Volume 12, Issue 1 (Winter 2024)
PCP 2024, 12(1): 33-42 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mohammadkhani S, Akbarian Firoozabadi M, Akbari M, Nasiri M. Metacognitions About Health and COVID-19 Preventive Behaviors: Experiential Avoidance and Coronavirus Anxiety as Mediators. PCP 2024; 12 (1) :33-42
URL: http://jpcp.uswr.ac.ir/article-1-868-en.html
URL: http://jpcp.uswr.ac.ir/article-1-868-en.html
1- Department of Clinical Psychology, Faculty of Psychology, Kharazmi University, Tehran, Iran. , mohammadkhani@khu.ac.ir
2- Department of Clinical Psychology, Faculty of Psychology, Kharazmi University, Tehran, Iran.
2- Department of Clinical Psychology, Faculty of Psychology, Kharazmi University, Tehran, Iran.
Full-Text [PDF 688 kb]
(901 Downloads)
| Abstract (HTML) (2488 Views)
Full-Text: (662 Views)
Introduction
According to the World Health Organization (WHO, 2020), coronavirus disease 2019 (COVID-19) has spread rapidly worldwide since late March 2020 (WHO, 2020). Following the prevalence of this disease and no reliable evidence regarding the most effective interventions for the treatment, COVID-19 preventive behaviors are essential to reduce the transmission rate. Accordingly, promoting adherence to public health mandates can lessen the prevalence of the disease (Shaw et al., 2020). Performing preventive behaviors, whether at the national or individual level, is highly needed to stop the virus’s transmission (Kim & Kim, 2020; Nguyen et al., 2020). Important COVID-19 preventive behaviors, such as wearing a mask, staying home, washing hands regularly &, etc., are activities toward promoting health that can be done individually and voluntarily (Mao, 2011).
Preventive behaviors toward COVID-19 are strongly related to cognitive and affective variables (Shen et al., 2021). A critical phenomenon is called metacognition which is in charge of the way cognitions and emotions act (Wells, 2011). In detail, metacognition is the knowledge or cognitive activity controlling and regulating cognition (Wells, 2011). It consists of sets of beliefs that a person has about the efficacy of thoughts (Wells, 2011). In the metacognitive model, individuals are caught in the trap of negative emotions and negative beliefs when their metacognition leads them to use a specific response pattern (Wells, 2011). They can lead to inflexible, maladaptive, and repetitive beliefs about thoughts and emotions, known as cognitive attentional syndrome (CAS) (Wells & Matthews, 1996). CAS controls thoughts through positive (e.g. worry helps me to deal with difficulties) and negative (e.g. my thoughts are uncontrollable and can make me crazy) metacognitive beliefs (Wells, 2011). One of the areas where the presence and function of metacognition are necessary is health anxiety (HA). Metacognition is correlated with HA and can predict its symptoms successfully (Bailey & Wells, 2013, 2015). Accordingly and as a result, Bailey and Wells (2015) investigated specific metacognition which is related to health anxiety. In this study, we focus on this specific type of metacognition.
Metacognition stimulates coping responses when facing an actual or perceived crisis, and they are related to anxiety and also the quality of life in individuals with chronic conditions as it increases distress decreases treatment adherence, and disrupts patients’ copying functions (Lenzo et al., 2020). Therefore, metacognitions seem to have the ability to lead an individual to remain in a pattern of behaviors increasing exposure to the COVID-19 infection (González-Castro et al., 2021); however, the information about this process, which may be either direct or indirect, is not sufficient. Although there is research on the relationship between cognition and preventive behaviors (Clancy et al., 2016), the relationship between metacognition and preventive behaviors has not yet been clarified, so we aimed to fill this gap with our study.
Additionally, anxiety can play a vital role in preventive behaviors. Previous studies have shown that a moderate level of anxiety (Riad et al., 2020) may increase the adoption of preventive behaviors, such as keeping social distance, washing hands, and wearing a mask (Cowling et al., 2020; Tyrer et al., 2011). On the other hand, this anxiety can change the behavior of an affected person and health service providers (Barsky et al., 2001; Fink et al., 2010) and decrease acceptance of suggested preventive behaviors (Ştefănuţ et al., 2021). We see that anxiety can lead to health impairing or protective behaviors (Asmundson & Taylor, 2020; Taylor, 2022). Considering these contradictory findings about the effects of anxiety, we need to investigate its relationship with preventive behaviors.
Another factor relating to one’s health is called experiential avoidance (Machell et al., 2015). Some studies on the relationship between experiential avoidance and diseases or behaviors have shown that it is significantly associated with high-risk health behaviors (Keinonen et al., 2021). Experiential avoidance is a behavior aimed at changing the forms and the experiences of unpleasant events, memories, thoughts, and physical senses, resulting in many psychopathological symptoms (Hayes et al., 1996). This construct consists of two parts: Reluctance to contact personal experiences; and efforts to avoid painful experiences or events (Waltz & Hayes, 2010). It was shown that experiential avoidance could lead to engaging in problematic behaviors (Hayes et al., 1996; Hildebrandt & Hayes, 2012; Kingston et al., 2010). A study showed that individuals with high levels of experiential avoidance have lower self-efficacy in illness management (Chartier et al., 2010), which may, as a result, change how a person performs preventive behaviors (Fledderus et al., 2010). If we consider the occurrence of a disease crisis, such as COVID-19, as a painful event, the role of experiential avoidance in this process is noticeable. Therefore, we wanted to answer whether experiential avoidance, which disrupts the process of experiencing the COVID-19 crisis, affects preventive behaviors.
In contrast, it has been shown that experiential avoidance does not necessarily lead to aversive outcomes (Karademas et al., 2017). It may even provide better coping styles (Suls & Fletcher, 1985). However, interacting with illness-related mechanisms increases the possibility of adverse effects (Karademas et al., 2017). To our knowledge, there are no studies on the relationship between experiential avoidance and, specifically, COVID-19 preventive behaviors which need to be clarified. Furthermore, it has been shown that maladaptive metacognitions are positively and significantly associated with experiential avoidance (McEvoy et al., 2013). Align with the research mentioned earlier, we tried to investigate the interaction between experiential avoidance and metacognitions which may change preventive behaviors.
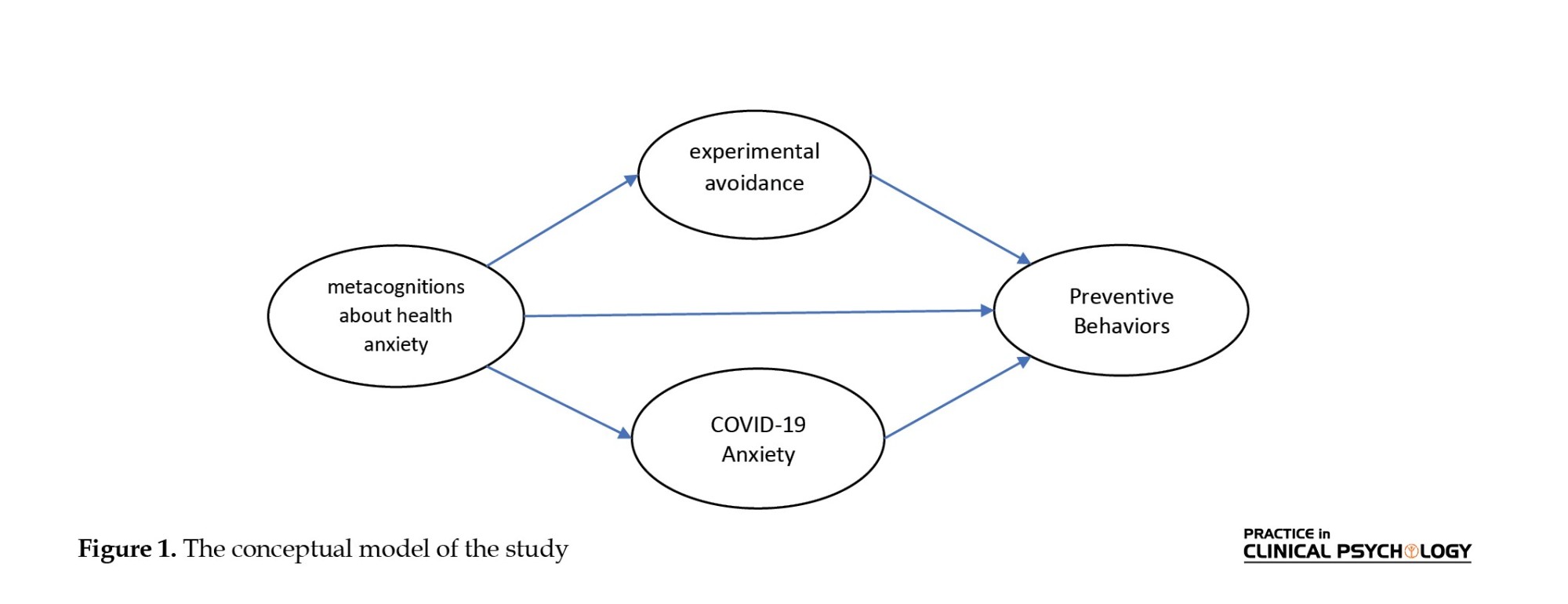
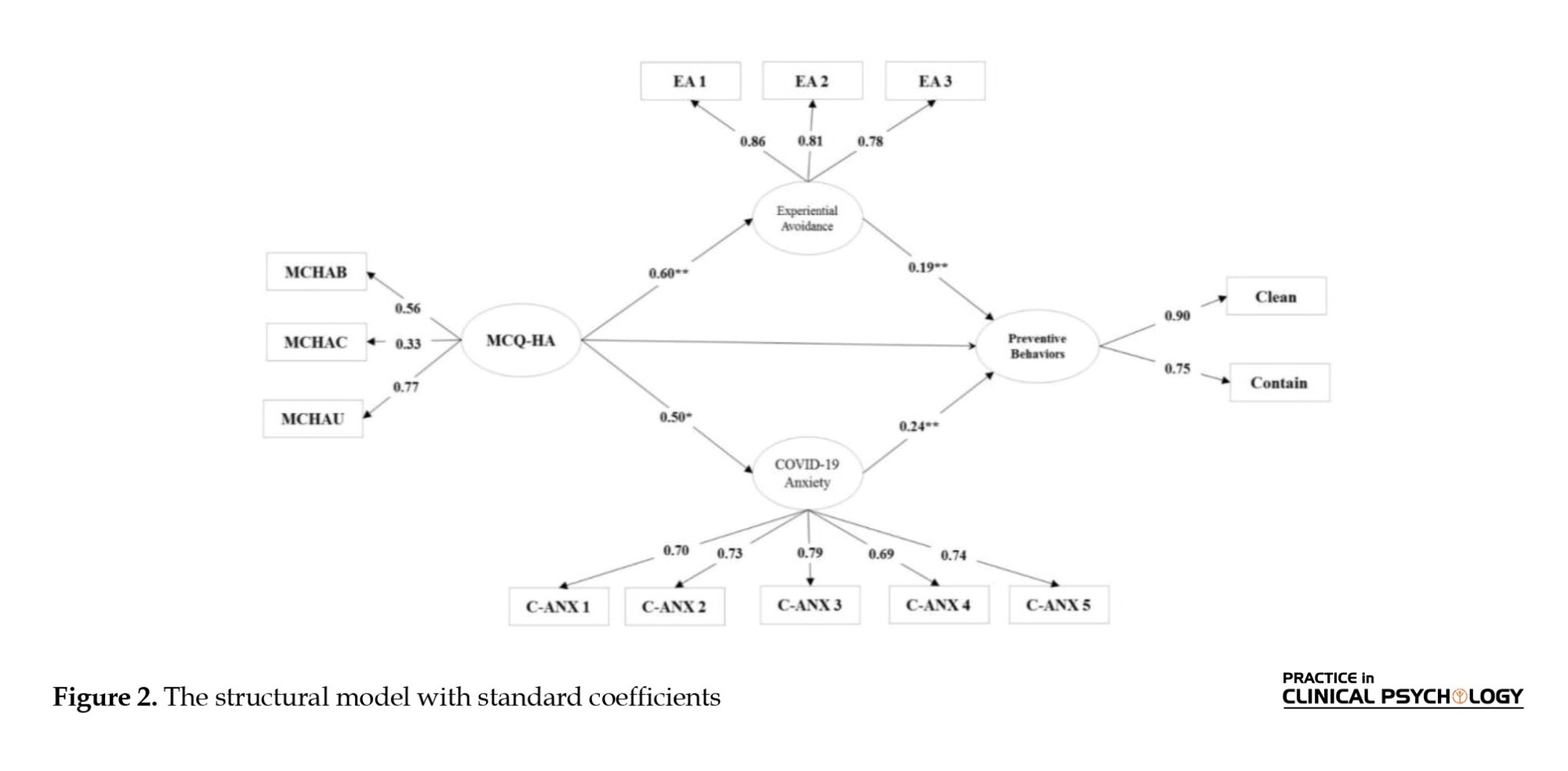
Altogether, crises like pandemics require extensive cooperation, and one of the most critical parts is individual preventive behaviors (Kim & Kim, 2020). Increasing such behaviors is vital in discontinuing the disease transmission cycle, even though many people have been fully vaccinated. Consequently, we targeted these behaviors as they should be followed even after getting vaccinated or in other contexts. Although metacognitions can help us analyze and understand many disorders’ behavioral, emotional, and cognitive psychopathology, there is not enough information about their direct or indirect effects on health-related behaviors, such as preventive behaviors (Lenzo et al., 2020). In conclusion, in this research, we answer whether health-related metacognition can change these behaviors and whether these changes are carried out with the mediating help of experiential avoidance or COVID-19 anxiety (Figure 1).
Materials and Methods
Procedure and participants
We distributed participation advertisements on Instagram and Facebook and gave a brief description of the study with a Google form link leading potential participants to consent forms and questionnaires. The ethics committee approved all the study procedures. Data were collected from November 3 to 14, 2021. Participants were recruited from the general population in Iran. The inclusion criteria were literacy, consent to participate in the research, and the age range of 18 to 60. Out of 963 invited individuals, 712 participated and completed the questionnaires, indicating a response rate of 73.93%. Ten data were excluded from the analysis due to incompleteness. After data deletion, data of 702 participants (61% female) were analyzed for the current study. According to the preferred sample size for structural equation modeling (SEM) analysis (min of 5 and max of 10 cases per estimated parameter), the required number of participants for this study with 35 items is 175-350, so our sample size seems adequate (Nunnally, 1967; Kim, 2015).
Measures
Socio-demographic form
A form for gathering information on variables such as age, gender, educational level, employment status, income, and criteria was made.
The metacognitions questionnaire -health anxiety (MCQ-HA)
The metacognition questionnaire-health anxiety (MCQ-HA) was developed by Baily and Wells (2015) to measure metacognition about health anxiety (Bailey & Wells, 2015). This scale consists of 14 items with a 4-point Likert scale ranging from 1 (“not agree”) to 4 (“very agree”). The total score of this questionnaire ranges from 14 to 56, with a higher score indicating higher levels of metacognitive beliefs associated with health anxiety. It consists of three subscales: (1) Beliefs that thoughts cause illness (MCQ‐HAC; e.g. “Thinking about illness can change my health.”); (2) Beliefs about biased thinking (MCQ‐HAB; e.g. “Thinking about the worst symptoms keeps me safe”); and (3) Beliefs that thoughts are uncontrollable (MCQ‐HAU; e.g. “Only if I have a diagnosis will I be able to stop worrying.”) A study has shown that this scale has good internal consistency and concurrent validity (Bailey & Wells, 2015). It is consistent with the Cronbach alpha reported (α=0.75) for its Persian version conducted by Mohammadkhani et al. (2022) and our study.
Coronavirus anxiety scale (CAS)
The coronavirus anxiety scale (CAS) is a valid, unidimensional scale developed by Lee (2020d) that assesses the physiological responses of dysfunctional fear and anxiety associated with the COVID-19 virus. This scale consists of five items (e.g. “I felt paralyzed or frozen when I thought about or was exposed to information about the coronavirus.”) Then, participants were assessed according to the 5-point scale (0=none / never, 4=almost every day for the past 2 weeks) on how often each anxiety symptom occurred (e.g. “I had trouble falling or staying asleep because I was thinking about the coronavirus.”) The total score of this questionnaire ranges from 0 to 20. This scale has acceptable internal consistency, reliability, structure, and concurrent validity. The Cronbach alpha of its Persian version was 0.79 in the study of Mohammadkhani et al. (2022). The cut score of this scale is ≥9, with 90% sensitivity and 85% specificity. The Cronbach alpha in the current study was 0.79.
Acceptance and action questionnaire (AAQ-2)
The acceptance and action questionnaire has been developed to examine psychological rigidity and experimental avoidance (Bond et al., 2011). It is a 7-item questionnaire using a 7-point Likert scale ranging from 1 (never) to 7 (always true). The total score of this questionnaire ranges from 7 to 49. Higher scores indicate higher levels of experiential avoidance. The Cronbach alpha has been reported as α=.93. Its Persian version has satisfactory internal consistency (0.71 to 0.89) and good test-retest reliability (Abasi et al., 2013). The Cronbach alpha of this questionnaire in this study was 0.85.
Preventive COVID-19 behaviors scale: the clean and contain measure
Considering the recommendations by the center for disease control (CDC) in March 2020, Toussaint et al. (2020) developed a 9-item, 5-Likert scale (from “not at all”: 1 to “always”: 5) to assess protective behaviors, including washing hands, keeping social distance, staying at home when feeling sick, respiratory exercises, and not touching eyes, nose, and mouth, against coronavirus infection over the past week. The total score of this questionnaire ranges from 9 to 45. A higher total score indicates a higher level of compliance with the CDC’s recommendations. The questionnaire has good internal consistency, α>84, and our results showed a satisfactory Cronbach alpha of .88 for its Persian version.
Data analysis
SPSS software, version 22, LISREL software, version 8.85, and MPlus software, version 7.4 statistical software were used to analyze the data and investigate the research hypotheses. Model fit for the modified hypothetical model was tested using structural equation modeling (SEM). Data analysis was performed using a two-stage approach (Anderson & Gerbing, 1988). First, confirmatory factor analysis (CFA) was used to evaluate the model fit of the modified model. The second step tested the hypothetical structural model using the SEM method.
Results
Descriptive statistics
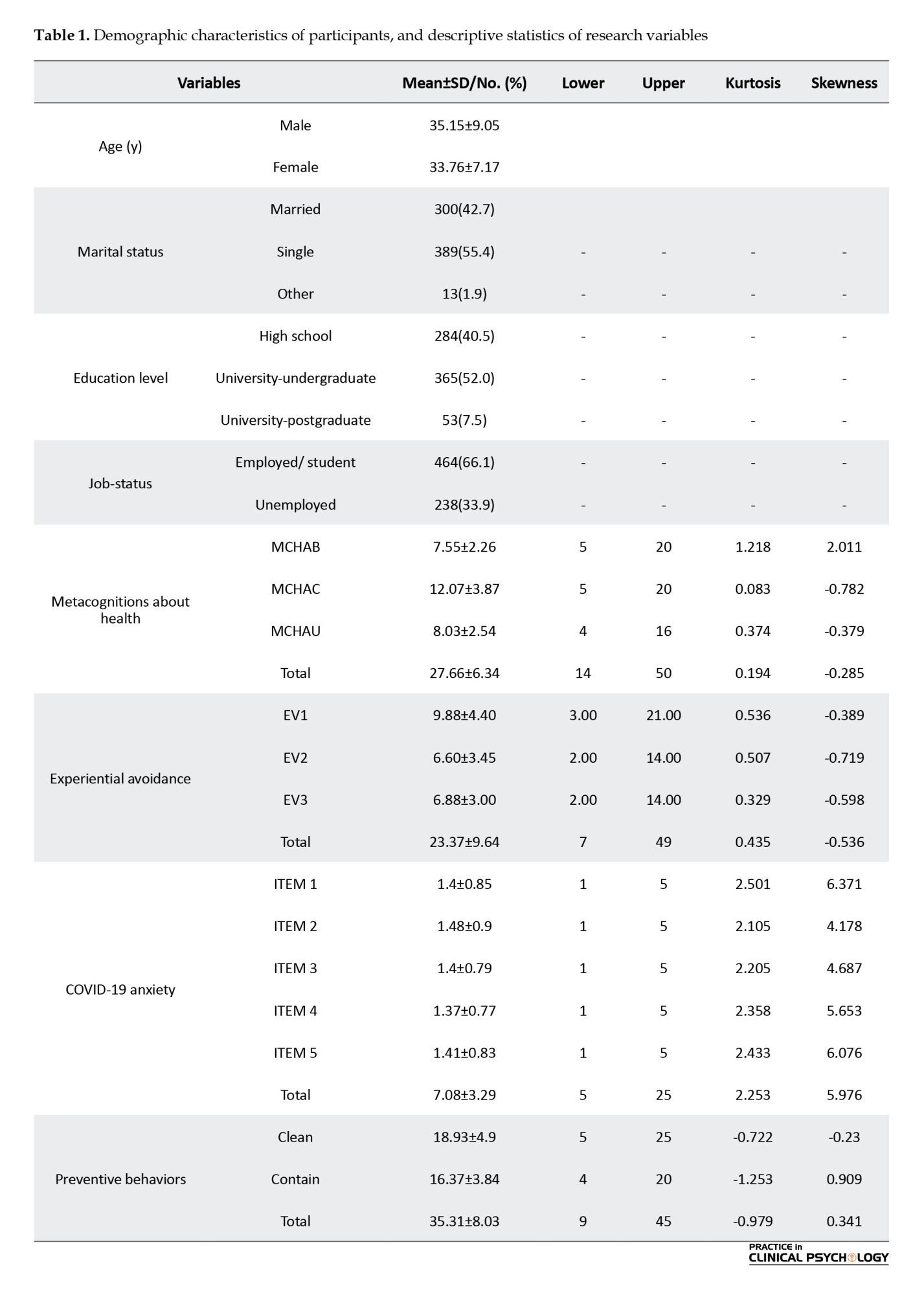
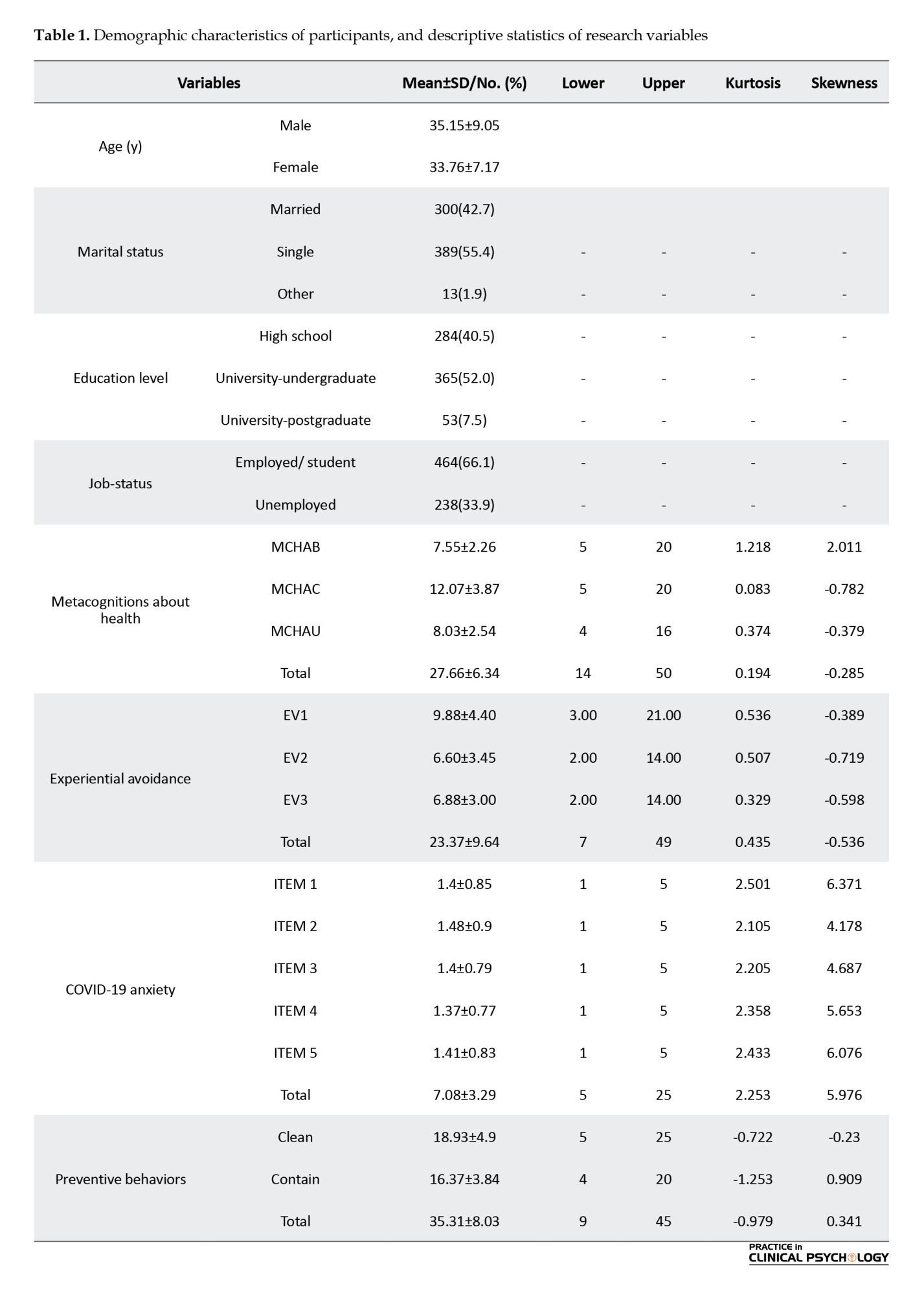
Participants’ characteristics are presented in Table 1. The final sample comprised 702 participants, 272 men (39%) and 430 women (61.%). Participants mean age was 35.15±9.05 and 33.76±17.17 for males and females, respectively. Also, in Table 1, descriptive indicators include the mean, standard deviation, kurtosis, and skewness of the research variables.
Structural equation modeling assumptions
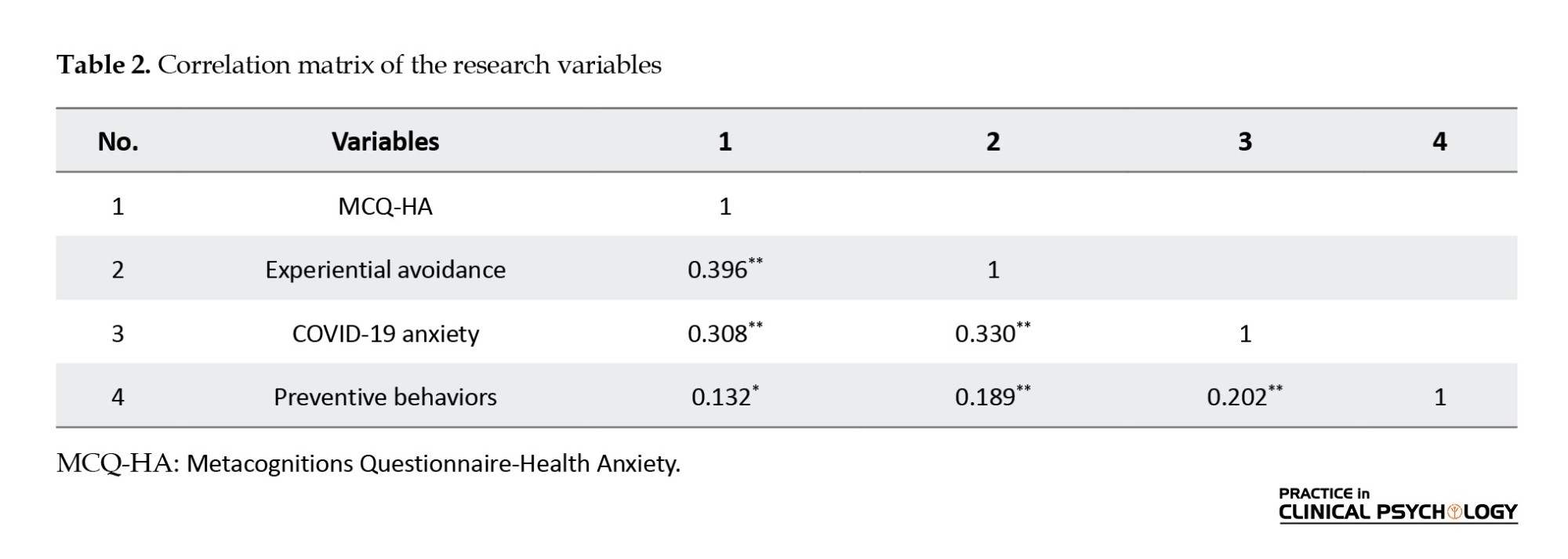
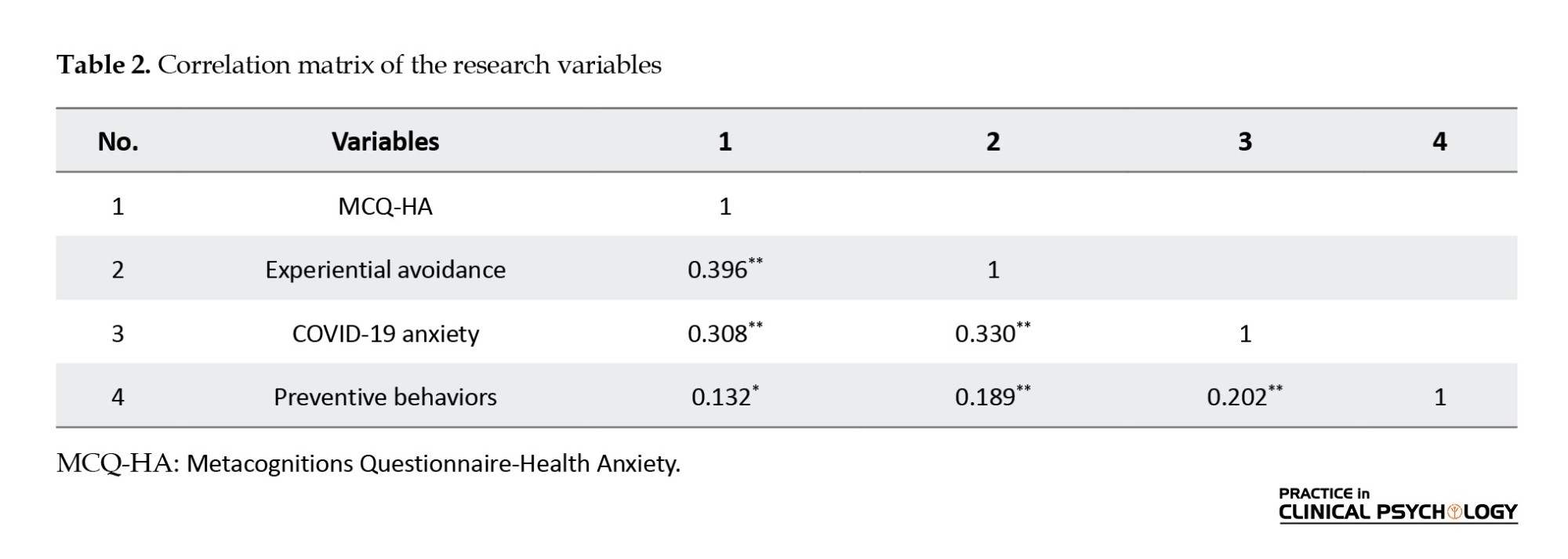
Before evaluating the structural model of the research, we examined SEM assumptions, which were confirmed. Also, the suitability of this statistical method for the present study was approved. One of the most important assumptions of this statistical approach is univariate and multivariate normality. To examine univariate normality, kurtosis, and skewness of the research variables are assessed. Kurtosis of the variables is in the range of 2.50 to -1.25, and their skewness is in the range of .782 to 6.371. For a suitable kurtosis, a cutting point of ±3 is considered satisfactory. A cutting point of skewness indicates that values more than ±10 are not acceptable (Kline, 2015). The relative multivariate skewness index, calculated to assess the hypothesis of multivariate normality, reached 1.320. To get multivariate normality, the value of this indicator should not be more than 3. The correlation matrix between evident variables can indicate the existence of multicollinearity between them. Accordingly, correlation coefficients above 0.85 can interrupt the estimation of the model (Kline, 2015). Correlation coefficients were in a range of -0.03 to 0.70. Preliminary analyses showed that data was suitable for structural equation modeling and the maximum estimation method. The matrix of correlations between the research variables and their mean and standard deviation are presented in Table 2. As this table shows, all correlations are moderate (.375≤ r≤0.502).
Measurement model (confirmatory factor analysis)
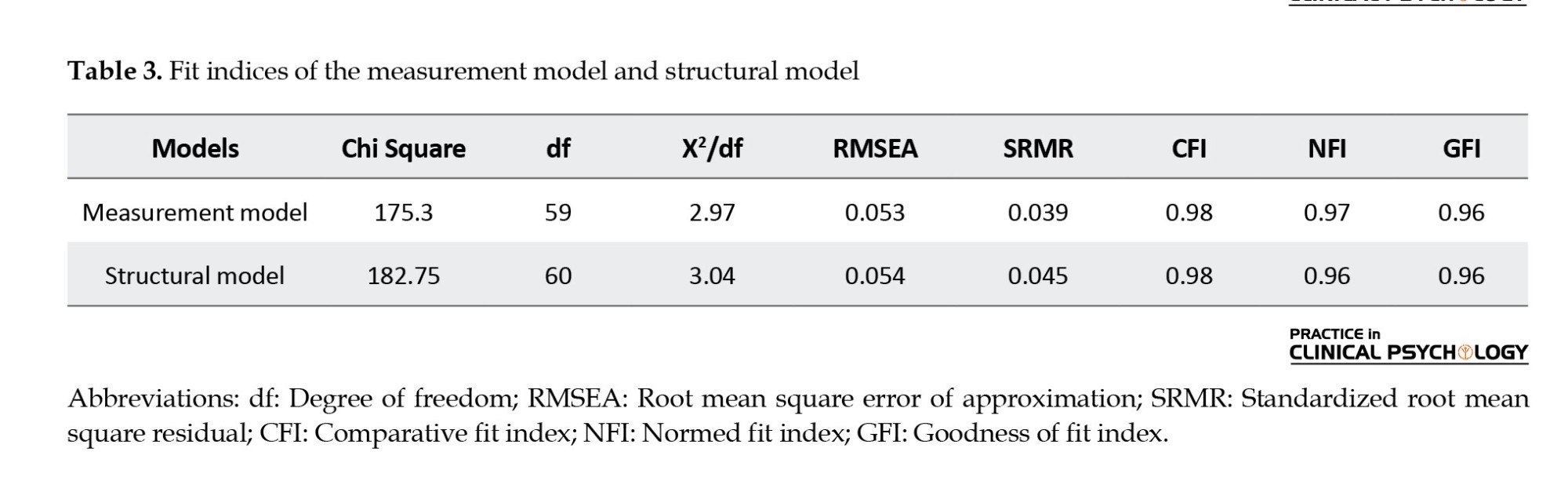
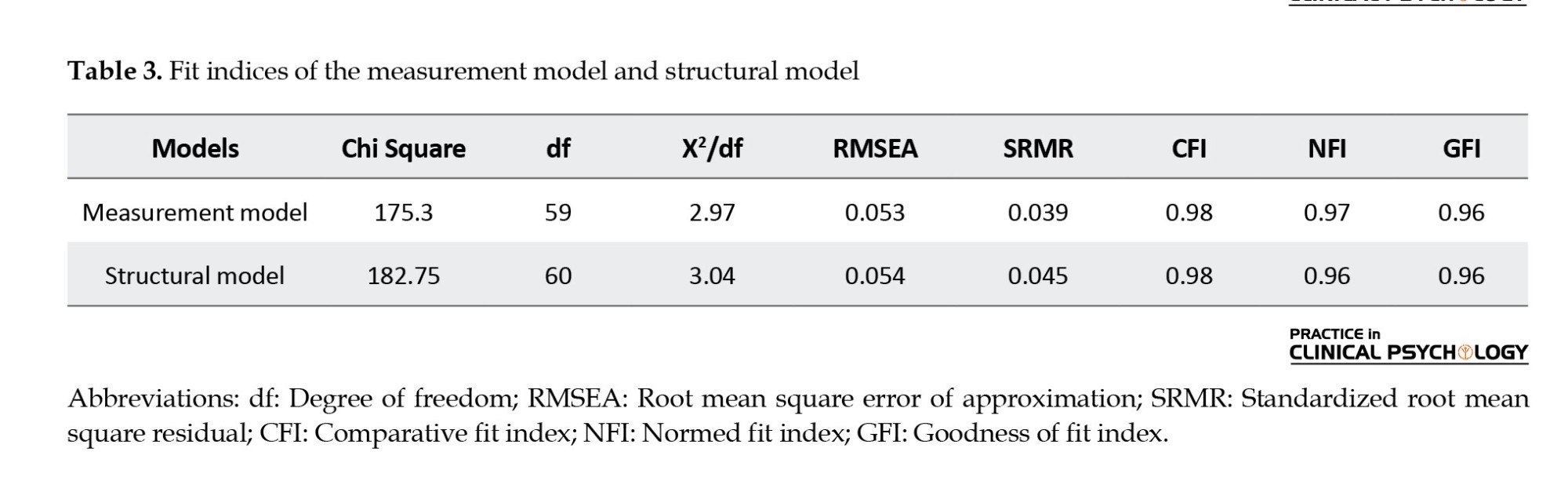
Before the structural model evaluation, indicators for model fit were calculated and presented in Table 3. The measurement model identifies the relationship between evident and latent variables. Evaluation of this model is performed by using the CFA method. Indicators of the model fit showed satisfactory values.
Structural model: Direct effects
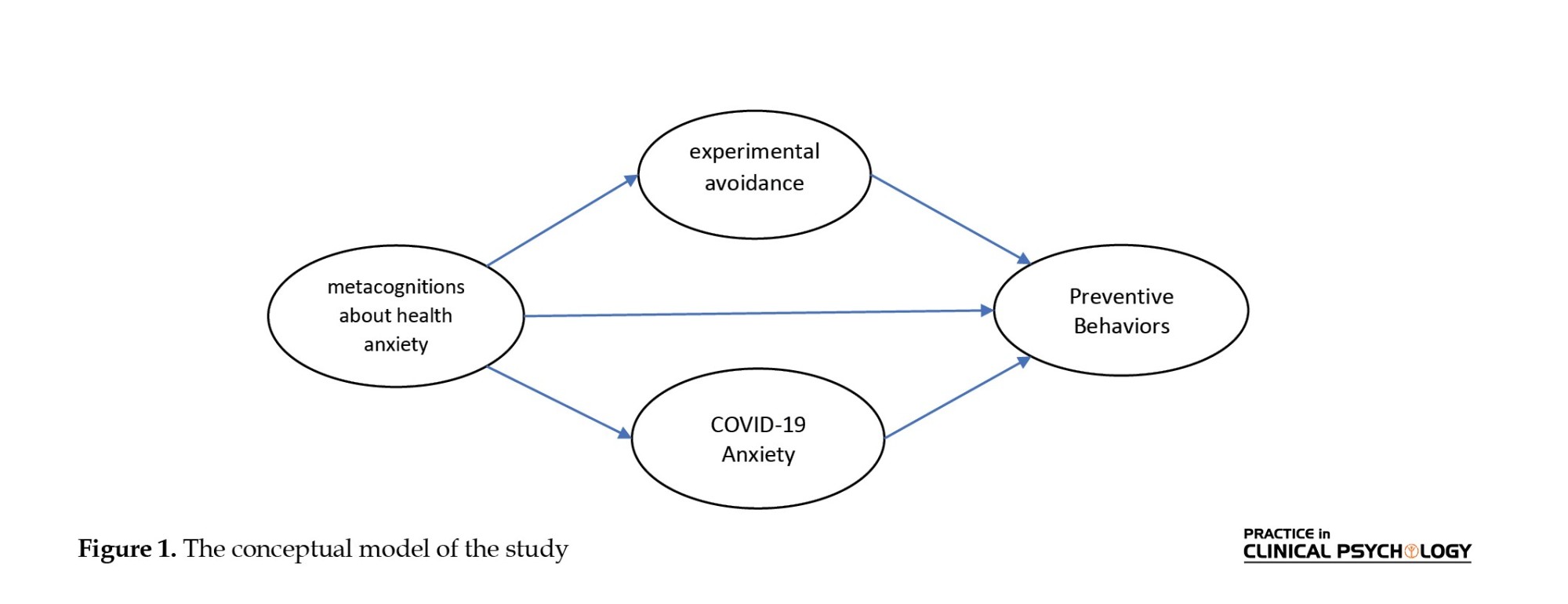
Figure 2 presents a hypothetical structural model with standard coefficients. As observed, metacognitive beliefs about health as an exogenous variable significantly affect COVID-19 anxiety and experiential avoidance of emotion as the mediating variables with a standard coefficient of 0.50 (t=10.03) and 0.60 (t=12.90), respectively. A standard coefficient of 0.11 (t=1.43) showed that metacognitive beliefs about health did not significantly affect the final dependent variable, preventive behaviors. On the other hand, experiential avoidance of emotion and COVID-19 anxiety as mediating variables significantly affect preventive behaviors, with standard coefficients of 0.19 (t=3.02) and 0.24 (t=4.33). Also, the determination coefficients of endogenous variables of the model are at satisfactory levels. These results indicate that the present model can explain 8% of preventive behaviors. Likewise, health-related metacognitive beliefs can explain 36% of the experiential avoidance of emotion and 25% of COVID-19 anxiety; therefore, the SEM fit is satisfactory.
Evaluation of the mediating model: Indirect effects
Bootstrap hypothesis testing was used to evaluate the effects of mediating variables. The mediating impact is significant if the Bootstrap limits are marked with the same symbols, – or +. Results showed that the bootstrap test’s upper and lower limit is positive, and there is no zero between these two limits. It indicates that the effects of health-related metacognitive beliefs on preventive behaviors through experiential avoidance and COVID-19 anxiety are significant, with an effect size of .12 (P=0.004, P=0.001). Therefore, it can be concluded that metacognitive beliefs about health can significantly affect preventive behaviors, through the mentioned mediating variables, experiential avoidance and COVID-19 anxiety (Figure 2).
Discussion
This study investigated the role of health metacognitions, COVID-19 anxiety, and experiential avoidance factors in predicting preventive behaviors during pandemics. The findings of our study showed that both COVID-19 anxiety and experiential avoidance factors could significantly predict preventive behaviors. However, health metacognition could indirectly predict preventive behaviors. If COVID-19 anxiety and experiential avoidance are increased due to health metacognition, an outcome will be the decreased number of preventive behaviors.
Consistent with studies showing that higher anxiety levels are related to multiple unhealthy behaviors (Lovell et al., 2015; Strine et al., 2005), this study found that COVID-19 anxiety was a predictive factor for preventive behaviors against COVID-19. It is implicated that the more anxiety individuals have, the more preventive behaviors they will do. This is consistent with research showing that higher levels of anxiety can motivate individuals to take more health-promoting behaviors (Cowling et al., 2020; Tyrer et al., 2011). Also, our results are consistent with studies highlighting the importance of anxiety in adverse outcomes of the disease process as it can lead to higher healthcare costs, avoiding visiting doctors and limiting related information (Fink et al., 2010; Kőszegi, 2003). These results show that more COVID-19 anxiety can motivate someone to refrain from risky behaviors. One explanation can be that with higher levels of anxiety, individuals show less attention to threats and, instead, limit their attention scope to overcome the threats (Kappenman et al., 2021). We see that a higher level of anxiety is positively correlated with more preventive behaviors which may lead to more compulsive type of behaviors in the future. This process needs to be investigated further in future research.
Another finding of this study was that experiential avoidance could predict preventive behaviors. Our results agree with Chartier et al., (2010) research, showing that when experiential avoidance is higher, persons have lower levels of self-efficacy, which prevents them from managing a chronic condition appropriately (Chartier et al., 2010). However, the results of this study are inconsistent with studies showing that experiential avoidance is not a negative response unless it interacts with and interrupts self-regulation mechanisms (Karademas et al., 2017). Consistent with our results, research shows that patients do not think about the adverse outcomes of their behaviors because they are suppressing aversive feelings and experiences about the disease (Hayes-Skelton & Eustis, 2020). Accordingly, during the COVID-19 pandemic, individuals show higher levels of experiential avoidance to control and avoid distressing experiences. Consequently, they do more preventive behaviors as it helps them stick to their ways of experiential avoidance more easily. They try to avoid the possibility of getting sick or experiencing the illness and the need to see a doctor.
Previous studies have demonstrated that health metacognition can increase or decrease specific behaviors. Also, the findings of this study showed that metacognition is associated with preventive behaviors. It is consistent with previous research indicating that metacognition is related to extended thinking and thought suppression, a condition in which individuals disregard threats and behavior outcomes (Roussis & Wells, 2008; Spada et al., 2015). One possible explanation for this process is that during a pandemic, CAS is activated, and the person is involved in an inflexible, maladaptive pattern of behaviors (Spada et al., 2015; Wells & Matthews, 1996). However, it was found that metacognition can only lead to more preventive behaviors if it increases experiential avoidance or COVID-19 anxiety. Our results were in line with previous research showing that metacognition can increase negative emotions, levels of anxiety, and experiential avoidance (Bailey & Wells, 2016; McEvoy et al., 2013; Woolrich et al., 2008). Therefore, it can be implicated that metacognitions can increase COVID-19 preventive behaviors only when they lead to emotional problems and negative self-evaluations. They cannot change the number of preventive behaviors directly. In this study, we can see that this number of preventive behaviors may be maladaptive as they are due to high anxiety and experiential avoidance.
The findings of our study showed that to improve and modify COVID-19 preventive behaviors, we must modify individuals’ metacognition. Metacognition is an essential factor that can increase anxiety and experiential avoidance, leading to more maladaptive behaviors. Consequently, we should identify maladaptive metacognition to reduce the spread of COVID-19 as well as behavioral problems. Giving some information about metacognitions and their effects on individuals can better explain what may prevent them from being aware of their risky behaviors. During the COVID-19 pandemic, it is helpful to teach individuals how to identify their metacognition and deal with it appropriately.
Conclusion
Although we achieved our study goals, there were several limitations. The SEM technique cannot determine the causal relationships between health metacognition, COVID-19 anxiety, experiential avoidance, and COVID-19 preventive behaviors. When generalizing the results, it should be noted that our study was conducted on Iranian individuals who use the Internet and are probably at higher education and higher socioeconomic levels. Our study was conducted on Iranian people and their behavior; therefore, cultural differences should be considered when generalizing the results to other individuals. Future research may focus on the patterns of preventive behaviors due to metacognitions; it should be clarified how much adherence is adaptive.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed of the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
This article was extracted from a research project, funded by Kharazmi University (Grand No.: 3799).
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors wish to thank Kharazmi University for its support and all the participants for attending the research.
References
Abasi, E., Fti, L., Molodi, R., & Zarabi, H. (2013). Psychometric properties of the Persian version of acceptance and action questionnaire-II. Psychological Methods and Models, 3(10), 65-80. [Link]
Anderson, J. C., & Gerbing, D. W. (1988). Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin, 103(3), 411. [DOI:10.1037/0033-2909.103.3.411]
Asmundson, G. J. G., & Taylor, S. (2020). How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. Journal of Anxiety Disorders, 71, 102211.[DOI:10.1016/j.janxdis.2020.102211] [PMID]
Bailey, R., & Wells, A. (2013). Does metacognition make a unique contribution to health anxiety when controlling for neuroticism, illness cognition, and somatosensory amplification?. Journal of Cognitive Psychotherapy, 27(4), 327–337.[DOI:10.1891/0889-8391.27.4.327] [PMID]
Bailey, R., & Wells, A. (2015). Development and initial validation of a measure of metacognitive beliefs in health anxiety: The MCQ-HA. Psychiatry Research, 230(3), 871–877.[DOI:10.1016/j.psychres.2015.11.035] [PMID]
Bailey, R., & Wells, A. (2016). The contribution of metacognitive beliefs and dysfunctional illness beliefs in predicting health anxiety: An evaluation of the metacognitive versus the cognitive models. Clinical Psychologist, 20(3), 129-137. [DOI:10.1111/cp.12078]
Barsky, A. J., Ettner, S. L., Horsky, J., & Bates, D. W. (2001). Resource utilization of patients with hypochondriacal health anxiety and somatization. Medical Care, 39(7), 705–715.[DOI:10.1097/00005650-200107000-00007] [PMID]
Bond, F. W., Hayes, S. C., Baer, R. A., Carpenter, K. M., Guenole, N., & Orcutt, H. K., et al. (2011). Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42(4), 676–688.[DOI:10.1016/j.beth.2011.03.007] [PMID]
Chartier, M., Vinatieri, T., Delonga, K., McGlynn, L. M., Gore-Felton, C., & Koopman, C. (2010). A pilot study investigating the effects of trauma, experiential avoidance, and disease management in HIV-positive MSM using methamphetamine. Journal of the International Association of Physicians in AIDS Care (Chicago, Ill. : 2002), 9(2), 78–81. [DOI:10.1177/1545109709360065] [PMID]
Clancy, F., Prestwich, A., Caperon, L., & O'Connor, D. B. (2016). Perseverative cognition and health behaviors: A systematic review and meta-analysis. Frontiers in Human Neuroscience, 10, 534. [DOI:10.3389/fnhum.2016.00534] [PMID]
Cowling, B. J., Ali, S. T., Ng, T. W., Tsang, T. K., Li, J. C., & Fong, M. W., et al. (2020). Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. The Lancet Public Health, 5(5), e279-e288. [DOI:10.1016/S2468-2667(20)30090-6]
Fink, P., Ørnbøl, E., & Christensen, K. S. (2010). The outcome of health anxiety in primary care. A two-year follow-up study on health care costs and self-rated health. Plos One, 5(3), e9873. [DOI:10.1371/journal.pone.0009873] [PMID]
Fledderus, M., Bohlmeijer, E. T., & Pieterse, M. E. (2010). Does experiential avoidance mediate the effects of maladaptive coping styles on psychopathology and mental health?. Behavior Modification, 34(6), 503–519. [DOI:10.1177/0145445510378379] [PMID]
González-Castro, J. L., Ubillos-Landa, S., Puente-Martínez, A., & Gracia-Leiva, M. (2021). Perceived vulnerability and severity predict adherence to COVID-19 protection measures: The mediating role of instrumental coping. Frontiers in Psychology, 12, 674032. [DOI:10.3389/fpsyg.2021.674032] [PMID]
Hayes-Skelton, S. A., & Eustis, E. H. (2020). Experiential avoidance. In J. S. Abramowitz & S. M. Blakey (Eds.), Clinical handbook of fear and anxiety: Maintenance processes and treatment mechanisms (pp. 115–131). Washington: American Psychological Association. [DOI:10.1037/0000150-007]
Hayes, S. C., Wilson, K. G., Gifford, E. V., Follette, V. M., & Strosahl, K. (1996). Experimental avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology, 64(6), 1152–1168. [DOI:10.1037/0022-006X.64.6.1152] [PMID]
Hildebrandt, M. J., & Hayes, S. C. (2012). The contributing role of negative affectivity and experiential avoidance to increased cardiovascular risk. Social and Personality Psychology Compass, 6(8), 551-565. [DOI:10.1111/j.1751-9004.2012.00448.x]
Kappenman, E. S., Geddert, R., Farrens, J. L., McDonald, J. J., & Hajcak, G. (2021). Recoiling from threat: Anxiety is related to heightened suppression of threat, not increased attention to threat. Clinical Psychological Science : A journal of the Association for Psychological Science, 9(3), 434–448.[DOI:10.1177/2167702620961074] [PMID]
Karademas, E. C., Karekla, M., Flouri, M., Vasiliou, V. S., Kasinopoulos, O., & Papacostas, S. S. (2017). The impact of experiential avoidance on the relations between illness representations, pain catastrophising and pain interference in chronic pain. Psychology & Health, 32(12), 1469–1484. [DOI:10.1080/08870446.2017.1346193] [PMID]
Keinonen, K., Puolakanaho, A., Lappalainen, P., Lappalainen, R., & Kiuru, N. (2021). Developmental trajectories of experiential avoidance and depressive symptoms and association to health behaviors among adolescents during brief guided online acceptance and commitment therapy. Journal of Contextual Behavioral Science, 22, 24-31. [DOI:10.1016/j.jcbs.2021.08.002]
Kim, S., & Kim, S. (2020). Analysis of the Impact of Health Beliefs and Resource Factors on Preventive Behaviors against the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 17(22), 8666. [DOI:10.3390/ijerph17228666] [PMID]
Kim, J. H., Shin, S., & Park, J. H. (2015). A methodological quality assessment of South Korean nursing research using structural equation modeling in South Korea. Journal of Korean Academy of Nursing, 45(2), 159-168. [Link]
Kingston, J., Clarke, S., & Remington, B. (2010). Experiential avoidance and problem behavior: A mediational analysis. Behavior Modification, 34(2), 145–163.[DOI:10.1177/0145445510362575] [PMID]
Kline, R. B. (2015). Principles and practice of structural equation modeling. New York: Guilford Publications. [Link]
Koszegi B. (2003). Health anxiety and patient behavior. Journal of Health Economics, 22(6), 1073–1084. [DOI:10.1016/j.jhealeco.2003.06.002] [PMID]
Lenzo, V., Sardella, A., Martino, G., & Quattropani, M. C. (2020). A systematic review of metacognitive beliefs in chronic medical conditions. Frontiers in Psychology, 10, 2875.[DOI:10.3389/fpsyg.2019.02875] [PMID] [PMCID]
Lovell, G. P., Nash, K., Sharman, R., & Lane, B. R. (2015). A cross-sectional investigation of depressive, anxiety, and stress symptoms and health-behavior participation in Australian university students. Nursing & Health Sciences, 17(1), 134–142. [DOI:10.1111/nhs.12147] [PMID]
Machell, K. A., Goodman, F. R., & Kashdan, T. B. (2015). Experiential avoidance and well-being: A daily diary analysis. Cognition & Emotion, 29(2), 351–359. [DOI:10.1080/02699931.2014.911143] [PMID]
Mao L. (2011). Evaluating the combined effectiveness of influenza control strategies and human preventive behavior. Plos One, 6(10), e24706. [DOI:10.1371/journal.pone.0024706] [PMID]
McEvoy, P. M., Moulds, M. L., & Mahoney, A. E. (2013). Mechanisms driving pre- and post-stressor repetitive negative thinking: metacognitions, cognitive avoidance, and thought control. Journal of Behavior Therapy and Experimental Psychiatry, 44(1), 84–93. [DOI:10.1016/j.jbtep.2012.07.011] [PMID]
Mohammadkhani, S., Akbari, M., Shahbahrami, M., Seydavi, M., & Kolubinski, D. C. (2023). Metacognitions about health in relation to coronavirus anxiety: The mediating role of Cognitive Attentional Syndrome And Distress Tolerance. Journal Of Rational-Emotive and Cognitive-Behavior Therapy : RET, 41(1), 222–236. [DOI:10.1007/s10942-022-00467-x] [PMID]
Nguyen, N. P. T., Hoang, T. D., Tran, V. T., Vu, C. T., Siewe Fodjo, J. N., & Colebunders, R., et al. (2020). Preventive behavior of vietnamese people in response to the COVID-19 pandemic. Plos One, 15(9), e0238830. [DOI:10.1371/journal.pone.0238830] [PMID]
Nunnally, J. C. (1967). Psychometric theory. New York: McGraw-Hill. [Link]
Riad, A., Huang, Y., Zheng, L., & Elavsky, S. (2020). COVID-19 induced anxiety and protective behaviors during COVID-19 outbreak: Scale development and validation. medRxiv, [Unpublished]. [DOI:10.2139/ssrn.3594370]
Roussis, P., & Wells, A. (2008). Psychological factors predicting stress symptoms: Metacognition, thought control, and varieties of worry. Anxiety, Stress, and Coping, 21(3), 213–225.[DOI:10.1080/10615800801889600] [PMID]
Shaw, R., Kim, Y. K., & Hua, J. (2020). Governance, technology and citizen behavior in pandemic: Lessons from COVID-19 in East Asia. Progress in Disaster Science, 6, 100090.[DOI:10.1016/j.pdisas.2020.100090] [PMID]
Shen, F., Min, C., Lu, Y., & Chu, Y. (2021). The effect of cognition and affect on preventive behaviors during the COVID-19 pandemic: A cross-sectional study in China. BMC Public Health, 21(1), 722. [DOI:10.1186/s12889-021-10784-y] [PMID]
Spada, M. M., Caselli, G., Nikčević, A. V., & Wells, A. (2015). Metacognition in addictive behaviors. Addictive Behaviors, 44, 9-15. [DOI:10.1016/j.addbeh.2014.08.002]
Ştefănuţ, A. M., Vintilă, M., Tomiţă, M., Treglia, E., Lungu, M. A., & Tomassoni, R. (2021). The influence of health beliefs, of resources, of vaccination history, and of health anxiety on intention to accept COVID-19 vaccination. Frontiers in Psychology, 12, 729803. [DOI:10.3389/fpsyg.2021.729803] [PMID]
Strine, T. W., Chapman, D. P., Kobau, R., & Balluz, L. (2005). Associations of self-reported anxiety symptoms with health-related quality of life and health behaviors. Social Psychiatry and Psychiatric Epidemiology, 40(6), 432-438. [DOI:10.1007/s00127-005-0914-1] [PMID]
Suls, J., & Fletcher, B. (1985). The relative efficacy of avoidant and nonavoidant coping strategies: A meta-analysis. Health Psychology, 4(3), 249–288. [DOI:10.1037/0278-6133.4.3.249] [PMID]
Taylor S. (2022). The psychology of pandemics. Annual Review of Clinical Psychology, 18, 581–609. [DOI:10.1146/annurev-clinpsy-072720-020131] [PMID]
Toussaint, L. L., Cheadle, A. D., Fox, J., & Williams, D. R. (2020). Clean and contain: Initial development of a measure of infection prevention behaviors during the COVID-19 pandemic. Annals of Behavioral Medicine, 54(9), 619–625. [DOI:10.1093/abm/kaaa064] [PMID]
Tyrer, P., Cooper, S., Crawford, M., Dupont, S., Green, J., & Murphy, D., et al. (2011). Prevalence of health anxiety problems in medical clinics. Journal of Psychosomatic Research, 71(6), 392–394. [DOI:10.1016/j.jpsychores.2011.07.004] [PMID]
Waltz, T. J., & Hayes, S. C. (2010). Acceptance and commitment therapy. In A. Freeman, M. A. Reinecke, & N. Kazantzis (Eds.) Cognitive and Behavioral Theories in Clinical Practice. New York: Guilford Press. [Link]
Wells, A. (2011). Metacognitive therapy for anxiety and depression. New York: Guilford Press. [Link]
Wells, A., & Matthews, G. (1996). Modelling cognition in emotional disorder: The S-REF model. Behaviour Research and Therapy, 34(11-12), 881-888. [DOI:10.1016/S0005-7967(96)00050-2]
Woolrich, R. A., Cooper, M. J., & Turner, H. M. (2008). Metacognition in patients with anorexia nervosa, dieting and non-dieting women: A preliminary study. European Eating Disorders Review, 16(1), 11–20. [DOI:10.1002/erv.802] [PMID]
According to the World Health Organization (WHO, 2020), coronavirus disease 2019 (COVID-19) has spread rapidly worldwide since late March 2020 (WHO, 2020). Following the prevalence of this disease and no reliable evidence regarding the most effective interventions for the treatment, COVID-19 preventive behaviors are essential to reduce the transmission rate. Accordingly, promoting adherence to public health mandates can lessen the prevalence of the disease (Shaw et al., 2020). Performing preventive behaviors, whether at the national or individual level, is highly needed to stop the virus’s transmission (Kim & Kim, 2020; Nguyen et al., 2020). Important COVID-19 preventive behaviors, such as wearing a mask, staying home, washing hands regularly &, etc., are activities toward promoting health that can be done individually and voluntarily (Mao, 2011).
Preventive behaviors toward COVID-19 are strongly related to cognitive and affective variables (Shen et al., 2021). A critical phenomenon is called metacognition which is in charge of the way cognitions and emotions act (Wells, 2011). In detail, metacognition is the knowledge or cognitive activity controlling and regulating cognition (Wells, 2011). It consists of sets of beliefs that a person has about the efficacy of thoughts (Wells, 2011). In the metacognitive model, individuals are caught in the trap of negative emotions and negative beliefs when their metacognition leads them to use a specific response pattern (Wells, 2011). They can lead to inflexible, maladaptive, and repetitive beliefs about thoughts and emotions, known as cognitive attentional syndrome (CAS) (Wells & Matthews, 1996). CAS controls thoughts through positive (e.g. worry helps me to deal with difficulties) and negative (e.g. my thoughts are uncontrollable and can make me crazy) metacognitive beliefs (Wells, 2011). One of the areas where the presence and function of metacognition are necessary is health anxiety (HA). Metacognition is correlated with HA and can predict its symptoms successfully (Bailey & Wells, 2013, 2015). Accordingly and as a result, Bailey and Wells (2015) investigated specific metacognition which is related to health anxiety. In this study, we focus on this specific type of metacognition.
Metacognition stimulates coping responses when facing an actual or perceived crisis, and they are related to anxiety and also the quality of life in individuals with chronic conditions as it increases distress decreases treatment adherence, and disrupts patients’ copying functions (Lenzo et al., 2020). Therefore, metacognitions seem to have the ability to lead an individual to remain in a pattern of behaviors increasing exposure to the COVID-19 infection (González-Castro et al., 2021); however, the information about this process, which may be either direct or indirect, is not sufficient. Although there is research on the relationship between cognition and preventive behaviors (Clancy et al., 2016), the relationship between metacognition and preventive behaviors has not yet been clarified, so we aimed to fill this gap with our study.
Additionally, anxiety can play a vital role in preventive behaviors. Previous studies have shown that a moderate level of anxiety (Riad et al., 2020) may increase the adoption of preventive behaviors, such as keeping social distance, washing hands, and wearing a mask (Cowling et al., 2020; Tyrer et al., 2011). On the other hand, this anxiety can change the behavior of an affected person and health service providers (Barsky et al., 2001; Fink et al., 2010) and decrease acceptance of suggested preventive behaviors (Ştefănuţ et al., 2021). We see that anxiety can lead to health impairing or protective behaviors (Asmundson & Taylor, 2020; Taylor, 2022). Considering these contradictory findings about the effects of anxiety, we need to investigate its relationship with preventive behaviors.
Another factor relating to one’s health is called experiential avoidance (Machell et al., 2015). Some studies on the relationship between experiential avoidance and diseases or behaviors have shown that it is significantly associated with high-risk health behaviors (Keinonen et al., 2021). Experiential avoidance is a behavior aimed at changing the forms and the experiences of unpleasant events, memories, thoughts, and physical senses, resulting in many psychopathological symptoms (Hayes et al., 1996). This construct consists of two parts: Reluctance to contact personal experiences; and efforts to avoid painful experiences or events (Waltz & Hayes, 2010). It was shown that experiential avoidance could lead to engaging in problematic behaviors (Hayes et al., 1996; Hildebrandt & Hayes, 2012; Kingston et al., 2010). A study showed that individuals with high levels of experiential avoidance have lower self-efficacy in illness management (Chartier et al., 2010), which may, as a result, change how a person performs preventive behaviors (Fledderus et al., 2010). If we consider the occurrence of a disease crisis, such as COVID-19, as a painful event, the role of experiential avoidance in this process is noticeable. Therefore, we wanted to answer whether experiential avoidance, which disrupts the process of experiencing the COVID-19 crisis, affects preventive behaviors.
In contrast, it has been shown that experiential avoidance does not necessarily lead to aversive outcomes (Karademas et al., 2017). It may even provide better coping styles (Suls & Fletcher, 1985). However, interacting with illness-related mechanisms increases the possibility of adverse effects (Karademas et al., 2017). To our knowledge, there are no studies on the relationship between experiential avoidance and, specifically, COVID-19 preventive behaviors which need to be clarified. Furthermore, it has been shown that maladaptive metacognitions are positively and significantly associated with experiential avoidance (McEvoy et al., 2013). Align with the research mentioned earlier, we tried to investigate the interaction between experiential avoidance and metacognitions which may change preventive behaviors.
Altogether, crises like pandemics require extensive cooperation, and one of the most critical parts is individual preventive behaviors (Kim & Kim, 2020). Increasing such behaviors is vital in discontinuing the disease transmission cycle, even though many people have been fully vaccinated. Consequently, we targeted these behaviors as they should be followed even after getting vaccinated or in other contexts. Although metacognitions can help us analyze and understand many disorders’ behavioral, emotional, and cognitive psychopathology, there is not enough information about their direct or indirect effects on health-related behaviors, such as preventive behaviors (Lenzo et al., 2020). In conclusion, in this research, we answer whether health-related metacognition can change these behaviors and whether these changes are carried out with the mediating help of experiential avoidance or COVID-19 anxiety (Figure 1).
Materials and Methods
Procedure and participants
We distributed participation advertisements on Instagram and Facebook and gave a brief description of the study with a Google form link leading potential participants to consent forms and questionnaires. The ethics committee approved all the study procedures. Data were collected from November 3 to 14, 2021. Participants were recruited from the general population in Iran. The inclusion criteria were literacy, consent to participate in the research, and the age range of 18 to 60. Out of 963 invited individuals, 712 participated and completed the questionnaires, indicating a response rate of 73.93%. Ten data were excluded from the analysis due to incompleteness. After data deletion, data of 702 participants (61% female) were analyzed for the current study. According to the preferred sample size for structural equation modeling (SEM) analysis (min of 5 and max of 10 cases per estimated parameter), the required number of participants for this study with 35 items is 175-350, so our sample size seems adequate (Nunnally, 1967; Kim, 2015).
Measures
Socio-demographic form
A form for gathering information on variables such as age, gender, educational level, employment status, income, and criteria was made.
The metacognitions questionnaire -health anxiety (MCQ-HA)
The metacognition questionnaire-health anxiety (MCQ-HA) was developed by Baily and Wells (2015) to measure metacognition about health anxiety (Bailey & Wells, 2015). This scale consists of 14 items with a 4-point Likert scale ranging from 1 (“not agree”) to 4 (“very agree”). The total score of this questionnaire ranges from 14 to 56, with a higher score indicating higher levels of metacognitive beliefs associated with health anxiety. It consists of three subscales: (1) Beliefs that thoughts cause illness (MCQ‐HAC; e.g. “Thinking about illness can change my health.”); (2) Beliefs about biased thinking (MCQ‐HAB; e.g. “Thinking about the worst symptoms keeps me safe”); and (3) Beliefs that thoughts are uncontrollable (MCQ‐HAU; e.g. “Only if I have a diagnosis will I be able to stop worrying.”) A study has shown that this scale has good internal consistency and concurrent validity (Bailey & Wells, 2015). It is consistent with the Cronbach alpha reported (α=0.75) for its Persian version conducted by Mohammadkhani et al. (2022) and our study.
Coronavirus anxiety scale (CAS)
The coronavirus anxiety scale (CAS) is a valid, unidimensional scale developed by Lee (2020d) that assesses the physiological responses of dysfunctional fear and anxiety associated with the COVID-19 virus. This scale consists of five items (e.g. “I felt paralyzed or frozen when I thought about or was exposed to information about the coronavirus.”) Then, participants were assessed according to the 5-point scale (0=none / never, 4=almost every day for the past 2 weeks) on how often each anxiety symptom occurred (e.g. “I had trouble falling or staying asleep because I was thinking about the coronavirus.”) The total score of this questionnaire ranges from 0 to 20. This scale has acceptable internal consistency, reliability, structure, and concurrent validity. The Cronbach alpha of its Persian version was 0.79 in the study of Mohammadkhani et al. (2022). The cut score of this scale is ≥9, with 90% sensitivity and 85% specificity. The Cronbach alpha in the current study was 0.79.
Acceptance and action questionnaire (AAQ-2)
The acceptance and action questionnaire has been developed to examine psychological rigidity and experimental avoidance (Bond et al., 2011). It is a 7-item questionnaire using a 7-point Likert scale ranging from 1 (never) to 7 (always true). The total score of this questionnaire ranges from 7 to 49. Higher scores indicate higher levels of experiential avoidance. The Cronbach alpha has been reported as α=.93. Its Persian version has satisfactory internal consistency (0.71 to 0.89) and good test-retest reliability (Abasi et al., 2013). The Cronbach alpha of this questionnaire in this study was 0.85.
Preventive COVID-19 behaviors scale: the clean and contain measure
Considering the recommendations by the center for disease control (CDC) in March 2020, Toussaint et al. (2020) developed a 9-item, 5-Likert scale (from “not at all”: 1 to “always”: 5) to assess protective behaviors, including washing hands, keeping social distance, staying at home when feeling sick, respiratory exercises, and not touching eyes, nose, and mouth, against coronavirus infection over the past week. The total score of this questionnaire ranges from 9 to 45. A higher total score indicates a higher level of compliance with the CDC’s recommendations. The questionnaire has good internal consistency, α>84, and our results showed a satisfactory Cronbach alpha of .88 for its Persian version.
Data analysis
SPSS software, version 22, LISREL software, version 8.85, and MPlus software, version 7.4 statistical software were used to analyze the data and investigate the research hypotheses. Model fit for the modified hypothetical model was tested using structural equation modeling (SEM). Data analysis was performed using a two-stage approach (Anderson & Gerbing, 1988). First, confirmatory factor analysis (CFA) was used to evaluate the model fit of the modified model. The second step tested the hypothetical structural model using the SEM method.
Results
Descriptive statistics
Participants’ characteristics are presented in Table 1. The final sample comprised 702 participants, 272 men (39%) and 430 women (61.%). Participants mean age was 35.15±9.05 and 33.76±17.17 for males and females, respectively. Also, in Table 1, descriptive indicators include the mean, standard deviation, kurtosis, and skewness of the research variables.
Structural equation modeling assumptions
Before evaluating the structural model of the research, we examined SEM assumptions, which were confirmed. Also, the suitability of this statistical method for the present study was approved. One of the most important assumptions of this statistical approach is univariate and multivariate normality. To examine univariate normality, kurtosis, and skewness of the research variables are assessed. Kurtosis of the variables is in the range of 2.50 to -1.25, and their skewness is in the range of .782 to 6.371. For a suitable kurtosis, a cutting point of ±3 is considered satisfactory. A cutting point of skewness indicates that values more than ±10 are not acceptable (Kline, 2015). The relative multivariate skewness index, calculated to assess the hypothesis of multivariate normality, reached 1.320. To get multivariate normality, the value of this indicator should not be more than 3. The correlation matrix between evident variables can indicate the existence of multicollinearity between them. Accordingly, correlation coefficients above 0.85 can interrupt the estimation of the model (Kline, 2015). Correlation coefficients were in a range of -0.03 to 0.70. Preliminary analyses showed that data was suitable for structural equation modeling and the maximum estimation method. The matrix of correlations between the research variables and their mean and standard deviation are presented in Table 2. As this table shows, all correlations are moderate (.375≤ r≤0.502).
Measurement model (confirmatory factor analysis)
Before the structural model evaluation, indicators for model fit were calculated and presented in Table 3. The measurement model identifies the relationship between evident and latent variables. Evaluation of this model is performed by using the CFA method. Indicators of the model fit showed satisfactory values.
Structural model: Direct effects
Figure 2 presents a hypothetical structural model with standard coefficients. As observed, metacognitive beliefs about health as an exogenous variable significantly affect COVID-19 anxiety and experiential avoidance of emotion as the mediating variables with a standard coefficient of 0.50 (t=10.03) and 0.60 (t=12.90), respectively. A standard coefficient of 0.11 (t=1.43) showed that metacognitive beliefs about health did not significantly affect the final dependent variable, preventive behaviors. On the other hand, experiential avoidance of emotion and COVID-19 anxiety as mediating variables significantly affect preventive behaviors, with standard coefficients of 0.19 (t=3.02) and 0.24 (t=4.33). Also, the determination coefficients of endogenous variables of the model are at satisfactory levels. These results indicate that the present model can explain 8% of preventive behaviors. Likewise, health-related metacognitive beliefs can explain 36% of the experiential avoidance of emotion and 25% of COVID-19 anxiety; therefore, the SEM fit is satisfactory.
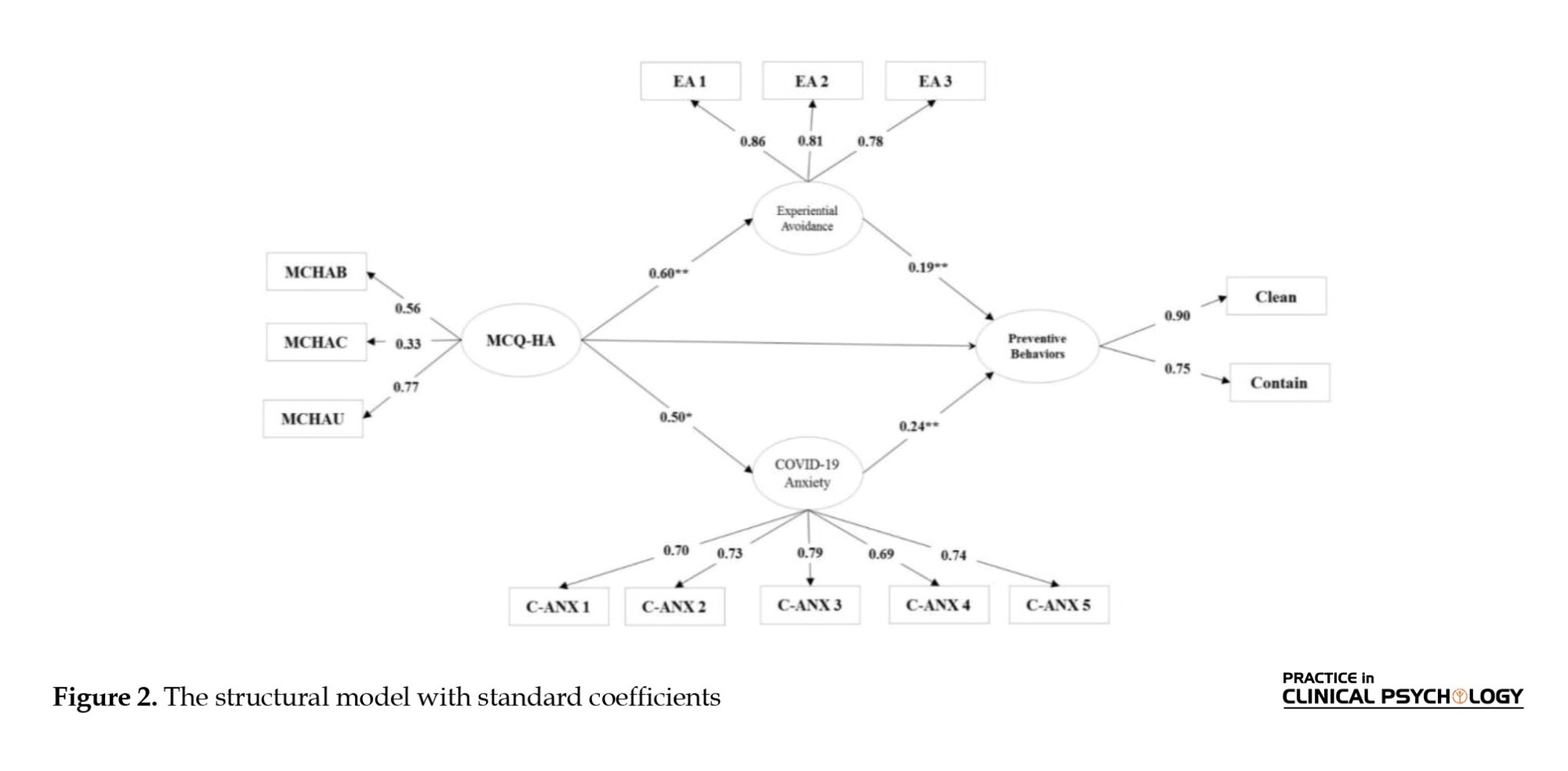
Evaluation of the mediating model: Indirect effects
Bootstrap hypothesis testing was used to evaluate the effects of mediating variables. The mediating impact is significant if the Bootstrap limits are marked with the same symbols, – or +. Results showed that the bootstrap test’s upper and lower limit is positive, and there is no zero between these two limits. It indicates that the effects of health-related metacognitive beliefs on preventive behaviors through experiential avoidance and COVID-19 anxiety are significant, with an effect size of .12 (P=0.004, P=0.001). Therefore, it can be concluded that metacognitive beliefs about health can significantly affect preventive behaviors, through the mentioned mediating variables, experiential avoidance and COVID-19 anxiety (Figure 2).
Discussion
This study investigated the role of health metacognitions, COVID-19 anxiety, and experiential avoidance factors in predicting preventive behaviors during pandemics. The findings of our study showed that both COVID-19 anxiety and experiential avoidance factors could significantly predict preventive behaviors. However, health metacognition could indirectly predict preventive behaviors. If COVID-19 anxiety and experiential avoidance are increased due to health metacognition, an outcome will be the decreased number of preventive behaviors.
Consistent with studies showing that higher anxiety levels are related to multiple unhealthy behaviors (Lovell et al., 2015; Strine et al., 2005), this study found that COVID-19 anxiety was a predictive factor for preventive behaviors against COVID-19. It is implicated that the more anxiety individuals have, the more preventive behaviors they will do. This is consistent with research showing that higher levels of anxiety can motivate individuals to take more health-promoting behaviors (Cowling et al., 2020; Tyrer et al., 2011). Also, our results are consistent with studies highlighting the importance of anxiety in adverse outcomes of the disease process as it can lead to higher healthcare costs, avoiding visiting doctors and limiting related information (Fink et al., 2010; Kőszegi, 2003). These results show that more COVID-19 anxiety can motivate someone to refrain from risky behaviors. One explanation can be that with higher levels of anxiety, individuals show less attention to threats and, instead, limit their attention scope to overcome the threats (Kappenman et al., 2021). We see that a higher level of anxiety is positively correlated with more preventive behaviors which may lead to more compulsive type of behaviors in the future. This process needs to be investigated further in future research.
Another finding of this study was that experiential avoidance could predict preventive behaviors. Our results agree with Chartier et al., (2010) research, showing that when experiential avoidance is higher, persons have lower levels of self-efficacy, which prevents them from managing a chronic condition appropriately (Chartier et al., 2010). However, the results of this study are inconsistent with studies showing that experiential avoidance is not a negative response unless it interacts with and interrupts self-regulation mechanisms (Karademas et al., 2017). Consistent with our results, research shows that patients do not think about the adverse outcomes of their behaviors because they are suppressing aversive feelings and experiences about the disease (Hayes-Skelton & Eustis, 2020). Accordingly, during the COVID-19 pandemic, individuals show higher levels of experiential avoidance to control and avoid distressing experiences. Consequently, they do more preventive behaviors as it helps them stick to their ways of experiential avoidance more easily. They try to avoid the possibility of getting sick or experiencing the illness and the need to see a doctor.
Previous studies have demonstrated that health metacognition can increase or decrease specific behaviors. Also, the findings of this study showed that metacognition is associated with preventive behaviors. It is consistent with previous research indicating that metacognition is related to extended thinking and thought suppression, a condition in which individuals disregard threats and behavior outcomes (Roussis & Wells, 2008; Spada et al., 2015). One possible explanation for this process is that during a pandemic, CAS is activated, and the person is involved in an inflexible, maladaptive pattern of behaviors (Spada et al., 2015; Wells & Matthews, 1996). However, it was found that metacognition can only lead to more preventive behaviors if it increases experiential avoidance or COVID-19 anxiety. Our results were in line with previous research showing that metacognition can increase negative emotions, levels of anxiety, and experiential avoidance (Bailey & Wells, 2016; McEvoy et al., 2013; Woolrich et al., 2008). Therefore, it can be implicated that metacognitions can increase COVID-19 preventive behaviors only when they lead to emotional problems and negative self-evaluations. They cannot change the number of preventive behaviors directly. In this study, we can see that this number of preventive behaviors may be maladaptive as they are due to high anxiety and experiential avoidance.
The findings of our study showed that to improve and modify COVID-19 preventive behaviors, we must modify individuals’ metacognition. Metacognition is an essential factor that can increase anxiety and experiential avoidance, leading to more maladaptive behaviors. Consequently, we should identify maladaptive metacognition to reduce the spread of COVID-19 as well as behavioral problems. Giving some information about metacognitions and their effects on individuals can better explain what may prevent them from being aware of their risky behaviors. During the COVID-19 pandemic, it is helpful to teach individuals how to identify their metacognition and deal with it appropriately.
Conclusion
Although we achieved our study goals, there were several limitations. The SEM technique cannot determine the causal relationships between health metacognition, COVID-19 anxiety, experiential avoidance, and COVID-19 preventive behaviors. When generalizing the results, it should be noted that our study was conducted on Iranian individuals who use the Internet and are probably at higher education and higher socioeconomic levels. Our study was conducted on Iranian people and their behavior; therefore, cultural differences should be considered when generalizing the results to other individuals. Future research may focus on the patterns of preventive behaviors due to metacognitions; it should be clarified how much adherence is adaptive.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles were considered in this article. The participants were informed of the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them.
Funding
This article was extracted from a research project, funded by Kharazmi University (Grand No.: 3799).
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors wish to thank Kharazmi University for its support and all the participants for attending the research.
References
Abasi, E., Fti, L., Molodi, R., & Zarabi, H. (2013). Psychometric properties of the Persian version of acceptance and action questionnaire-II. Psychological Methods and Models, 3(10), 65-80. [Link]
Anderson, J. C., & Gerbing, D. W. (1988). Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin, 103(3), 411. [DOI:10.1037/0033-2909.103.3.411]
Asmundson, G. J. G., & Taylor, S. (2020). How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. Journal of Anxiety Disorders, 71, 102211.[DOI:10.1016/j.janxdis.2020.102211] [PMID]
Bailey, R., & Wells, A. (2013). Does metacognition make a unique contribution to health anxiety when controlling for neuroticism, illness cognition, and somatosensory amplification?. Journal of Cognitive Psychotherapy, 27(4), 327–337.[DOI:10.1891/0889-8391.27.4.327] [PMID]
Bailey, R., & Wells, A. (2015). Development and initial validation of a measure of metacognitive beliefs in health anxiety: The MCQ-HA. Psychiatry Research, 230(3), 871–877.[DOI:10.1016/j.psychres.2015.11.035] [PMID]
Bailey, R., & Wells, A. (2016). The contribution of metacognitive beliefs and dysfunctional illness beliefs in predicting health anxiety: An evaluation of the metacognitive versus the cognitive models. Clinical Psychologist, 20(3), 129-137. [DOI:10.1111/cp.12078]
Barsky, A. J., Ettner, S. L., Horsky, J., & Bates, D. W. (2001). Resource utilization of patients with hypochondriacal health anxiety and somatization. Medical Care, 39(7), 705–715.[DOI:10.1097/00005650-200107000-00007] [PMID]
Bond, F. W., Hayes, S. C., Baer, R. A., Carpenter, K. M., Guenole, N., & Orcutt, H. K., et al. (2011). Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42(4), 676–688.[DOI:10.1016/j.beth.2011.03.007] [PMID]
Chartier, M., Vinatieri, T., Delonga, K., McGlynn, L. M., Gore-Felton, C., & Koopman, C. (2010). A pilot study investigating the effects of trauma, experiential avoidance, and disease management in HIV-positive MSM using methamphetamine. Journal of the International Association of Physicians in AIDS Care (Chicago, Ill. : 2002), 9(2), 78–81. [DOI:10.1177/1545109709360065] [PMID]
Clancy, F., Prestwich, A., Caperon, L., & O'Connor, D. B. (2016). Perseverative cognition and health behaviors: A systematic review and meta-analysis. Frontiers in Human Neuroscience, 10, 534. [DOI:10.3389/fnhum.2016.00534] [PMID]
Cowling, B. J., Ali, S. T., Ng, T. W., Tsang, T. K., Li, J. C., & Fong, M. W., et al. (2020). Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. The Lancet Public Health, 5(5), e279-e288. [DOI:10.1016/S2468-2667(20)30090-6]
Fink, P., Ørnbøl, E., & Christensen, K. S. (2010). The outcome of health anxiety in primary care. A two-year follow-up study on health care costs and self-rated health. Plos One, 5(3), e9873. [DOI:10.1371/journal.pone.0009873] [PMID]
Fledderus, M., Bohlmeijer, E. T., & Pieterse, M. E. (2010). Does experiential avoidance mediate the effects of maladaptive coping styles on psychopathology and mental health?. Behavior Modification, 34(6), 503–519. [DOI:10.1177/0145445510378379] [PMID]
González-Castro, J. L., Ubillos-Landa, S., Puente-Martínez, A., & Gracia-Leiva, M. (2021). Perceived vulnerability and severity predict adherence to COVID-19 protection measures: The mediating role of instrumental coping. Frontiers in Psychology, 12, 674032. [DOI:10.3389/fpsyg.2021.674032] [PMID]
Hayes-Skelton, S. A., & Eustis, E. H. (2020). Experiential avoidance. In J. S. Abramowitz & S. M. Blakey (Eds.), Clinical handbook of fear and anxiety: Maintenance processes and treatment mechanisms (pp. 115–131). Washington: American Psychological Association. [DOI:10.1037/0000150-007]
Hayes, S. C., Wilson, K. G., Gifford, E. V., Follette, V. M., & Strosahl, K. (1996). Experimental avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology, 64(6), 1152–1168. [DOI:10.1037/0022-006X.64.6.1152] [PMID]
Hildebrandt, M. J., & Hayes, S. C. (2012). The contributing role of negative affectivity and experiential avoidance to increased cardiovascular risk. Social and Personality Psychology Compass, 6(8), 551-565. [DOI:10.1111/j.1751-9004.2012.00448.x]
Kappenman, E. S., Geddert, R., Farrens, J. L., McDonald, J. J., & Hajcak, G. (2021). Recoiling from threat: Anxiety is related to heightened suppression of threat, not increased attention to threat. Clinical Psychological Science : A journal of the Association for Psychological Science, 9(3), 434–448.[DOI:10.1177/2167702620961074] [PMID]
Karademas, E. C., Karekla, M., Flouri, M., Vasiliou, V. S., Kasinopoulos, O., & Papacostas, S. S. (2017). The impact of experiential avoidance on the relations between illness representations, pain catastrophising and pain interference in chronic pain. Psychology & Health, 32(12), 1469–1484. [DOI:10.1080/08870446.2017.1346193] [PMID]
Keinonen, K., Puolakanaho, A., Lappalainen, P., Lappalainen, R., & Kiuru, N. (2021). Developmental trajectories of experiential avoidance and depressive symptoms and association to health behaviors among adolescents during brief guided online acceptance and commitment therapy. Journal of Contextual Behavioral Science, 22, 24-31. [DOI:10.1016/j.jcbs.2021.08.002]
Kim, S., & Kim, S. (2020). Analysis of the Impact of Health Beliefs and Resource Factors on Preventive Behaviors against the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 17(22), 8666. [DOI:10.3390/ijerph17228666] [PMID]
Kim, J. H., Shin, S., & Park, J. H. (2015). A methodological quality assessment of South Korean nursing research using structural equation modeling in South Korea. Journal of Korean Academy of Nursing, 45(2), 159-168. [Link]
Kingston, J., Clarke, S., & Remington, B. (2010). Experiential avoidance and problem behavior: A mediational analysis. Behavior Modification, 34(2), 145–163.[DOI:10.1177/0145445510362575] [PMID]
Kline, R. B. (2015). Principles and practice of structural equation modeling. New York: Guilford Publications. [Link]
Koszegi B. (2003). Health anxiety and patient behavior. Journal of Health Economics, 22(6), 1073–1084. [DOI:10.1016/j.jhealeco.2003.06.002] [PMID]
Lenzo, V., Sardella, A., Martino, G., & Quattropani, M. C. (2020). A systematic review of metacognitive beliefs in chronic medical conditions. Frontiers in Psychology, 10, 2875.[DOI:10.3389/fpsyg.2019.02875] [PMID] [PMCID]
Lovell, G. P., Nash, K., Sharman, R., & Lane, B. R. (2015). A cross-sectional investigation of depressive, anxiety, and stress symptoms and health-behavior participation in Australian university students. Nursing & Health Sciences, 17(1), 134–142. [DOI:10.1111/nhs.12147] [PMID]
Machell, K. A., Goodman, F. R., & Kashdan, T. B. (2015). Experiential avoidance and well-being: A daily diary analysis. Cognition & Emotion, 29(2), 351–359. [DOI:10.1080/02699931.2014.911143] [PMID]
Mao L. (2011). Evaluating the combined effectiveness of influenza control strategies and human preventive behavior. Plos One, 6(10), e24706. [DOI:10.1371/journal.pone.0024706] [PMID]
McEvoy, P. M., Moulds, M. L., & Mahoney, A. E. (2013). Mechanisms driving pre- and post-stressor repetitive negative thinking: metacognitions, cognitive avoidance, and thought control. Journal of Behavior Therapy and Experimental Psychiatry, 44(1), 84–93. [DOI:10.1016/j.jbtep.2012.07.011] [PMID]
Mohammadkhani, S., Akbari, M., Shahbahrami, M., Seydavi, M., & Kolubinski, D. C. (2023). Metacognitions about health in relation to coronavirus anxiety: The mediating role of Cognitive Attentional Syndrome And Distress Tolerance. Journal Of Rational-Emotive and Cognitive-Behavior Therapy : RET, 41(1), 222–236. [DOI:10.1007/s10942-022-00467-x] [PMID]
Nguyen, N. P. T., Hoang, T. D., Tran, V. T., Vu, C. T., Siewe Fodjo, J. N., & Colebunders, R., et al. (2020). Preventive behavior of vietnamese people in response to the COVID-19 pandemic. Plos One, 15(9), e0238830. [DOI:10.1371/journal.pone.0238830] [PMID]
Nunnally, J. C. (1967). Psychometric theory. New York: McGraw-Hill. [Link]
Riad, A., Huang, Y., Zheng, L., & Elavsky, S. (2020). COVID-19 induced anxiety and protective behaviors during COVID-19 outbreak: Scale development and validation. medRxiv, [Unpublished]. [DOI:10.2139/ssrn.3594370]
Roussis, P., & Wells, A. (2008). Psychological factors predicting stress symptoms: Metacognition, thought control, and varieties of worry. Anxiety, Stress, and Coping, 21(3), 213–225.[DOI:10.1080/10615800801889600] [PMID]
Shaw, R., Kim, Y. K., & Hua, J. (2020). Governance, technology and citizen behavior in pandemic: Lessons from COVID-19 in East Asia. Progress in Disaster Science, 6, 100090.[DOI:10.1016/j.pdisas.2020.100090] [PMID]
Shen, F., Min, C., Lu, Y., & Chu, Y. (2021). The effect of cognition and affect on preventive behaviors during the COVID-19 pandemic: A cross-sectional study in China. BMC Public Health, 21(1), 722. [DOI:10.1186/s12889-021-10784-y] [PMID]
Spada, M. M., Caselli, G., Nikčević, A. V., & Wells, A. (2015). Metacognition in addictive behaviors. Addictive Behaviors, 44, 9-15. [DOI:10.1016/j.addbeh.2014.08.002]
Ştefănuţ, A. M., Vintilă, M., Tomiţă, M., Treglia, E., Lungu, M. A., & Tomassoni, R. (2021). The influence of health beliefs, of resources, of vaccination history, and of health anxiety on intention to accept COVID-19 vaccination. Frontiers in Psychology, 12, 729803. [DOI:10.3389/fpsyg.2021.729803] [PMID]
Strine, T. W., Chapman, D. P., Kobau, R., & Balluz, L. (2005). Associations of self-reported anxiety symptoms with health-related quality of life and health behaviors. Social Psychiatry and Psychiatric Epidemiology, 40(6), 432-438. [DOI:10.1007/s00127-005-0914-1] [PMID]
Suls, J., & Fletcher, B. (1985). The relative efficacy of avoidant and nonavoidant coping strategies: A meta-analysis. Health Psychology, 4(3), 249–288. [DOI:10.1037/0278-6133.4.3.249] [PMID]
Taylor S. (2022). The psychology of pandemics. Annual Review of Clinical Psychology, 18, 581–609. [DOI:10.1146/annurev-clinpsy-072720-020131] [PMID]
Toussaint, L. L., Cheadle, A. D., Fox, J., & Williams, D. R. (2020). Clean and contain: Initial development of a measure of infection prevention behaviors during the COVID-19 pandemic. Annals of Behavioral Medicine, 54(9), 619–625. [DOI:10.1093/abm/kaaa064] [PMID]
Tyrer, P., Cooper, S., Crawford, M., Dupont, S., Green, J., & Murphy, D., et al. (2011). Prevalence of health anxiety problems in medical clinics. Journal of Psychosomatic Research, 71(6), 392–394. [DOI:10.1016/j.jpsychores.2011.07.004] [PMID]
Waltz, T. J., & Hayes, S. C. (2010). Acceptance and commitment therapy. In A. Freeman, M. A. Reinecke, & N. Kazantzis (Eds.) Cognitive and Behavioral Theories in Clinical Practice. New York: Guilford Press. [Link]
Wells, A. (2011). Metacognitive therapy for anxiety and depression. New York: Guilford Press. [Link]
Wells, A., & Matthews, G. (1996). Modelling cognition in emotional disorder: The S-REF model. Behaviour Research and Therapy, 34(11-12), 881-888. [DOI:10.1016/S0005-7967(96)00050-2]
Woolrich, R. A., Cooper, M. J., & Turner, H. M. (2008). Metacognition in patients with anorexia nervosa, dieting and non-dieting women: A preliminary study. European Eating Disorders Review, 16(1), 11–20. [DOI:10.1002/erv.802] [PMID]
Type of Study: Original Research Article |
Subject:
Cognitive behavioral
Received: 2023/01/22 | Accepted: 2023/08/30 | Published: 2024/01/1
Received: 2023/01/22 | Accepted: 2023/08/30 | Published: 2024/01/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








