Volume 6, Issue 3 (Summer 2018)
PCP 2018, 6(3): 143-152 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mowlaie M, Hajloo N, Sadeghi Hashjin G, Mikaeili N, Heidari S. The Effectiveness of Empathic Dynamic Psychotherapy and Anxiety-Regulating Psychodynamic Therapy in Treating Adult Separation Anxiety Disorder. PCP 2018; 6 (3) :143-152
URL: http://jpcp.uswr.ac.ir/article-1-526-en.html
URL: http://jpcp.uswr.ac.ir/article-1-526-en.html
1- Department of Psychology, Faculty of Educational Sciences and Psychology, University of Mohaghegh Ardabili, Ardabil, Iran.
2- Department of Psychology, Faculty of Educational Sciences and Psychology, University of Mohaghegh Ardabili, Ardabil, Iran. ,Hajloo53@uma.ac.ir
3- Department of Veterinary Medicine, Faculty of Veterinary Medicine, University of Tehran, Tehran, Iran.
4- Department of Psychology, Faculty of Educational Sciences and Psychology, Payame Noor University, Amol, Iran.
2- Department of Psychology, Faculty of Educational Sciences and Psychology, University of Mohaghegh Ardabili, Ardabil, Iran. ,
3- Department of Veterinary Medicine, Faculty of Veterinary Medicine, University of Tehran, Tehran, Iran.
4- Department of Psychology, Faculty of Educational Sciences and Psychology, Payame Noor University, Amol, Iran.
Full-Text [PDF 709 kb]
(2889 Downloads)
| Abstract (HTML) (8808 Views)
Full-Text: (3093 Views)
1. Introduction
Separation Anxiety (SA) is a severe, chronic, and disabling anxiety disorder (Kessler et al., 2006). Research has confirmed that SA and SA Disorders (SAD) are prevalent among adults; according to a WHO study, 43% of patients with SAD report adult onset of symptoms (Milord, 2015; Silove, Lonso Bromet, Grunber, Sampson, & Scott, 2015). The new DSM-V considers Adult Separation Anxiety Disorder (ASAD) as a diagnosis separate from childhood SAD and facilitates its diagnosis and treatment (APA, 2013), Comorbid ASAD is characterized by panic disorder, agoraphobia, and generalized anxiety. Silove & Rees (2014) reported that individuals with ASAD have symptoms similar to those of childhood SAD, such as feeling threat of separation from attachment figures, continuing intimate relationship with attachment figures, and excessive worry. SA is characterized by chronic anxiety, fear, or avoidance behavior upon separation from attachment figures. When these symptoms are present for at least 6 months in adults, the disorder is diagnosed as ASAD (Rochester & Baldwin, 2015). The symptoms in individuals with ASAD begin in adulthood, without any symptom in childhood ((Rochester & Baldwin, 2015). Shear, Jin, Ruscio, Walters and Kessler (2006) reported the lifetime prevalence of ASAD as 6.6%. These reports indicate that SA could have adult onset (Mayseless & Scher, 2000), whereas Manicavasagar, Silove, Curtis and Wagner (2000) believed that childhood SAD could continue into adulthood.
It has been shown that individuals with severe ASAD have a high score on the neuroticism scale of NEO-PI (Silove, Marnane, Wagner, & Manicavasagar, 2011) as well as high comorbidity with panic disorder and agoraphobia compared with individuals with other anxiety disorders (Silove, Marnane, Wagner, Manicavasagar, & Rees, 2010). The combination of mood disorders and SADis highly prevalent, and such patients show poor treatment response (Rochester & Baldwin, 2015); reportedly, patients with mood disorders show significantly high scores on the Adult Separation Anxiety questionnaire (ASA-27), and a significant positive correlation has also been found between the ASA-27 total score and depression (r=0.34) (Carmassia et al., 2015). In addition, patients with SAD constantly feel negative emotions, such as loss, loneliness, and sadness, that are normally experienced by individuals when they are separated from an important person in their life (Hock, McBride, & Gnezda, 1989). These findings indicate that ASAD patients are prone to severe depression and anxiety.
ASAD is considered as an important disorder because reportedly, 20%–40% adults with other anxiety and mood disorders exhibit its symptoms (Bögels, Knappe, & Clark, 2013). Although many pharmacological and psychological therapies are effective in ameliorating childhood SA, in most cases, these therapies fail to completely prevent the symptoms. Patients with ASAD exhibit high levels of dysfunction and poor response to conventional treatments, such as pharmacological and psychological therapies (Copeland, Angold, & Shanahan, 2014), compared with those with other anxiety disorders (Miniati, Calugi, & Rucci, 2012). Thus, these therapies are not effective in treating ASAD. This evidence indicates that there is a need to develop novel and in-depth interventions for treating ASAD.
A growing body of evidence has indicated that dynamic psychotherapies are effective in treating anxiety disorders (Ferrero et al., 2007; Leichsenring & Salzer, 2014; Busch & Milord, 2015; Knekt et al., 2008; Knekt et al., 2015). Dynamic psychotherapies for anxiety disorders, especially childhood SAD, have shown promising results in reducing anxiety and depression; therefore, based on these therapies, different types of interventions should be developed to treat ASAD. Most studies on the effectiveness of psychotherapy on SAD have focused on childhood SAD. Only one study has been conducted on ASAD that has shown promising results of Panic-Focused Psychodynamic Psychotherapy-Extended Range in treating SAD in a 21-session treatment (Busch & Milord, 2015). Because in ASAD patients, it is necessary to address anxiety, depression, and guilt as well as rejection experienced in their past, Brief Empathic Psychotherapy (BEP) (Seruya, 1997) and anxiety-regulating dynamic psychotherapy or Affect Phobia Therapy (APT) (McCullough et al., 2003), which are targeted dynamic psychotherapies, have proven to be successful. In BEP, empathy is the fundamental approach to cope with depression and anxiety, and self-object needs are actively satisfied. In APT, affect phobias, such as sense of guilt, rejection, hatred, and damaged emotional relatedness, in ASAD patients are examined and treated via defense, exposure to affects, and self-esteem reconstruction.
To build on the above-mentioned studies, we tested four major hypotheses. Hypothesis 1 states that BEP significantly reduces anxiety. Hypothesis 2 state that BEP significantly reduces depression. Hypothesis 3 states that APT significantly reduces anxiety. Hypothesis 4 states that APT significantly reduces depression. We also conducted a 2-month follow-up assessment to define the stability of the effectiveness of these therapies. Most previous studies have focused on testing only one type of dynamic treatment on one ASAD patient. By contrast, the present research evaluated two types of dynamic psychotherapies (BEP and APT) on a sample of university students and included a follow-up assessment. Thus, the present research was aimed to examine the effectiveness of BEP and APT in reducing depression and anxiety and the differences in their effectiveness in a sample of Iranian students with ASAD symptoms.
2. Methods
The present study had an experimental design involving pre-treatment, post-treatment, and follow-up assessments. Iranian university students with ASAD symptoms were screened using the ASA-27 questionnaire for inclusion in this study. In total, 573 students completed ASA-27, 120 of whom met the inclusion criteria and were recruited for interviews. Eventually, a total of 30participantswith ASA-27 scores of >22 and Global Assessment of Functioning (GAF) scores of >50 (determined by structured clinical interviews) were randomly assigned to BEP (n=10), APT (n=10), and control (n=10) groups. Participants with ASA-27 scores of >22 (Manicavasagar, Silove, Wagner, & Drobny, 2003) were considered to have ASAD. Questionnaires were administered in pre-treatment, post-treatment, and follow-up sessions. BEP and APT were provided to the experimental groups in 12 sessions over 4 weeks. The study protocol was approved by the ethical committee of Ardabil University of Medical Sciences (IR.ARUMS.REC.1396.257) and was explained to the participants before obtaining written informed consent during the pre-treatment assessment. The participation of students in the research was completely voluntarily, and they were free to opt out of the research at any time.
Inclusion criteria were as follows: ASA symptoms (according to the result of structured interview and ASA-27 scores of >22 ); GAF scores of >50; moderate deficiency in performance; no psychical diseases; no other psychological disorders; no current use of psychological, pharmacology, or other psychotherapies, and psychological mindedness or the ability to use psychodynamic therapy. Exclusion criteria were as follows: chemical dependency or substance abuse, severe psychical disease or chronic life stressors, poor impulse control, comorbidity with Cluster B personality disorders such as borderline or narcissistic personality disorders, or any other Axis I DSM-IV-TR diagnosis.
Seruya (1997) conducted BEP model upon self-psychology that sexuality and aggression are no longer seen as the basic drives of psyche, so self-psychology is the core concept in this approach. Empathy and empathic listening are crucial parts of this treatment strategy that includes more active involvement of the therapist (in interpretation and psychoeducation) and participants (in asking questions and showing curiosity about themselves) than in other approaches. The therapist responds to the self-object needs of the patients by interpreting patient’s other relationships in his self-self-object milieu.
The first phase(sessions1–3) includes examining feelings (positive or negative) about coming for treatment, expectations, and narcissistic injuries; exploring fears of dependency and shame; defining focal goals; examining self-state, including vitality-depletion and cohesive-fragmentation; using the triangle of insight for recognizing interpersonal relationships; examining appropriate and inappropriate adaptive strategies of patients; tracking the connection between affective reactions of patients, their expectations from themselves, and upcoming behaviors; educating about the attachment concept; and helping patients recognize their attachment in intimate relationships.
The therapeutic alliances between the therapist and patients are an important component in these sessions. The middle phase (sessions 4–10) of the treatment includes examining transference and countertransference; educating about empathic introspection as a way to explore themselves and their defects; evaluating self-state of patients and their ability to comprehend their own experiences; examining and explaining the relationship between patients’ experiences from responded needs and their positive effects on self-state as well as between non-reopened needs and their negative effects on self-state, such as self-confidence, self-concept, and expectances; and recognizing protective defenses, distorted expectances, and maladaptive interpersonal behavioral patterns. The final phase (sessions 11-12) are focused on meeting focal goals, identifying and starting to modify the specific maladaptive affective and cognitive intrapsychic patterns, understanding the self-psychological issues underlying the presenting problems, reducing the vulnerabilities around the focal issues, examining dependency on the therapist prevalent in final sessions, and emphasizing on increasing protective self-object milieu and decreasing dependency on attachment figures.
Another model was APT model which was described by McCullough et al. (2003) in psychodynamic theory. This model follows Malan’s triangle of conflict and triangle of persons. In this model, the therapist asks about the patient’s feelings and defenses and tries to clarify and observe the underlying affects related to the current behavior. This treatment includes three phases: defense restructuring (recognizing and releasing maladaptive defenses), affect restructuring (desensitization to fearful affects through exposure to conflicted feelings), and self/other restructuring (improvement of the sense of self and relationship with others).
Desensitization of internal phobias is the core technique. Patients are recurrently exposed to intense fearful affects, such as anger, loss, and compassion. This exposure continues till the time they are able to experience any level of adaptive feelings with less inhibition (anxiety, guilt, shame, and pain). The first phase (sessions 1–3) includes recognizing underlying affect phobia (inhibited and activated affects); checking phobic responses, blocked feelings, and anxieties; and formulating phobias in affect phobia framework. The middle phase (sessions 4–10) includes exploring affect phobia patterns; educating about the triangle of conflicts to examine the underlying affect phobia; recognizing adaptive activated feelings, anxieties, inhibitions, and causes of inhibitions from adaptive feelings; changing defenses from egosyntonic to egodystonic; educating about empathy to themselves; exposing to defenses and interpretations; releasing maladaptive defenses and desensitization to fearful affects (exposing to frightening feelings and response prevention); regulating anxiety and fears related to experiencing affects; and encouraging to express affects.
The final phase (sessions 11-12) includes reducing anxieties related to adaptive feelings about themselves; creating capacity for feelings related to the self and others; changing the attitude about themselves; encouraging them to imagine themselves in relation to others; reconstructing affect phobia with focus on others; expressing emotions as adaptive expression of feelings, demands, and needs in relationship to the therapist and others; educating skills related to the self and others, with more focus on balancing people skills; checking and evaluating affect phobia solutions. Instruments used were ASA-27, Depression, anxiety, and stress scale-21 (DASS-21), Structured Clinical Interview for SA Symptoms (SCI-SAS), GAF.
ASA-27 is a 27-item self-report questionnaire developed by Manicavasagar et al. (2003) to assess ASAD. The items are rated from 0 (this never happens) to 3 (this happens all the time). Scores of >22 indicate clinically significant levels of ASA; this cut-off score has been reported to have high sensitivity (81%) and specificity (84%) (Manicavasagar et al, 2003). In another study conducted by Dirioz, Alkin, Yemez, Onur, and Eminagaoglu (2012) in Turkey, ASA-27 was shown to have high degree of internal consistency (Cronbach’s α=0.93) and good test–retest reliability. In one study in Iran, the internal consistency reliability coefficient was found to be 0.87 and content validity was confirmed by five practitioners (Khorshidvand, Rahimian Boogar, & Talepasand, 2015). In the present research, Cronbach’s α for the entire scale was 0.90 and for five subscales was 0.88, 0.90, 0.78, 0.87, and 0.91, respectively.
DASS-21 is a 21-item self-report questionnaire designed to assess distress along three axes, namely depression, anxiety, and stress (Lovibond & Lovibond, 1995). The depression subscale of DASS (DASS-D) scores of 0–9 indicate normal, 10–13 indicate mild, 14–20 indicate moderate, 21–27 indicate severe, and +28 indicate extremely severe depression; the anxiety subscale of DASS (DASS-A) scores of 0–7 indicate normal, 8-9 indicate mild, 10–14 indicate moderate, 15–19 indicate severe, and +20 indicate extremely severe anxiety. Reliability and validity of this scale have previously confirmed (Tran, Tran, & Fisher, 2013; Trauer, Dodd, Callaly, Campbell, & Berk, 2007). Two subscales of depression and anxiety were used in this study. Sahebi, Asghari and Salari (2005) reported high α coefficients of 0.77, 0.79, and 0.78 for depression, anxiety, and stress subscales, respectively. In the present research, Cronbach’s α for the DASS-21 scale was 0.89 and for the subscales depression and anxiety was 0.86 and 0.89, respectively.
SCI-SAS is a scale for assessing all symptoms of SAD in ASA (Cyranowski et al., 2002). Eight-criterion symptoms of SAD in DSM-IV have been rated for SCI-SAS and scored from 0 (not at all), 1 (sometimes), 2 (often), or ? (do not recall); three or more of these symptoms indicate the threshold to determine a diagnosis of ASAD. Cyranowski (2002) have reported that this scale has excellent psychometric properties, such as good internal consistency and convergent and discriminate validities.
GAF (Sass, 2003) is a numeric scale that assesses global functioning, which comprises psychological, social, and vocational functioning. Scores range from 1 (minimum level of functioning) to 100 (maximum level of functioning and lack of any symptoms). Its reliability has been proven by Startup, Jackson and Bendix (2002). To test our hypotheses, all statistical analyses were performed using SPSS 22. Repeated measures analysis of variance (ANOVA) was used to examine the difference in variables between the three groups. Kolmogorov–Smirnov test was used to test the normality of the data distribution. Levene’s test was used to evaluate the homogeneity of variance.
3. Results
All participants were females and BSc students, with mean age of 20.93±1.50 (range, 19–26) years; 76.66% of the participants were single and 23.33% were married. Further, 59.9% of the participants were studying in the field of human sciences, 29.99% in engineering, and 9.9% in basic sciences. The Kolmogorov–Smirnov test (P<0.05) revealed that the data distribution followed normal distribution. The Levene’s test showed that the null hypothesis was accepted and homogeneity of variance was met (P>0.05).
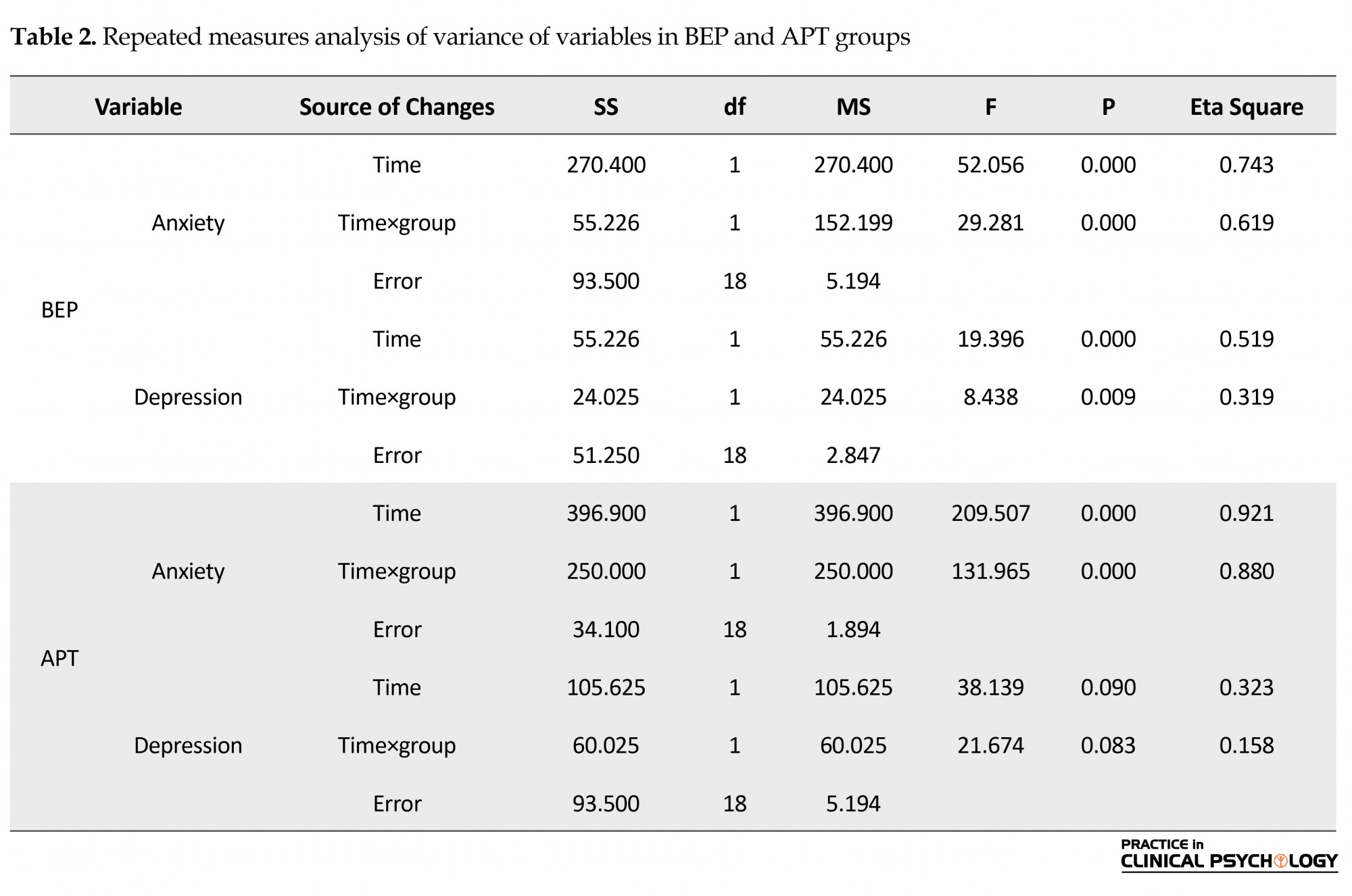
The mean and standard deviations of pre-treatment, post-treatment, and follow-up assessments in the three groups are presented in Table 1, and inferential statistics using repeated measures ANOVA is shown in Table 2.
Separation Anxiety (SA) is a severe, chronic, and disabling anxiety disorder (Kessler et al., 2006). Research has confirmed that SA and SA Disorders (SAD) are prevalent among adults; according to a WHO study, 43% of patients with SAD report adult onset of symptoms (Milord, 2015; Silove, Lonso Bromet, Grunber, Sampson, & Scott, 2015). The new DSM-V considers Adult Separation Anxiety Disorder (ASAD) as a diagnosis separate from childhood SAD and facilitates its diagnosis and treatment (APA, 2013), Comorbid ASAD is characterized by panic disorder, agoraphobia, and generalized anxiety. Silove & Rees (2014) reported that individuals with ASAD have symptoms similar to those of childhood SAD, such as feeling threat of separation from attachment figures, continuing intimate relationship with attachment figures, and excessive worry. SA is characterized by chronic anxiety, fear, or avoidance behavior upon separation from attachment figures. When these symptoms are present for at least 6 months in adults, the disorder is diagnosed as ASAD (Rochester & Baldwin, 2015). The symptoms in individuals with ASAD begin in adulthood, without any symptom in childhood ((Rochester & Baldwin, 2015). Shear, Jin, Ruscio, Walters and Kessler (2006) reported the lifetime prevalence of ASAD as 6.6%. These reports indicate that SA could have adult onset (Mayseless & Scher, 2000), whereas Manicavasagar, Silove, Curtis and Wagner (2000) believed that childhood SAD could continue into adulthood.
It has been shown that individuals with severe ASAD have a high score on the neuroticism scale of NEO-PI (Silove, Marnane, Wagner, & Manicavasagar, 2011) as well as high comorbidity with panic disorder and agoraphobia compared with individuals with other anxiety disorders (Silove, Marnane, Wagner, Manicavasagar, & Rees, 2010). The combination of mood disorders and SADis highly prevalent, and such patients show poor treatment response (Rochester & Baldwin, 2015); reportedly, patients with mood disorders show significantly high scores on the Adult Separation Anxiety questionnaire (ASA-27), and a significant positive correlation has also been found between the ASA-27 total score and depression (r=0.34) (Carmassia et al., 2015). In addition, patients with SAD constantly feel negative emotions, such as loss, loneliness, and sadness, that are normally experienced by individuals when they are separated from an important person in their life (Hock, McBride, & Gnezda, 1989). These findings indicate that ASAD patients are prone to severe depression and anxiety.
ASAD is considered as an important disorder because reportedly, 20%–40% adults with other anxiety and mood disorders exhibit its symptoms (Bögels, Knappe, & Clark, 2013). Although many pharmacological and psychological therapies are effective in ameliorating childhood SA, in most cases, these therapies fail to completely prevent the symptoms. Patients with ASAD exhibit high levels of dysfunction and poor response to conventional treatments, such as pharmacological and psychological therapies (Copeland, Angold, & Shanahan, 2014), compared with those with other anxiety disorders (Miniati, Calugi, & Rucci, 2012). Thus, these therapies are not effective in treating ASAD. This evidence indicates that there is a need to develop novel and in-depth interventions for treating ASAD.
A growing body of evidence has indicated that dynamic psychotherapies are effective in treating anxiety disorders (Ferrero et al., 2007; Leichsenring & Salzer, 2014; Busch & Milord, 2015; Knekt et al., 2008; Knekt et al., 2015). Dynamic psychotherapies for anxiety disorders, especially childhood SAD, have shown promising results in reducing anxiety and depression; therefore, based on these therapies, different types of interventions should be developed to treat ASAD. Most studies on the effectiveness of psychotherapy on SAD have focused on childhood SAD. Only one study has been conducted on ASAD that has shown promising results of Panic-Focused Psychodynamic Psychotherapy-Extended Range in treating SAD in a 21-session treatment (Busch & Milord, 2015). Because in ASAD patients, it is necessary to address anxiety, depression, and guilt as well as rejection experienced in their past, Brief Empathic Psychotherapy (BEP) (Seruya, 1997) and anxiety-regulating dynamic psychotherapy or Affect Phobia Therapy (APT) (McCullough et al., 2003), which are targeted dynamic psychotherapies, have proven to be successful. In BEP, empathy is the fundamental approach to cope with depression and anxiety, and self-object needs are actively satisfied. In APT, affect phobias, such as sense of guilt, rejection, hatred, and damaged emotional relatedness, in ASAD patients are examined and treated via defense, exposure to affects, and self-esteem reconstruction.
To build on the above-mentioned studies, we tested four major hypotheses. Hypothesis 1 states that BEP significantly reduces anxiety. Hypothesis 2 state that BEP significantly reduces depression. Hypothesis 3 states that APT significantly reduces anxiety. Hypothesis 4 states that APT significantly reduces depression. We also conducted a 2-month follow-up assessment to define the stability of the effectiveness of these therapies. Most previous studies have focused on testing only one type of dynamic treatment on one ASAD patient. By contrast, the present research evaluated two types of dynamic psychotherapies (BEP and APT) on a sample of university students and included a follow-up assessment. Thus, the present research was aimed to examine the effectiveness of BEP and APT in reducing depression and anxiety and the differences in their effectiveness in a sample of Iranian students with ASAD symptoms.
2. Methods
The present study had an experimental design involving pre-treatment, post-treatment, and follow-up assessments. Iranian university students with ASAD symptoms were screened using the ASA-27 questionnaire for inclusion in this study. In total, 573 students completed ASA-27, 120 of whom met the inclusion criteria and were recruited for interviews. Eventually, a total of 30participantswith ASA-27 scores of >22 and Global Assessment of Functioning (GAF) scores of >50 (determined by structured clinical interviews) were randomly assigned to BEP (n=10), APT (n=10), and control (n=10) groups. Participants with ASA-27 scores of >22 (Manicavasagar, Silove, Wagner, & Drobny, 2003) were considered to have ASAD. Questionnaires were administered in pre-treatment, post-treatment, and follow-up sessions. BEP and APT were provided to the experimental groups in 12 sessions over 4 weeks. The study protocol was approved by the ethical committee of Ardabil University of Medical Sciences (IR.ARUMS.REC.1396.257) and was explained to the participants before obtaining written informed consent during the pre-treatment assessment. The participation of students in the research was completely voluntarily, and they were free to opt out of the research at any time.
Inclusion criteria were as follows: ASA symptoms (according to the result of structured interview and ASA-27 scores of >22 ); GAF scores of >50; moderate deficiency in performance; no psychical diseases; no other psychological disorders; no current use of psychological, pharmacology, or other psychotherapies, and psychological mindedness or the ability to use psychodynamic therapy. Exclusion criteria were as follows: chemical dependency or substance abuse, severe psychical disease or chronic life stressors, poor impulse control, comorbidity with Cluster B personality disorders such as borderline or narcissistic personality disorders, or any other Axis I DSM-IV-TR diagnosis.
Seruya (1997) conducted BEP model upon self-psychology that sexuality and aggression are no longer seen as the basic drives of psyche, so self-psychology is the core concept in this approach. Empathy and empathic listening are crucial parts of this treatment strategy that includes more active involvement of the therapist (in interpretation and psychoeducation) and participants (in asking questions and showing curiosity about themselves) than in other approaches. The therapist responds to the self-object needs of the patients by interpreting patient’s other relationships in his self-self-object milieu.
The first phase(sessions1–3) includes examining feelings (positive or negative) about coming for treatment, expectations, and narcissistic injuries; exploring fears of dependency and shame; defining focal goals; examining self-state, including vitality-depletion and cohesive-fragmentation; using the triangle of insight for recognizing interpersonal relationships; examining appropriate and inappropriate adaptive strategies of patients; tracking the connection between affective reactions of patients, their expectations from themselves, and upcoming behaviors; educating about the attachment concept; and helping patients recognize their attachment in intimate relationships.
The therapeutic alliances between the therapist and patients are an important component in these sessions. The middle phase (sessions 4–10) of the treatment includes examining transference and countertransference; educating about empathic introspection as a way to explore themselves and their defects; evaluating self-state of patients and their ability to comprehend their own experiences; examining and explaining the relationship between patients’ experiences from responded needs and their positive effects on self-state as well as between non-reopened needs and their negative effects on self-state, such as self-confidence, self-concept, and expectances; and recognizing protective defenses, distorted expectances, and maladaptive interpersonal behavioral patterns. The final phase (sessions 11-12) are focused on meeting focal goals, identifying and starting to modify the specific maladaptive affective and cognitive intrapsychic patterns, understanding the self-psychological issues underlying the presenting problems, reducing the vulnerabilities around the focal issues, examining dependency on the therapist prevalent in final sessions, and emphasizing on increasing protective self-object milieu and decreasing dependency on attachment figures.
Another model was APT model which was described by McCullough et al. (2003) in psychodynamic theory. This model follows Malan’s triangle of conflict and triangle of persons. In this model, the therapist asks about the patient’s feelings and defenses and tries to clarify and observe the underlying affects related to the current behavior. This treatment includes three phases: defense restructuring (recognizing and releasing maladaptive defenses), affect restructuring (desensitization to fearful affects through exposure to conflicted feelings), and self/other restructuring (improvement of the sense of self and relationship with others).
Desensitization of internal phobias is the core technique. Patients are recurrently exposed to intense fearful affects, such as anger, loss, and compassion. This exposure continues till the time they are able to experience any level of adaptive feelings with less inhibition (anxiety, guilt, shame, and pain). The first phase (sessions 1–3) includes recognizing underlying affect phobia (inhibited and activated affects); checking phobic responses, blocked feelings, and anxieties; and formulating phobias in affect phobia framework. The middle phase (sessions 4–10) includes exploring affect phobia patterns; educating about the triangle of conflicts to examine the underlying affect phobia; recognizing adaptive activated feelings, anxieties, inhibitions, and causes of inhibitions from adaptive feelings; changing defenses from egosyntonic to egodystonic; educating about empathy to themselves; exposing to defenses and interpretations; releasing maladaptive defenses and desensitization to fearful affects (exposing to frightening feelings and response prevention); regulating anxiety and fears related to experiencing affects; and encouraging to express affects.
The final phase (sessions 11-12) includes reducing anxieties related to adaptive feelings about themselves; creating capacity for feelings related to the self and others; changing the attitude about themselves; encouraging them to imagine themselves in relation to others; reconstructing affect phobia with focus on others; expressing emotions as adaptive expression of feelings, demands, and needs in relationship to the therapist and others; educating skills related to the self and others, with more focus on balancing people skills; checking and evaluating affect phobia solutions. Instruments used were ASA-27, Depression, anxiety, and stress scale-21 (DASS-21), Structured Clinical Interview for SA Symptoms (SCI-SAS), GAF.
ASA-27 is a 27-item self-report questionnaire developed by Manicavasagar et al. (2003) to assess ASAD. The items are rated from 0 (this never happens) to 3 (this happens all the time). Scores of >22 indicate clinically significant levels of ASA; this cut-off score has been reported to have high sensitivity (81%) and specificity (84%) (Manicavasagar et al, 2003). In another study conducted by Dirioz, Alkin, Yemez, Onur, and Eminagaoglu (2012) in Turkey, ASA-27 was shown to have high degree of internal consistency (Cronbach’s α=0.93) and good test–retest reliability. In one study in Iran, the internal consistency reliability coefficient was found to be 0.87 and content validity was confirmed by five practitioners (Khorshidvand, Rahimian Boogar, & Talepasand, 2015). In the present research, Cronbach’s α for the entire scale was 0.90 and for five subscales was 0.88, 0.90, 0.78, 0.87, and 0.91, respectively.
DASS-21 is a 21-item self-report questionnaire designed to assess distress along three axes, namely depression, anxiety, and stress (Lovibond & Lovibond, 1995). The depression subscale of DASS (DASS-D) scores of 0–9 indicate normal, 10–13 indicate mild, 14–20 indicate moderate, 21–27 indicate severe, and +28 indicate extremely severe depression; the anxiety subscale of DASS (DASS-A) scores of 0–7 indicate normal, 8-9 indicate mild, 10–14 indicate moderate, 15–19 indicate severe, and +20 indicate extremely severe anxiety. Reliability and validity of this scale have previously confirmed (Tran, Tran, & Fisher, 2013; Trauer, Dodd, Callaly, Campbell, & Berk, 2007). Two subscales of depression and anxiety were used in this study. Sahebi, Asghari and Salari (2005) reported high α coefficients of 0.77, 0.79, and 0.78 for depression, anxiety, and stress subscales, respectively. In the present research, Cronbach’s α for the DASS-21 scale was 0.89 and for the subscales depression and anxiety was 0.86 and 0.89, respectively.
SCI-SAS is a scale for assessing all symptoms of SAD in ASA (Cyranowski et al., 2002). Eight-criterion symptoms of SAD in DSM-IV have been rated for SCI-SAS and scored from 0 (not at all), 1 (sometimes), 2 (often), or ? (do not recall); three or more of these symptoms indicate the threshold to determine a diagnosis of ASAD. Cyranowski (2002) have reported that this scale has excellent psychometric properties, such as good internal consistency and convergent and discriminate validities.
GAF (Sass, 2003) is a numeric scale that assesses global functioning, which comprises psychological, social, and vocational functioning. Scores range from 1 (minimum level of functioning) to 100 (maximum level of functioning and lack of any symptoms). Its reliability has been proven by Startup, Jackson and Bendix (2002). To test our hypotheses, all statistical analyses were performed using SPSS 22. Repeated measures analysis of variance (ANOVA) was used to examine the difference in variables between the three groups. Kolmogorov–Smirnov test was used to test the normality of the data distribution. Levene’s test was used to evaluate the homogeneity of variance.
3. Results
All participants were females and BSc students, with mean age of 20.93±1.50 (range, 19–26) years; 76.66% of the participants were single and 23.33% were married. Further, 59.9% of the participants were studying in the field of human sciences, 29.99% in engineering, and 9.9% in basic sciences. The Kolmogorov–Smirnov test (P<0.05) revealed that the data distribution followed normal distribution. The Levene’s test showed that the null hypothesis was accepted and homogeneity of variance was met (P>0.05).
The mean and standard deviations of pre-treatment, post-treatment, and follow-up assessments in the three groups are presented in Table 1, and inferential statistics using repeated measures ANOVA is shown in Table 2.
Descriptive findings
The mean scores (±standard deviation) of the depression and anxiety subscales are shown in Table 1. Results of repeated measures ANOVA on the effectiveness of BEP and APT on depression and anxiety are shown in Table 2. In the BEP group, the effects of time on the anxiety score (F=52.056, P=0.000) and depression score (F=24.025, P=0.009) were more significant than those in the control group (F=32.24, P=0.09). These results also revealed significant differences in the anxiety and depression scores between pre-treatment, post-treatment, and follow-up stages, indicating significant effects of BEP. Moreover, in the APT group, the effects of time were significant on the anxiety score (F=209.507, P=0.000) but not on the depression score (F=38.139, P=0.08), indicating no difference in the depression score between the APT and control groups (F=36.16, P=0.07).
4. Discussion
The present research investigated the effectiveness of BEP and APT in reducing depression and anxiety in university students with ASAD symptoms. To our knowledge, this is the first study to examine two types of dynamic psychotherapies on ASAD and showing their ameliorating effects on the depression and anxiety symptoms in Iranian ASAD patients. We found a significant reduction in anxiety by BEP (Hypothesis 1) and APT (Hypothesis 3) in post-treatment and follow-up assessments. Moreover, we found a significant reduction in depression by BEP (Hypothesis 2) but not by APT (Hypothesis 4) in post-treatment and follow-up assessments.
Consistent with Hypothesis 1, BEP was significantly effective in reducing anxiety, which confirms the previous finding on the effectiveness of BEP on anxiety (Heidari, Lewis, Allahyari, Azadfallah, & Bertino, 2013). In this therapy, the therapist empathetically immerses him/herself in the subjective world of the patients. This method is useful in reducing anxiety in patients caused by severe insecurity and fear of rejection. The self-object needs of patients are met using nonjudgmental attitude, therapeutic alliances, optimistic view, and growth-oriented attitude. The patients use empathic introspection to deal with their anxieties. Significant reduction in anxiety was observed in these patients using exposure to conflicted feelings as well as clarifications and interpretations of the maladaptive defenses, repetitive behavioral patterns, unconscious conflicts and fears about dependency, shame, and emotional expression.
The patients use the therapeutic relationship as an opportunity to better comprehend themselves, test their fears of assertiveness, and become assertive to the point where they are not evaluated with criticism, punishment, and rejection in their life anymore. In addition, the main reason contributing to this effectiveness is that the therapist responses empathetically to patients’ critical feelings and poor relationships, leading to positive perception about themselves. To organize the intervention, the therapist uses the triangle of conflict and the triangle of insight to formulate the problems. The patients use the interpretation of these triangles to integrate internal and external experiences; they also explore their sense of guilt and anxiety and try reducing them using the triangle of conflict. The therapist here aims to help patients internalize psychological functions, such as regulating emotions and increasing energy, and build a sustainable self-object milieu (Seruya, 1997).
Consistent with the previous findings (Johansson, Bjorklund, Hornborg, & Anderson 2013; Leichsenring et al, 2014; Swartz et al., 2016) and Hypothesis 2, BEP was significantly effective in reducing depression. There are some explanations for this finding. First, the approach used in BEP is of empathy; therefore, the supportive behavior and active involvement of the therapist (Seruya, 1997) must have been effective in treating depression. In BEP, such empathic relationship is of importance as it leads to empathic self-object changes in the patients that initiate the internalization of aliveness, hope, and happiness, ultimately improving object relatedness. Patients benefit from this approach because their feelings of uniqueness and specialness are fostered. Further, in our research, most participants were 19–30 years old and were females; this is explained by the previous finding that age and gender predict better outcome of short-term psychodynamic therapy in minor depression (Frank et al., 2002). Studies have shown that the female gender is highly correlated with better treatment outcome (Frank et al., 2002). Third explanation is that in the approach used in BEP, the therapist has more active involvement and attempts to identify the intrapsychic conflicts that led to depression. Depression in ASAD patients involves self-oriented aggression; therefore, empathic introspection that is learned during the therapy helps them develop a compassionate view about themselves.
The present research also showed that APT was significantly effective in reducing anxiety, consistent with Hypothesis 3 and previous findings (Johansson, Hesser, Ljótsson, Frederick, & Andersson, 2016; Maljanen et al., 2016; Abbass, Hancock, Henderson, & Kisely, 2014). In APT, the therapist helps patients via three strategies, including defense restructuring (recognizing and relinquishing maladaptive defenses), affect restructuring (desensitization to fearful affects via exposure to conflicted feeling), and self/other restructuring (promotion of the sense of self and relationship with others). In addition, in this model, anxiety is reduced through systematic desensitization (McCullough et al., 2003). In many anxiety disorders, such as SAD, pathological behaviors are manifested as defensive behavioral patterns that block adaptive coping strategies. In chronic anxiety, the defensive behaviors are inappropriate. To gradually desensitize the patients to fearful affects, the therapist gently shifts between exposing the patients with affects and encouraging them not to defend or avoid this process so as to help them cope with anxieties.
Lastly, our study finding ruled out Hypothesis 4, which stated that APT is effective in reducing depression. Thus, this result is not consistent with previous findings that confirmed the effectiveness of APT in reducing depression (Johansson et al., 2016; Johansson et al., 2013; Dornelas, Ferrand, & Stepnowski, 2010). Our result can be explained by the fact that APT focuses on desensitizing patients to affect phobias. Because our patients had severe anxiety, most of the therapy focused on fears and affect phobias related to their fears. Most of our patients had unconscious fears about being rejected by attachment figures, sense of pity about themselves, and conflicts about anxiety expression; therefore, in our study, APT focused on reducing anxiety using desensitization and not on depression.
Our research has some limitations that should be taken into account while interpreting the results. First, this study was the first one to use two interventions, and patients with severe ASAD were recruited instead of those with moderate ASAD; therefore, it is necessary to conduct a similar study on patients with moderate ASAD and compare its findings with ours. Second, all our participants were females; this limits the extrapolation of our findings to male patients. Therefore, future studies involving both genders are warranted. In addition, due to the time limit, a 2-month follow-up was conducted in the present research; therefore, a 6-month follow-up is recommended to examine long-term stability of such patients. Despite these limitations, this research demonstrated useful results of BEP and APT in ASAD. Both BEP and APT were found to be effective in reducing anxiety in the sample population, and BEP, but not APT, was also effective in reducing depression. We used not only a questionnaire to assess ASAD but also interviews to select subjects with severe ASAD. Our results highlight the potential of these interventions in treating depression and anxiety in ASAD patients. Because dynamic psychotherapies are highly effective in treating anxiety disorders, especially SAD, such intervention protocols, similar to those used in our research, should be designed for clinical use. In addition, due to the high prevalence of ASAD and its adverse effects on the quality of life of ASAD patients, it is necessary to accurately diagnose and treat such patients to improve their lifestyles, coping strategies, self-esteem, and well-being. These needs can be met using dynamic psychotherapies.
Ethical Considerations
Compliance with ethical guidelines
The present research is a part of first authors phd thesis and have ethical code from Ardabil university of medical sciences.
Funding
This article was part of the first author’s PhD thesis in the Department of Psychology and was financially supported by the research grant from the office of vice chancellor of the University of Mohaghegh Ardabili.
Conflicts of interest
The authors declare that they have no conflict of interest.
Acknowledgments
The authors would like to thank all university students who participated in this research.
References
The mean scores (±standard deviation) of the depression and anxiety subscales are shown in Table 1. Results of repeated measures ANOVA on the effectiveness of BEP and APT on depression and anxiety are shown in Table 2. In the BEP group, the effects of time on the anxiety score (F=52.056, P=0.000) and depression score (F=24.025, P=0.009) were more significant than those in the control group (F=32.24, P=0.09). These results also revealed significant differences in the anxiety and depression scores between pre-treatment, post-treatment, and follow-up stages, indicating significant effects of BEP. Moreover, in the APT group, the effects of time were significant on the anxiety score (F=209.507, P=0.000) but not on the depression score (F=38.139, P=0.08), indicating no difference in the depression score between the APT and control groups (F=36.16, P=0.07).
4. Discussion
The present research investigated the effectiveness of BEP and APT in reducing depression and anxiety in university students with ASAD symptoms. To our knowledge, this is the first study to examine two types of dynamic psychotherapies on ASAD and showing their ameliorating effects on the depression and anxiety symptoms in Iranian ASAD patients. We found a significant reduction in anxiety by BEP (Hypothesis 1) and APT (Hypothesis 3) in post-treatment and follow-up assessments. Moreover, we found a significant reduction in depression by BEP (Hypothesis 2) but not by APT (Hypothesis 4) in post-treatment and follow-up assessments.
Consistent with Hypothesis 1, BEP was significantly effective in reducing anxiety, which confirms the previous finding on the effectiveness of BEP on anxiety (Heidari, Lewis, Allahyari, Azadfallah, & Bertino, 2013). In this therapy, the therapist empathetically immerses him/herself in the subjective world of the patients. This method is useful in reducing anxiety in patients caused by severe insecurity and fear of rejection. The self-object needs of patients are met using nonjudgmental attitude, therapeutic alliances, optimistic view, and growth-oriented attitude. The patients use empathic introspection to deal with their anxieties. Significant reduction in anxiety was observed in these patients using exposure to conflicted feelings as well as clarifications and interpretations of the maladaptive defenses, repetitive behavioral patterns, unconscious conflicts and fears about dependency, shame, and emotional expression.
The patients use the therapeutic relationship as an opportunity to better comprehend themselves, test their fears of assertiveness, and become assertive to the point where they are not evaluated with criticism, punishment, and rejection in their life anymore. In addition, the main reason contributing to this effectiveness is that the therapist responses empathetically to patients’ critical feelings and poor relationships, leading to positive perception about themselves. To organize the intervention, the therapist uses the triangle of conflict and the triangle of insight to formulate the problems. The patients use the interpretation of these triangles to integrate internal and external experiences; they also explore their sense of guilt and anxiety and try reducing them using the triangle of conflict. The therapist here aims to help patients internalize psychological functions, such as regulating emotions and increasing energy, and build a sustainable self-object milieu (Seruya, 1997).
Consistent with the previous findings (Johansson, Bjorklund, Hornborg, & Anderson 2013; Leichsenring et al, 2014; Swartz et al., 2016) and Hypothesis 2, BEP was significantly effective in reducing depression. There are some explanations for this finding. First, the approach used in BEP is of empathy; therefore, the supportive behavior and active involvement of the therapist (Seruya, 1997) must have been effective in treating depression. In BEP, such empathic relationship is of importance as it leads to empathic self-object changes in the patients that initiate the internalization of aliveness, hope, and happiness, ultimately improving object relatedness. Patients benefit from this approach because their feelings of uniqueness and specialness are fostered. Further, in our research, most participants were 19–30 years old and were females; this is explained by the previous finding that age and gender predict better outcome of short-term psychodynamic therapy in minor depression (Frank et al., 2002). Studies have shown that the female gender is highly correlated with better treatment outcome (Frank et al., 2002). Third explanation is that in the approach used in BEP, the therapist has more active involvement and attempts to identify the intrapsychic conflicts that led to depression. Depression in ASAD patients involves self-oriented aggression; therefore, empathic introspection that is learned during the therapy helps them develop a compassionate view about themselves.
The present research also showed that APT was significantly effective in reducing anxiety, consistent with Hypothesis 3 and previous findings (Johansson, Hesser, Ljótsson, Frederick, & Andersson, 2016; Maljanen et al., 2016; Abbass, Hancock, Henderson, & Kisely, 2014). In APT, the therapist helps patients via three strategies, including defense restructuring (recognizing and relinquishing maladaptive defenses), affect restructuring (desensitization to fearful affects via exposure to conflicted feeling), and self/other restructuring (promotion of the sense of self and relationship with others). In addition, in this model, anxiety is reduced through systematic desensitization (McCullough et al., 2003). In many anxiety disorders, such as SAD, pathological behaviors are manifested as defensive behavioral patterns that block adaptive coping strategies. In chronic anxiety, the defensive behaviors are inappropriate. To gradually desensitize the patients to fearful affects, the therapist gently shifts between exposing the patients with affects and encouraging them not to defend or avoid this process so as to help them cope with anxieties.
Lastly, our study finding ruled out Hypothesis 4, which stated that APT is effective in reducing depression. Thus, this result is not consistent with previous findings that confirmed the effectiveness of APT in reducing depression (Johansson et al., 2016; Johansson et al., 2013; Dornelas, Ferrand, & Stepnowski, 2010). Our result can be explained by the fact that APT focuses on desensitizing patients to affect phobias. Because our patients had severe anxiety, most of the therapy focused on fears and affect phobias related to their fears. Most of our patients had unconscious fears about being rejected by attachment figures, sense of pity about themselves, and conflicts about anxiety expression; therefore, in our study, APT focused on reducing anxiety using desensitization and not on depression.
Our research has some limitations that should be taken into account while interpreting the results. First, this study was the first one to use two interventions, and patients with severe ASAD were recruited instead of those with moderate ASAD; therefore, it is necessary to conduct a similar study on patients with moderate ASAD and compare its findings with ours. Second, all our participants were females; this limits the extrapolation of our findings to male patients. Therefore, future studies involving both genders are warranted. In addition, due to the time limit, a 2-month follow-up was conducted in the present research; therefore, a 6-month follow-up is recommended to examine long-term stability of such patients. Despite these limitations, this research demonstrated useful results of BEP and APT in ASAD. Both BEP and APT were found to be effective in reducing anxiety in the sample population, and BEP, but not APT, was also effective in reducing depression. We used not only a questionnaire to assess ASAD but also interviews to select subjects with severe ASAD. Our results highlight the potential of these interventions in treating depression and anxiety in ASAD patients. Because dynamic psychotherapies are highly effective in treating anxiety disorders, especially SAD, such intervention protocols, similar to those used in our research, should be designed for clinical use. In addition, due to the high prevalence of ASAD and its adverse effects on the quality of life of ASAD patients, it is necessary to accurately diagnose and treat such patients to improve their lifestyles, coping strategies, self-esteem, and well-being. These needs can be met using dynamic psychotherapies.
Ethical Considerations
Compliance with ethical guidelines
The present research is a part of first authors phd thesis and have ethical code from Ardabil university of medical sciences.
Funding
This article was part of the first author’s PhD thesis in the Department of Psychology and was financially supported by the research grant from the office of vice chancellor of the University of Mohaghegh Ardabili.
Conflicts of interest
The authors declare that they have no conflict of interest.
Acknowledgments
The authors would like to thank all university students who participated in this research.
References
- Abbass, A. A., Hancock, J. T., Henderson, J., & Kisely, S. (2014). Short-term psychodynamic psychotherapies for common mental disorders. The Cochrane Database of Systematic Reviews, 18(4):CD004687. [DOI:10.1002/14651858.CD004687.pub3]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Washington, D.C.: American Psychiatric Association Publishing.
- Bögels, S. M., Knappe, S., & Clark, L. A. (2013). Adult separation anxiety disorder in DSM-V. Clinical Psychological Review, 33(5), 663–74. [DOI:10.1016/j.cpr.2013.03.006]
- Busch, F. N., & Milord, B. L. (2015). Psychodynamic treatment for separation anxiety disorder in a treatment nonresponder. Journal of the American Psychoanalytic Association, 63(5), 893-919. [DOI:10.1177/0003065115607491]
- Carmassia, C., Gesia C., Corsia M., Pergentinia I., Cremonea I. M, Conversanoa C., et al. (2015). Adult separation anxiety differentiates patients with complicated grief and/or major depression and is related to lifetime mood spectrum symptoms. Comprehensive Psychiatry, 58, 45-49. [DOI:10.1016/j.comppsych.2014.11.012]
- Copeland, W. E., Angold, A., & Shanahan, L. (2014). Longitudinal patterns of anxiety from childhood to adulthood: The Great Smoky Mountains Study. Journal of American Academic Child Adolescence Psychiatry, 53(1), 21-33. [DOI:10.1016/j.jaac.2013.09.017]
- Cyranowski, J. M., Shear, M. K., Rucci, P., Fagiolini, A., Frank, E., & Grochocinski, V. J. (2002). Adult separation anxiety: Psychometric properties of a new structured clinical interview. Journal of Psychiatric Research, 36(2), 77–86. [DOI:10.1016/S0022-3956(01)00051-6]
- Dirioz, M., Alkin, T., Yemez, B., Onur, E., & Eminağaoğlu, N. (2012). the validity and reliability of Turkish version of separation anxiety symptom inventory and adult separation anxiety question-naire. Turkish Journal of Psychiatry, 23(2), 108-116. [PMID]
- Dornelas, E., Ferrand, J., & Stepnowski, R. (2010). A pilot study of affect-focused psychotherapy for antepartum depression. Journal of Psychotherapy Integration, 20(4), 364–82. [DOI:10.1037/a0022035]
- Ferrero A., Piero, A., Fassina, S., Massola, T., Lanteri, A., & AbbateDaga, G. (2007). A 12-month comparison of brief psychodynamic psychotherapy and pharmacotherapy treatment in subjects with generalized anxiety disorders in a community setting. European Psychiatry, 22(8), 530-9. [DOI:10.1016/j.eurpsy.2007.07.004]
- Frank, E., Rucci, P., Katon, W., Barrett, J., Williams, J. W., Oxman, T., et al. (2002). Correlates of remission in primary care patient treated for minor depression. General Hospital Psychiatry, 24(1), 12-9. [DOI:10.1016/S0163-8343(01)00173-6]
- Heidari, S., Lewis, A. J., Allahyari, A., Azadfallah, P., & Bertino, M. D. (2013). A pilot study of brief psychodynamic psychotherapy for depression and anxiety in young Iranian adults: The effect of attachment style on outcomes. Psychoanalytic Psychology, 30(3), 381-93. [DOI:10.1037/a0033503]
- Hock, E., McBride, S., & Gnezda, M. T. (1989). Maternal Separation Anxiety: Mother-Infant Separation from the Maternal Perspective. Child Development, 60(4), 793–802. [DOI:10.2307/1131019]
- Johansson, R., Bjorklund, M., Hornborg, C., & Anderson, G. (2013). Affect-focused psychodynamic psychotherapy for depression and anxiety through the internet: A randomized controlled trial. Peer Journal, 1(2), 102. [DOI:10.7717/peerj.102]
- Johansson, R., Hesser, H., Ljótsson, B., Frederick, R. J., & Andersson, G. (2016). Transdiagnostic, affect-focused, psychodynamic, guided self-help for depression and anxiety through the internet: study protocol for a randomized controlled trial. BMJ Open, 2(6), e002167. [DOI:10.1136/bmjopen-2012-002167]
- Kessler, R. C., Chiu, W. T., Jin, R., Ruscio, A. M., Shear, K., & Walters, E. E. (2006). The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Archives of General Psychiatry, 63(4), 415–24. [DOI:10.1001/archpsyc.63.4.415]
- Khorshidvand, Z., RahimianBoogar, I., & Talepasand, S. (2015). Comparison of Temperament–character Dimensions of Personality among Patients with Separation Anxiety Disorderand Healthy Individuals. Iranian Journal of Psychiatry and Clinical Psychology, 21(3), 201-193.
- Knekt, P., Heinonen, E., Härkäpää, K., Järvikoski, A., Virtala, E., Rissanen, J., et al. (2015). Randomized trial on the effectiveness of long- and short-term psychotherapy on psychosocial functioning and quality of life during a5-year follow-up. Psychiatry Research, 229(1-2), 381-88. [DOI:10.1016/j.psychres.2015.05.113]
- Knekt, P., Lindfors, O., Laaksonen, M. A., Raitasalo, R., Haaramo, P., & Järvikoski, A. (2008). The Helsinki Psychotherapy Study Group Effectiveness of short-term and long-term psychotherapy on work ability and functional capacity — A randomized clinical trial on depressive and anxiety disorders. Journal of Affective Disorders, 107(1-3), 95–106. [DOI:10.1016/j.jad.2007.08.005]
- Leichsenring, F., & Salzer, S. (2014). A unified protocol for the transdiagnostic psychodynamic treatment of anxiety disorders: an evidence-based approach. Psychotherapy, 51(2), 224–45. [DOI:10.1037/a0033815]
- Leichsenring, F., Salzer, S., Beutel, M. E., Herpertz, S., Hiller, W., Hoyer, J., et al. (2014). Long-term outcome of psychodynamic therapy and cognitive-behavioral therapy in social anxiety disorder. American Journal of Psychiatry, 171(10), 1074-82. [DOI:10.1176/appi.ajp.2014.13111514]
- Lovibond, P. F., Lovibond, S. H. (1995). The Structure Of Negative Emotional States: Comparison Of The Depression Anxiety Stress Scales (DASS) With The Beck Depression And Anxiety Inventories. Behavior Research and Therapy, 33(3), 335-43. [DOI:10.1016/0005-7967(94)00075-U]
- Maljanen, T., Knekt, P., Lindfors, O., Virtala, E., Tillman, P., Harkanen, T., et al. (2016). The cost-effectiveness of short-term and long-term psychotherapy in the treatment of depressive and anxiety disorders during 5-year follow up. Journal of Afective Disorders, 15(190), 254-63. [DOI:10.1016/j.jad.2015.09.065]
- Manicavasagar, V., Silove, D., Curtis, J., & Wagner, R. (2000). Continuities of separation anxiety from early life into adulthood. Journal of Anxiety Disorders, 14(1), 1–18. [DOI:10.1016/S0887-6185(99)00029-8]
- Manicavasagar, V., Silove, D., Wagner, R., & Drobny, J. (2003). A Self-Report Questionnaire for Measuring Separation Anxiety in Adulthood. Comprehensive Psychiatry, 44(2), 146-53. [DOI:10.1053/comp.2003.50024]
- Mayseless, O., & Scher, A. (2000). Mother’s attachment concerns regarding spouse and infant’s temperament as modulators of maternal separation anxiety. Journal of Child Psychology and Psychiatry and Allied Disciplines, 41(7), 917-25. [DOI:10.1111/1469-7610.00679]
- McCullough, L., Kuhn, N., Andrews, S., Kaplan, A., Wolf, J., & Hurley, C. L. (2003). Treating affect phobia: A manual for short-term dynamic psychotherapy. New York: Guilford Press.
- Milord, B. (2015). An epidemiological contribution to clinical understanding of anxiety. American Journal of Psychiatry, 72(7), 601-2. [DOI:10.1176/appi.ajp.2015.15030312]
- Miniati, M., Calugi, S., & Rucci, P. (2012). Predictors of response among patients with panic disorder treated with medications in a naturalistic follow-up: the role of adult separation anxiety. Journal of Affective Disorders, 136(3), 675–79. [DOI:10.1016/j.jad.2011.10.008]
- Rochester, J., & Baldwin, D. (2015). Adult separation anxiety disorder: accepted but little understood. Human Psychopharmacology, 30(1), 1-3. [DOI:10.1002/hup.2452]
- Sahebi, A., Asghari, M. A., & Salari, R. S. (2005). [Validation of Depression, Anxiety and Stress test (DASS-21) for Iranian population (Persian)]. Evolutionary Psychology, 1(4), 299-312.
- Sass, H. (2003). [Diagnostic and Statistical Manual of mental disorders: Text Revision – DSM-IV-TR (French)]. Göttingen: Hogrefe.
- Seruya, B. (1997). Brief empathic psychotherapy. Northvale, New Jersey: Janson Aronson.
- Cyranowski, J., Shear, M. K., Rucci, P., Fagiolini, A., Frank, E., Grochocinsky, V. J., et al. (2002). Adult separation anxiety: Psychometric properties of a new structured clinical interview. Journal of Psychiatric Research, 36(2), 77–86. [DOI:10.1016/S0022-3956(01)00051-6]
- Shear, K., Jin, R., Ruscio, A. M., Walters, E. E., & Kessler, R. C. (2006). Prevalence and correlates of estimated DSM-IV child and adult separation anxiety disorder in the National Comorbidity Survey Replication. American Journal of Psychiatry, 163(6), 1074–83. [DOI:10.1176/ajp.2006.163.6.1074]
- Silove D, Lonso J., Bromet, E., Grunber, M., & Sampson N., Scott K., (2015). Pediatric-onset and adult onset separation anxiety disorder across countries in the world mental health survey. American Journal of Psychiatry, 172(7), 647-656. [DOI:10.1176/appi.ajp.2015.14091185]
- Silove, D. M., Marnane, C. L., Wagner, R., Manicavasagar, V. L., & Rees, S. (2010). The prevalence and correlates of adult separation anxiety disorder in an anxiety clinic. BMC Psychiatry, 10(1), 21. [DOI:10.1186/1471-244X-10-21]
- Silove, D., Marnane, C., Wagner, R., & Manicavasagar, V. (2011). Brief report associations of personality disorder with early separation anxiety in patients with adult separation anxiety disorder. Journal of Personality Disorders, 25(1), 128–33. [DOI:10.1521/pedi.2011.25.1.128]
- Silove, D., & Rees, S. (2014). Separation anxiety disorder across the lifespan: DSM-5 lifts age restriction on diagnosis. Asian Journal of Psychiatry, 11, 98-101. [DOI:10.1016/j.ajp.2014.06.021]
- Startup, M., Jackson, M. C., & Bendix, S. (2002). The concurrent validity of the Global Assessment of Functioning (GAF). British Journal of Clinical Psychology, 41(4), 417-22. [DOI:10.1348/014466502760387533]
- Swartz, H. A., Cyranowsky, J. M., Cheng, Y., Zuckoff, A., Brent, D. A., Markowitz, J. C., et al. (2016). Brief Psychotherapy for Maternal Depression: Impact on Mothers and Children. Journal of the American Academy of Child & Adolescent Psychiatry, 55(6), 495-503. [DOI:10.1016/j.jaac.2016.04.003]
- Tran, T. D., Tran, T., & Fisher, J. (2013). Validation of the Depression Anxiety Stress Scales (DASS) 21 as a screening instrument for depression and anxiety in a rural community-based cohort of northern Vietnamese women. BMC Psychiatry, 13, 24. [DOI:10.1186/1471-244X-13-24]
- Trauer, N. G. F. T., Dodd, S., Callaly, T., Campbell, S., & Berk, M. (2007). The validity of the 21-item version of the Depression Anxiety Stress Scales as a routine clinical outcome measure. Acta Neuropsychiatric, 19(5), 304-10. [DOI:10.1111/j.1601-5215.2007.00217.x]
Type of Study: Original Research Article |
Subject:
Analytical approach
Received: 2017/11/17 | Accepted: 2018/05/5 | Published: 2018/07/1
Received: 2017/11/17 | Accepted: 2018/05/5 | Published: 2018/07/1
References
1. Abbass, A. A., Hancock, J. T., Henderson, J., & Kisely, S. (2014). Short-term psychodynamic psychotherapies for common mental disorders. The Cochrane Database of Systematic Reviews, 18(4):CD004687. [DOI:10.1002/14651858.CD004687.pub3] [DOI:10.1002/14651858.CD004687.pub3]
2. American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Washington, D.C.: American Psychiatric Association Publishing. [DOI:10.1176/appi.books.9780890425596]
3. Bögels, S. M., Knappe, S., & Clark, L. A. (2013). Adult separation anxiety disorder in DSM-V. Clinical Psychological Review, 33(5), 663–74. [DOI:10.1016/j.cpr.2013.03.006] [DOI:10.1016/j.cpr.2013.03.006]
4. Busch, F. N., & Milord, B. L. (2015). Psychodynamic treatment for separation anxiety disorder in a treatment nonresponder. Journal of the American Psychoanalytic Association, 63(5), 893-919. [DOI:10.1177/0003065115607491] [DOI:10.1177/0003065115607491]
5. Carmassia, C., Gesia C., Corsia M., Pergentinia I., Cremonea I. M, Conversanoa C., et al. (2015). Adult separation anxiety differentiates patients with complicated grief and/or major depression and is related to lifetime mood spectrum symptoms. Comprehensive Psychiatry, 58, 45-49. [DOI:10.1016/j.comppsych.2014.11.012] [DOI:10.1016/j.comppsych.2014.11.012]
6. Copeland, W. E., Angold, A., & Shanahan, L. (2014). Longitudinal patterns of anxiety from childhood to adulthood: The Great Smoky Mountains Study. Journal of American Academic Child Adolescence Psychiatry, 53(1), 21-33. [DOI:10.1016/j.jaac.2013.09.017] [DOI:10.1016/j.jaac.2013.09.017]
7. Cyranowski, J. M., Shear, M. K., Rucci, P., Fagiolini, A., Frank, E., & Grochocinski, V. J. (2002). Adult separation anxiety: Psychometric properties of a new structured clinical interview. Journal of Psychiatric Research, 36(2), 77–86. [DOI:10.1016/S0022-3956(01)00051-6] [DOI:10.1016/S0022-3956(01)00051-6]
8. Dirioz, M., Alkin, T., Yemez, B., Onur, E., & Eminağaoğlu, N. (2012). the validity and reliability of Turkish version of separation anxiety symptom inventory and adult separation anxiety question-naire. Turkish Journal of Psychiatry, 23(2), 108-116. [PMID] [PMID]
9. Dornelas, E., Ferrand, J., & Stepnowski, R. (2010). A pilot study of affect-focused psychotherapy for antepartum depression. Journal of Psychotherapy Integration, 20(4), 364–82. [DOI:10.1037/a0022035] [DOI:10.1037/a0022035]
10. Ferrero A., Piero, A., Fassina, S., Massola, T., Lanteri, A., & AbbateDaga, G. (2007). A 12-month comparison of brief psychodynamic psychotherapy and pharmacotherapy treatment in subjects with generalized anxiety disorders in a community setting. European Psychiatry, 22(8), 530-9. [DOI:10.1016/j.eurpsy.2007.07.004] [DOI:10.1016/j.eurpsy.2007.07.004]
11. Frank, E., Rucci, P., Katon, W., Barrett, J., Williams, J. W., Oxman, T., et al. (2002). Correlates of remission in primary care patient treated for minor depression. General Hospital Psychiatry, 24(1), 12-9. [DOI:10.1016/S0163-8343(01)00173-6] [DOI:10.1016/S0163-8343(01)00173-6]
12. Heidari, S., Lewis, A. J., Allahyari, A., Azadfallah, P., & Bertino, M. D. (2013). A pilot study of brief psychodynamic psychotherapy for depression and anxiety in young Iranian adults: The effect of attachment style on outcomes. Psychoanalytic Psychology, 30(3), 381-93. [DOI:10.1037/a0033503] [DOI:10.1037/a0033503]
13. Hock, E., McBride, S., & Gnezda, M. T. (1989). Maternal Separation Anxiety: Mother-Infant Separation from the Maternal Perspective. Child Development, 60(4), 793–802. [DOI:10.2307/1131019] [DOI:10.2307/1131019]
14. Johansson, R., Bjorklund, M., Hornborg, C., & Anderson, G. (2013). Affect-focused psychodynamic psychotherapy for depression and anxiety through the internet: A randomized controlled trial. Peer Journal, 1(2), 102. [DOI:10.7717/peerj.102] [DOI:10.7717/peerj.102]
15. Johansson, R., Hesser, H., Ljótsson, B., Frederick, R. J., & Andersson, G. (2016). Transdiagnostic, affect-focused, psychodynamic, guided self-help for depression and anxiety through the internet: study protocol for a randomized controlled trial. BMJ Open, 2(6), e002167. [DOI:10.1136/bmjopen-2012-002167] [DOI:10.1136/bmjopen-2012-002167]
16. Kessler, R. C., Chiu, W. T., Jin, R., Ruscio, A. M., Shear, K., & Walters, E. E. (2006). The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Archives of General Psychiatry, 63(4), 415–24. [DOI:10.1001/archpsyc.63.4.415] [DOI:10.1001/archpsyc.63.4.415]
17. Khorshidvand, Z., RahimianBoogar, I., & Talepasand, S. (2015). Comparison of Temperament–character Dimensions of Personality among Patients with Separation Anxiety Disorderand Healthy Individuals. Iranian Journal of Psychiatry and Clinical Psychology, 21(3), 201-193.
18. Knekt, P., Heinonen, E., Härkäpää, K., Järvikoski, A., Virtala, E., Rissanen, J., et al. (2015). Randomized trial on the effectiveness of long- and short-term psychotherapy on psychosocial functioning and quality of life during a5-year follow-up. Psychiatry Research, 229(1-2), 381-88. [DOI:10.1016/j.psychres.2015.05.113] [DOI:10.1016/j.psychres.2015.05.113]
19. Knekt, P., Lindfors, O., Laaksonen, M. A., Raitasalo, R., Haaramo, P., & Järvikoski, A. (2008). The Helsinki Psychotherapy Study Group Effectiveness of short-term and long-term psychotherapy on work ability and functional capacity — A randomized clinical trial on depressive and anxiety disorders. Journal of Affective Disorders, 107(1-3), 95–106. [DOI:10.1016/j.jad.2007.08.005] [DOI:10.1016/j.jad.2007.08.005]
20. Leichsenring, F., & Salzer, S. (2014). A unified protocol for the transdiagnostic psychodynamic treatment of anxiety disorders: an evidence-based approach. Psychotherapy, 51(2), 224–45. [DOI:10.1037/a0033815] [DOI:10.1037/a0033815]
21. Leichsenring, F., Salzer, S., Beutel, M. E., Herpertz, S., Hiller, W., Hoyer, J., et al. (2014). Long-term outcome of psychodynamic therapy and cognitive-behavioral therapy in social anxiety disorder. American Journal of Psychiatry, 171(10), 1074-82. [DOI:10.1176/appi.ajp.2014.13111514] [DOI:10.1176/appi.ajp.2014.13111514]
22. Lovibond, P. F., Lovibond, S. H. (1995). The Structure Of Negative Emotional States: Comparison Of The Depression Anxiety Stress Scales (DASS) With The Beck Depression And Anxiety Inventories. Behavior Research and Therapy, 33(3), 335-43. [DOI:10.1016/0005-7967(94)00075-U] [DOI:10.1016/0005-7967(94)00075-U]
23. Maljanen, T., Knekt, P., Lindfors, O., Virtala, E., Tillman, P., Harkanen, T., et al. (2016). The cost-effectiveness of short-term and long-term psychotherapy in the treatment of depressive and anxiety disorders during 5-year follow up. Journal of Afective Disorders, 15(190), 254-63. [DOI:10.1016/j.jad.2015.09.065] [DOI:10.1016/j.jad.2015.09.065]
24. Manicavasagar, V., Silove, D., Curtis, J., & Wagner, R. (2000). Continuities of separation anxiety from early life into adulthood. Journal of Anxiety Disorders, 14(1), 1–18. [DOI:10.1016/S0887-6185(99)00029-8] [DOI:10.1016/S0887-6185(99)00029-8]
25. Manicavasagar, V., Silove, D., Wagner, R., & Drobny, J. (2003). A Self-Report Questionnaire for Measuring Separation Anxiety in Adulthood. Comprehensive Psychiatry, 44(2), 146-53. [DOI:10.1053/comp.2003.50024] [DOI:10.1053/comp.2003.50024]
26. Mayseless, O., & Scher, A. (2000). Mother's attachment concerns regarding spouse and infant's temperament as modulators of maternal separation anxiety. Journal of Child Psychology and Psychiatry and Allied Disciplines, 41(7), 917-25. [DOI:10.1111/1469-7610.00679] [DOI:10.1111/1469-7610.00679]
27. McCullough, L., Kuhn, N., Andrews, S., Kaplan, A., Wolf, J., & Hurley, C. L. (2003). Treating affect phobia: A manual for short-term dynamic psychotherapy. New York: Guilford Press.
28. Milord, B. (2015). An epidemiological contribution to clinical understanding of anxiety. American Journal of Psychiatry, 72(7), 601-2. [DOI:10.1176/appi.ajp.2015.15030312] [DOI:10.1176/appi.ajp.2015.15030312]
29. Miniati, M., Calugi, S., & Rucci, P. (2012). Predictors of response among patients with panic disorder treated with medications in a naturalistic follow-up: the role of adult separation anxiety. Journal of Affective Disorders, 136(3), 675–79. [DOI:10.1016/j.jad.2011.10.008] [DOI:10.1016/j.jad.2011.10.008]
30. Rochester, J., & Baldwin, D. (2015). Adult separation anxiety disorder: accepted but little understood. Human Psychopharmacology, 30(1), 1-3. [DOI:10.1002/hup.2452] [DOI:10.1002/hup.2452]
31. Sahebi, A., Asghari, M. A., & Salari, R. S. (2005). [Validation of Depression, Anxiety and Stress test (DASS-21) for Iranian population (Persian)]. Evolutionary Psychology, 1(4), 299-312.
32. Sass, H. (2003). [Diagnostic and Statistical Manual of mental disorders: Text Revision – DSM-IV-TR (French)]. Göttingen: Hogrefe.
33. Seruya, B. (1997). Brief empathic psychotherapy. Northvale, New Jersey: Janson Aronson.
34. Cyranowski, J., Shear, M. K., Rucci, P., Fagiolini, A., Frank, E., Grochocinsky, V. J., et al. (2002). Adult separation anxiety: Psychometric properties of a new structured clinical interview. Journal of Psychiatric Research, 36(2), 77–86. [DOI:10.1016/S0022-3956(01)00051-6] [DOI:10.1016/S0022-3956(01)00051-6]
35. Shear, K., Jin, R., Ruscio, A. M., Walters, E. E., & Kessler, R. C. (2006). Prevalence and correlates of estimated DSM-IV child and adult separation anxiety disorder in the National Comorbidity Survey Replication. American Journal of Psychiatry, 163(6), 1074–83. [DOI:10.1176/ajp.2006.163.6.1074] [DOI:10.1176/ajp.2006.163.6.1074]
36. Silove D, Lonso J., Bromet, E., Grunber, M., & Sampson N., Scott K., (2015). Pediatric-onset and adult onset separation anxiety disorder across countries in the world mental health survey. American Journal of Psychiatry, 172(7), 647-656. [DOI:10.1176/appi.ajp.2015.14091185] [DOI:10.1176/appi.ajp.2015.14091185]
37. Silove, D. M., Marnane, C. L., Wagner, R., Manicavasagar, V. L., & Rees, S. (2010). The prevalence and correlates of adult separation anxiety disorder in an anxiety clinic. BMC Psychiatry, 10(1), 21. [DOI:10.1186/1471-244X-10-21] [DOI:10.1186/1471-244X-10-21]
38. Silove, D., Marnane, C., Wagner, R., & Manicavasagar, V. (2011). Brief report associations of personality disorder with early separation anxiety in patients with adult separation anxiety disorder. Journal of Personality Disorders, 25(1), 128–33. [DOI:10.1521/pedi.2011.25.1.128] [DOI:10.1521/pedi.2011.25.1.128]
39. Silove, D., & Rees, S. (2014). Separation anxiety disorder across the lifespan: DSM-5 lifts age restriction on diagnosis. Asian Journal of Psychiatry, 11, 98-101. [DOI:10.1016/j.ajp.2014.06.021] [DOI:10.1016/j.ajp.2014.06.021]
40. Startup, M., Jackson, M. C., & Bendix, S. (2002). The concurrent validity of the Global Assessment of Functioning (GAF). British Journal of Clinical Psychology, 41(4), 417-22. [DOI:10.1348/014466502760387533] [DOI:10.1348/014466502760387533]
41. Swartz, H. A., Cyranowsky, J. M., Cheng, Y., Zuckoff, A., Brent, D. A., Markowitz, J. C., et al. (2016). Brief Psychotherapy for Maternal Depression: Impact on Mothers and Children. Journal of the American Academy of Child & Adolescent Psychiatry, 55(6), 495-503. [DOI:10.1016/j.jaac.2016.04.003] [DOI:10.1016/j.jaac.2016.04.003]
42. Tran, T. D., Tran, T., & Fisher, J. (2013). Validation of the Depression Anxiety Stress Scales (DASS) 21 as a screening instrument for depression and anxiety in a rural community-based cohort of northern Vietnamese women. BMC Psychiatry, 13, 24. [DOI:10.1186/1471-244X-13-24] [DOI:10.1186/1471-244X-13-24]
43. Trauer, N. G. F. T., Dodd, S., Callaly, T., Campbell, S., & Berk, M. (2007). The validity of the 21-item version of the Depression Anxiety Stress Scales as a routine clinical outcome measure. Acta Neuropsychiatric, 19(5), 304-10. [DOI:10.1111/j.1601-5215.2007.00217.x] [DOI:10.1111/j.1601-5215.2007.00217.x]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |