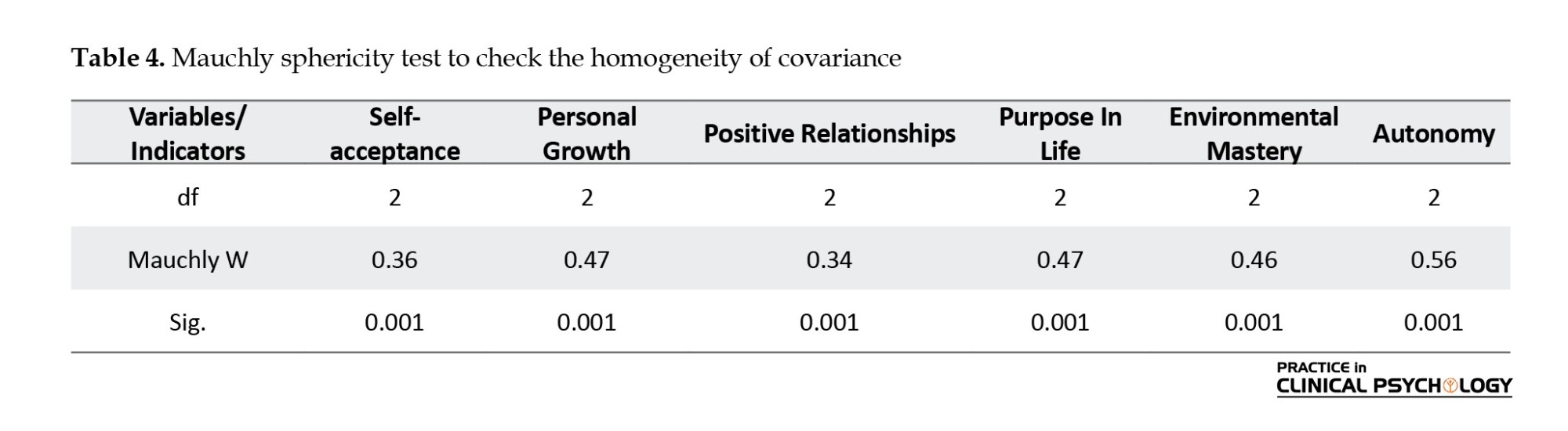
The test of sphericity to check the homogeneity of covariance was not established (P>0.05). Accordingly, the greenhouse–Geisser test is used in the hypothesis test to obtain a more accurate approximation, and the results of the within-group analysis of variance are calculated using the lack of the sphericity assumption (Table 4).
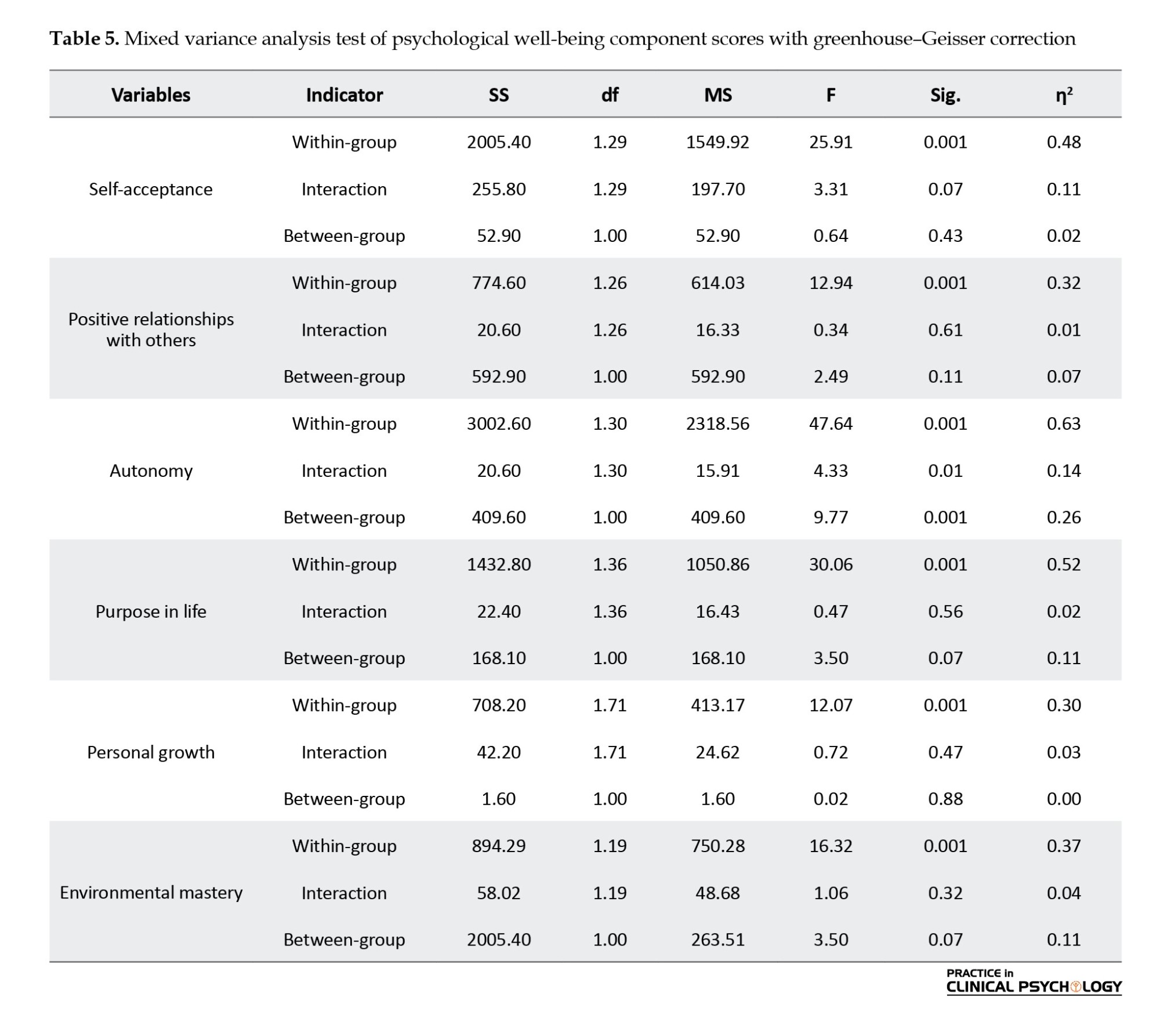
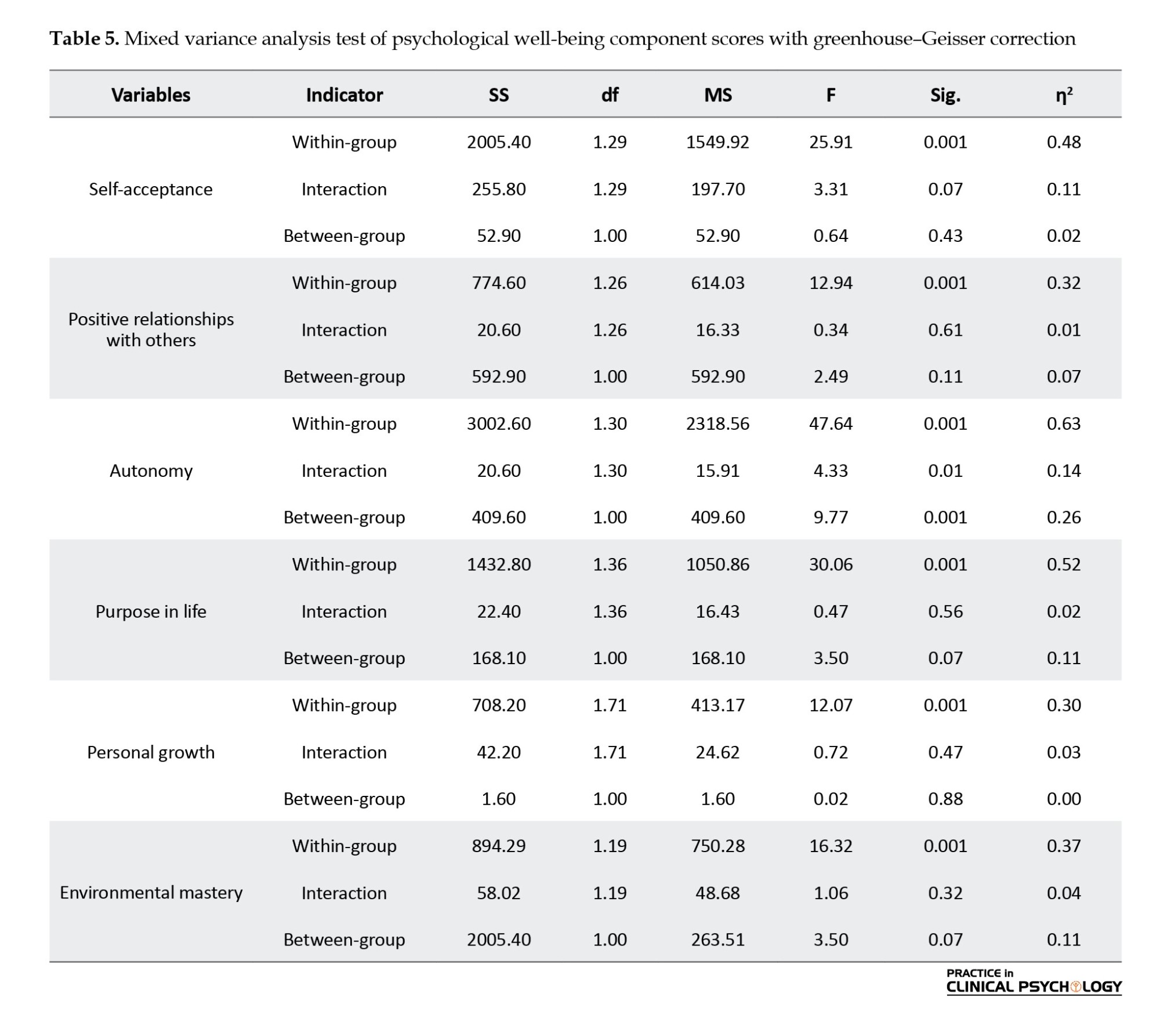
According to the results of Table 5, the difference between the scores of the psychological well-being components in the three study periods is significant (P<0.01). Furthermore, the mean autonomy scores and psychological well-being exhibited considerable discrepancies within the two analyzed groups (P<0.01). In addition, the interaction between research stages and group membership was also significant in the variables of autonomy and psychological well-being (P<0.01). In other words, the difference between autonomy scores and psychological well-being in the three study periods in the two experimental groups was significant. Therefore, it can be concluded that metacognitive therapy and acceptance and commitment therapy have different effects on improving autonomy and psychological well-being. The results show a significant difference in autonomy and psychological well-being levels in the pre-test, post-test, and follow-up periods.
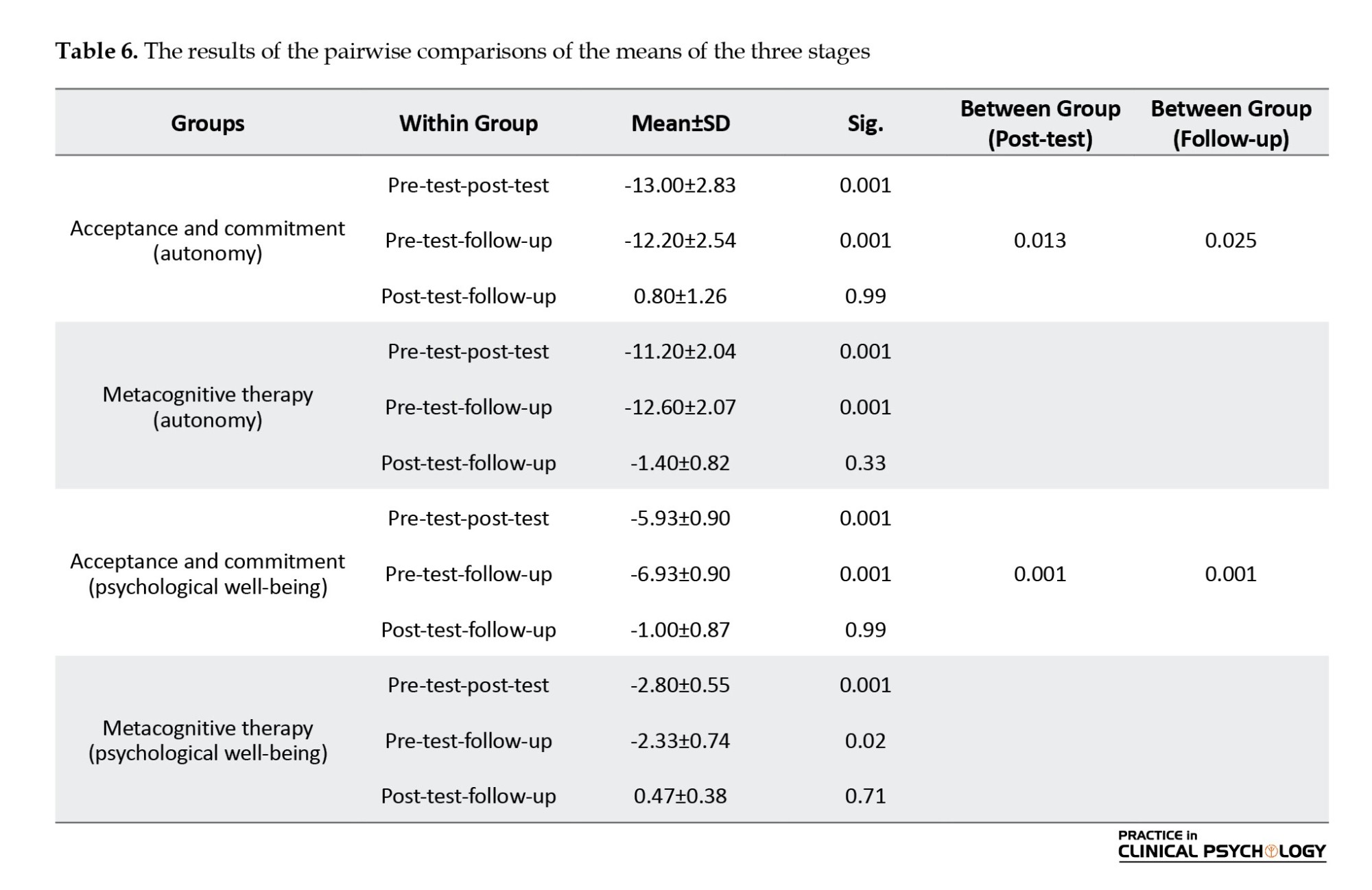
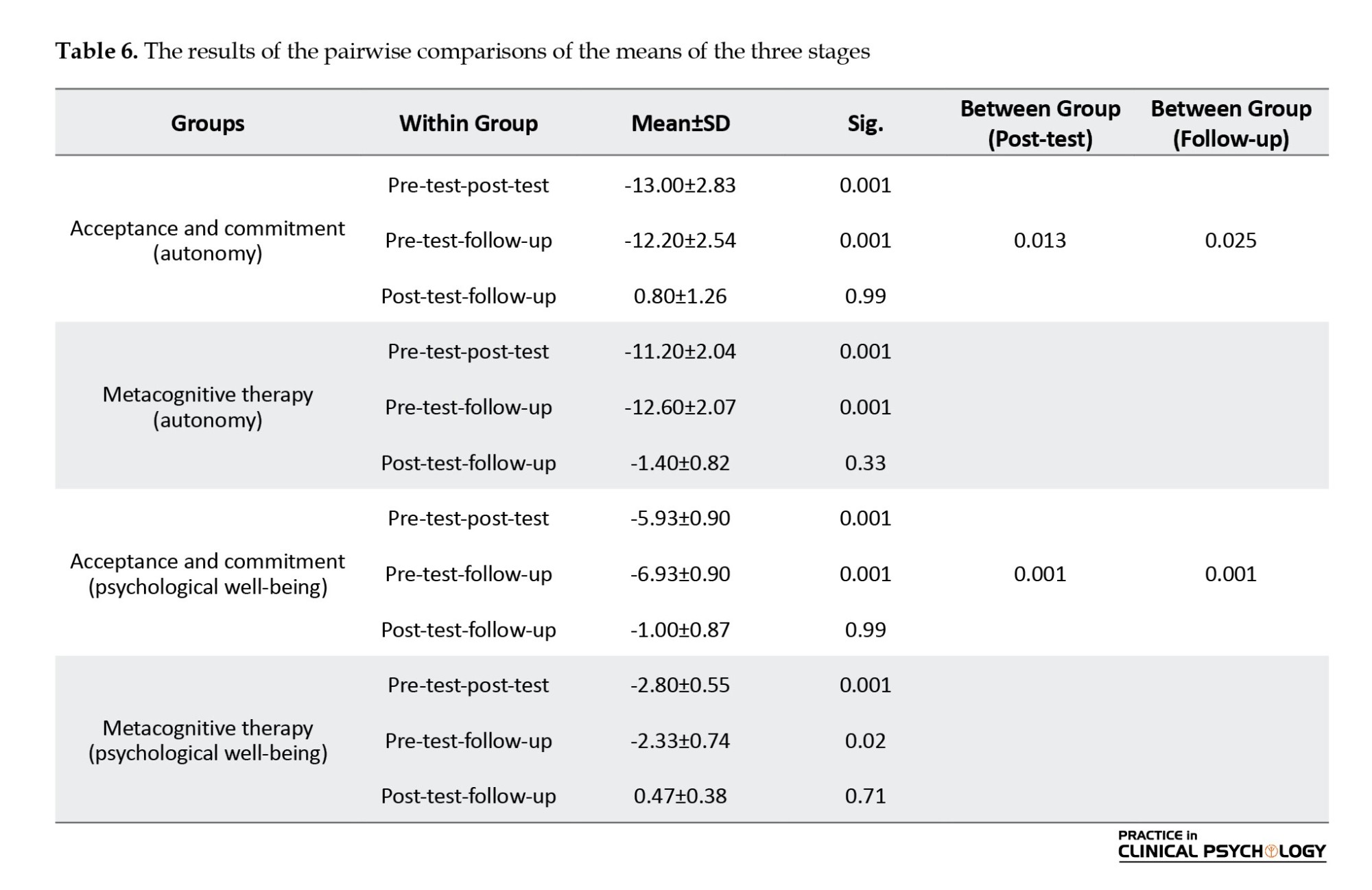
The results of Table 6 show that the difference between the pre-test and the two post-test and follow-up stages in the two experimental groups is significant (P<0.01). 0.55 Also, the difference between the post-test and follow-up scores in the two groups of MCT and therapy based on ACT is significant, showing the treatment effect’s greater effectiveness and stability in the therapy group based on ACT (P<0.05).
Discussion
This study determined whether ACT or MCT could improve the psychological well-being of women diagnosed with GAD. In contrast to MCT, ACT demonstrated notable superiority, and its positive outcomes endured for an extended period in the follow-up phase.
Consistent with the findings of this study, Eqharari et al., 2019; Sharif Ara et al., 2023; Demehri et al. 2019, and Mani et al., 2019 confirmed the effectiveness of ACT.
According to the results of multivariate analysis of covariance, ACT treatment has a positive effect on self-acceptance, positive relationships with others, autonomy, purposeful life, and overall psychological well-being and sexual function scores. The results also showed that ACT treatment had no significant effect on the components of environmental dominance and individual growth. According to repeated measures analysis of variance, the effect of ACT treatment has been effective on psychological well-being, including total psychological well-being and sexual performance, as well as on self-acceptance, positive relationships with others, and purposeful life (Hasanzadeh et al., 2019). ACT is a distinct form of behavioral and cognitive therapy that places significant emphasis on the context of behavior (Hayes et al., 2013; Whiting et al., 2017). It builds upon a relational frame model that connects behavioral principles to psychological issues and positive behavior (Hayes et al., 2013; Whiting et al., 2017). The primary goal of ACT is to optimize human potential and enable individuals to lead a fulfilling and meaningful life (White et al., 2021). Within ACT, experiential acceptance or mindfulness is a fundamental process closely linked to well-being (Eadeh et al., 2023). Furthermore, ACT places great importance on fostering valued or engaged living. Making committed choices and pursuing goals that align with intrinsic values and motivations has been identified as a predictor of well-being (Assor et al., 2020). The ability to live mindfully, accept current experiences, and act under one’s core values is psychological flexibility (Katajavuori et al., 2023).
In contrast to prior research, this study revealed varying outcomes regarding how much MCT enhances psychological well-being. Research has consistently shown that MCT is a highly effective approach (Wells, 2010; Normann & Morina, 2018; Haseth et al., 2019; Callesen et al., 2019; Mikaeili, 2022; Strand et al., 2023).
Wells and Matthews (1996) introduced an earlier trans-diagnostic approach known as the self-regulatory executive function model, which proposes universal psychological factors across various pathologies. They argued that psychological disorders are sustained by a common maladaptive cognitive attentional syndrome that should be the focus of treatment (Callesen et al., 2019). An increased focus on oneself characterizes the CAS, repetitive negative thinking involving worry and rumination, and unhelpful coping strategies and behaviors such as monitoring threats, suppressing thoughts, and avoiding situations (Strand et al., 2023). This syndrome results from an individual’s metacognitive beliefs, which result in prolonged negative processing and subsequent distress. There are two types of metacognitive beliefs as follows: Negative metacognitive beliefs and positive metacognitive beliefs. Negative metacognitive beliefs revolve around the idea that worry is uncontrollable and dangerous (for example, “I have no control over my worries” or “My worries can harm me”). On the other hand, positive metacognitive beliefs emphasize the usefulness of worry (for instance, “Worrying helps me cope,” or “If I worry, I’ll be prepared”). These underlying metacognitive beliefs play a significant role in driving the CAS. MCT, developed based on this model, eliminates the CAS and modifies positive and negative metacognitive beliefs (Wells, 2010).
While these two approaches were first applied to the psychological well-being of women with generalized anxiety, in contrast to the strong background in favor of MCT treatment, most previous studies compared ACT treatment with other treatments, and both showed results in favor of the ACT. For example, a study comparing the effect of commitment-based acceptance and treatment and a mindfulness-based stress reduction program on work attitudes, health-related anxiety, psychological well-being, and body image showed that ACT is more effective than a mindfulness-based stress reduction program (Pasyar et al., 2023). In addition, the study was conducted to compare the effect of acceptance and commitment therapy and metacognition therapy on the recovery of women on dialysis. Both treatments improve the endurance of patients on hemodialysis (Tajbakhsh et al., 2023). Ahmadi et al. (2022) have shown that ACT and MCT are effective in increasing adaptive cognitive emotion regulation strategies and decreasing cognitive emotional regulation strategies. Furthermore, the results suggest that ACT is more effective than MCT in modulating cognitive-emotional regulation strategies (Ahmadi et al., 2022). Instead of teaching better and better strategies to change or reduce unwanted thoughts and emotions, ACT teaches patients skills to perceive and observe unpleasant thoughts and emotions as they are (Yasaie Sokeh et al., 2017).
Conclusion
Women with GAD benefited from therapy courses in terms of psychological well-being. Thus, unlike the MCT, the results suggest that ACT-based exercises would be of additional value for improving psychological well-being. As this is the first study on the topic, more research is needed to determine the effectiveness of these two therapies for general anxiety in individuals.
Study limitations
There are limitations to the study. Initially, a small sample size and nonrandom sampling put the validity of our findings at risk. Our results may have been influenced by recall bias and answer accuracy due to the use of self-report instruments. Despite our efforts to control extraneous variables statistically, there may have been additional effects of subject variables that we overlooked, such as comorbid physical conditions that could contribute to anxiety symptoms. Therefore, we recommend that future studies consider these variables as exclusion criteria.
Furthermore, since our sample consisted of individuals with mild anxiety symptoms, it is possible that different results would be observed at different severity stages of anxiety disorders. Additionally, the cross-sectional design of this study cannot determine a cause-and-effect relationship for the observed associations. Future studies should employ longitudinal designs to examine changes in mindfulness and metacognitions over time and identify causal predictors of anxiety disorder symptom severity. Finally, it would have been preferable to assess mindfulness and metacognition in individuals with anxiety disorders who are not undergoing pharmacological or non-pharmacological treatment to avoid the potential effects of these treatments on symptom severity.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Islamic Azad University, Semnan Branch (Code: IR.IAU.SHAHROOD.REC.1401.058).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest
Acknowledgments
The authors would like to thank everyone who participated in the research.
References
Abdollahi, S. M., Rafiepoor, A., & Sabet, M. (2020). The effectiveness of acceptance and commitment therapy on mental health, hopefulness and meaningfulness in people with cardiovascular disease. Iranian Journal of Health Psychology, 3(1), 61-70. [DOI:10.30473/ijohp.2020.50883.1069]
Aghababaei, N., Błachnio, A., Arji, A., Chiniforoushan, M., Tekke, M., & Fazeli Mehrabadi, A. (2016). Honesty-humility and the HEXACO structure of religiosity and well-being. Current Psychology, 35, 421-426. [DOI:10.1007/s12144-015-9310-5]
Ahmadi Roghabadi, A., Bagherzadeh Golmakani, Z., Akbarzade, M., Mansouri, A., & Khodabakhsh, M. (2022). [Comparison of the effectiveness of acceptance and commitment therapy and metacognitive therapy on adaptive and maladaptive strategies of cognitive emotion regulation in patients with substance use disorder undergoing methadone maintenance treatment (Persian)]. Research in Clinical Psychology and Counseling, 12(1), 60-78. [DOI:10.22067/TPCCP.2022.70654.1118]
Assor, A., Soenens, B., Yitshaki, N., Ezra, O., Geifman, Y., & Olshtein, G. (2020). Towards a wider conception of autonomy support in adolescence: The contribution of reflective inner-compass facilitation to the formation of an authentic inner compass and well-being. Motivation and Emotion, 44, 159-174. [DOI:10.1007/s11031-019-09809-2]
Azkhosh, M., Farhoudianm, A., Saadati, H., Shoaee, F., & Lashani, L. (2016). Comparing acceptance and commitment group therapy and 12-steps narcotics anonymous in addict’s rehabilitation process: A randomized controlled trial. Iranian Journal of Psychiatry, 11(4), 244. [PMID]
Callesen, P., Capobianco, L., Heal, C., Juul, C., Find Nielsen, S., & Wells, A. (2019). A preliminary evaluation of transdiagnostic group metacognitive therapy in a mixed psychological disorder sample. Frontiers in Psychology, 10, 1341. [DOI:10.3389/fpsyg.2019.01341] [PMID]
Chaturvedi, S. K., Manche Gowda, S., Ahmed, H. U., Alosaimi, F. D., Andreone, N., & Bobrov, A., et al. (2019). More anxious than depressed: Prevalence and correlates in a 15-nation study of anxiety disorders in people with type 2 diabetes mellitus. General Psychiatry, 32(4), e100076. [DOI:10.1136/gpsych-2019-100076] [PMID]
Daryadel, J., Mikaeili, N., Atadokht, A., & Molavi, P. (2022). The efficacy of metacognitive therapy based on detached mindfulness on meta-worry and interpersonal cognitive distortion in women with postpartum depression. Journal of Psychologicalscience, 21(110), 349-366. [DOI:10.52547/JPS.21.110.349]
Demehri, F., Saeedmanesh, M., & Jala, N. (2018). [The effectiveness of acceptance and commitment therapy (ACT) on rumination and well-being in adolescents with general anxiety disorder (Persian)]. Journal of Disability Studies, 8, 25. [Link]
Eadeh, H. M., Adamowicz, J. L., Markon, K., & Thomas, E. B. K. (2023). Using network analysis to examine connections between Acceptance and Commitment Therapy (ACT) processes, internalizing symptoms, and well-being in a sample of undergraduates. Journal of Affective Disorders, 320, 701-709. [DOI:10.1016/j.jad.2022.10.004] [PMID]
Eqharari, L., Asadi, F., Javazi, S., & Vahid, T. (2019). [Effectiveness of Acceptance and Commitment (ACT) therapy on behavioral inhibition and cognitive-behavioral avoidance of women with generalized anxiety disorder (Persian)]. Iranian Journal of Nursing Research, 13(6), 31-38. [Link]
Faraci, P., Bottaro, R., Valenti, G. D., & Craparo, G. (2022). Psychological well-being during the second wave of COVID-19 pandemic: The mediation role of generalized anxiety. Psychology Research and Behavior Management, 15, 695–709. [DOI:10.2147/PRBM.S354083] [PMID]
Hasanzadeh, M., Akbari, B., & Abolghasemi, A. (2019). [Efficiency of acceptance and commitment therapy on psychological well-being and sexual function in women with infertility history (Persian)]. Avicenna Journal of Nursing and Midwifery Care, 27(4), 250-259. [DOI:10.30699/ajnmc.27.4.250]
Haseth, S., Solem, S., Sørø, G. B., Bjørnstad, E., Grøtte, T., & Fisher, P. (2019). Group metacognitive therapy for generalized anxiety disorder: A pilot feasibility trial. Frontiers in Psychology, 10, 290. [DOI:10.3389/fpsyg.2019.00290] [PMID]
Hayes, S. C., Levin, M. E., Plumb-Vilardaga, J., Villatte, J. L., & Pistorello, J. (2013). Acceptance and commitment therapy and contextual behavioral science: Examining the progress of a distinctive model of behavioral and cognitive therapy. Behavior Therapy, 44(2), 180-198. [DOI:10.1016/j.beth.2009.08.002] [PMID]
Hayes, S. C., Pistorello, J., & Levin, M. E. (2012). Acceptance and commitment therapy as a unified model of behavior change. The Counseling Psychologist, 40(7), 976-1002. [DOI:10.1177/0011000012460836]
Hossein Nazari, N., Nejat, H., & Saffarian Tosi, M. (2022). [The comparison of the effectiveness of well‐being therapy with acceptance and commitment therapy on death anxiety in the elderly (Persian)]. Aging Psychology, 8(1), 25-38. [Link]
Iani, L., Quinto, R. M., Lauriola, M., Crosta, M. L., & Pozzi, G. (2019). Psychological well-being and distress in patients with generalized anxiety disorder: The roles of positive and negative functioning. PloS One, 14(11), e0225646. [DOI:10.1371/journal.pone.0225646] [PMID]
Katajavuori, N., Vehkalahti, K., & Asikainen, H. (2023). Promoting university students’ well-being and studying with an acceptance and commitment therapy (ACT)-based intervention. Current Psychology, 42(6), 4900-4912. [DOI:10.1007/s12144-021-01837-x]
Köcher, L. M., Schneider, K., & Christiansen, H. (2021). Thinking about worry: A systematic review and meta-analysis on the assessment of metacognitions in children and adolescents. World Journal of Psychiatry, 11(9), 635. [DOI: 10.5498/wjp.v11.i9.635] [PMID]
LaFreniere, L. S., & Newman, M. G. (2020). Exposing worry’s deceit: Percentage of untrue worries in generalized anxiety disorder treatment. Behavior Therapy, 51(3), 413-423. [DOI:10.1016/j.beth.2019.07.003] [PMID]
LeardMann, C. A., McMaster, H. S., Warner, S., Esquivel, A. P., Porter, B., & Powell, T. M., et al. (2021). Comparison of posttraumatic stress disorder checklist instruments from diagnostic and statistical manual of mental disorders, fourth edition vs fifth edition in a large cohort of US Military Service Members and Veterans. JAMA Network Open, 4(4), e218072. [PMID]
Li, J., Xia, Y., Cheng, X., & Li, S. (2020). Fear of uncertainty makes you more anxious? Effect of intolerance of uncertainty on college students’ social anxiety: A moderated mediation model. Frontiers in Psychology, 11, 565107. [DOI:10.3389/fpsyg.2020.565107] [PMID]
Luo, X., Tong, S., Fang, Z., & Qu, Z. (2019). Frontiers: Machines vs. humans: The impact of artificial intelligence chatbot disclosure on customer purchases. Marketing Science, 38(6), 937-947. [DOI:10.1287/mksc.2019.1192]
Mani, A., Mehdipour, Z., Ahmadzadeh, L., Tahmasebi, S., Khabir, L., & Mosalaei, A. (2019). The effectiveness of group acceptance and commitment psychotherapy on psychological well-being of breast cancer patients in Shiraz, Iran. Middle East Journal of Cancer, 10(3), 231-238. [DOI:10.30476/mejc.2019.45316]
McEvoy, P. M. (2019). Metacognitive therapy for anxiety disorders: A review of recent advances and future research directions. Current Psychiatry Reports, 21(5), 29. [DOI:10.1007/s11920-019-1014-3] [PMID]
Mohammadi, H., Khalatbari, J., & Abolmaali, K. (2021). The effect of integrating cognitive-behavioral therapy and mindfulness therapy on lifestyle of women with irritable bowel syndrome. Women’s Health Bulletin, 8(4), 220-227. [DOI:10.30476/whb.2021.91397.1124]
Montazernia, B., Kooshki, S., Oraki, M., & Mirzaian, B. (2021). Comparing The Efficacy of Acceptance and Commitment Therapy (ACT) and Dialectical Behavior Therapy Skills Training (DBT-ST) on cognitive emotion regulation in patients with type II Diabetes. Iranian Journal of Health Psychology, 4(1), 33-48. [Link]
Normann, N., & Morina, N. (2018). The efficacy of metacognitive therapy: A systematic review and meta-analysis. Frontiers in Psychology, 9, 2211. [DOI:10.3389/fpsyg.2018.02211] [PMID]
Omani-Samani, R., Ghaheri, A., Navid, B., Sepidarkish, M., & Maroufizadeh, S. (2018). Prevalence of generalized anxiety disorder and its related factors among infertile patients in Iran: A cross-sectional study. Health and Quality of Life Outcomes, 16(129), 1-5. [Link]
Pasyar, S., Baghooli, H., Barzegar, M., & Sohrabi, N. (2023). [Comparing the effectiveness of acceptance and commitment therapy and mindfulness-based stress reduction program on negative feedback, health anxiety, psychological well-being, and body image in women undergoing mastectomy (Persian)]. Psychological Achievements, 30(1), 285-314. [DOI:10.22055/psy.2023.43119.2969]
Sharif Ara, B., Khosropour, F., & Molayi Zarandi, H. (2023). Effectiveness of Acceptance and Commitment Therapy (ACT) on emotional processing, irrational beliefs and rumination in patients with generalized anxiety disorder. Journal of Adolescent and Youth Psychological Studies, 4(4), 34-44. [Link]
Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092-1097. [DOI:10.1001/archinte.166.10.1092] [PMID]
Strand, E. R., Veium, L. T., Engvik, L. S., & Nordahl, H. (2023). Generic group metacognitive therapy for patients with major depressive disorder and related problems: A preliminary evaluation in specialized mental health care. International Journal of Cognitive Therapy, 16, 497–509. [DOI:10.1007/s41811-023-00175-z]
Tajbakhsh, R., Haddadi, S., Zeighami Mohammadi, S., Malihi Alzakerini, S., & Borumand, M. (2023). [Comparison of the effect of “acceptance and commitment therapy” and “metacognitive therapy” on the resilience of women undergoing hemodialysis (Persian)]. Journal of Health Promotion Management, 12(3), 82-94. [Link]
Takebayashi, Y., Tanaka, K., Sugiura, Y., & Sugiura, T. (2018). Well-being and generalized anxiety in Japanese undergraduates: a prospective cohort study. Journal of Happiness Studies, 19, 917-937. [DOI:10.1007/s10902-017-9852-3]
Varaee, P., Momeni, K., & Moradi, A. (2018). The prediction of psychological well-being based on death anxiety and self-compassion in the Elderly. International Journal of Behavioral Sciences, 12(1), 18-24. [Link]
Weisman, J. S., & Rodebaugh, T. L. (2018). Exposure therapy augmentation: A review and extension of techniques informed by an inhibitory learning approach. Clinical Psychology Review, 59, 41-51. [DOI:10.1016/j.cpr.2017.10.010] [PMID]
Wells, A. (1995). Meta-cognition and worry: A cognitive model of generalized anxiety disorder. Behavioural and Cognitive Psychotherapy, 23(3), 301-320. [DOI:10.1017/S1352465800015897]
Wells, A. (2010). Metacognitive theory and therapy for worry and generalized anxiety disorder: Review and status. Journal of Experimental Psychopathology, 1(1), jep-007910. [DOI:10.5127/jep.007910]
Wells, A., & Matthews, G. (1996). Modelling cognition in emotional disorder: The S-REF model. Behaviour Research and Therapy, 34(11-12), 881-888. [DOI:10.1016/S0005-7967(96)00050-2]
White, R. G., Bethell, A., Charnock, L., Leckey, S., & Penpraze, V. (2021). Acceptance and commitment approaches for athletes’ wellbeing and performance. Cham: Palgrave Macmillan. [DOI:10.1007/978-3-030-64942-5]
Whiting, D. L., Deane, F. P., Simpson, G. K., McLeod, H. J., & Ciarrochi, J. (2017). Cognitive and psychological flexibility after a traumatic brain injury and the implications for treatment in acceptance-based therapies: A conceptual review. Neuropsychological Rehabilitation, 27(2), 263-299. [DOI:10.1080/09602011.2015.1062115] [PMID]
Wroblewski, A., Hollandt, M., Yang, Y., Ridderbusch, I. C., Pietzner, A., & Szeska, C., et al. (2022). Sometimes I feel the fear of uncertainty: How intolerance of uncertainty and trait anxiety impact fear acquisition, extinction and the return of fear. International Journal of Psychophysiology, 181, 125-140. [DOI:10.1016/j.ijpsycho.2022.09.001] [PMID]
Yasaie Sokeh, M., Shafiabadi, A., & Farzad, V. (2017). Comparison of the efficacy of acceptance and commitment group therapy (ACT) with mindfulness-based cognitive therapy (MBCT) on hemodialysis patients in terms of anxiety and depression. Journal of Fundamentals of Mental Health, 19(special issue), 317-324. [DOI:10.22038/JFMH.2017.9127]
Generalized anxiety disorder (GAD) is a common disorder associated with a chronic course and significantly reduced quality of life (Haseth et al., 2019). This disorder, as outlined in The diagnostic and statistical manual of mental disorders, fifth edition, refers to an excessive and prolonged state of anxiety regarding various events and activities that persists for a minimum of six months and significantly hampers the individual’s ability to function properly. Managing and controlling anxiety is particularly challenging in this disorder (LeardMann et al., 2021; Luo et al., 2019). Anxiety is a fear of uncertainty that a person cannot interpret but experiences unpleasant sensations related to physical stimulation (Wroblewski et al., 2023). Accordingly, the person experiencing this feeling does not know the cause of the anxiety (Li et al., 2020). GAD is a common type of anxiety disorder with a prevalence rate of 5.2% in individuals aged 18–64 years (Chaturvedi et al., 2019). Regardless of likelihood, GAD continuously predicts future irrational or exaggerated negative events (LaFreniere et al., 2020)
Previous research showed each indicator of psychological well-being had strong associations with generalized anxiety (Faraci et al., 2022). In addition, research findings indicated that concern was inversely correlated with psychological well-being (PWB) and tended to be positively linked with symptoms of anxiety, even after accounting for other variables (Iani et al., 2019). The results suggested that fostering a sense of purpose in life and the autonomy dimension of PWB could potentially prevent GAD while strengthening the positive relationship with others dimension of PWB that might contribute to generalized anxiety based on the fear of anxiety. Hence, the dimensions of PWB may be beneficial in a primary prevention setting (Takebayashi et al., 2018). A prior study demonstrated that individuals with GAD who paid less attention to their emotions and moods showed higher levels of PWB, aligning with previous research that found reduced attention to feelings predicted better mental health and positive mood (Iani et al., 2019). Furthermore, it was found that PWB acted as a protective factor in the connection between cognitive vulnerabilities and symptoms of generalized anxiety; thus, anxiety symptoms would not escalate in individuals with high cognitive vulnerability if PWB was high (Takebayashi et al., 2018).
Although researchers have shown that various therapeutic approaches can be effective in the treatment of GAD, the discussion of having empirical support and different types of psychotherapies in the treatment of this disorder have always faced challenges. Acceptance and commitment therapy (ACT) help these individuals develop personal strengths, optimal functioning, and well-being (Mani et al., 2019). A recent study conducted by Hossein Nazari et al (2022) suggests that well-being therapy and ACT have the potential to alleviate death anxiety in older adults. Implementing ACT involves encouraging participants to enhance their dedication to leading healthier and more fulfilling lives. This approach also uses behavioral strategies to cope with negative thoughts and emotions. Consequently, ACT can improve psychological well-being and reduce rumination (Mikaeili, 2022). The outcomes of a prior investigation further support the effectiveness of ACT in diminishing behavioral inhibition and cognitive behavioral avoidance in women afflicted with GAD. Moreover, the use of this cost-effective and straightforward therapeutic approach can serve as a foundation for promoting psychological well-being, managing excitement, and establishing healthy interpersonal relationships (Eqharari et al., 2019; Sharif Ara et al., 2023).
The treatment approach discussed here is a psychological intervention incorporating behavioral and modern evolutionary principles. It employs techniques like mindfulness, acceptance, and commitment to enhance psychological flexibility. The fundamental principles of this approach are as follows: 1) Acknowledging and embracing pain or other unpleasant events and thoughts without attempting to control them; 2) Engaging in actions that align with one’s values and committing to them as meaningful objectives while not disregarding unfamiliar experiences (Montazernia et al., 2021). The integration of verbal and cognitive processes with non-verbal elements contributes to the effectiveness of this treatment. It involves exercises that expose individuals to their fears, linguistic metaphors, and mindfulness practices (Abdollahi et al., 2020). ACT, which is a form of a mindfulness intervention, employs metaphors and proverbs to assist clients in enhancing their lives through increased awareness, acceptance, and present-moment focus instead of engaging in internal conflicts and avoiding internal experiences, such as thoughts, memories, and emotions (Azkhosh et al., 2016).
There have been various studies indicating that exposure techniques lead to significant reductions in GAD symptoms (Weisman & Rodebaugh, 2018). The existing evidence suggests that metacognitive therapy (MCT) is effective in treating anxiety and related disorders (McEvoy, 2019; Normann & Morina, 2018). As an alternative to CBT, MCT specifically focuses on modifying cognitive processes rather than the content of thoughts (Wells, 1995). The foundation of MCT lies in the self-regulatory executive function (S-REF) model (Wells & Matthews, 1996), which suggests that psychological disorders arise from a common set of processes referred to as the cognitive attentional syndrome (CAS). CAS entails persistent negative thinking patterns (rumination and worry), inflexible attention and threat monitoring, and maladaptive behavioral strategies that perpetuate negative thought patterns (Strand et al., 2023). According to the metacognitive model of GAD, individuals’ thoughts and beliefs about worry (known as metacognitive beliefs) play a significant role in developing and maintaining the disorder (Haseth et al., 2019).
From a metacognitive perspective, meta-worry can result in avoidance behaviors, such as situational avoidance, seeking reassurance, distraction, and efforts to control anxious thoughts. When these attempts fail, it further reinforces the individual’s belief in the uncontrollability of worry (Köcher et al., 2021). A recent systematic review and meta-analysis conducted by Normann & Morina, 2018 focused on MCT for anxiety and depression. Their findings significantly improved the pre- to post-treatment effect size when comparing MCT to waitlist controls. Previous research has also explored the effectiveness of group MCT for individuals with GAD. The results demonstrated large effect sizes in the reduction of anxiety, depression, and comorbid measures, as well as improvements in metacognitive beliefs and maladaptive coping strategies (Callesen et al., 2019; Haseth et al., 2019).
According to the mentioned studies, there is a shortage of research regarding the lack of comparison between these treatments. Therefore, this research can be considered innovative from this perspective. Additionally, given the significance of anxiety and its profound impact on various aspects of life and mental well-being, there is a necessity for such studies. However, to establish definitive conclusions, further trials with a larger number of participants are required. The current findings indicate that MCT may be more effective than other psychotherapy forms, including ACT. To comprehend the characteristics, rationale, and underlying concepts of these two approaches, an examination of their impact on individuals can be undertaken. Individuals with anxiety who do not respond well to conventional treatments and exhibit low mental and social well-being along with a poor quality of life might benefit from these therapies. This study assesses and compares the impact of ACT and MCT on women diagnosed with GAD. The researchers evaluate how these therapies influence the psychological well-being of women.
Materials and Methods
Study design and participants
The current study has an applied purpose, utilizes a semi-experimental research method, and follows a pre-test-post-test design with a control group and a two-month follow-up phase. The statistical population for this study comprises women living in Tehran City, Iran, who have GAD. The research was conducted in Tehran, Iran, during the summer and autumn of 2022. Due to the unavailability of statistics and information on all individuals with GAD syndrome in Tehran, a non-random and purposeful sampling process was employed. Only individuals who met the criteria for GAD based on the questionnaire and diagnostic interview were included. The sample size consisted of 36 patients with GAD who agreed to participate in the research (n=12 women in each group). The sample size was determined using G*Power software, with a significance level of 0.05, test power of 0.90, and effect size of 1.42 (Mohammadi et al., 2021). Meanwhile, 60 individuals were initially selected as the sample to account for potential dropouts. Following the sample selection, the participants were randomly divided into three groups, with two experimental groups assigned to each intervention and one control group (n=17 for each group). All treatment and control groups were matched in terms of all the criteria for participating in the sessions.
To participate in the research, the individuals had to meet certain requirements. These requirements included not taking any psychiatric medications, not having specific physical issues or personality disorders, not having a history of hospitalization or psychological treatment, having between 18 to 60 years of age, not having a clinical diagnosis of GAD, having a basic level of education in reading and writing, and providing informed consent. On the other hand, there are also criteria for exclusion from the research. These include having the co-occurring disorders mentioned in the entry criteria, participating in simultaneous counseling or other forms of psychotherapy, having a severe physical or mental disorder (such as a substance use disorder, personality disorders, psychosis, or symptoms like delusions, hallucinations, or lack of awareness of time and place) that would prevent intervention, receiving drug therapy, or having three consecutive sessions without attendance.
Study procedure
Once the necessary permissions were obtained to carry out the research, communication was initiated through social media platforms and with cultural and artistic centers in Tehran municipality (specifically the library) and three psychological clinics in the city, covering regions 2, 3, and 4. Subsequently, negotiations were held with the management and officials of these centers, and permission was secured to collaborate and conduct sampling within the target community of women suffering from GAD syndrome. The individuals who scored below the cut-off line on the questionnaire were contacted individually for further evaluation and to determine their eligibility for participation in the research. A clinical interview for GAD was conducted during a telephone meeting, where individuals were assessed based on specific entry and exit criteria. Those who met the criteria and expressed their willingness were invited to take part in the research.
In addition, these individuals received the necessary information regarding the study’s overall goals, advantages, disadvantages, research process, and duration. This ensured that they could make an informed decision about their participation. A total of 60 individuals were chosen for the investigation. Following the research design and using random assignment, the participants were divided into two groups: The control group (n=17) and the experimental group (n=17). Subsequently, a pre-test was administered, and all participants completed a series of questionnaires. The participants also completed a written consent form to indicate their willingness to participate in the research alongside the pre-test.
In the next step, individuals from the first experimental group (Table 1) underwent a 10-session therapy program based on ACT, as outlined by Hayes et al. (2012).
For the second experimental group, a 10-session program of MCT (developed by Wells in 2010) was implemented individually (Table 2). The control group had regular contact with the tester but received no specific active treatment. These therapy sessions took place at the Taliee Clinical Psychology Center and were administered by a PhD candidate in psychology. After the final counseling session, a post-test was conducted for all experimental and control group participants. Additionally, a follow-up phase occurred two months later. To uphold ethical principles, individuals in the control group who desired professional assistance received GAD treatment after completing the study. Figure 1 displays the consolidated standards of reporting trials flow diagram.
Research instruments were used to evaluate all participants during the pre-test and post-test stages.
Research instruments
Research-made demographic questionnaire
A researcher-made demographic was used to determine the participant’s age, education, occupation, and marital status.
Generalized anxiety disorder short scale
The scale developed by Spitzer et al. (2006) consists of 7 primary questions and 1 additional question to assess the level of impairment in various aspects of the individual’s life, including social, family, and occupational functioning. Each item was scored using a Likert scale with 4 options ranging from never to almost every day. The seven main questions of the generalized anxiety scale evaluate the mental state and difficulties experienced by the respondent over the past two weeks. Each question is assigned a score from 0 to 3, resulting in a total score range of 0 to 21. Regarding internal consistency, the Iranian scale version demonstrated good reliability with a Cronbach α value of 0.876 (Omani-Samani et al., 2018).
Ryff scales of psychological well-being
The researchers utilized the 42-item version of the Ryff scales of psychological well-being to measure psychological well-being. This index is widely used and focuses on eudaimonic well-being, encompassing various aspects, such as autonomy, environmental mastery, personal growth, positive relationships, purpose in life, and self-acceptance. An example item from this scale is as follows: “I feel a sense of purpose and direction in my life.” Ryff’s measure possesses factorial validity, high internal consistency, and high criterion-related validity. In a previous study, the Persian version of this measure achieved a Cronbach α of 0.89 (Aghababaei et al., 2016), while the short 18-item version obtained the same α value (Varaee et al., 2018). In the present study, the Persian versions of these scales exhibited Cronbach α values that ranged from 0.57 to 0.81. The survey packages used for data collection contained the Persian adaptations of the measures above and were administered to various classroom groups. The participants provided informed consent before answering demographic questions and completing the measures described earlier.
All procedures adhered to the ethical guidelines of the respective institution for research involving human subjects.
Statistical analyses
An analysis of variance of the repeated measure with a within-group effect was utilized to examine the impact of acceptance and commitment treatments and MCT on the scores of psychological well-being components in the pre-test, post-test, and follow-up periods. Initially, the hypothesis of the homogeneity of the variables was assessed to investigate the mean difference between the mean components of psychological well-being in the three groups at the three treatment stages. The normality of the data was tested using the Shapiro-Wilk test, and the significance threshold for each research variable was found to be above 0.05, indicating that parametric tests can be employed. Additionally, the Levene test was conducted to verify the equality of variance in groups, assuming all variables’ variances are equal (P>0.05). The obtained data were subjected to statistical analysis using the SPSS software, version 25, at a 0.05 significance level.
Results
The Mean±SD of the age of women with GAD was 44.23±5.32. Demographic variables of women with this disorder are presented in Table 3. The results of the Kruskal–Wallis showed no significant difference in the age (P=0.78) and education level (P=0.57) of the three groups.
The test of sphericity to check the homogeneity of covariance was not established (P>0.05). Accordingly, the greenhouse–Geisser test is used in the hypothesis test to obtain a more accurate approximation, and the results of the within-group analysis of variance are calculated using the lack of the sphericity assumption (Table 4).
According to the results of Table 5, the difference between the scores of the psychological well-being components in the three study periods is significant (P<0.01). Furthermore, the mean autonomy scores and psychological well-being exhibited considerable discrepancies within the two analyzed groups (P<0.01). In addition, the interaction between research stages and group membership was also significant in the variables of autonomy and psychological well-being (P<0.01). In other words, the difference between autonomy scores and psychological well-being in the three study periods in the two experimental groups was significant. Therefore, it can be concluded that metacognitive therapy and acceptance and commitment therapy have different effects on improving autonomy and psychological well-being. The results show a significant difference in autonomy and psychological well-being levels in the pre-test, post-test, and follow-up periods.
The results of Table 6 show that the difference between the pre-test and the two post-test and follow-up stages in the two experimental groups is significant (P<0.01). 0.55 Also, the difference between the post-test and follow-up scores in the two groups of MCT and therapy based on ACT is significant, showing the treatment effect’s greater effectiveness and stability in the therapy group based on ACT (P<0.05).
Discussion
This study determined whether ACT or MCT could improve the psychological well-being of women diagnosed with GAD. In contrast to MCT, ACT demonstrated notable superiority, and its positive outcomes endured for an extended period in the follow-up phase.
Consistent with the findings of this study, Eqharari et al., 2019; Sharif Ara et al., 2023; Demehri et al. 2019, and Mani et al., 2019 confirmed the effectiveness of ACT.
According to the results of multivariate analysis of covariance, ACT treatment has a positive effect on self-acceptance, positive relationships with others, autonomy, purposeful life, and overall psychological well-being and sexual function scores. The results also showed that ACT treatment had no significant effect on the components of environmental dominance and individual growth. According to repeated measures analysis of variance, the effect of ACT treatment has been effective on psychological well-being, including total psychological well-being and sexual performance, as well as on self-acceptance, positive relationships with others, and purposeful life (Hasanzadeh et al., 2019). ACT is a distinct form of behavioral and cognitive therapy that places significant emphasis on the context of behavior (Hayes et al., 2013; Whiting et al., 2017). It builds upon a relational frame model that connects behavioral principles to psychological issues and positive behavior (Hayes et al., 2013; Whiting et al., 2017). The primary goal of ACT is to optimize human potential and enable individuals to lead a fulfilling and meaningful life (White et al., 2021). Within ACT, experiential acceptance or mindfulness is a fundamental process closely linked to well-being (Eadeh et al., 2023). Furthermore, ACT places great importance on fostering valued or engaged living. Making committed choices and pursuing goals that align with intrinsic values and motivations has been identified as a predictor of well-being (Assor et al., 2020). The ability to live mindfully, accept current experiences, and act under one’s core values is psychological flexibility (Katajavuori et al., 2023).
In contrast to prior research, this study revealed varying outcomes regarding how much MCT enhances psychological well-being. Research has consistently shown that MCT is a highly effective approach (Wells, 2010; Normann & Morina, 2018; Haseth et al., 2019; Callesen et al., 2019; Mikaeili, 2022; Strand et al., 2023).
Wells and Matthews (1996) introduced an earlier trans-diagnostic approach known as the self-regulatory executive function model, which proposes universal psychological factors across various pathologies. They argued that psychological disorders are sustained by a common maladaptive cognitive attentional syndrome that should be the focus of treatment (Callesen et al., 2019). An increased focus on oneself characterizes the CAS, repetitive negative thinking involving worry and rumination, and unhelpful coping strategies and behaviors such as monitoring threats, suppressing thoughts, and avoiding situations (Strand et al., 2023). This syndrome results from an individual’s metacognitive beliefs, which result in prolonged negative processing and subsequent distress. There are two types of metacognitive beliefs as follows: Negative metacognitive beliefs and positive metacognitive beliefs. Negative metacognitive beliefs revolve around the idea that worry is uncontrollable and dangerous (for example, “I have no control over my worries” or “My worries can harm me”). On the other hand, positive metacognitive beliefs emphasize the usefulness of worry (for instance, “Worrying helps me cope,” or “If I worry, I’ll be prepared”). These underlying metacognitive beliefs play a significant role in driving the CAS. MCT, developed based on this model, eliminates the CAS and modifies positive and negative metacognitive beliefs (Wells, 2010).
While these two approaches were first applied to the psychological well-being of women with generalized anxiety, in contrast to the strong background in favor of MCT treatment, most previous studies compared ACT treatment with other treatments, and both showed results in favor of the ACT. For example, a study comparing the effect of commitment-based acceptance and treatment and a mindfulness-based stress reduction program on work attitudes, health-related anxiety, psychological well-being, and body image showed that ACT is more effective than a mindfulness-based stress reduction program (Pasyar et al., 2023). In addition, the study was conducted to compare the effect of acceptance and commitment therapy and metacognition therapy on the recovery of women on dialysis. Both treatments improve the endurance of patients on hemodialysis (Tajbakhsh et al., 2023). Ahmadi et al. (2022) have shown that ACT and MCT are effective in increasing adaptive cognitive emotion regulation strategies and decreasing cognitive emotional regulation strategies. Furthermore, the results suggest that ACT is more effective than MCT in modulating cognitive-emotional regulation strategies (Ahmadi et al., 2022). Instead of teaching better and better strategies to change or reduce unwanted thoughts and emotions, ACT teaches patients skills to perceive and observe unpleasant thoughts and emotions as they are (Yasaie Sokeh et al., 2017).
Conclusion
Women with GAD benefited from therapy courses in terms of psychological well-being. Thus, unlike the MCT, the results suggest that ACT-based exercises would be of additional value for improving psychological well-being. As this is the first study on the topic, more research is needed to determine the effectiveness of these two therapies for general anxiety in individuals.
Study limitations
There are limitations to the study. Initially, a small sample size and nonrandom sampling put the validity of our findings at risk. Our results may have been influenced by recall bias and answer accuracy due to the use of self-report instruments. Despite our efforts to control extraneous variables statistically, there may have been additional effects of subject variables that we overlooked, such as comorbid physical conditions that could contribute to anxiety symptoms. Therefore, we recommend that future studies consider these variables as exclusion criteria.
Furthermore, since our sample consisted of individuals with mild anxiety symptoms, it is possible that different results would be observed at different severity stages of anxiety disorders. Additionally, the cross-sectional design of this study cannot determine a cause-and-effect relationship for the observed associations. Future studies should employ longitudinal designs to examine changes in mindfulness and metacognitions over time and identify causal predictors of anxiety disorder symptom severity. Finally, it would have been preferable to assess mindfulness and metacognition in individuals with anxiety disorders who are not undergoing pharmacological or non-pharmacological treatment to avoid the potential effects of these treatments on symptom severity.
Ethical Considerations
Compliance with ethical guidelines
The study was approved by the Ethics Committee of Islamic Azad University, Semnan Branch (Code: IR.IAU.SHAHROOD.REC.1401.058).
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest
Acknowledgments
The authors would like to thank everyone who participated in the research.
References
Abdollahi, S. M., Rafiepoor, A., & Sabet, M. (2020). The effectiveness of acceptance and commitment therapy on mental health, hopefulness and meaningfulness in people with cardiovascular disease. Iranian Journal of Health Psychology, 3(1), 61-70. [DOI:10.30473/ijohp.2020.50883.1069]
Aghababaei, N., Błachnio, A., Arji, A., Chiniforoushan, M., Tekke, M., & Fazeli Mehrabadi, A. (2016). Honesty-humility and the HEXACO structure of religiosity and well-being. Current Psychology, 35, 421-426. [DOI:10.1007/s12144-015-9310-5]
Ahmadi Roghabadi, A., Bagherzadeh Golmakani, Z., Akbarzade, M., Mansouri, A., & Khodabakhsh, M. (2022). [Comparison of the effectiveness of acceptance and commitment therapy and metacognitive therapy on adaptive and maladaptive strategies of cognitive emotion regulation in patients with substance use disorder undergoing methadone maintenance treatment (Persian)]. Research in Clinical Psychology and Counseling, 12(1), 60-78. [DOI:10.22067/TPCCP.2022.70654.1118]
Assor, A., Soenens, B., Yitshaki, N., Ezra, O., Geifman, Y., & Olshtein, G. (2020). Towards a wider conception of autonomy support in adolescence: The contribution of reflective inner-compass facilitation to the formation of an authentic inner compass and well-being. Motivation and Emotion, 44, 159-174. [DOI:10.1007/s11031-019-09809-2]
Azkhosh, M., Farhoudianm, A., Saadati, H., Shoaee, F., & Lashani, L. (2016). Comparing acceptance and commitment group therapy and 12-steps narcotics anonymous in addict’s rehabilitation process: A randomized controlled trial. Iranian Journal of Psychiatry, 11(4), 244. [PMID]
Callesen, P., Capobianco, L., Heal, C., Juul, C., Find Nielsen, S., & Wells, A. (2019). A preliminary evaluation of transdiagnostic group metacognitive therapy in a mixed psychological disorder sample. Frontiers in Psychology, 10, 1341. [DOI:10.3389/fpsyg.2019.01341] [PMID]
Chaturvedi, S. K., Manche Gowda, S., Ahmed, H. U., Alosaimi, F. D., Andreone, N., & Bobrov, A., et al. (2019). More anxious than depressed: Prevalence and correlates in a 15-nation study of anxiety disorders in people with type 2 diabetes mellitus. General Psychiatry, 32(4), e100076. [DOI:10.1136/gpsych-2019-100076] [PMID]
Daryadel, J., Mikaeili, N., Atadokht, A., & Molavi, P. (2022). The efficacy of metacognitive therapy based on detached mindfulness on meta-worry and interpersonal cognitive distortion in women with postpartum depression. Journal of Psychologicalscience, 21(110), 349-366. [DOI:10.52547/JPS.21.110.349]
Demehri, F., Saeedmanesh, M., & Jala, N. (2018). [The effectiveness of acceptance and commitment therapy (ACT) on rumination and well-being in adolescents with general anxiety disorder (Persian)]. Journal of Disability Studies, 8, 25. [Link]
Eadeh, H. M., Adamowicz, J. L., Markon, K., & Thomas, E. B. K. (2023). Using network analysis to examine connections between Acceptance and Commitment Therapy (ACT) processes, internalizing symptoms, and well-being in a sample of undergraduates. Journal of Affective Disorders, 320, 701-709. [DOI:10.1016/j.jad.2022.10.004] [PMID]
Eqharari, L., Asadi, F., Javazi, S., & Vahid, T. (2019). [Effectiveness of Acceptance and Commitment (ACT) therapy on behavioral inhibition and cognitive-behavioral avoidance of women with generalized anxiety disorder (Persian)]. Iranian Journal of Nursing Research, 13(6), 31-38. [Link]
Faraci, P., Bottaro, R., Valenti, G. D., & Craparo, G. (2022). Psychological well-being during the second wave of COVID-19 pandemic: The mediation role of generalized anxiety. Psychology Research and Behavior Management, 15, 695–709. [DOI:10.2147/PRBM.S354083] [PMID]
Hasanzadeh, M., Akbari, B., & Abolghasemi, A. (2019). [Efficiency of acceptance and commitment therapy on psychological well-being and sexual function in women with infertility history (Persian)]. Avicenna Journal of Nursing and Midwifery Care, 27(4), 250-259. [DOI:10.30699/ajnmc.27.4.250]
Haseth, S., Solem, S., Sørø, G. B., Bjørnstad, E., Grøtte, T., & Fisher, P. (2019). Group metacognitive therapy for generalized anxiety disorder: A pilot feasibility trial. Frontiers in Psychology, 10, 290. [DOI:10.3389/fpsyg.2019.00290] [PMID]
Hayes, S. C., Levin, M. E., Plumb-Vilardaga, J., Villatte, J. L., & Pistorello, J. (2013). Acceptance and commitment therapy and contextual behavioral science: Examining the progress of a distinctive model of behavioral and cognitive therapy. Behavior Therapy, 44(2), 180-198. [DOI:10.1016/j.beth.2009.08.002] [PMID]
Hayes, S. C., Pistorello, J., & Levin, M. E. (2012). Acceptance and commitment therapy as a unified model of behavior change. The Counseling Psychologist, 40(7), 976-1002. [DOI:10.1177/0011000012460836]
Hossein Nazari, N., Nejat, H., & Saffarian Tosi, M. (2022). [The comparison of the effectiveness of well‐being therapy with acceptance and commitment therapy on death anxiety in the elderly (Persian)]. Aging Psychology, 8(1), 25-38. [Link]
Iani, L., Quinto, R. M., Lauriola, M., Crosta, M. L., & Pozzi, G. (2019). Psychological well-being and distress in patients with generalized anxiety disorder: The roles of positive and negative functioning. PloS One, 14(11), e0225646. [DOI:10.1371/journal.pone.0225646] [PMID]
Katajavuori, N., Vehkalahti, K., & Asikainen, H. (2023). Promoting university students’ well-being and studying with an acceptance and commitment therapy (ACT)-based intervention. Current Psychology, 42(6), 4900-4912. [DOI:10.1007/s12144-021-01837-x]
Köcher, L. M., Schneider, K., & Christiansen, H. (2021). Thinking about worry: A systematic review and meta-analysis on the assessment of metacognitions in children and adolescents. World Journal of Psychiatry, 11(9), 635. [DOI: 10.5498/wjp.v11.i9.635] [PMID]
LaFreniere, L. S., & Newman, M. G. (2020). Exposing worry’s deceit: Percentage of untrue worries in generalized anxiety disorder treatment. Behavior Therapy, 51(3), 413-423. [DOI:10.1016/j.beth.2019.07.003] [PMID]
LeardMann, C. A., McMaster, H. S., Warner, S., Esquivel, A. P., Porter, B., & Powell, T. M., et al. (2021). Comparison of posttraumatic stress disorder checklist instruments from diagnostic and statistical manual of mental disorders, fourth edition vs fifth edition in a large cohort of US Military Service Members and Veterans. JAMA Network Open, 4(4), e218072. [PMID]
Li, J., Xia, Y., Cheng, X., & Li, S. (2020). Fear of uncertainty makes you more anxious? Effect of intolerance of uncertainty on college students’ social anxiety: A moderated mediation model. Frontiers in Psychology, 11, 565107. [DOI:10.3389/fpsyg.2020.565107] [PMID]
Luo, X., Tong, S., Fang, Z., & Qu, Z. (2019). Frontiers: Machines vs. humans: The impact of artificial intelligence chatbot disclosure on customer purchases. Marketing Science, 38(6), 937-947. [DOI:10.1287/mksc.2019.1192]
Mani, A., Mehdipour, Z., Ahmadzadeh, L., Tahmasebi, S., Khabir, L., & Mosalaei, A. (2019). The effectiveness of group acceptance and commitment psychotherapy on psychological well-being of breast cancer patients in Shiraz, Iran. Middle East Journal of Cancer, 10(3), 231-238. [DOI:10.30476/mejc.2019.45316]
McEvoy, P. M. (2019). Metacognitive therapy for anxiety disorders: A review of recent advances and future research directions. Current Psychiatry Reports, 21(5), 29. [DOI:10.1007/s11920-019-1014-3] [PMID]
Mohammadi, H., Khalatbari, J., & Abolmaali, K. (2021). The effect of integrating cognitive-behavioral therapy and mindfulness therapy on lifestyle of women with irritable bowel syndrome. Women’s Health Bulletin, 8(4), 220-227. [DOI:10.30476/whb.2021.91397.1124]
Montazernia, B., Kooshki, S., Oraki, M., & Mirzaian, B. (2021). Comparing The Efficacy of Acceptance and Commitment Therapy (ACT) and Dialectical Behavior Therapy Skills Training (DBT-ST) on cognitive emotion regulation in patients with type II Diabetes. Iranian Journal of Health Psychology, 4(1), 33-48. [Link]
Normann, N., & Morina, N. (2018). The efficacy of metacognitive therapy: A systematic review and meta-analysis. Frontiers in Psychology, 9, 2211. [DOI:10.3389/fpsyg.2018.02211] [PMID]
Omani-Samani, R., Ghaheri, A., Navid, B., Sepidarkish, M., & Maroufizadeh, S. (2018). Prevalence of generalized anxiety disorder and its related factors among infertile patients in Iran: A cross-sectional study. Health and Quality of Life Outcomes, 16(129), 1-5. [Link]
Pasyar, S., Baghooli, H., Barzegar, M., & Sohrabi, N. (2023). [Comparing the effectiveness of acceptance and commitment therapy and mindfulness-based stress reduction program on negative feedback, health anxiety, psychological well-being, and body image in women undergoing mastectomy (Persian)]. Psychological Achievements, 30(1), 285-314. [DOI:10.22055/psy.2023.43119.2969]
Sharif Ara, B., Khosropour, F., & Molayi Zarandi, H. (2023). Effectiveness of Acceptance and Commitment Therapy (ACT) on emotional processing, irrational beliefs and rumination in patients with generalized anxiety disorder. Journal of Adolescent and Youth Psychological Studies, 4(4), 34-44. [Link]
Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092-1097. [DOI:10.1001/archinte.166.10.1092] [PMID]
Strand, E. R., Veium, L. T., Engvik, L. S., & Nordahl, H. (2023). Generic group metacognitive therapy for patients with major depressive disorder and related problems: A preliminary evaluation in specialized mental health care. International Journal of Cognitive Therapy, 16, 497–509. [DOI:10.1007/s41811-023-00175-z]
Tajbakhsh, R., Haddadi, S., Zeighami Mohammadi, S., Malihi Alzakerini, S., & Borumand, M. (2023). [Comparison of the effect of “acceptance and commitment therapy” and “metacognitive therapy” on the resilience of women undergoing hemodialysis (Persian)]. Journal of Health Promotion Management, 12(3), 82-94. [Link]
Takebayashi, Y., Tanaka, K., Sugiura, Y., & Sugiura, T. (2018). Well-being and generalized anxiety in Japanese undergraduates: a prospective cohort study. Journal of Happiness Studies, 19, 917-937. [DOI:10.1007/s10902-017-9852-3]
Varaee, P., Momeni, K., & Moradi, A. (2018). The prediction of psychological well-being based on death anxiety and self-compassion in the Elderly. International Journal of Behavioral Sciences, 12(1), 18-24. [Link]
Weisman, J. S., & Rodebaugh, T. L. (2018). Exposure therapy augmentation: A review and extension of techniques informed by an inhibitory learning approach. Clinical Psychology Review, 59, 41-51. [DOI:10.1016/j.cpr.2017.10.010] [PMID]
Wells, A. (1995). Meta-cognition and worry: A cognitive model of generalized anxiety disorder. Behavioural and Cognitive Psychotherapy, 23(3), 301-320. [DOI:10.1017/S1352465800015897]
Wells, A. (2010). Metacognitive theory and therapy for worry and generalized anxiety disorder: Review and status. Journal of Experimental Psychopathology, 1(1), jep-007910. [DOI:10.5127/jep.007910]
Wells, A., & Matthews, G. (1996). Modelling cognition in emotional disorder: The S-REF model. Behaviour Research and Therapy, 34(11-12), 881-888. [DOI:10.1016/S0005-7967(96)00050-2]
White, R. G., Bethell, A., Charnock, L., Leckey, S., & Penpraze, V. (2021). Acceptance and commitment approaches for athletes’ wellbeing and performance. Cham: Palgrave Macmillan. [DOI:10.1007/978-3-030-64942-5]
Whiting, D. L., Deane, F. P., Simpson, G. K., McLeod, H. J., & Ciarrochi, J. (2017). Cognitive and psychological flexibility after a traumatic brain injury and the implications for treatment in acceptance-based therapies: A conceptual review. Neuropsychological Rehabilitation, 27(2), 263-299. [DOI:10.1080/09602011.2015.1062115] [PMID]
Wroblewski, A., Hollandt, M., Yang, Y., Ridderbusch, I. C., Pietzner, A., & Szeska, C., et al. (2022). Sometimes I feel the fear of uncertainty: How intolerance of uncertainty and trait anxiety impact fear acquisition, extinction and the return of fear. International Journal of Psychophysiology, 181, 125-140. [DOI:10.1016/j.ijpsycho.2022.09.001] [PMID]
Yasaie Sokeh, M., Shafiabadi, A., & Farzad, V. (2017). Comparison of the efficacy of acceptance and commitment group therapy (ACT) with mindfulness-based cognitive therapy (MBCT) on hemodialysis patients in terms of anxiety and depression. Journal of Fundamentals of Mental Health, 19(special issue), 317-324. [DOI:10.22038/JFMH.2017.9127]
Type of Study: Original Research Article |
Subject:
Rehabilitation
Received: 2023/08/22 | Accepted: 2023/10/23 | Published: 2024/04/1
Received: 2023/08/22 | Accepted: 2023/10/23 | Published: 2024/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |