Volume 6, Issue 1 (Winter 2018- 2018)
PCP 2018, 6(1): 57-62 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Aflakseir A, Manafi F. Posttraumatic Growth and its Relationship With Cognitive Emotion Regulation Strategies in Patients With Multiple Sclerosis in Shiraz, Iran. PCP 2018; 6 (1) :57-62
URL: http://jpcp.uswr.ac.ir/article-1-450-en.html
URL: http://jpcp.uswr.ac.ir/article-1-450-en.html
1- Department of Psychology, School of Education & Psychology, University of Shiraz, Shiraz, Iran. , aaflakseir@shirazu.ac.ir
2- Department of Psychology, Faculty of Educational Sciences and Psychology, Alzahra University, Tehran, Iran.
2- Department of Psychology, Faculty of Educational Sciences and Psychology, Alzahra University, Tehran, Iran.
Full-Text [PDF 494 kb]
(3580 Downloads)
| Abstract (HTML) (8031 Views)
Full-Text: (2185 Views)
1. Introduction
Multiple sclerosis (MS) is a chronic disease that affects people in early adulthood and is more prevalent among women than men (Lode, Bru, Klevan, Myhr, & Larsen, 2010). Suffering from MS is annoying and can affect physical abilities as well as psychological well-being (Fazzito Jordy, & Tilbery, 2009). Being diagnosed with a life-threatening illness can be a traumatic experience and provoke anxiety tremendously (Hoang, Laursen, Stenager, & Stenager, 2015). On the other hand, posttraumatic growth is the experience of personal growth after a traumatic or adverse life event (Stanton, Bower, & Low, 2014). This type of growth is explicitly experienced in the case of a severe life crisis, loss and traumatic event, but not with minor daily stressors (Tedeschi & Calloun, 2004).
Since Tedeschi & Calloun, 2004 introduced the theory of posttraumatic growth, numerous studies have investigated posttraumatic growth within stressful condition such as the diagnosis of cancer, heart disease, AIDS, MS, spinal cord injury, and rheumatic disease. These studies have reported mixed results. Most studies have reported a positive change after the stressful situation, while some others studies have reported no growth (Tedeschi & Calloun, 2004). For example, a positive change was reported by 60% of patients suffering from myocardial infarction in response to their illness (Losiak & Nikiel, 2014). Furthermore, in a longitudinal study, posttraumatic growth increased over two years following breast cancer diagnosis (Danhauer et al., 2013).
Emotion regulation is the process of modifying emotions to provide an appropriate response to situations (Rabinowitz & Arnett, 2013; Aldao, & Nolen-Hoeksema, 2010). Cognitive and emotion regulation strategies are postulated to be mechanisms that are open and change (Bargh & Williams, 2007). Cognitive processes are involved in the experience and expression of emotion (Garnefski, Kraaij, & Schroevers, 2008). Furthermore, it is reported that cognitive coping methods are mechanisms under constant potential influence and modification (Gorgen, Hiller & Witthoft, 2014). Different theoretical models of cognitive emotion regulation have offered specific strategies as either adaptive (e.g. reappraisal) or maladaptive (e.g. avoidance) (Alado, Jazaieri, Goldin, & Gross, 2014).
Studies associated with adaptive emotion regulation with psychological well-being, improved relationships and academic and work performance. For example; a positive association has been found between posttraumatic growth and effective cognitive strategies (Schraub, Turgut, Clavairoly, & Sonntag, 2013). Studies have also shown that difficulties with emotion regulation are related to a mental disorder such as anxiety, depression, and personality disorders (Mennin & Farach, 2007). Cognitive emotion regulation has been considered as a significant factor to influence growth following stressful conditions such as chronic illnesses (Philips, Henry, Nouzova, Cooper, Radlak, & Summers, 2014). Studies investigating types of cognitive emotion regulation strategies that are associated with posttraumatic growth have yielded mixed results.
Understanding the association between cognitive emotion coping and posttraumatic growth is significant because it can help in developing more effective interventions (Garnefski, et al., 2008). Hence, understanding the type of cognitive-emotion regulation strategies relevant to posttraumatic growth is of high importance. There are only a few studies which examined posttraumatic growth among patients with chronic illness in Iran (Seyed-Mahmoodi, Rahimit & Mohammadi, 2013). Posttraumatic growth and its association with cognitive emotion regulation strategies among Iranian patients with MS have remained poorly explored. Therefore, the present study aims to examine posttraumatic growth and its relationship with cognitive emotion regulation strategies in a group of Iranian patients with MS in Shiraz. It was hypothesized that cognitive emotion regulation strategies could predict posttraumatic growth in patients with MS.
2. Methods
A correlation design was adopted in this study, and 92 patients who were diagnosed with MS participated in the study in 2014. For sampling purposes, 10-15 cases of data for each predictor variable in the model were sufficient for multiple regression analysis (Field, 2007). This study involved nine predictor variables; therefore, a sample comprising of 90 participants was required. The total sample mean age was 35 years ranges from 20 to 50 years. Convenience sampling method was used to recruit participants from the MS society in Shiraz. The questionnaires were completed at the participants’ convenience from March to July 2014. The inclusion criteria were patients aged 20-60 years, fifth-grade education, being in non-relapsing phase, no previous psychiatric or physical disorder.
Posttraumatic growth was assessed by the Posttraumatic Growth Inventory (PTGI) (Tedeschi & Calhoun, 1996). The PTGI evaluates perceived personal growth as a result of the trauma. The instrument contains 21 items that require a respondent to rate each on 0 (I did not experience) to 5 (I experienced this to a very significant degree) scale. The total scores range from 0 to 105. Analyses yielded five dimensions that measure five factors. Researchers have reported an excellent internal consistency of α=0.90, with the emerging factors also showing substantial internal consistency (Taku, Calhoun, Tedeschi, Gil-Rivas, Kilmer, & Cann, 2007). Studies conducted in Iran have used the MHLC and reported excellent reliability and validity, with alpha coefficients 0.92 for the scale, and test-retest reliability coefficients of 0.94 and also 0.92 for concurrent validity (Seyed-Mahmoodi, Rahimit & Mohammadi, 2013).
Cognitive emotion regulation was assessed by the Cognitive Emotion Regulation Questionnaire (CERQ). The CERQ is a 36-item questionnaire, consisting of nine dimensions (Garnefski, Kraaij & Spinhoven, 2002). Each scale consists of four items, and the answers were rated on a five-point scale ranging from 1 (almost never) to 5 (almost always). Psychometrics studies have yielded alpha coefficients for the total scale ranging from 0.68 to 0.80 (Garnefski, Kraaij & Spinhoven, 2002). This scale has been used in several studies in Iran and a Cronbach’s alpha reliability of 0.92 was reported (Dadkhah & Shirinbayan, 2012).
Using SPSS version 20, descriptive statistics was performed, and the mean, standard deviation, Pearson’s correlation coefficient and multiple regression analysis were computed, while P<0.05 value was considered as the level of significance in this study. Informed consent was obtained from the interested participants. This study was approved by the Ethics Committee of the School of Psychology at Shiraz University.
3. Results
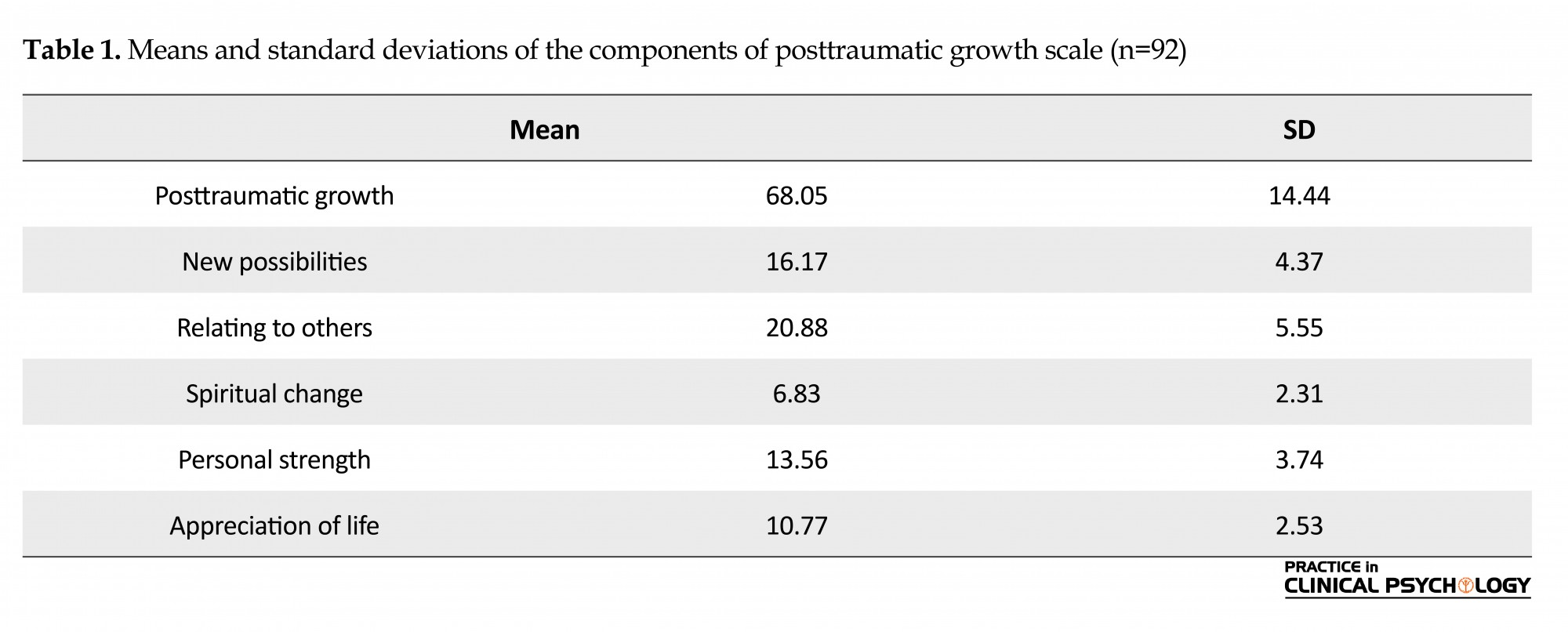
Sixty-seven (79%) of individuals with MS were females, and 23 (21%) were males. The average duration of illness was 6.5 years. Furthermore, 67.3% of the patients were married. The majority of the patients with MS had high school education, and 20 patients had a university education. Regarding the types of MS, 78% of the patients had the relapsing-remitting form, 15% had secondary-progressive MS, and 7% had the primary progressive form of MS. The majority of the sample perceived positive psychological growth associated with their experience of trauma (Mean=68.05; Standard deviation=14.44). The mean score of this sample on PTGI can be classified as above average score, falling into the range from 58 to 70. High scores are rated from 80 and above on the PTGI. Ninety percent of the sample reported a low posttraumatic growth score (40 and below), 56% reported moderate scores (41 to 79), and 25% reported high scores (80 to 101). Of the posttraumatic growth dimensions, the highest score belonged to the appreciation of life (mean=10.77, standard deviation=2.53) followed by spiritual change. Table 1 shows the means and standard deviations for a sample on the dependent variables and the posttraumatic variable.
Multiple sclerosis (MS) is a chronic disease that affects people in early adulthood and is more prevalent among women than men (Lode, Bru, Klevan, Myhr, & Larsen, 2010). Suffering from MS is annoying and can affect physical abilities as well as psychological well-being (Fazzito Jordy, & Tilbery, 2009). Being diagnosed with a life-threatening illness can be a traumatic experience and provoke anxiety tremendously (Hoang, Laursen, Stenager, & Stenager, 2015). On the other hand, posttraumatic growth is the experience of personal growth after a traumatic or adverse life event (Stanton, Bower, & Low, 2014). This type of growth is explicitly experienced in the case of a severe life crisis, loss and traumatic event, but not with minor daily stressors (Tedeschi & Calloun, 2004).
Since Tedeschi & Calloun, 2004 introduced the theory of posttraumatic growth, numerous studies have investigated posttraumatic growth within stressful condition such as the diagnosis of cancer, heart disease, AIDS, MS, spinal cord injury, and rheumatic disease. These studies have reported mixed results. Most studies have reported a positive change after the stressful situation, while some others studies have reported no growth (Tedeschi & Calloun, 2004). For example, a positive change was reported by 60% of patients suffering from myocardial infarction in response to their illness (Losiak & Nikiel, 2014). Furthermore, in a longitudinal study, posttraumatic growth increased over two years following breast cancer diagnosis (Danhauer et al., 2013).
Emotion regulation is the process of modifying emotions to provide an appropriate response to situations (Rabinowitz & Arnett, 2013; Aldao, & Nolen-Hoeksema, 2010). Cognitive and emotion regulation strategies are postulated to be mechanisms that are open and change (Bargh & Williams, 2007). Cognitive processes are involved in the experience and expression of emotion (Garnefski, Kraaij, & Schroevers, 2008). Furthermore, it is reported that cognitive coping methods are mechanisms under constant potential influence and modification (Gorgen, Hiller & Witthoft, 2014). Different theoretical models of cognitive emotion regulation have offered specific strategies as either adaptive (e.g. reappraisal) or maladaptive (e.g. avoidance) (Alado, Jazaieri, Goldin, & Gross, 2014).
Studies associated with adaptive emotion regulation with psychological well-being, improved relationships and academic and work performance. For example; a positive association has been found between posttraumatic growth and effective cognitive strategies (Schraub, Turgut, Clavairoly, & Sonntag, 2013). Studies have also shown that difficulties with emotion regulation are related to a mental disorder such as anxiety, depression, and personality disorders (Mennin & Farach, 2007). Cognitive emotion regulation has been considered as a significant factor to influence growth following stressful conditions such as chronic illnesses (Philips, Henry, Nouzova, Cooper, Radlak, & Summers, 2014). Studies investigating types of cognitive emotion regulation strategies that are associated with posttraumatic growth have yielded mixed results.
Understanding the association between cognitive emotion coping and posttraumatic growth is significant because it can help in developing more effective interventions (Garnefski, et al., 2008). Hence, understanding the type of cognitive-emotion regulation strategies relevant to posttraumatic growth is of high importance. There are only a few studies which examined posttraumatic growth among patients with chronic illness in Iran (Seyed-Mahmoodi, Rahimit & Mohammadi, 2013). Posttraumatic growth and its association with cognitive emotion regulation strategies among Iranian patients with MS have remained poorly explored. Therefore, the present study aims to examine posttraumatic growth and its relationship with cognitive emotion regulation strategies in a group of Iranian patients with MS in Shiraz. It was hypothesized that cognitive emotion regulation strategies could predict posttraumatic growth in patients with MS.
2. Methods
A correlation design was adopted in this study, and 92 patients who were diagnosed with MS participated in the study in 2014. For sampling purposes, 10-15 cases of data for each predictor variable in the model were sufficient for multiple regression analysis (Field, 2007). This study involved nine predictor variables; therefore, a sample comprising of 90 participants was required. The total sample mean age was 35 years ranges from 20 to 50 years. Convenience sampling method was used to recruit participants from the MS society in Shiraz. The questionnaires were completed at the participants’ convenience from March to July 2014. The inclusion criteria were patients aged 20-60 years, fifth-grade education, being in non-relapsing phase, no previous psychiatric or physical disorder.
Posttraumatic growth was assessed by the Posttraumatic Growth Inventory (PTGI) (Tedeschi & Calhoun, 1996). The PTGI evaluates perceived personal growth as a result of the trauma. The instrument contains 21 items that require a respondent to rate each on 0 (I did not experience) to 5 (I experienced this to a very significant degree) scale. The total scores range from 0 to 105. Analyses yielded five dimensions that measure five factors. Researchers have reported an excellent internal consistency of α=0.90, with the emerging factors also showing substantial internal consistency (Taku, Calhoun, Tedeschi, Gil-Rivas, Kilmer, & Cann, 2007). Studies conducted in Iran have used the MHLC and reported excellent reliability and validity, with alpha coefficients 0.92 for the scale, and test-retest reliability coefficients of 0.94 and also 0.92 for concurrent validity (Seyed-Mahmoodi, Rahimit & Mohammadi, 2013).
Cognitive emotion regulation was assessed by the Cognitive Emotion Regulation Questionnaire (CERQ). The CERQ is a 36-item questionnaire, consisting of nine dimensions (Garnefski, Kraaij & Spinhoven, 2002). Each scale consists of four items, and the answers were rated on a five-point scale ranging from 1 (almost never) to 5 (almost always). Psychometrics studies have yielded alpha coefficients for the total scale ranging from 0.68 to 0.80 (Garnefski, Kraaij & Spinhoven, 2002). This scale has been used in several studies in Iran and a Cronbach’s alpha reliability of 0.92 was reported (Dadkhah & Shirinbayan, 2012).
Using SPSS version 20, descriptive statistics was performed, and the mean, standard deviation, Pearson’s correlation coefficient and multiple regression analysis were computed, while P<0.05 value was considered as the level of significance in this study. Informed consent was obtained from the interested participants. This study was approved by the Ethics Committee of the School of Psychology at Shiraz University.
3. Results
Sixty-seven (79%) of individuals with MS were females, and 23 (21%) were males. The average duration of illness was 6.5 years. Furthermore, 67.3% of the patients were married. The majority of the patients with MS had high school education, and 20 patients had a university education. Regarding the types of MS, 78% of the patients had the relapsing-remitting form, 15% had secondary-progressive MS, and 7% had the primary progressive form of MS. The majority of the sample perceived positive psychological growth associated with their experience of trauma (Mean=68.05; Standard deviation=14.44). The mean score of this sample on PTGI can be classified as above average score, falling into the range from 58 to 70. High scores are rated from 80 and above on the PTGI. Ninety percent of the sample reported a low posttraumatic growth score (40 and below), 56% reported moderate scores (41 to 79), and 25% reported high scores (80 to 101). Of the posttraumatic growth dimensions, the highest score belonged to the appreciation of life (mean=10.77, standard deviation=2.53) followed by spiritual change. Table 1 shows the means and standard deviations for a sample on the dependent variables and the posttraumatic variable.
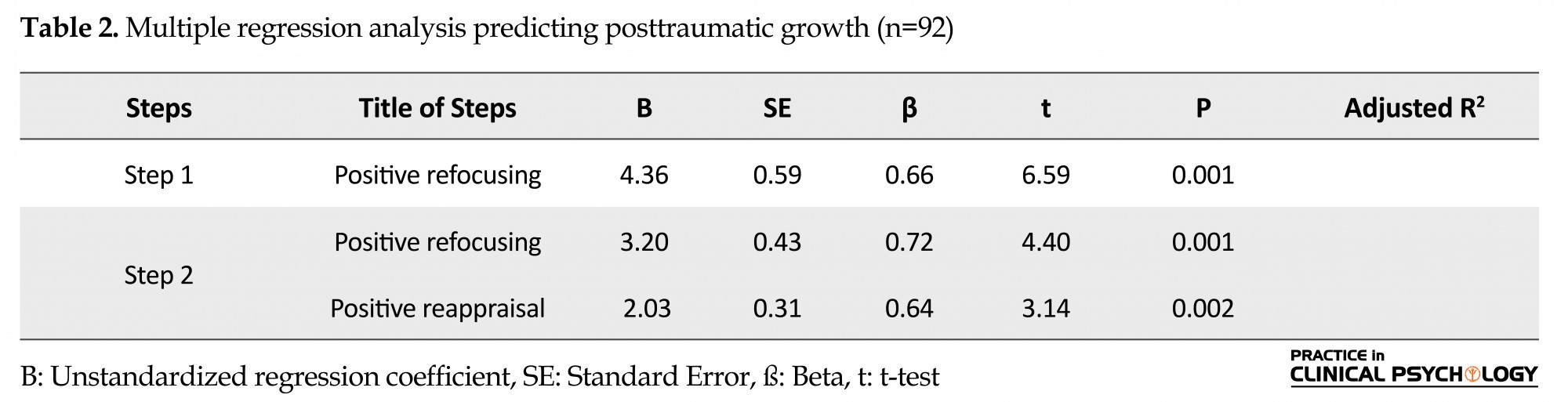
Findings also indicated that greater posttraumatic growth was related to reappraisal, positive refocusing, planning, and acceptance. The regression analysis emerged a significant model (F=3.65, P<0.01). The model explains 26% of the criterion variable (R2=0.26). With regard to cognitive emotion regulation variables, only reappraisal (β=0.64, P<0.002) and positive refocusing (β=0.72, P<0.001) significantly predicted posttraumatic growth. Posttraumatic growth was not predicted by the other cognitive emotion regulation strategies in individuals with MS. Results of multiple regression analysis are presented in Table 2.
4. Discussion
The findings showed that almost all patients with MS experienced posttraumatic growth at least to some degree. The level of posttraumatic growth observed in this study was higher than that previously reported in other MS (Ackroyd, Fortune, Price, Howell, Sharrack, & Issac, 2011), cardiac (Leung, Gravely-Witte, Macpherson, Irvine, Stewart, & Grace, 2010), and breast cancer (Holland Breitbart, Butow, Jacobsen, Loscalzo, & McCorkle, 2015) patients. The discrepancy on posttraumatic growth observed among the participants of this study compared with other studies may be related to the age, severity of illness and degree of controllability. Furthermore, the patients in this study suffered from a severe illness, and this condition may provide patients to get some positive view. MS has severe consequences as unpredictability, limitations of role, physical pressure, exhaustion, and change in family relations (Malachy, Donald & Stenhoff, 2007).
The findings of study partially confirmed the research hypothesis and also confirmed Tedeschi and Calhoun’s theory (2004). Results of enhancing appreciate for life among patients with MS in the present study are also consistent with other studies suggesting an improved appreciation for life and modified perceptions about what experiences are important for people dealing with significant difficulties (Garnefski, Kraaij, & Schroevers, 2008). Participants reported betterment for the spiritual changes. Spirituality may help people to view their suffering in a meaningful framework. The findings of the present study corroborate with the previous study suggesting that spirituality is related to posttraumatic growth as a way of making meaning out of the stressful event (Losiak & Nikiel, 2014).
This result is consistent with the study indicating a positive change following a diagnosis of chronic illness such as cancer, AIDS, and heart disease. It has been reported in some studies that patients with severe conditions perceiving positive changes were more likely to experience growth and also a better quality of life (Carroll, 2014). The findings of this study are also in agreement with several studies exploring posttraumatic growth in patients with MS. For example, Ackroyd et al., (2011) found a higher growth in these patients following the diagnosis of illness.
Furthermore; the findings showed that among cognitive emotion regulation strategies, only reappraisal and positive refocusing significantly predicted posttraumatic growth. These results are in line with a previous study indicating that reappraisal and positive refocusing are related to posttraumatic growth (Aldao, et al., 2014). It has also been found that in patients with myocardial infarction, posttraumatic growth was significantly correlated with positive refocusing and positive reappraisal (Losiak & Nikiel, 2014). Moreover, in a study carried out on women with breast cancer, a positive association was found between patients’ positive growth and reappraisal (Holland, et al., 2015). Another study has also reported a positive relation between posttraumatic growth and adaptive coping (Tedeschi & Calhoun, 2004). In general, active and problem-focused coping strategies have been shown to be related to psychological well-being in chronic disease patients, whereas avoidant and emotion-focused strategies are associated with negative outcomes (Kennedy, 2012).
This study highlighted the important role of positive refocusing and positive reappraisal in the adjustment of the patients with MS. Positive refocusing entails thinking about the steps to take ways of coping with a negative event (Li, Zhu, Yang, He, Yi, Wang, & Zhang, 2005). Reappraisal coping strategies are likely to lead an individual to engage in cognitive and emotional processes that are necessary to better cope with traumatic conditions (Smith, Ruiz, & Uchino, 2000). Indeed, cognitive processing is crucial to being able to experience posttraumatic growth (Calhoun & Tedeschi, 1998). Cognitive processing focused on individual’s struggles to make sense of the trauma, and the creation of a new view is necessary for posttraumatic growth to happen (Calhoun & Tedeschi, 1998).
One possible explanation may be that use of positive refocusing or reappraisal coping strategies leads to better outcomes in situations where individuals have no control over the stressful situation. Furthermore, this type of coping strategies allows patients to focus their energy on controllable aspects of stressful situations (Askay & Magyar-Russell 2009). Additionally, the results of this study provide partial support to the posttraumatic growth theory which assumes that traumatic events such as chronic diseases have the potential to lead to positive results as a function of cognitive (Tedeschi & Calhoun, 2004).
This study has some limitations. First, using the self-report measures was one of the drawbacks of this study. Further studies are encouraged to take qualitative method into account. Second, the relatively small sample size was another limitation to this study. Future studies should recruit a more diverse group of patients with MS. Third, using convenience sampling method was another limitation of this study. For patients with MS who face considerable stress related to neurological problems and impairments in personal functioning, coping may be a particularly important factor in promoting health and quality of life. This study showed that the majority of patients with MS experienced some degree of posttraumatic growth. It was also highlighted that using reappraisal and refocusing strategies may have a significant impact on patients’ positive posttraumatic growth.
This research has significant implications for clinicians working with patients struggling with chronic diseases. Based on the results of this study, psychological interventions and training program should be applied in a therapeutic plan to promote the coping strategies for MS patients.
The present study demonstrated that the majority of the patients with MS experienced posttraumatic growth. The findings also indicated that reappraisal and positive refocusing coping strategies had a significant role in posttraumatic growth. This study highlighted the positive consequences of stressful conditions such as chronic illnesses.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. We would like to thank the MS society in Shiraz for cooperation in this study and also multiple sclerosis patients for their participation.
Conflict of Interest
The authors have no conflicts of interest to declare.
References
Ackroyd, K., Fortune, D. G., Price, S., Howell, S., Sharrack, B., & Issac, C. L. (2011). Adversarial growth in patients with multiple sclerosis and their partners: relationships with illness perception, disability and distress. Journal of Clinical Psychology in Medical Settings, 18(4), 372-9. doi: 10.1007/s10880-011-9265-0
Aldao, A., Jazaieri, H., Goldin, P. R., & Gross, J. J. (2014). Adaptive and maladaptive emotion regulation strategies: Interactive effects during CBT for social anxiety disorder. Journal of Anxiety Disorders, 28(4), 382–389. doi: 10.1016/j.janxdis.2014.03.005
Aldao, A., & Nolen-Hoeksema, S. (2010). Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Behaviour Research and Therapy, 48(10), 974–983. doi: 10.1016/j.brat.2010.06.002
Askay, S. W., & Magyar-Russell., G. (2009). Posttraumatic growth and spirituality in burn recovery. International Review of Psychiatry, 21(6), 570-579. doi: 10.3109/09540260903344107
Bargh, J. A., & Williams, L. E. (2007). On the non-conscious of emotion regulation. In J. Gross (Ed.), Handbook of Emotion Regulation (pp. 225). New York: Guilford Press.
Calhoun, L. G., & Tedeschi, R. G. (1998). Beyond Recovery From Trauma: Implications for Clinical Practice and Research. Journal of Social Issues, 54(2), 357–71. doi: 10.1111/0022-4537.701998070
Calhoun, L. G., & Tedeschi, R. G. (2006). Handbook of Posttraumatic Growth: Research and Practice. Abingdon: Routledge.
Carroll, M. (2014). Personal growth after traumatic experience. Nursing Times, 31, 23-25.
Dadkhah, A., & Shirinbayan, P. (2012). Cognitive emotion regulation in aged people: Standardization of Cognitive Emotion Regulation Questionnaire in Iran. Iranian Rehabilitation Journal, 10(1), 24-7.
Danhauer, S. C., Case, L. D., Tedeschi, R., Russell, G., Vishnevsky, T., Triplett, K., et al. (2013). Predictors of posttraumatic growth in women with breast cancer. Psycho-Oncology, 22(12), 2676–2683. doi: 10.1002/pon.3298
Fazzito, M. M., Jordy, S. S., & Tilbery, C. P. (2009). Psychiatric disorders in multiple sclerosis patients. Arquivos de Neuro-Psiquiatria, 67(3a), 664–667. doi: 10.1590/s0004-282x2009000400017
Field, A. (2007). Discovering statistics using SPSS. Thousand Oaks, California: Sage.
Garnefski, N., Kraaij, V., & Spinhoven, P. (2002). Manual for the use of the Cognitive Emotion Regulation Questionnaire. Netherlands: DATEC.
Garnefski, N., Kraaij, V., & Schroevers, M. J. (2008). Post-traumatic growth after a myocardial infarction: A matter of personality, psychological health, or cognitive coping. Journal of Clinical Psychology in Medical Settings, 15(4), 270-77. doi: 10.1007/s10880-008-9136-5
Gorgen, S. M., Hiller, W., & Witthoft, M. (2014). Health anxiety, cognitive coping, and emotion regulation: A latent variable approach. International Journal of Behavior Medicine, 21(2), 364-74. doi: 10.1007/s12529-013-9297-y
Holland, J. C., Breitbart, W. S., Butow, P. N., Jacobsen, P. B., Loscalzo, M. J., & McCorkle, P. (2015). Psycho-Oncology. Oxford: Oxford University Press.
Hoang, H., Laursen, B., Stenager, E. N., & Stenager, E. (2015). Psychiatric co-morbidity in multiple sclerosis: The risk of depression and anxiety before and after MS diagnosis. Multiple Sclerosis Journal, 22(3), 347–353. doi: 10.1177/1352458515588973
Li, L., Zhu, X., Yang, Y., He, J., Yi, J., Wang, Y., & Zhang, J. (2015). Cognitive emotion regulation: Characteristics and effect on quality of life in women with breast cancer. Health and Quality of Life Outcomes, 13, 51. doi: 10.1186/s12955-015-0242-4
Kennedy, P. (2012). The Oxford handbook of rehabilitation psychology. Oxford: Oxford University Press.
Leung, Y. W., Gravely-Witte, S., Macpherson, A., Irvine, J., Stewart, D. E., & Grace, S. L. (2010). Post-traumatic growth among cardiac outpatients. Journal of Health Psychology, 15(7), 1049-63. doi: 10.1177/1359105309360577
Lode, K., Bru, E., Klevan, G., Myhr, K. M., & Larsen, J. P. (2010). Coping with multiple sclerosis: a 5-year follow-up study. Acta Neurologica Scandinavia, 122(5), 336-42. doi: 10.1111/j.1600-0404.2009.01313.x
Losiak, W., & Nikiel, J. (2014). Posttraumatic growth in patients after myocardial infarction: The role of cognitive coping and experience of life threat. Health Psychology Report, 2(4), 256-62. doi: 10.5114/hpr.2014.45894
Malachy, B., Donald, M., & Stenhoff, S. (2007). Psychological adaptation and quality of life in multiple sclerosis: Assessment of the disability centrality model. Rehabilitation, 73(1), 3-12.
Mennin, D. S., & Farach, F. J. (2007). Emotion and evolving treatments for adult psychopathology. Clinical Psychology: Science and Practice, 14(4), 329–352. doi: 10.1111/j.1468-2850.2007.00094.x
Philips, L. H., Henry, J. D., Nouzova, E., Cooper, C., Radlak, B., & Summers, F. (2014). Difficulties with emotion regulation in multiple sclerosis: Links to executive function, mood, and quality of life. Journal of Clinical Neuropsychology, 36(8), 831-42. doi: 10.1080/13803395.2014.946891
Rabinowitz, A. R., & Arnett, P. A. (2013). Coping in neuropsychological disorders. In J. J. Randolph (Ed.), Positive Neuropsychology: Evidence-Based Perspectives on Promoting (pp. 13-24). Berlin: Springer.
Schraub, E. M., Turgut, S., Clavairoly, V., & Sonntag, K. (2013). Emotion regulation as a determinant of recovery experience and well-being: A day-level study. International Journal of Stress Management, 20(4), 307-335. doi: 10.1037/a0034483
Seyed-Mahmoodi, J., Rahimi, C., & Mohammadi, N. (2013). [Psychometric Properties of Posttraumatic Growth Inventory in an Iranian Sample (Persian)]. Journal of Psychological Models and Methods, 3(12), 93-108.
Smith, T. W., Ruiz, J. M., & Uchino, B. N. (2000). Vigilance, active coping, and cardiovascular reactivity during social interaction in young men. Health Psychology, 19(4), 382–392. doi: 10.1037/0278-6133.19.4.382
Stanton, A. L., Bower, J. E., & Low, C. A. (2006). Posttraumatic growth after cancer. In: Calhoun G, Tedeschi RG., (Eds). Handbook of Posttraumatic Growth: Research and Practice. Abingdon: Routledge.
Taku, K., Calhoun, L. G., Tedeschi, R. G., Gil-Rivas, V., Kilmer, R. P., & Cann, A. (2007). Examining posttraumatic growth among Japanese university students. Anxiety, Stress, & Coping, 20(4), 353–367. doi: 10.1080/10615800701295007
Tedeschi, R. G., & Calhoun, L. G. (2004). Posttraumatic growth: conceptual foundations and empirical evidence. Psychological Inquiry, 15(1), 1–18. doi: 10.1207/s15327965pli1501_01
Tedeschi, R. G., & Calhoun, L. G. (1996). The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. doi: 10.1007/bf02103658
The findings showed that almost all patients with MS experienced posttraumatic growth at least to some degree. The level of posttraumatic growth observed in this study was higher than that previously reported in other MS (Ackroyd, Fortune, Price, Howell, Sharrack, & Issac, 2011), cardiac (Leung, Gravely-Witte, Macpherson, Irvine, Stewart, & Grace, 2010), and breast cancer (Holland Breitbart, Butow, Jacobsen, Loscalzo, & McCorkle, 2015) patients. The discrepancy on posttraumatic growth observed among the participants of this study compared with other studies may be related to the age, severity of illness and degree of controllability. Furthermore, the patients in this study suffered from a severe illness, and this condition may provide patients to get some positive view. MS has severe consequences as unpredictability, limitations of role, physical pressure, exhaustion, and change in family relations (Malachy, Donald & Stenhoff, 2007).
The findings of study partially confirmed the research hypothesis and also confirmed Tedeschi and Calhoun’s theory (2004). Results of enhancing appreciate for life among patients with MS in the present study are also consistent with other studies suggesting an improved appreciation for life and modified perceptions about what experiences are important for people dealing with significant difficulties (Garnefski, Kraaij, & Schroevers, 2008). Participants reported betterment for the spiritual changes. Spirituality may help people to view their suffering in a meaningful framework. The findings of the present study corroborate with the previous study suggesting that spirituality is related to posttraumatic growth as a way of making meaning out of the stressful event (Losiak & Nikiel, 2014).
This result is consistent with the study indicating a positive change following a diagnosis of chronic illness such as cancer, AIDS, and heart disease. It has been reported in some studies that patients with severe conditions perceiving positive changes were more likely to experience growth and also a better quality of life (Carroll, 2014). The findings of this study are also in agreement with several studies exploring posttraumatic growth in patients with MS. For example, Ackroyd et al., (2011) found a higher growth in these patients following the diagnosis of illness.
Furthermore; the findings showed that among cognitive emotion regulation strategies, only reappraisal and positive refocusing significantly predicted posttraumatic growth. These results are in line with a previous study indicating that reappraisal and positive refocusing are related to posttraumatic growth (Aldao, et al., 2014). It has also been found that in patients with myocardial infarction, posttraumatic growth was significantly correlated with positive refocusing and positive reappraisal (Losiak & Nikiel, 2014). Moreover, in a study carried out on women with breast cancer, a positive association was found between patients’ positive growth and reappraisal (Holland, et al., 2015). Another study has also reported a positive relation between posttraumatic growth and adaptive coping (Tedeschi & Calhoun, 2004). In general, active and problem-focused coping strategies have been shown to be related to psychological well-being in chronic disease patients, whereas avoidant and emotion-focused strategies are associated with negative outcomes (Kennedy, 2012).
This study highlighted the important role of positive refocusing and positive reappraisal in the adjustment of the patients with MS. Positive refocusing entails thinking about the steps to take ways of coping with a negative event (Li, Zhu, Yang, He, Yi, Wang, & Zhang, 2005). Reappraisal coping strategies are likely to lead an individual to engage in cognitive and emotional processes that are necessary to better cope with traumatic conditions (Smith, Ruiz, & Uchino, 2000). Indeed, cognitive processing is crucial to being able to experience posttraumatic growth (Calhoun & Tedeschi, 1998). Cognitive processing focused on individual’s struggles to make sense of the trauma, and the creation of a new view is necessary for posttraumatic growth to happen (Calhoun & Tedeschi, 1998).
One possible explanation may be that use of positive refocusing or reappraisal coping strategies leads to better outcomes in situations where individuals have no control over the stressful situation. Furthermore, this type of coping strategies allows patients to focus their energy on controllable aspects of stressful situations (Askay & Magyar-Russell 2009). Additionally, the results of this study provide partial support to the posttraumatic growth theory which assumes that traumatic events such as chronic diseases have the potential to lead to positive results as a function of cognitive (Tedeschi & Calhoun, 2004).
This study has some limitations. First, using the self-report measures was one of the drawbacks of this study. Further studies are encouraged to take qualitative method into account. Second, the relatively small sample size was another limitation to this study. Future studies should recruit a more diverse group of patients with MS. Third, using convenience sampling method was another limitation of this study. For patients with MS who face considerable stress related to neurological problems and impairments in personal functioning, coping may be a particularly important factor in promoting health and quality of life. This study showed that the majority of patients with MS experienced some degree of posttraumatic growth. It was also highlighted that using reappraisal and refocusing strategies may have a significant impact on patients’ positive posttraumatic growth.
This research has significant implications for clinicians working with patients struggling with chronic diseases. Based on the results of this study, psychological interventions and training program should be applied in a therapeutic plan to promote the coping strategies for MS patients.
The present study demonstrated that the majority of the patients with MS experienced posttraumatic growth. The findings also indicated that reappraisal and positive refocusing coping strategies had a significant role in posttraumatic growth. This study highlighted the positive consequences of stressful conditions such as chronic illnesses.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. We would like to thank the MS society in Shiraz for cooperation in this study and also multiple sclerosis patients for their participation.
Conflict of Interest
The authors have no conflicts of interest to declare.
References
Ackroyd, K., Fortune, D. G., Price, S., Howell, S., Sharrack, B., & Issac, C. L. (2011). Adversarial growth in patients with multiple sclerosis and their partners: relationships with illness perception, disability and distress. Journal of Clinical Psychology in Medical Settings, 18(4), 372-9. doi: 10.1007/s10880-011-9265-0
Aldao, A., Jazaieri, H., Goldin, P. R., & Gross, J. J. (2014). Adaptive and maladaptive emotion regulation strategies: Interactive effects during CBT for social anxiety disorder. Journal of Anxiety Disorders, 28(4), 382–389. doi: 10.1016/j.janxdis.2014.03.005
Aldao, A., & Nolen-Hoeksema, S. (2010). Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Behaviour Research and Therapy, 48(10), 974–983. doi: 10.1016/j.brat.2010.06.002
Askay, S. W., & Magyar-Russell., G. (2009). Posttraumatic growth and spirituality in burn recovery. International Review of Psychiatry, 21(6), 570-579. doi: 10.3109/09540260903344107
Bargh, J. A., & Williams, L. E. (2007). On the non-conscious of emotion regulation. In J. Gross (Ed.), Handbook of Emotion Regulation (pp. 225). New York: Guilford Press.
Calhoun, L. G., & Tedeschi, R. G. (1998). Beyond Recovery From Trauma: Implications for Clinical Practice and Research. Journal of Social Issues, 54(2), 357–71. doi: 10.1111/0022-4537.701998070
Calhoun, L. G., & Tedeschi, R. G. (2006). Handbook of Posttraumatic Growth: Research and Practice. Abingdon: Routledge.
Carroll, M. (2014). Personal growth after traumatic experience. Nursing Times, 31, 23-25.
Dadkhah, A., & Shirinbayan, P. (2012). Cognitive emotion regulation in aged people: Standardization of Cognitive Emotion Regulation Questionnaire in Iran. Iranian Rehabilitation Journal, 10(1), 24-7.
Danhauer, S. C., Case, L. D., Tedeschi, R., Russell, G., Vishnevsky, T., Triplett, K., et al. (2013). Predictors of posttraumatic growth in women with breast cancer. Psycho-Oncology, 22(12), 2676–2683. doi: 10.1002/pon.3298
Fazzito, M. M., Jordy, S. S., & Tilbery, C. P. (2009). Psychiatric disorders in multiple sclerosis patients. Arquivos de Neuro-Psiquiatria, 67(3a), 664–667. doi: 10.1590/s0004-282x2009000400017
Field, A. (2007). Discovering statistics using SPSS. Thousand Oaks, California: Sage.
Garnefski, N., Kraaij, V., & Spinhoven, P. (2002). Manual for the use of the Cognitive Emotion Regulation Questionnaire. Netherlands: DATEC.
Garnefski, N., Kraaij, V., & Schroevers, M. J. (2008). Post-traumatic growth after a myocardial infarction: A matter of personality, psychological health, or cognitive coping. Journal of Clinical Psychology in Medical Settings, 15(4), 270-77. doi: 10.1007/s10880-008-9136-5
Gorgen, S. M., Hiller, W., & Witthoft, M. (2014). Health anxiety, cognitive coping, and emotion regulation: A latent variable approach. International Journal of Behavior Medicine, 21(2), 364-74. doi: 10.1007/s12529-013-9297-y
Holland, J. C., Breitbart, W. S., Butow, P. N., Jacobsen, P. B., Loscalzo, M. J., & McCorkle, P. (2015). Psycho-Oncology. Oxford: Oxford University Press.
Hoang, H., Laursen, B., Stenager, E. N., & Stenager, E. (2015). Psychiatric co-morbidity in multiple sclerosis: The risk of depression and anxiety before and after MS diagnosis. Multiple Sclerosis Journal, 22(3), 347–353. doi: 10.1177/1352458515588973
Li, L., Zhu, X., Yang, Y., He, J., Yi, J., Wang, Y., & Zhang, J. (2015). Cognitive emotion regulation: Characteristics and effect on quality of life in women with breast cancer. Health and Quality of Life Outcomes, 13, 51. doi: 10.1186/s12955-015-0242-4
Kennedy, P. (2012). The Oxford handbook of rehabilitation psychology. Oxford: Oxford University Press.
Leung, Y. W., Gravely-Witte, S., Macpherson, A., Irvine, J., Stewart, D. E., & Grace, S. L. (2010). Post-traumatic growth among cardiac outpatients. Journal of Health Psychology, 15(7), 1049-63. doi: 10.1177/1359105309360577
Lode, K., Bru, E., Klevan, G., Myhr, K. M., & Larsen, J. P. (2010). Coping with multiple sclerosis: a 5-year follow-up study. Acta Neurologica Scandinavia, 122(5), 336-42. doi: 10.1111/j.1600-0404.2009.01313.x
Losiak, W., & Nikiel, J. (2014). Posttraumatic growth in patients after myocardial infarction: The role of cognitive coping and experience of life threat. Health Psychology Report, 2(4), 256-62. doi: 10.5114/hpr.2014.45894
Malachy, B., Donald, M., & Stenhoff, S. (2007). Psychological adaptation and quality of life in multiple sclerosis: Assessment of the disability centrality model. Rehabilitation, 73(1), 3-12.
Mennin, D. S., & Farach, F. J. (2007). Emotion and evolving treatments for adult psychopathology. Clinical Psychology: Science and Practice, 14(4), 329–352. doi: 10.1111/j.1468-2850.2007.00094.x
Philips, L. H., Henry, J. D., Nouzova, E., Cooper, C., Radlak, B., & Summers, F. (2014). Difficulties with emotion regulation in multiple sclerosis: Links to executive function, mood, and quality of life. Journal of Clinical Neuropsychology, 36(8), 831-42. doi: 10.1080/13803395.2014.946891
Rabinowitz, A. R., & Arnett, P. A. (2013). Coping in neuropsychological disorders. In J. J. Randolph (Ed.), Positive Neuropsychology: Evidence-Based Perspectives on Promoting (pp. 13-24). Berlin: Springer.
Schraub, E. M., Turgut, S., Clavairoly, V., & Sonntag, K. (2013). Emotion regulation as a determinant of recovery experience and well-being: A day-level study. International Journal of Stress Management, 20(4), 307-335. doi: 10.1037/a0034483
Seyed-Mahmoodi, J., Rahimi, C., & Mohammadi, N. (2013). [Psychometric Properties of Posttraumatic Growth Inventory in an Iranian Sample (Persian)]. Journal of Psychological Models and Methods, 3(12), 93-108.
Smith, T. W., Ruiz, J. M., & Uchino, B. N. (2000). Vigilance, active coping, and cardiovascular reactivity during social interaction in young men. Health Psychology, 19(4), 382–392. doi: 10.1037/0278-6133.19.4.382
Stanton, A. L., Bower, J. E., & Low, C. A. (2006). Posttraumatic growth after cancer. In: Calhoun G, Tedeschi RG., (Eds). Handbook of Posttraumatic Growth: Research and Practice. Abingdon: Routledge.
Taku, K., Calhoun, L. G., Tedeschi, R. G., Gil-Rivas, V., Kilmer, R. P., & Cann, A. (2007). Examining posttraumatic growth among Japanese university students. Anxiety, Stress, & Coping, 20(4), 353–367. doi: 10.1080/10615800701295007
Tedeschi, R. G., & Calhoun, L. G. (2004). Posttraumatic growth: conceptual foundations and empirical evidence. Psychological Inquiry, 15(1), 1–18. doi: 10.1207/s15327965pli1501_01
Tedeschi, R. G., & Calhoun, L. G. (1996). The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. doi: 10.1007/bf02103658
Type of Study: Original Research Article |
Subject:
Cognitive behavioral
Received: 2017/04/10 | Accepted: 2017/08/5 | Published: 2018/01/1
Received: 2017/04/10 | Accepted: 2017/08/5 | Published: 2018/01/1
References
1. Ackroyd, K., Fortune, D. G., Price, S., Howell, S., Sharrack, B., & Issac, C. L. (2011). Adversarial growth in patients with multiple sclerosis and their partners: relationships with illness perception, disability and distress. Journal of Clinical Psychology in Medical Set-tings, 18(4), 372-9. doi: 10.1007/s10880-011-9265-0 [DOI:10.1007/s10880-011-9265-0]
2. Aldao, A., Jazaieri, H., Goldin, P. R., & Gross, J. J. (2014). Adaptive and maladaptive emotion regulation strategies: Interactive ef-fects during CBT for social anxiety disorder. Journal of Anxiety Disorders, 28(4), 382–389. doi: 10.1016/j.janxdis.2014.03.005 [DOI:10.1016/j.janxdis.2014.03.005]
3. Aldao, A., & Nolen-Hoeksema, S. (2010). Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Be-haviour Research and Therapy, 48(10), 974–983. doi: 10.1016/j.brat.2010.06.002 [DOI:10.1016/j.brat.2010.06.002]
4. Askay, S. W., & Magyar-Russell., G. (2009). Posttraumatic growth and spirituality in burn recovery. International Review of Psychia-try, 21(6), 570-579. doi: 10.3109/09540260903344107 [DOI:10.3109/09540260903344107]
5. Bargh, J. A., & Williams, L. E. (2007). On the non-conscious of emotion regulation. In J. Gross (Ed.), Handbook of Emotion Regulation (pp. 225). New York: Guilford Press.
6. Calhoun, L. G., & Tedeschi, R. G. (1998). Beyond Recovery From Trauma: Implications for Clinical Practice and Research. Journal of Social Issues, 54(2), 357–71. doi: 10.1111/0022-4537.701998070 [DOI:10.1111/0022-4537.701998070]
7. Calhoun, L. G., & Tedeschi, R. G. (2006). Handbook of Posttraumatic Growth: Research and Practice. Abingdon: Routledge.
8. Carroll, M. (2014). Personal growth after traumatic experience. Nursing Times, 31, 23-25.
9. Dadkhah, A., & Shirinbayan, P. (2012). Cognitive emotion regulation in aged people: Standardization of Cognitive Emotion Regula-tion Questionnaire in Iran. Iranian Rehabilitation Journal, 10(1), 24-7.
10. Danhauer, S. C., Case, L. D., Tedeschi, R., Russell, G., Vishnevsky, T., Triplett, K., et al. (2013). Predictors of posttraumatic growth in women with breast cancer. Psycho-Oncology, 22(12), 2676–2683. doi: 10.1002/pon.3298 [DOI:10.1002/pon.3298]
11. Fazzito, M. M., Jordy, S. S., & Tilbery, C. P. (2009). Psychiatric disorders in multiple sclerosis patients. Arquivos de Neuro-Psiquiatria, 67(3a), 664–667. doi: 10.1590/s0004-282x2009000400017 [DOI:10.1590/S0004-282X2009000400017]
12. Field, A. (2007). Discovering statistics using SPSS. Thousand Oaks, California: Sage.
13. Garnefski, N., Kraaij, V., & Spinhoven, P. (2002). Manual for the use of the Cognitive Emotion Regulation Questionnaire. Netherlands: DATEC.
14. Garnefski, N., Kraaij, V., & Schroevers, M. J. (2008). Post-traumatic growth after a myocardial infarction: A matter of personality, psychological health, or cognitive coping. Journal of Clinical Psychology in Medical Settings, 15(4), 270-77. doi: 10.1007/s10880-008-9136-5 [DOI:10.1007/s10880-008-9136-5]
15. Gorgen, S. M., Hiller, W., & Witthoft, M. (2014). Health anxiety, cognitive coping, and emotion regulation: A latent variable ap-proach. International Journal of Behavior Medicine, 21(2), 364-74. doi: 10.1007/s12529-013-9297-y [DOI:10.1007/s12529-013-9297-y]
16. Holland, J. C., Breitbart, W. S., Butow, P. N., Jacobsen, P. B., Loscalzo, M. J., & McCorkle, P. (2015). Psycho-Oncology. Oxford: Ox-ford University Press. [DOI:10.1093/med/9780199363315.001.0001]
17. Hoang, H., Laursen, B., Stenager, E. N., & Stenager, E. (2015). Psychiatric co-morbidity in multiple sclerosis: The risk of depression and anxiety before and after MS diagnosis. Multiple Sclerosis Journal, 22(3), 347–353. doi: 10.1177/1352458515588973 [DOI:10.1177/1352458515588973]
18. Li, L., Zhu, X., Yang, Y., He, J., Yi, J., Wang, Y., & Zhang, J. (2015). Cognitive emotion regulation: Characteristics and effect on qual-ity of life in women with breast cancer. Health and Quality of Life Outcomes, 13, 51. doi: 10.1186/s12955-015-0242-4 [DOI:10.1186/s12955-015-0242-4]
19. Kennedy, P. (2012). The Oxford handbook of rehabilitation psychology. Oxford: Oxford University Press. [DOI:10.1093/oxfordhb/9780199733989.001.0001]
20. Leung, Y. W., Gravely-Witte, S., Macpherson, A., Irvine, J., Stewart, D. E., & Grace, S. L. (2010). Post-traumatic growth among cardiac outpatients. Jour-nal of Health Psychology, 15(7), 1049-63. doi: 10.1177/1359105309360577 [DOI:10.1177/1359105309360577]
21. Lode, K., Bru, E., Klevan, G., Myhr, K. M., & Larsen, J. P. (2010). Coping with multiple sclerosis: a 5-year follow-up study. Acta Neurologica Scandinavia, 122(5), 336-42. doi: 10.1111/j.1600-0404.2009.01313.x [DOI:10.1111/j.1600-0404.2009.01313.x]
22. Losiak, W., & Nikiel, J. (2014). Posttraumatic growth in patients after myocardial infarction: The role of cognitive coping and expe-rience of life threat. Health Psychology Report, 2(4), 256-62. doi: 10.5114/hpr.2014.45894 [DOI:10.5114/hpr.2014.45894]
23. Malachy, B., Donald, M., & Stenhoff, S. (2007). Psychological adaptation and quality of life in multiple sclerosis: Assessment of the disability centrality model. Rehabilitation, 73(1), 3-12.
24. Mennin, D. S., & Farach, F. J. (2007). Emotion and evolving treatments for adult psychopathology. Clinical Psychology: Science and Practice, 14(4), 329–352. doi: 10.1111/j.1468-2850.2007.00094.x [DOI:10.1111/j.1468-2850.2007.00094.x]
25. Philips, L. H., Henry, J. D., Nouzova, E., Cooper, C., Radlak, B., & Summers, F. (2014). Difficulties with emotion regulation in mul-tiple sclerosis: Links to executive function, mood, and quality of life. Journal of Clinical Neuropsychology, 36(8), 831-42. doi: 10.1080/13803395.2014.946891 [DOI:10.1080/13803395.2014.946891]
26. Rabinowitz, A. R., & Arnett, P. A. (2013). Coping in neuropsychological disorders. In J. J. Randolph (Ed.), Positive Neuropsychology: Evidence-Based Perspectives on Promoting (pp. 13-24). Berlin: Springer. [DOI:10.1007/978-1-4614-6605-5_2]
27. Schraub, E. M., Turgut, S., Clavairoly, V., & Sonntag, K. (2013). Emotion regulation as a determinant of recovery experience and well-being: A day-level study. International Journal of Stress Management, 20(4), 307-335. doi: 10.1037/a0034483 [DOI:10.1037/a0034483]
28. Seyed-Mahmoodi, J., Rahimi, C., & Mohammadi, N. (2013). [Psychometric Properties of Posttraumatic Growth Inventory in an Ira-nian Sample (Persian)]. Journal of Psychological Models and Methods, 3(12), 93-108.
29. Smith, T. W., Ruiz, J. M., & Uchino, B. N. (2000). Vigilance, active coping, and cardiovascular reactivity during social interaction in young men. Health Psychology, 19(4), 382–392. doi: 10.1037/0278-6133.19.4.382 [DOI:10.1037/0278-6133.19.4.382]
30. Stanton, A. L., Bower, J. E., & Low, C. A. (2006). Posttraumatic growth after cancer. In: Calhoun G, Tedeschi RG., (Eds). Handbook of Posttraumatic Growth: Research and Practice. Abingdon: Routledge.
31. Taku, K., Calhoun, L. G., Tedeschi, R. G., Gil-Rivas, V., Kilmer, R. P., & Cann, A. (2007). Examining posttraumatic growth among Japanese university students. Anxiety, Stress, & Coping, 20(4), 353–367. doi: 10.1080/10615800701295007 [DOI:10.1080/10615800701295007]
32. Tedeschi, R. G., & Calhoun, L. G. (2004). Posttraumatic growth: conceptual foundations and empirical evidence. Psychological In-quiry, 15(1), 1–18. doi: 10.1207/s15327965pli1501_01 [DOI:10.1207/s15327965pli1501_01]
33. Tedeschi, R. G., & Calhoun, L. G. (1996). The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9(3), 455–471. doi: 10.1007/bf02103658 [DOI:10.1007/BF02103658]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |