BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://jpcp.uswr.ac.ir/article-1-422-en.html
2- Department of Clinical Psychology, Faculty of Education and Psychology, Ferdowsi University of Mashhad, Mashhad, Iran.
3- Cognitive Science Research Center, Mashhad University of Medical Sciences, Mashhad, Iran.
1. Introduction
The main challenge of the 20th century was to survive, but the challenge of this century is the quality of life (Canbaz, Sunter, Dabak, & Peksen, 2003). The quality of life in aging is affected by three important factors: physical, emotional, and cognitive health (Lee, Ko, & Lee, 2006). Cognitive health in older age includes maintaining cognitive abilities that promote social interactions, goal-seeking, independence, and adjusting with age-related cognitive decline (Hendrie et al., 2006). While a society grows older, the risk of age-related cognitive decline and dementia also increases.
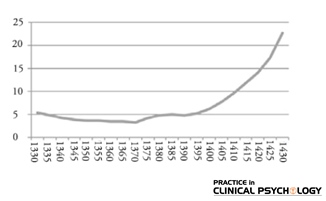
In the next 40 years, the world’s population over 60 will be doubled; 52% of them live in Asia and 40% of total elderly population live in developed countries (Center, 2007). According to the 2007 census, Iran with more than 7.27% aged population over 60 years has become an aging country and in the next 15 years, this percentage will reach 10.7. According to Figure 1, the Iranian population is getting old (Darabi, Torkashvand, & Latifi, 2012).
Figure 1. The The percentage of elderly in the population of Iran over the period 1330-1430 AH (1951-2051) (Darabi et al., 2012)
Thus, there is an increasing need for developing tools that quickly and reliably screen for elderly people at risk of cognitive disorders. Early detection of cognitive disorders in older adults can promote timely intervention. A short but sensitive screening tool for early diagnosis of dementia may help make initial distinctions between elderlies experiencing age-related cognitive decline and those experiencing cognitive deficits related to dementing disorders such as Alzheimer disease (Solomon et al., 1998).
Among the most widely used screening tests for cognitive functions are the Mini-Mental State Examination (MMSE) and the Clock Drawing Test (CDT). MMSE is a commonly used screening tool for cognitive impairment in older adults. The test can be used to distinguish between older adults with and without neuropsychiatric disorders and as a follow up test to measure the progress of the disorder across time (Cacho et al., 2010). MMSE asks questions that assess 5 areas of cognitive functioning (i.e., orientation, immediate memory, attention/concentration, delayed recall, language) (Shigemori, Ohgi, Okuyama, Shimura, & Schneider, 2010). The results of a few surveys indicate that the MSSE has become the most commonly used cognitive test by the health professionals such that approximately 9 out of 10 experts have reported using the test predominantly (Cacho et al., 2010). Farmer and his colleagues (1995) showed that in elderly people with baseline MMSE>23, education was a significant predictor of cognitive decline, not only in the elderly but also in younger participants. Cognitive function measured by the MMSE decreased with age (Butler, Ashford, & Snowdon, 1996).
CDT is widely used as a quick measure of cognitive impairment and dementia in primary care units (Shulman, 2000). Although CDT is a simple task, it requires most brain regions to generate a complete version of a clock face. When a subject is first given the verbal command to “draw a clock”, A) his or her temporal lobes decode the verbal information into semantic knowledge (Gazzaniga, Ivry, & Mangun, 2002), B) hippocampal regions, which are responsible for long-term visual memory get activated to regenerate an appropriate clock face layout (Bauer, Grande, & Valenstein, 2003), C) parietal lobe manage accurate visual perception needed to guide the recreation of a clock’s spatial arrangement (Jouk & Tuokko, 2012), D) frontal lobes responsible for executive functions assist in the planning, organization, and coordination of all multiple steps of clock drawing, monitoring and correcting for any errors, and E) motor cortex executes the drawing of the clock. It becomes clear that CDT relies on the integration of a wide variety of cortical and subcortical regions (Gazzaniga et al., 2002). Ferri and his colleagues (2005) found that age, sex, and educational level have statistically significant effects on CDT test scores. Older age and male gender are associated with lower performance on MMSE and CDT (Ferri et al., 2005). And there is a significant relationship between education and CDT performance (Fabricio, Aprahamian, & Yassuda, 2014).
Although the correlation between MMSE and CDT in the elderly has been studied in other countries (Shulman, Pushkar Gold, Cohen, & Zucchero, 1993; Schramm et al., 2002), there was no study addressing the strength of the relationship between the two tests among Iranian population of older adults. However, there was only one study which assessed reliability and validity of CDT in Iranian older population (Sadeghipour Roodsari, Akbari Kamrani, Foroughan, Mohammadi, & Karimloo, 2013). Hence, the present study of older adults evaluated the correlation between these two tests, and also the effect of three important factors; gender, age and educational level on MMSE and CDT performance.
A decline in memory and cognitive function is considered by many authorities to be a normal consequence of aging. Increased life expectancy does not associate with decreasing disabilities before death; despite the longer life, the older adults experience much disability until death that cause considerable suffering for them, their families, and incur huge socioeconomic costs to society (Sherwin, 2006). Therefore, prevention and treatment of cognitive impairment is important for aging population (Bae et al., 2015). In this regard, timely assessment and screening to identify older adults who are at risk of cognitive impairment seem necessary.
2. Methods
Participation in the study was voluntary and participants did not receive any monetary or other forms of incentives for their participation. The study population consisted of older adults aged over 60 years who referred to local health centers of Mashhad City with no Alzheimer disease or other cognitive disorders. A total of 70 healthy non-clinical sample of older adults were selected via convenience sampling method from two local health centers from the same civil servant area in Mashhad with the mean (SD) age of 69.70(6.41) years; (range=61-82 years); 57% females; mean (SD) years of education of 10.61(3.49) years. The inclusion criteria were as follows: 1) aged between 60 and 85 years; 2) Speak Persian as the native language; Exclusion criteria were as follows: having Alzheimer disease and a history of neurological disorders, 2) unwillingness to participate in the study, 3) Exclusion criteria were having no history of psychiatric and neurological disorders, 4) having no information about potential diagnosis indicative of compromised cognition.
The study was approved by Ethics Committee of Ferdowsi University of Mashhad. All participants completed the CDT and MMSE. Participants were tested individually in a quiet room at the health center. The test administration took approximately 15 minutes. Participants completed the MMSE and CDT in a fixed order. For the CDT, they were presented with a blank paper and a pencil, and were given the following instructions: “I would like you to draw a clock, put in all the numbers, and set the hands for 10 past 11.” A pre-drawn circle was not provided. For the MMSE, the participants were asked individually by the examiner and noted their answers.
MMSE was designed by Flosetin more than 40 years ago in 1975 as a practical method of grading cognitive impairment (Folstein, Folstein, & McHugh, 1975). The maximum score of MMSE is 30. It measures 5 cognitive domains: orientation to time and place, memory, attention and calculation, and language. Scores lower than 25 indicate cognitive impairment. Its test-retest reliability and the inter-rater reliability are 0.89 and 0.82, respectively (Koch, Gürtler, & Szecsey, 2005). The psychometric properties of MMSE evaluated in Iran, represent the reliability and validity of MMSE as 0.78; and at the cut point of 21, it showed 90% sensitivity and 84% specificity (Foroughan, Jafari, Shirin Bayan, Ghaem Magham Faraahani, & Rahgozar, 2008).
CDT is one of the seven neuropsychological tests most frequently used to assess cognitive functions in aging (Faria, Alves, & Charchat-Fichman, 2015). It was introduced in the early 20th century as an indicator of constructional apraxia (it is characterized by an inability or difficulty to build, assemble, or draw objects despite the patient’s understanding of the task, the instructions, and his/her capabilities and willingness to complete it) (Guérin, Ska, & Belleville, 1999). In 1986, Shulman and his colleagues published the first study associating CDT with the screening of elderly patients with cognitive disorders. Although CDT is a specific indicator of executive functions, the test assesses many cognitive skills that may be involved in early stage of Alzheimer disease, such as short-term memory, spatial orientation, abstract thinking, planning, concentration, executive and visuospatial skills (Aprahamian, Martinelli, Neri, & Yassuda, 2009).
This test requires the subject to draw the face of a clock with numbers and set the hands to “10 after 11.” There are also several scoring methods for this test (Solomon et al., 1998) and we used Shulman scoring system. The results are classified into 5 categories from 1 to 5, (Shulman et al., 1993), where 0 indicates a plot which has no reasonable resemblance to a clock, 1 denotes severe level of disorganization, 2 indicates moderate visuospatial disorganizations of times, 3 refers to inaccurate representation of 10 after 11 with only minor deviations, 4 indicates minor visuospatial errors, and 5 denotes a perfect clock. Test-retest correlation using these categories was 0.89 and inter-rater correlation achieved 0.81. Its specificity and sensitivity appear to be slightly lower compared to the MMSE (Koch et al., 2005). The psychometric properties of CDT were evaluated in Iran, and would result in the test-retest reliability of 0.554 and ICC for inter-rater reliability was 0.96 (Sadeghipour Roodsari et al., 2013). CDT is quicker and easier to administer since there is no need for special materials.
3. Results
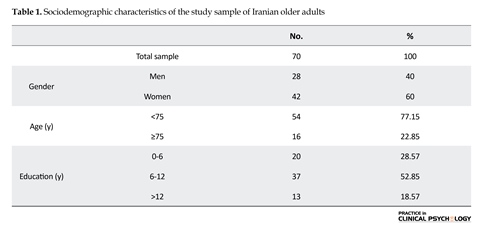
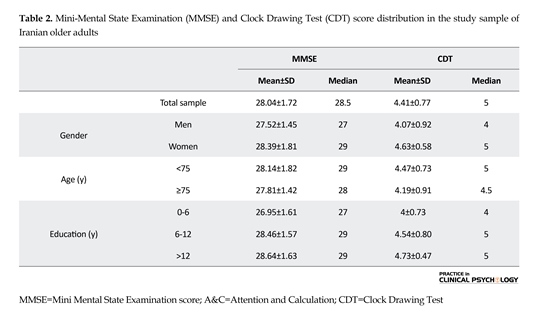
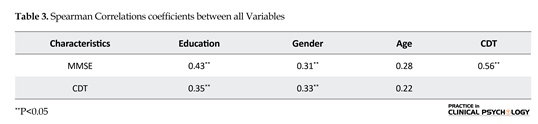
A correlation matrix was calculated among the MMSE and CDT, gender, age (<75 years or ≥75 years of age) and educational level (0-6, 6-12, and 12 year and higher). Because the distribution of data was not normal, Spearman’s correlation coefficient (ρ), a nonparametric test, was used. Table 1 presents the sociodemographic characteristics of the study population. The mean age was 69.70 years (SD=6.41) with a range of 61 to 88 years and 57% of participants were women. The median MMSE score was 28.5 (range 23–30). The median CDT score was 4.5 (range=2-5). Score distribution of both tests in the total sample and according to gender, age and educational level are presented in Table 2.
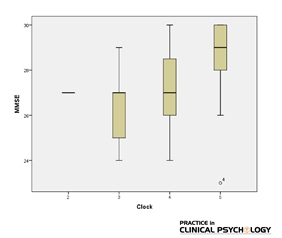
The MMSE score distribution for each CDT score in the total sample is shown in Figure 2. The higher the CDT score, the higher the MMSE scores would be. Thus, there is an increasing need for developing tools that quickly and reliably screen for elderly people at risk of cognitive disorders. Early detection of cognitive disorders in older adults can promote timely intervention. A short but sensitive screening tool for early diagnosis of dementia may help make initial distinctions between elderlies experiencing age-related cognitive decline and those experiencing cognitive deficits related to dementing disorders such as Alzheimer disease (Solomon et al., 1998).
Among the most widely used screening tests for cognitive functions are the mini-mental state examination (MMSE) and the Clock Drawing Test (CDT). MMSE is a commonly used screening tool for cognitive impairment in older adults. The test can be used to distinguish between older adults with and without neuropsychiatric disorders and as a follow up test to measure the progress of the disorder across time (Cacho et al., 2010). MMSE asks questions that assess 5 areas of cognitive functioning (i.e., orientation, immediate memory, attention/concentration, delayed recall, language) (Shigemori et al., 2010). The results of a few surveys indicate that the MSSE has become the most commonly used cognitive
test by the health professionals such that approximately 9 out of 10 experts have reported using the test predominantly (Cacho et al., 2010). Farmer and his colleagues (1995) showed that in elderly people with baseline MMSE>23, education was a significant predictor of cognitive decline, not only in the elderly but also in younger participants. Cognitive function measured by the MMSE decreased with age (Butler, et al., 1996).
CDT has been also broadly used as a quick measure of cognitive impairment and dementia in primary care (Shulman, 2000). Although CDT is a simple task, it requires most of the brain regions to generate a complete version of a clock face. When a subject is first given the verbal command to “draw a clock,” A), temporal lobes decodes the verbal information into semantic knowledge (Gazzaniga et al., 2002), B), hippocampal regions, which are responsible for long-term visual memory should be activated to retrieve mechanisms needed to regenerate an appropriate clock face layout (Bauer et al., 2003), C), parietal lobe should manage accurate visual perception that is needed to guide the recreation of a clock’s spatial arrangement (Jouk & Tuokko, 2012), D), frontal lobes responsible for executive functions assist in the planning, organization, and coordination of all multiple steps of clock drawing, monitoring and correcting for any errors, and E) motor cortex must execute the drawing of the clock. It becomes clear that CDT relies on the integration of a wide variety of cortical and subcortical regions (Gazzaniga et al., 2002). Ferri and his colleagues (1991) found that age, sex, and educational level have statistically significant effects on CDT test scores. Older age and male gender are associated with lower performance on MMSE and CDT (Ferri et al., 2005). And there is a significant relationship between education and CDT performance (Fabricio et al., 2014).
Figure 2. Distribution of Mini-Mental State Examination (MMSE) scores according to Clock Drawing Test (CDT) scores in the study sample of Iranian older adults
Although the correlation between MMSE and CDT in the elderly has been studied in other countries (Shulman et al., 1993; Schramm et al., 2002), there was no study addressing the strength of the relationship between the two tests among Iranian population of older adults. However, there was only one study which assessed reliability and validity of CDT in Iranian older population (Sadeghipour Roodsari et al., 2013). Hence, the present study of older adults evaluated the correlation between these two tests, and also the effect of three important factors; gender, age and educational level on MMSE and CDT performance.
A decline in memory and cognitive function is considered by many authorities to be a normal consequence of aging. Increased life expectancy does not associate with decreasing disabilities before death; despite the longer life, the older adults experience much disability until death that cause considerable suffering for them, their families, and incur huge socioeconomic costs to society (Sherwin, 2006). Therefore, prevention and treatment of cognitive impairment is important for aging population (Bae et al., 2015). In this regard, timely assessment and screening to identify older adults who are at risk of cognitive impairment seem necessary.
4. Discussion
The early diagnosis of cognitive impairment and efficient interventions allow the elderly to maintain social interaction, abilities to function independently, functional recovery from illness, and to cope with residual functional deficits and finally can increase the quality of life in the elderly (Centers for Disease Control and Prevention, & Alzheimer's Association, 2007). The present study aimed to assess the relationship between CDT and MMSE in a nonclinical sample of 70 Iranians elderly.
The correlation between the MMSE and CDT was moderate (P=0.56) in this population of Iranian older adults with different educational level. This value was similar to the median Spearman correlation coefficient obtained in 8 studies (ρ=0.58) (Fuzikawa, Lima-Costa, Uchôa, & Shulman, 2007). Our study showed that older adults who received high scores in MMSE, have also good performance on CDT. Furthermore, there was a significant correlation between years of education and MMSE score (ρ=0.43) and also CDT score (ρ=0.33).
Likewise according to the result of Mann-Whitney U test, well-educated population are expected to obtain a high MMSE and CDT score. It showed that elderlies with high educational level received high scores in MMSE and also CDT. That is older adults with a higher educational level had a better cognitive function. We conclude that higher education might have protective effects in cognitive decline in old ages. This finding supports the passive theory of cognitive reserve; that is, higher levels of education are associated with better cognitive performance than lower level of education, a capability that may well be extended into the elderly postponing the onset of cognitive decline (Lenehan, Summers, Saunders, Summers, & Vickers, 2014). This result is consistent with previous studies which demonstrated the association of education with better performance in cognitive domains (Tucker-Drob, Johnson, & Jones, 2009; Zahodne et al., 2011).
There was a significant difference between male and female performance in MMSE and CDT tests. In general, the results showed that women tend to perform at a higher level than men on these two tests. The higher performance of older women in MMSE and CDT is likely due to their higher educational level, but the performance of elderly in these two tests was not affected by age. This result is consistent with the findings of Fabricio et al (2014) which revealed no significant differences between the age groups in cognitive performances in CDT and MMSE. One possible explanation is that no significant age differences were found due to the limited variability in age distribution in this study. The sample contained a small number of people over 75 years and also the educational level of them delayed age-related cognitive decline.
CDT and MMSE can be used as a very simple and quick method for assessing cognitive functions of elderly. They tap into a wide range of cognitive abilities. They are easy to administer, take very little time and more cost-effective screening instrument for use in primary care (Nishiwaki, 2004). Although these two tests measure different aspects of cognitive functioning, they are suited for screening elderlies who are at the risk of age-related cognitive decline. Many studies have shown that clock drawing (with a score range of 1-5) is strongly correlated with MMSE (Folstein et al., 1975); furthermore, CDT has a high correlation with the MMSE and other tests of cognitive dysfunction which are in consistence with our finding.
Although, Schramm et al (2002) found that combining CDT with MMSE improved sensitivity, Heinik, Solomesh, Bleich, and Berkman (2003) showed that the CDT plus MMSE combined improved both sensitivity and specificity compared with the CDT alone (Agrell & Dehlin, 1998). In addition, Samton et al (2005) found that MMSE performance and CDT were correlated as anticipated, but CDT was a more sensitive and consistent predictor of disposition compared to the MMSE. Therefore, early screening of cognitive decline to prevent and apply efficient and timely treatments in elderly is very important.
It seems that early screening and diagnosis in middle age, can provide early intervention and also implementation of some cognitive rehabilitation like cognitive training. Also stimulation program in daily routine of the elderly may delay age-related cognitive decline as there has been a general consensus that if older adults are motivated cognitively and trained to improve their mental powers, aging will not necessarily lead to cognitive decline (Papalia, Olds, & Feldman 1992).
It is suggested that future studies use more samples and cognitive screening tools and start cognitive assessments in early old age. Furthermore, the potential benefits of using cognitive rehabilitation programs include (cognitive training and cognitive stimulation) on elderly people who experience age-related cognitive decline and who are at risk of Alzheimer disease and mild cognitive impairment are assessed.
Although the results of this study showed that the performance of MMSE is similar and correlated with that of CDT in a group of 70 older adults, we are uncertain about the diagnostic power of the CDT when used as the only tool for screening people with cognitive impairment; therefore, our findings do not imply that clinicians should merely rely on CDT in their clinical assessments. However, we suggest that when administration skills and time are problematic, the CDT is quicker and easier tool to administer and score than the MMSE, and it can provide an initial reliable assessment of the clients’ cognitive status (Fuzikawa et al., 2007). Furthermore, CDT may be more practical in situations where the time for assessment or screening is limited, another limitation is the fact that this study did not include a complete clinical characterization of participants. It is suggested that future studies explore the contribution of the qualitative analysis of CDT in samples with various diseases associated with cognitive changes.
Acknowledgements
The present paper was extracted from M.A. thesis of the first author, Department of Clinical Psychology, Faculty of Education and Psychology, Ferdowsi University of Mashhad. We thank Dr. Reza Pishghadam for his productive comments on the earlier draft of the manuscript.
Conflict of Interest
The authors declared no conflicts of interest.
References
Agrell, B., & Dehlin, O (1998). The clock-drawing test. Age and Ageing, 27(3), 399–403. doi: 10.1093/ageing/27.3.399
Aprahamian, I., Martinelli, J. E., Neri, A. L., & Yassuda, M. S (2009). The Clock Drawing Test: A review of its accuracy in screening for dementia. Dementia & Neuropsychologia, 3(2), 74–80. doi: 10.1590/s1980-57642009dn30200002
Bae, J. B., Kim, Y. J., Han, J. W., Kim, T. H., Park, J. H., Lee, S. B., et al (2015). Incidence of and risk factors for Alzheimer's disease and mild cognitive impairment in Korean elderly. Dementia and Geriatric Cognitive Disorders, 39(1-2), 105-15. doi: 10.1159/000366555
Bauer, R. M., Grande, L., & Valenstein, E (2003). Amnesic disorders. In K. M. Heilman & E. Valenstein, (Eds.), Clinical Neuropsycholgy (pp. 495-573). New York: Oxford University Press.
Butler, S. M., Ashford, J. W., Snowdon, D. A (1996). Age, education, and changes in the Mini-Mental State Exam scores of older women: Findings from the Nun Study. Journal of the American Geriatrics Society, 44(6), 675-81. PMID: 8642159
Cacho, J., Benito-León, J., García-García, R., Fernández-Calvo, B., Vicente-Villardón, J. L., & Mitchell, A. J (2010). Does the combination of the MMSE and Clock Drawing Test (mini-clock) improve the detection of mild Alzheimer's disease and mild cognitive impairment. Journal of Alzheimer's Disease, 22(3), 889-96. doi: 10.3233/jad-2010-101182
Canbaz, S., Sünter, A. T., Dabak, S. & Pekşen, Y (2003). The prevalence of chronic diseases and quality of life in elderly people in Samsun. Turkish Journal of Medical Sciences, 33(5), 335-40.
Centers for Disease Control and Prevention, & Alzheimer's Association (2007). The healthy brain initiative: a national public health road map to maintaining cognitive health. Chicago: Alzheimer's Association.
Dadkhah, A (2007). [Review of aged rendered services in USA and Japan and Guidelines for Iran aging strategic plan (Persian)]. Iranian Journal of Aging, 2(3), 166-76.
Darabi, S., Torkashvand, M., & Latifi, G (2012). [Socio-economic consequences of the aging population in Iran (1951-1961) (Persian)]. Journal of Social Science, 58(16), 17-28.
Fabricio, A. T., Aprahamian, I., & Yassuda, M. S (2014). Qualitative analysis of the Clock Drawing Test by educational level and cognitive profile. Arquivos De Neuro-Psiquiatria, 72(4), 289–95. doi: 10.1590/0004-282x20140004
Faria, C. de A., Alves, H. V. D., & Charchat-Fichman, H (2015). The most frequently used tests for assessing executive functions in aging. Dementia & Neuropsychologia, 9(2), 149–55. doi: 10.1590/1980-57642015dn92000009
Farmer, M. E., Kittner, S. J., Rae, D. S., Bartko, J. J., & Regier, D. A (1995). Education and change in cognitive function. Annals of Epidemiology, 5(1), 1–7. doi: 10.1016/1047-2797(94)00047-w
Ferri, C. P., Prince, M., Brayne, C., Brodaty, H., Fratiglioni, L., Ganguli, M., et al (2005). Global prevalence of dementia: A Delphi consensus study. The Lancet, 366(9503), 2112–7. doi: 10.1016/s0140-6736(05)67889-0
Folstein, M. F., Folstein, S. E., & McHugh, P. R (1975). Mini-mental state. Journal of Psychiatric Research, 12(3), 189–98. doi: 10.1016/0022-3956(75)90026-6
Foroughan, M., Jafari, Z., Shirin Bayan P., Ghaem Magham Faraahani Z., & Rahgozar M (2008). [Validation of mini-mental state examination (MMSE) in the elderly population of Tehran (Persian)]. Advances in Cognitive Science, 10(2), 29-37.
Fuzikawa, C., Lima-Costa, M. F., Uchôa, E., & Shulman, K (2007). Correlation and agreement between the Mini-Mental State Examination and the Clock Drawing Test in older adults with low levels of schooling: The Bambuí Health Aging Study (BHAS). International Psychogeriatrics, 19(4), 657. doi: 10.1017/s1041610207005467
Gazzaniga, M. S., Ivry, R. B., & Mangun, G. R (2002). Cognitive neuroscience: The biology of the mind. New York: WW Norton & Company.
Guérin, F., Ska, B., & Belleville, S (1999). Cognitive processing of drawing abilities. Brain and Cognition, 40(3), 464–78. doi: 10.1006/brcg.1999.1079
Heinik, J., Solomesh, I., Bleich, A., & Berkman, P (2003). Are the Clock-Drawing Test and the MMSE combined interchangeable with CAMCOG as a dementia evaluation instrument in a specialized outpatient setting. Journal of Geriatric Psychiatry and Neurology, 16(2), 74–9. doi: 10.1177/0891988703016002002
Hendrie, H. C., Albert, M. S., Butters, M. A., Gao, S., Knopman, D. S., Launer, L. J., et al (2006). The NIH cognitive and emotional health project. Alzheimer’s & Dementia, 2(1), 12–32. doi: 10.1016/j.jalz.2005.11.004
Jouk, A., & Tuokko, H (2012). A reduced scoring system for the Clock Drawing Test using a population based sample. International Psychogeriatrics, 24(11), 1738–48. doi: 10.1017/s1041610212000804
Received: 2016/12/12 | Accepted: 2017/03/2 | Published: 2017/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |