Volume 13, Issue 4 (Autumn 2025)
PCP 2025, 13(4): 361-370 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Davari R. Effectiveness of Schema Therapy in Improving Defense Mechanisms and Mental Health in Patients With Acne Vulgaris. PCP 2025; 13 (4) :361-370
URL: http://jpcp.uswr.ac.ir/article-1-1041-en.html
URL: http://jpcp.uswr.ac.ir/article-1-1041-en.html
Department of Psychology, Roudehen Branch, Islamic Azad University, Roudehen, Iran. , dr.davari-rahim@yahoo.com
Full-Text [PDF 604 kb]
(602 Downloads)
| Abstract (HTML) (734 Views)
Full-Text: (281 Views)
Introduction
Acne vulgaris, commonly referred to as “teenage acne,” is a chronic inflammatory skin disease classified as a psychosomatic disorder. It affects approximately 9.4% of the global population (Ding et al., 2024). As the third most prevalent dermatological condition worldwide, it primarily manifests during adolescence and early adulthood, particularly in the second and third decades of life. The prevalence of this skin condition is estimated to be approximately 80%–85% (Marković et al., 2019).
Acne results from the clogging of skin pores due to excess oil (sebum) and dead skin cells. It can appear on the face, neck, chest, back, or shoulders, which are areas rich in sebaceous (oil) glands (Bhambri & Del Rosso, 2009). Research indicates that facial acne is significantly more common than acne on other body regions. The prevalence rates are reported to be 91% for facial acne, 54% for back acne, and 36% for chest acne. Approximately 20% of individuals experience severe acne, which can lead to permanent scarring (Sutaria & Schlessinger, 2020).
The clinical presentation of acne varies and includes papules (small red bumps), pustules (pus-filled lesions), cysts (painful pus-filled lumps beneath the skin), nodules (large painful lumps under the skin), whiteheads (closed clogged pores), and blackheads (open clogged pores where the sebum oxidizes upon exposure to air and darkens) (Ding et al., 2024).
The four primary physical causes of acne are as follows: (1) sebum overproduction, (2) accumulation of dead skin cells, (3) clogged hair follicles, and (4) bacterial infection. Hair follicles are connected to sebaceous glands that secrete sebum to lubricate the skin and hair. When excessive sebum and dead cells accumulate, they form a soft plug that creates an ideal environment for bacterial growth. Infected clogged pores trigger skin inflammation. If the clogged pore remains closed, it forms a whitehead; if open, a blackhead forms. Red pimples with white centers result from inflamed or infected follicles, while deeper blockages may develop into cysts (William & Delavar, 2012).
Psychosomatic skin disorders, such as nail biting, trichotillomania, psychogenic pruritus, dermatitis, urticaria, burning sensations, and exaggerated pain responses, are common conditions encountered by dermatologists (Bhambri & Del Rosso, 2009). Halvorsen et al. (2011) found that psychological stress plays a significant role in the development of acne, often arising from daily life events or as a consequence of having acne itself.
Stress contributes to the physiological processes of acne through biochemical pathways. Sebaceous glands have specific receptors for stress-related hormones, including corticotropin-releasing hormone, melanocortins, neuropeptide Y, and beta-endorphins. When these hormones bind to their receptors, they trigger the release of pro-inflammatory cytokines, stimulating sebaceous glands and exacerbating acne (Zouboulis et al., 2005; Zoulis & Bomm, 2004; Magin et al., 2008). Under stress, the production of corticosteroids and adrenal androgens increases, worsening acne symptoms.
The psychological impact of acne is profound. Many individuals, especially adolescents, experience heightened anxiety, depression, and diminished self-esteem. Acne can also interfere with the formation of one’s identity and personal development. These mental health challenges are often intensified by the social stigma associated with visible skin conditions (Ding et al., 2024).
Mental health and acne: Theoretical foundations and the role of schema therapy
The American Psychological Association (APA) defines mental health as a state in which individuals can cope appropriately with life challenges and utilize their emotional and psychological capacities to enhance their quality of life (QoL) and achieve success. According to the National Institute of Mental Health (NIMH), mental health involves a balance of cognitive, emotional, and behavioral functioning, enabling individuals to learn, manage stress, establish relationships, and adapt effectively to changes. The World Health Organization (WHO) describes mental health as a state in which an individual recognizes their own abilities, can cope with normal life stressors, work productively, and contribute to their community (Jain et al., 2024).
Although individuals live in objective (external) environments, they respond to events based on their subjective (internal) perceptions. Therefore, mental health is considered a key indicator of QoL (Dolan & Cautesous, 2014). It encompasses emotional responses to life events, psychological states, and judgments about satisfaction in areas such as marriage, work, and personal development (Nie et al., 2024).
Acne can inflict invisible psychological harm, significantly undermining self-esteem, particularly among women. Despite its psychological consequences, only a minority of acne sufferers seek psychological treatment (Galatino & Berson, 2018). Given the psychological underpinnings and the role of emotional conflict in such disorders, solely physiological treatments are often insufficient, highlighting the need for psychological interventions. This has led dermatologists and mental health professionals to collaborate on psychosomatic dermatology research and treatment (Behnam et al., 2010).
Dermatological lesions of acne, especially facial acne, which is the most prevalent, not only cause physical discomfort but also have negative psychosocial impacts on interpersonal interactions. Since acne often begins in adolescence, a period marked by heightened sensitivity to physical appearance, its presence can result in deeper psychological damage (Ding et al., 2024). This may initiate a psychosomatic cycle, where stress and emotional disturbances exacerbate acne symptoms and lead to chronic conditions, eventually contributing to the emergence of mental disorders, such as anxiety and depression. This, in turn, reinforces the cycle of psychosomatic dysfunction. Studies have shown that anxiety and stress delay wound healing by approximately 40% and are recognized as key factors in prolonging acne symptoms (Halvorsen, 2011).
Psychodermatological patients often present with comorbid conditions, including obsessive-compulsive personality disorder, body dysmorphic disorder, obsessive thoughts related to oily skin, eating disorders, substance abuse, trichotillomania, and borderline personality disorder (Picardi et al., 2006). Acne may trigger psychological distress and is frequently associated with psychiatric disorders (Misery, 2011). Halvorsen et al. (2011) found that self-image disturbances in acne patients are often more severe than what clinical evaluations reveal. Acne vulgaris can lead to suicidal ideation, mental health issues, and emotional isolation, particularly in adolescents. The risk of suicide attempts is two to three times higher in individuals with severe acne, making it a potential independent risk factor for suicidal thoughts, especially in males.
From a theoretical standpoint, psychological distress is closely linked to frequent use of immature defense mechanisms. These mechanisms involve higher levels of reality distortion and may result in maladaptive behavior, making individuals more vulnerable to mental disorders. In contrast, adaptive defenses involve lower levels of distortion and lead to healthier stress responses. Numerous psychodynamic studies have supported this hypothesis (Békés et al., 2023).
Attractiveness is a highly valued trait in many cultures, often associated with skin appearance and the absence of blemishes. Self-esteem and personal identity are critical developmental tasks for adolescents and young adults. A visible and potentially stigmatizing skin condition can lead to social rejection, interpersonal difficulties, and reduced perceived sexual or professional competence, all of which negatively impact self-perception (Magin et al., 2008). Adolescents’ perceptions of acne are often shaped by misconceptions and negative stereotypes (Marković et al., 2019).
According to Hank W. Bass, patients’ responses to acne are influenced by visibility, lesion location, sex, age, disease chronicity, childhood experiences, sensitivity to appearance, emotional difficulties, and self-confidence (Koblenzer, 2005). Adverse childhood experiences can foster a negative self-image and diminish self-worth, making individuals more susceptible to acne-related psychological challenges during adolescence and early adulthood (Koblenzer, 2005).
Research indicates that self-perception in patients with acne is a stronger predictor of psychosocial issues than the actual severity of acne (Pavaris et al., 2006). Magin et al. identified self-consciousness and embarrassment as key psychological factors among acne sufferers. These individuals often perceive themselves as targets of ridicule or judgment (Magin et al. 2006; Magin et al., 2008).
According to Young et al. (2008), schemas are deep, stable beliefs individuals form about themselves and the world, shaped by early life experiences. Schemas act as cognitive frameworks through which individuals interpret themselves and their environment (Leahy, 2013). Young et al. identified a specific category of schemas, early maladaptive schemas (EMS), which are core psychological themes driving emotional disorders (Young et al., 2008). These schemas consist of recurring memories, emotions, cognitions, and bodily sensations that guide behavior and are rooted in early developmental experiences (Bamber, 2023).
EMS are pervasive patterns originating in childhood or adolescence, often dysfunctional, and are related to one’s sense of self and relationships with others (Young, 2008). In schema therapy, particular attention is given to these dysfunctional themes, especially in patients with personality disorders and chronic psychological issues who may not respond well to traditional cognitive-behavioral approaches (Askari, 2025). Depending on the patient’s needs, schema therapy may be short-term, medium-term, or long-term. In the cognitive domain, a schema serves as a structure formed from experience and reality that helps individuals interpret their experiences (Young et al., 2008).
Schema therapy has been effective in treating persistent depression and anxiety, eating disorders, marital problems, and difficulties in maintaining close relationships. It has also been applied in criminal populations and in relapse prevention among individuals with substance use disorders (Young, 2008).
Theoretical and empirical background
EMS is correlated with various psychiatric symptoms, including somatization, obsessive-compulsive tendencies, anxiety, depression, and paranoid ideation. In particular, schemas, such as abandonment, vulnerability to harm and illness, self-sacrifice, and emotional inhibition, have been identified as significant predictors of anxiety and depression (Ahmadpanah et al., 2017).
A study by Shahmoradi demonstrated the effectiveness of schema therapy in modifying maladaptive schemas in patients with psoriasis, a chronic, recurrent inflammatory skin condition (Shahmoradi et al., 2018). In another study, Shahamat (2011) examined the predictive value of EMS on psychological symptoms such as somatization, anxiety, and depression in university students. The results indicated a significant relationship between EMS and these symptoms, with the defect/shame schema being a strong predictor of all three. Furthermore, specific schemas significantly predicted different aspects of psychological dysfunction.
Shahmoradi et al. (2018) also found that both schema therapy and mindfulness-based cognitive therapy were effective in reducing maladaptive schemas and enhancing mental health in patients with vitiligo. Vitiligo is an acquired skin disorder characterized by melanocyte loss in the epidermis, mucous membranes, and other tissues. It often presents considerable aesthetic and psychological challenges, resulting in significant psychosocial consequences. Notably, this study reported no significant difference in treatment efficacy between the two therapeutic approaches.
In another study, Hassanvand et al. (2014) investigated the predictive role of EMS in social anxiety symptoms (fear, avoidance, and physiological discomfort). The findings revealed significant correlations between EMS and all three symptoms. Specifically, the schema of social isolation/alienation significantly predicted fear, avoidance, and physiological distress. Moreover, certain schemas significantly predicted the variance in each symptom.
Alipour et al. (2013) demonstrated the efficacy of group cognitive-behavioral therapy, closely related to schema therapy, in improving the mental health of patients with psoriasis.
Coping styles refer to a set of cognitive, emotional, and behavioral patterns that individuals use to manage and reduce psychological stress. These styles can evolve over time and across various life situations, playing a vital role in mental health and personal adjustment (Askari, 2025). The use of effective problem- and emotion-focused coping strategies can reduce stress, improve psychological well-being, and enhance life satisfaction. One of the primary objectives of therapy is to assist individuals in identifying and modifying maladaptive coping styles, replacing them with more adaptive and effective styles (Maleki, 2023).
Dehesh found that schema therapy was effective in improving anger management styles (both internal and external), increasing the use of mature defense mechanisms, and reducing the use of immature and neurotic defenses among women on the verge of divorce. In another study, Arab Amiri and Khodabakhshi examined the role of EMS in coping styles and found positive correlations between EMS and maladaptive coping patterns. Their results indicated that emotional inhibition, entitlement/grandiosity, enmeshment, unrelenting standards, excessive self-criticism, and insufficient self-control were positively associated with fear of cancer recurrence (Arab Amiri & Khodabakhshi, 2021).
Furthermore, Abdolkhani (2016), in a study on cancer patients in Shiraz, found that psychological well-being could be predicted through all three categories of defense mechanisms: mature, immature, and neurotic.
Research question
Given these findings, the present study seeks to answer the following question: Is schema therapy effective in improving defense mechanisms and enhancing the mental health of individuals suffering from acne vulgaris?
Materials and Methods
This study employed a quasi-experimental design with pre-test, post-test, and control groups. The study population consisted of patients diagnosed with acne vulgaris who attended dermatology clinics in northeastern Tehran in 2024. Using purposive sampling, 28 individuals were selected and randomly assigned to two groups of 14 participants each (total: 28 individuals). The experimental group consisted of six men and eight women, while the control group included nine men and five women.
The inclusion criteria for participation included age between 15 and 25 years, completion of at least middle school education, presence of facial acne symptoms, and absence of any diagnosed physical or psychiatric disorders.
At baseline (pre-test), both groups completed the symptom checklist-90 (SCL-90) and the defense style questionnaire (DSQ-40). The experimental group then underwent 12 group schema therapy sessions over six weeks (two sessions per week). Upon completion of the intervention, the same questionnaires were administered to both groups for post-testing.
The SCL-90 is one of the most widely used diagnostic tools in psychiatry. This self-report inventory consists of 90 items that assess psychological symptoms across nine dimensions: Somatization, obsessive-compulsive symptoms, depression, anxiety, hostility, phobic anxiety, paranoid ideation, psychoticism, and interpersonal sensitivity. The instrument was originally developed by Derogatis et al. in 1973 and revised in 1976 based on clinical experience and psychometric analyses.
The defense style questionnaire-40 (DSQ-40), developed by Andrews et al. in 1993 based on revisions of earlier versions, was standardized for use in Iran by Heidari Nasab (2006). This questionnaire contains 40 items rated on a 9-point Likert scale (ranging from “strongly disagree” to “strongly agree”) and assesses 20 defense mechanisms across three main defense styles: mature, neurotic, and immature. Each of the 20 defense mechanisms is evaluated using two statements.
Mature defenses include suppression, sublimation, humor, and anticipation.
Neurotic defenses include reaction formation, idealization, rationalization, and pseudo-altruism.
Immature defenses include projection, passive hostility, acting out, displacement, denial, autistic fantasy, devaluation, somatization, splitting, omnipotence, and isolation.
Besharat et al. (2019) reported Cronbach’s α coefficients for mature, neurotic, and immature defense styles as 0.75, 0.74, and 0.73, respectively. The test re-test reliability over a two-week interval was 0.82. Heidari Nasab et al. (2007) also reported satisfactory construct validity, comparable to the original version.
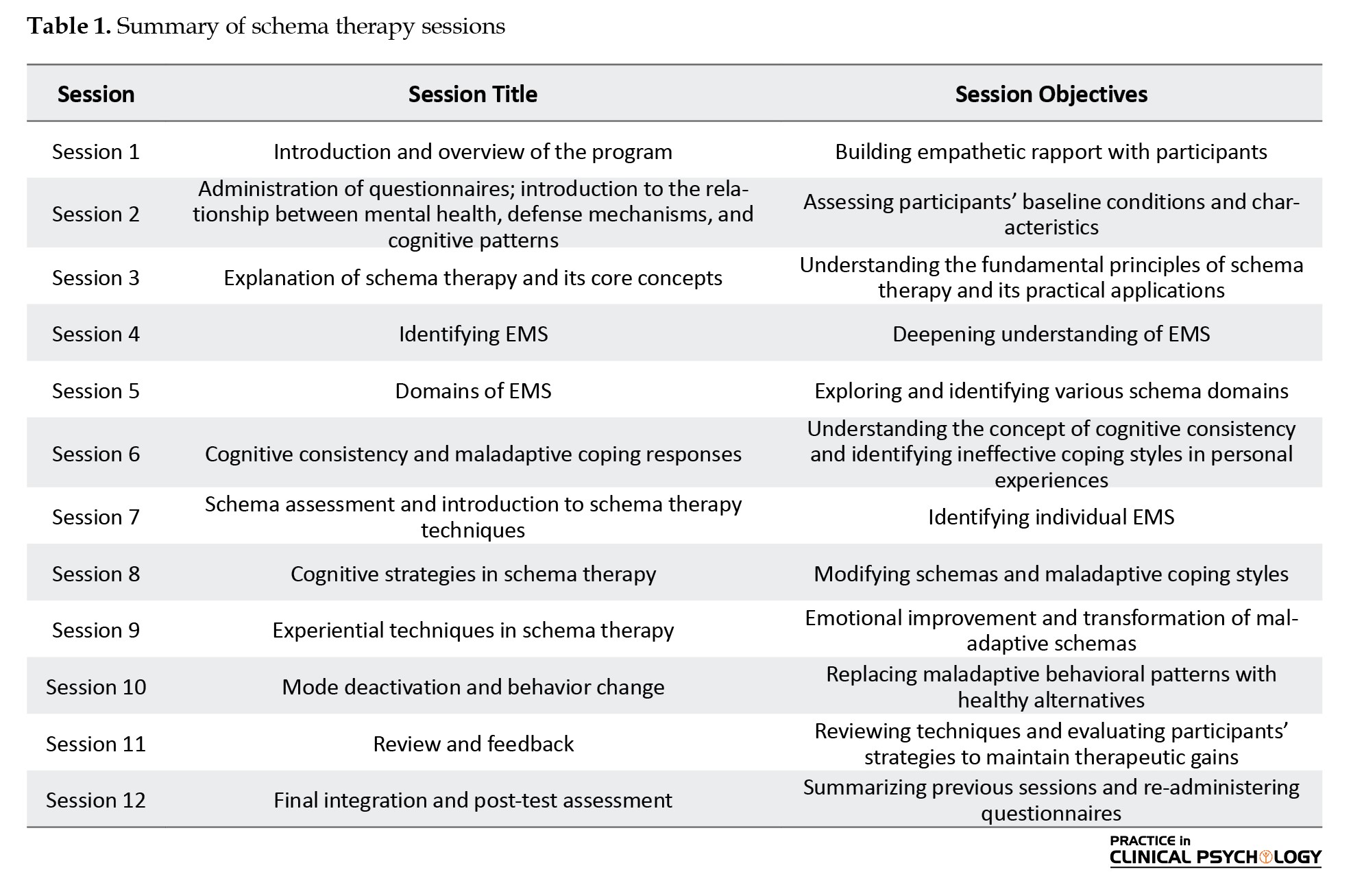
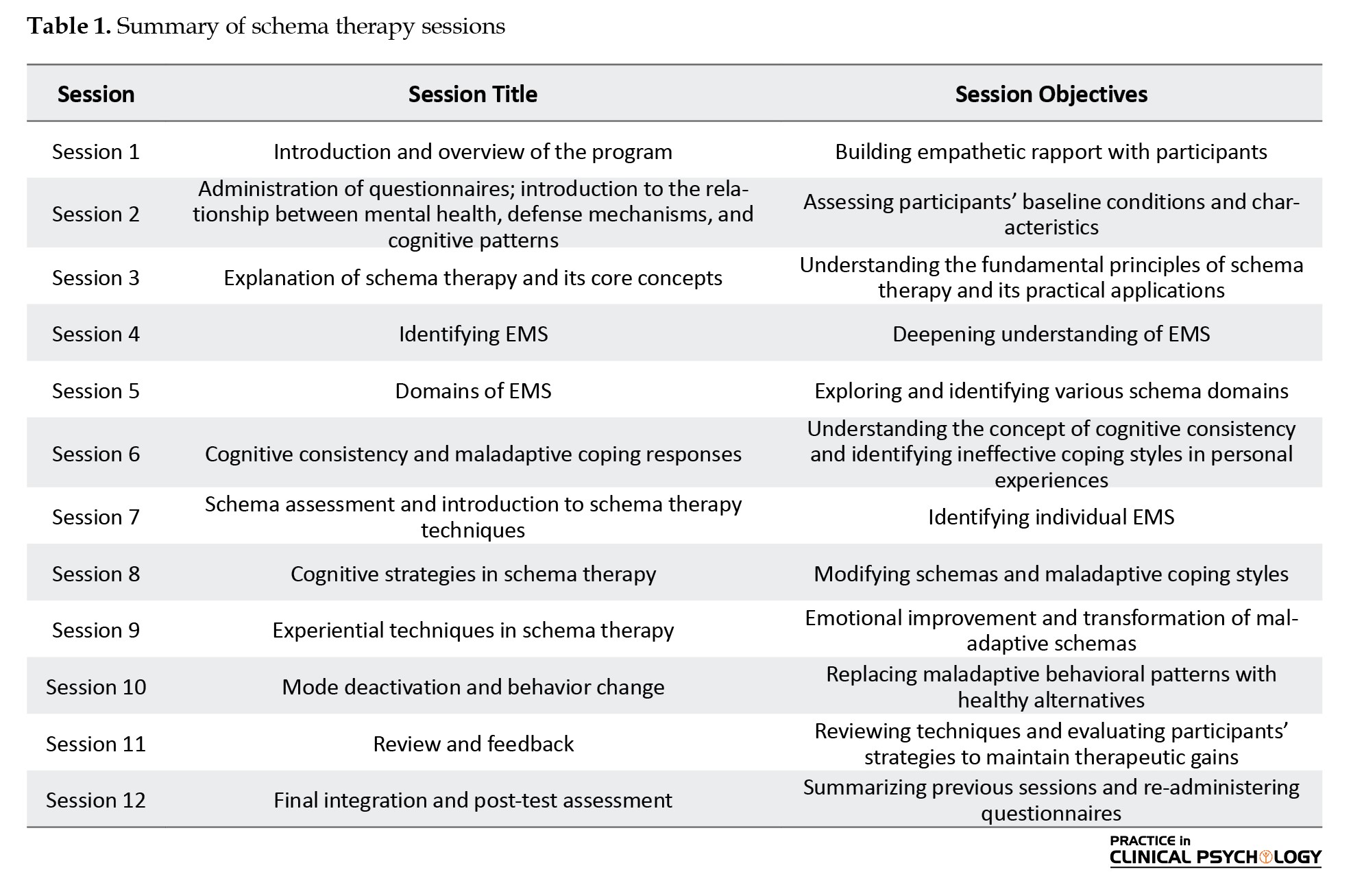
The schema therapy intervention consisted of 12 group sessions conducted over six weeks, with two one-hour sessions per week. Table 1 presents a detailed session plan (not included here).
Results
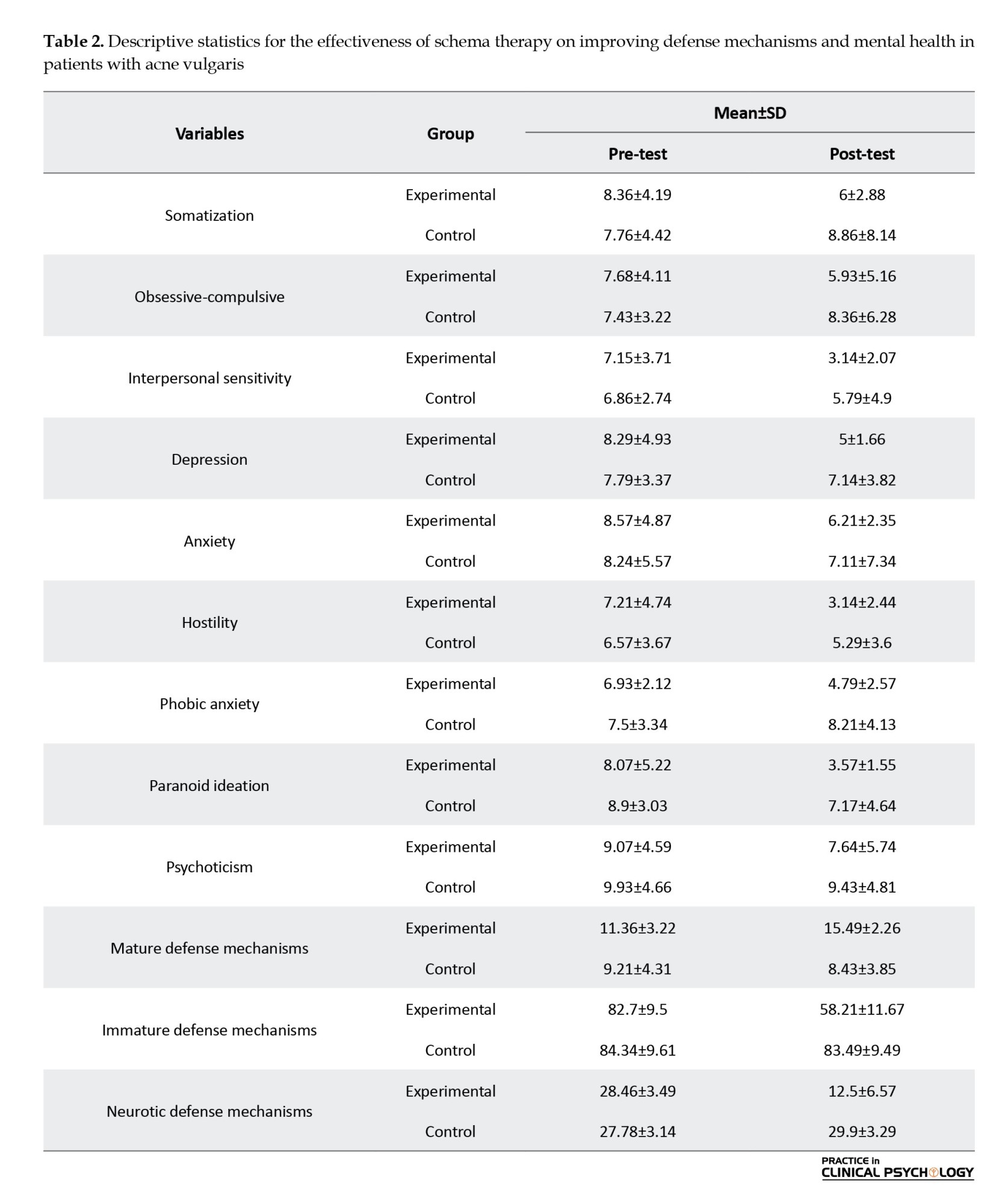
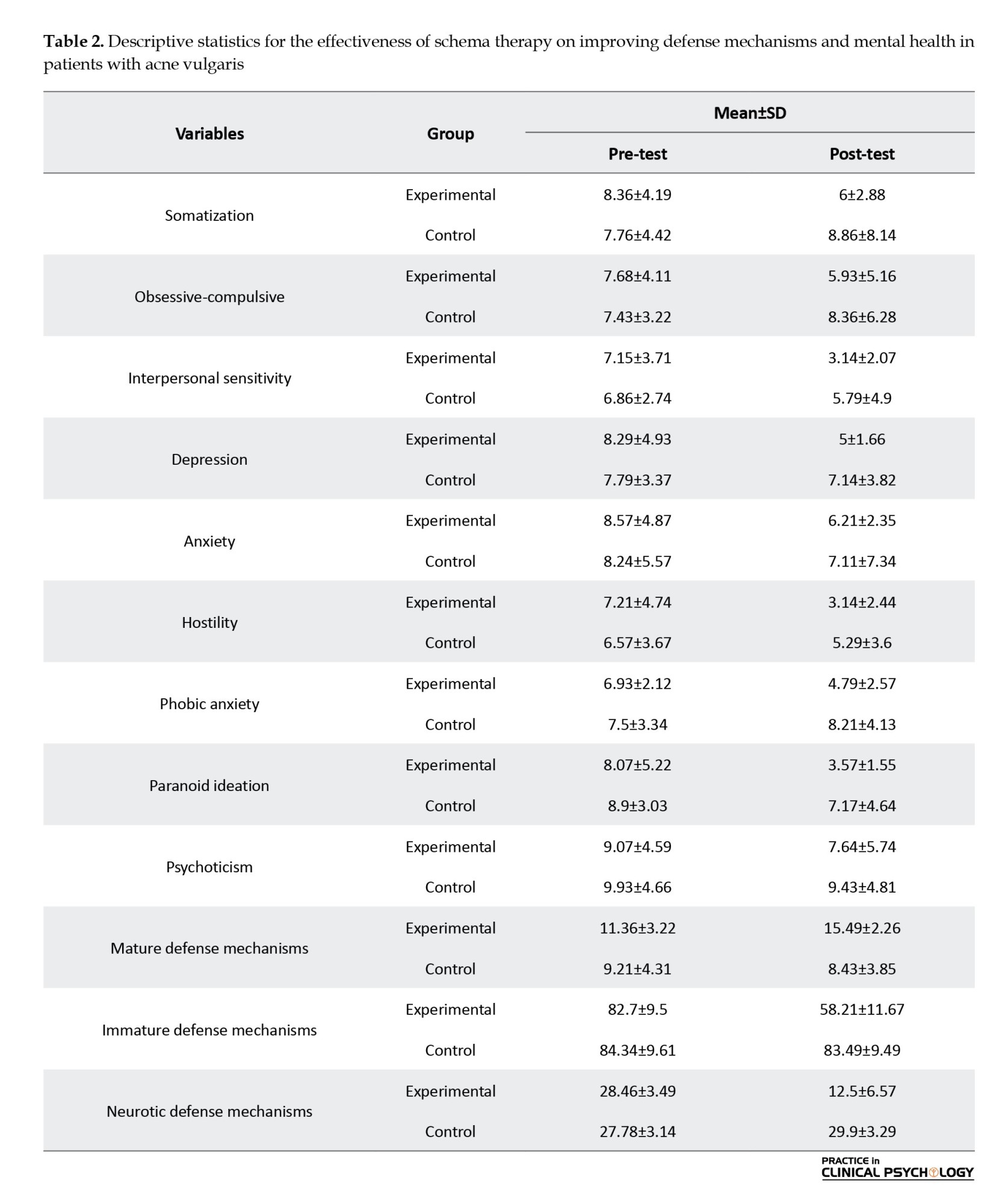
Table 2 presents the descriptive statistics for each variable, separated by experimental and control groups, for the participants.
Schema therapy protocol based on Young’s therapeutic model
Prior to conducting the covariance analysis, the necessary assumptions for using this method, including the normal distribution of scores (assessed via the Kolmogorov-Smirnov test), homogeneity of variances (assessed via Levene’s test), and homogeneity of regression slopes (assessed through covariance analysis), were evaluated and confirmed for all research variables at the 0.05 significance level.
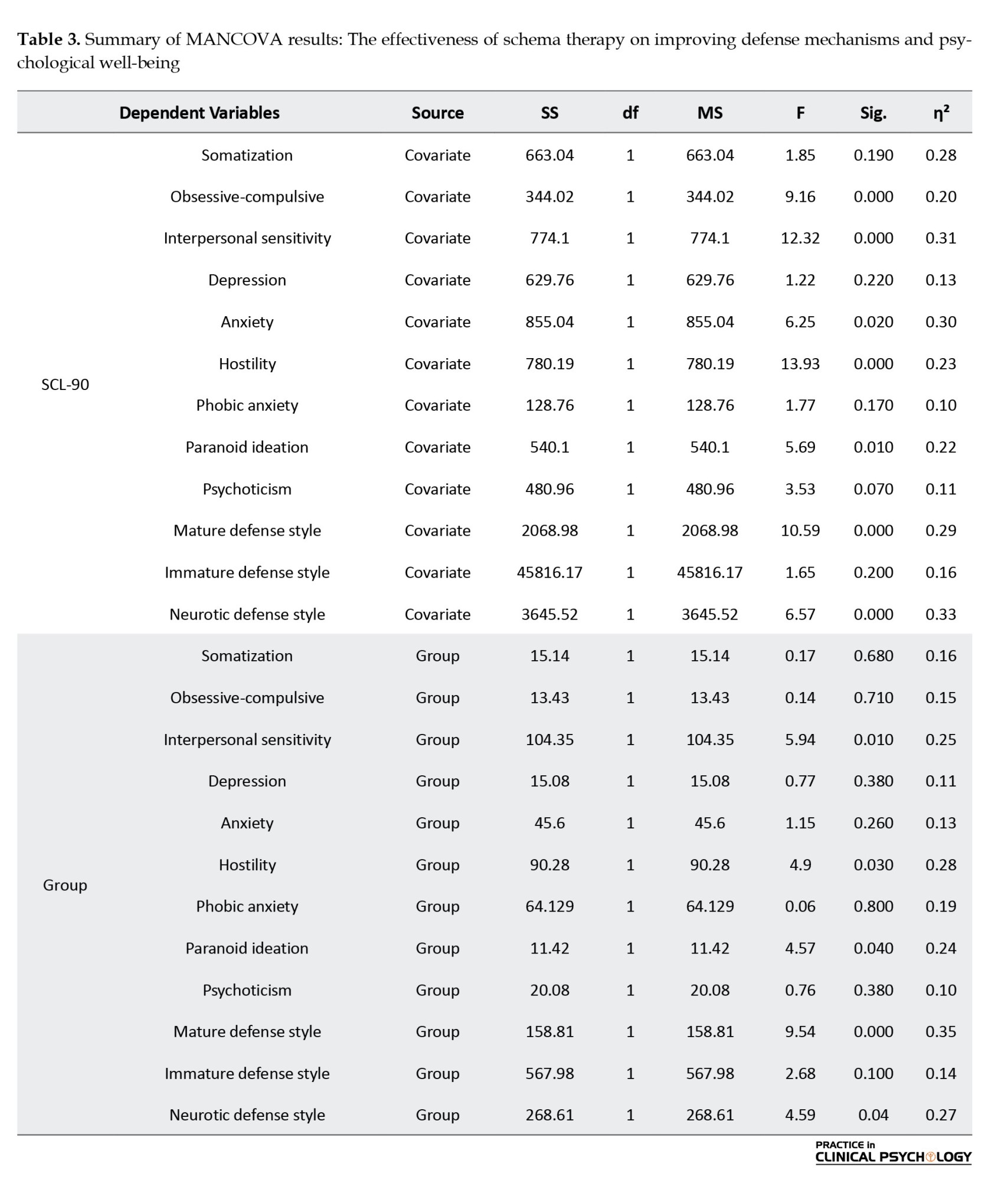
The results indicated that, after controlling for the pre-test scores (i.e. accounting for the covariate effect of the pre-test), a significant difference was observed between the experimental and control groups in terms of defense mechanisms and psychological well-being. Therefore, the effectiveness of schema therapy in improving the defensive styles and psychological health of individuals with acne was confirmed (F=4.60, P<0.001).
Table 3 presents a summary of the multivariate analysis of covariance (MANCOVA) results, analyzed at an alpha level of 0.05.
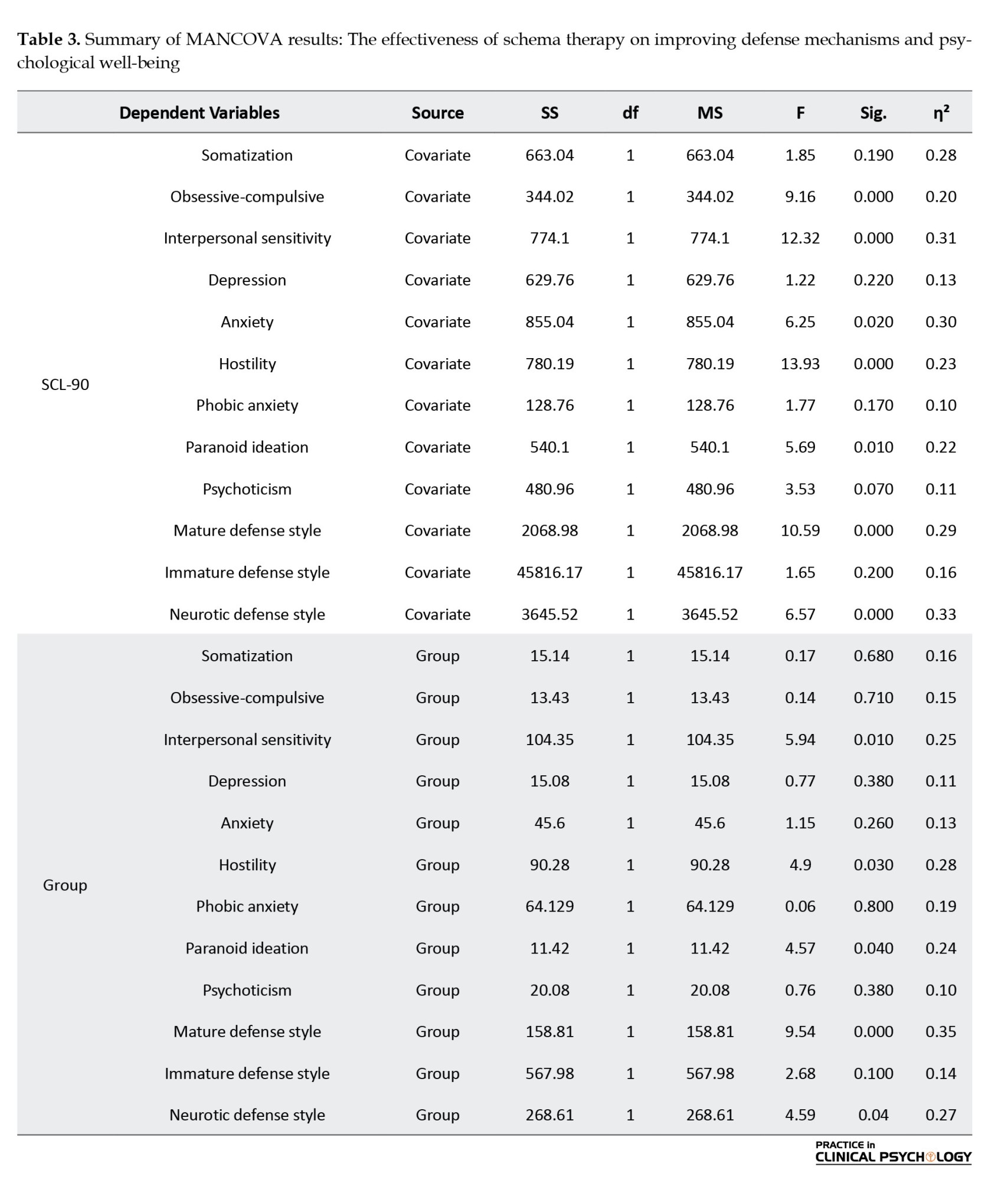
Discussion
This study aimed to investigate the effectiveness of schema therapy in improving defense mechanisms and psychological well-being among individuals with acne vulgaris. The results indicated that schema therapy can positively impact defense styles and mental health in patients suffering from this dermatological condition. Based on these findings, schema therapy had a significant effect on the subscales of interpersonal sensitivity, hostility, and paranoid ideation (as components of psychological well-being). The eta squared values revealed that schema therapy explained 25% of the variance in interpersonal sensitivity, 28% in hostility, and 24% in paranoid ideation.
According to Magin et al. (2008), psychological responses to acne are closely associated with factors such as heightened sensitivity to appearance, emotional difficulties, and self-esteem issues. Individuals with acne often perceive others as mocking or belittling them, and factors such as self-awareness and shame play a crucial role in the psychological challenges they face. These findings are consistent with those of prior studies by Shahamat (2011), Hassanvand et al. (2014), Alipour et al. (2013), Khoshnood et al. (2013), Gojani et al. (2017), and Shahmoradi et al. (2018). For example, Shahamat’s study indicated that EMS, particularly the defectiveness/shame schema, significantly predicted somatization, anxiety, and depression (Shahamat, 2011). Similarly, Hassanvand’s research demonstrated that maladaptive schemas predict avoidance and social anxiety (Hassanvand et al., 2014).
These results can be explained by the therapeutic mechanism of schema therapy, which targets EMS and dysfunctional cognitive patterns. By facilitating cognitive restructuring and replacing maladaptive beliefs with healthier alternatives, schema therapy appears to improve the emotional and affective dimensions of maladaptive schemas. This process leads to notable improvements in interpersonal sensitivity, hostility, and paranoid ideation among acne patients.
Although the current study did not find significant differences between the experimental and control groups in the subscales of somatization, depression, phobic anxiety, general anxiety, obsessive-compulsive symptoms, and psychoticism, the descriptive data (Table 2) showed noticeable reductions in post-test mean scores for these variables. The lack of statistical significance, despite meaningful mean differences, may be attributed to the short duration and compressed format of the schema therapy intervention. It seems likely that certain symptoms, particularly phobic anxiety, obsessive-compulsive traits, and psychoticism, are deeply rooted and more resistant to change, potentially requiring longer-term or more intensive schema-based interventions.
The findings also support the effectiveness of schema therapy in enhancing mature defense mechanisms and reducing neurotic defense styles in individuals with acne vulgaris. Eta squared (η²) values showed that 35% of the variance in mature defense styles and 27% of the variance in neurotic defense styles were accounted for by schema therapy. These results align with studies by Arab Amiri and Khodabakhshi (2021), Abdolkhani (2016), and Dehesh (2015). Abdolkhani’s research showed that all three defense styles (mature, immature, and neurotic) significantly predicted psychological well-being (Abdolkhani, 2016). Prior research supports the notion that the use of more mature defense mechanisms and fewer neurotic styles are positively related to better mental health. Dehesh’s study further emphasized the effectiveness of schema therapy in reducing neurotic and immature defense styles while promoting mature defenses among women on the verge of divorce (Dehesh, 2015).
Conclusion
The present study demonstrated that schema therapy is an effective psychological intervention for patients with acne vulgaris, leading to improvements in both mental health and defense mechanisms. The therapy can significantly reduce interpersonal sensitivity, hostility, and paranoid ideation while enhancing the use of mature defense mechanisms and reducing neurotic mechanisms. Although it had no significant effect on some mental symptoms, such as depression, somatization, and anxiety, the observed numerical reductions suggest that longer or more intensive interventions may further enhance outcomes. Overall, the findings highlight the importance of integrating schema therapy into psychosomatic and dermatological care, as it not only alleviates psychological distress but also promotes healthier coping strategies and a better quality of life for individuals affected by acne vulgaris.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles are considered in this article. The participants were informed of the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them. A written consent has been obtained from the subjects. principles of the Helsinki Convention was also observed.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The author declared no conflict of interest.
Acknowledgments
The author would like to thank all those who contributed to the data collection.
References
Abdolkhani, M., & Moen, L. (2016). [Relationship between defense styles and quality of life with psychological well-being of patients with cancer in Shiraz (Persian)]. Paper presented at: 4national Conference on Counseling and Mental Health, Qochan, Iran, 3 May, 2016. [Link]
Ahmadpanah, M., Astinsadaf, S., Akhondi, A., Haghighi, M., Sadeghi Bahmani, D., & Nazaribadie, M., et al. (2017). Early maladaptive schemas of emotional deprivation, social isolation, shame and abandonment are related to a history of suicide attempts among patients with major depressive disorders. Comprehensive Psychiatry, 77, 71–79. [DOI:10.1016/j.comppsych.2017.05.008] [PMID]
Alipour, A., Hossein, Z., Seyyed Naser, E., & Hassan, A. (2013). [The impact of group cognitive behavioral therapy on the disease severity and mental health of psoriasis patients (Persian)]. Journal of Dermatology and Cosmetic, 4 (4), 196-204. [Link]
Askari, A. (2015). [New concepts of schema therapy the 6 coping styles (Persian)]. Tehran: Arjmand Publishing. [Link]
Bamber, M. R. (2023). Schema Therapy for Occupational Stress [H. Hamidpour & H. Zirak, Persian trans.).Tehran: Arjomand Publications. [Link]
Behnam, B., Taheri, R., Sadat Hashemi, S. M., & Nesari-Rad Motlagh, M. (2010). [Frequency of psychopathological manifestations in psoriatic patients in Semnan city, central part of Iran (Persian)]. Journal of Fundamentals of Mental Health, 12(3), 604-611. [Link]
Besharat, M. A., Khadem, H., Zarei, V., & Motavalli Haghi, S. A. (2019). Predicting anxiety symptoms based on confrontation with existential issues: The moderating role of defense mechanisms. PCP, 7(4) :235-244. [DOI: 10.32598/jpcp.7.4.235]
Bhambri, S., Del Rosso, J. Q., & Bhambri, A. (2009). Pathogenesis of acne vulgaris: recent advances. Journal of Drugs in Dermatology : JDD, 8(7), 615–618. [PMID]
Békés, V., Starrs, C. J., Perry, J. C., Prout, T. A., Conversano, C., & Di Giuseppe, M. (2023). Defense mechanisms are associated with mental health symptoms across six countries. Research in Psychotherapy (Milano), 26(3), 729. [DOI:10.4081/ripppo.2023.729] [PMID]
Dahesh, M. (2015). [Investigating the effectiveness of schema therapy on anger management styles, defense mechanisms and determining the dominant schemas of women on the verge of divorce (Persian)] [MA thesis]. Kurdistan: University of Kurdistan. [Link]
Ding, R., He, Y., Wu, Q., & Lin, T. (2024). Quality of life in patients with acne vulgaris: An observational study. International Journal of Dermatology and Venereology, 7, E155-E182. [Link]
Dolan, P., Kavetsos, G., & Vlaev, I. (2014). The happiness workout. Social Indicators Research, 119(3), 1363-1377. [DOI:10.1007/s11205-013-0543-0]
Gallitano, S. M., & Berson, D. S. (2017). How acne bumps cause the blues: The influence of acne vulgaris on self-esteem. International Journal of Women's Dermatology, 4(1), 12–17.[DOI:10.1016/j.ijwd.2017.10.004] [PMID]
Gojani, P. J., Masjedi, M., Khaleghipour, S., & Behzadi, E. (2017). Effects of the schema therapy and mindfulness on the maladaptive schemas hold by the psoriasis patients with the psychopathology symptoms. Advanced biomedical research, 6(1), 4. [DOI:10.4103/2277-9175.190988]
Halvorsen, J. A., Stern, R. S., Dalgard, F., Thoresen, M., Bjertness, E., & Lien, L. (2011). Suicidal ideation, mental health problems, and social impairment are increased in adolescents with acne: A population-based study. Journal of Investigative Dermatology, 131(2), 363–370. [DOI:10.1038/jid.2010.264] [PMID]
Hassanvand, A. M., Hassanvand, A. A., & Ghadampour, M. (2014). [The prediction of social anxiety symptoms (fear, avoidance, physiological arousal) on the basis of early maladaptive dchemas (Persian)]. The Journal of Modern Psychological Researches, 8(32): 89-110. [Link]
Heidari Nasab, L., Mansouri, M., Azadfallah, P., & Shaieeri, M. (2007). Validity and reliability of defens style questionaire (DSQ-40) in Iranian Samples. Clinical Psychology and Personality, 5(1), 11-26.[Link]
Jain, S., Pillai, P., & Mathias, K. (2024). Opening up the 'black-box': what strategies do community mental health workers use to address the social dimensions of mental health? Social Psychiatry and Psychiatric Epidemiology, 59(3), 493–502.[DOI:10.1007/s00127-023-02582-1] [PMID]
Shahamat, F. (2011). [Predicting General Health Symptoms (Somatization, anxiety, depression) from Early Maladaptive Schemas (Persian)]. Journal of Modern Psychological Researches, 5(20), 103-124. [Link]
Shahmoradi, Z., Khaleghipour, S., & Masjedi, M. (2009). [Comparing effectiveness of “schema therapy” and “mindfulness- based cognitive therapy” on maladaptive schemas and general health in patients with Vitiligo (Persian)]. Journal of Health Promotion Management, 7 (6), 42-52. [Link]
Leahy, R. (2013). Scheme emotional therapy (H, Zirak., & R, Azadi, Persian trans). Tehran: Arjomand Publications. [Link]
Maleki, M. (2023). [Coping styles (Persian)]. Gorgan: Noroouzi Publications. [Link]
Magin, P., Adams, J., Heading, G., Pond, D., & Smith, W. (2006). Psychological sequelae of acne vulgaris: Results of a qualitative study. Canadian Family Physician Medecin de Famille Canadien, 52(8), 978–979. [PMID]
Magin, P., Adams, J., Heading, G., Pond, D., & Smith, W. (2008). Experiences of appearance-related teasing and bullying in skin diseases and their psychological sequelae: Results of a qualitative study. Scandinavian Journal of Caring Sciences, 22(3), 430–436. [DOI:10.1111/j.1471-6712.2007.00547.x] [PMID]
Markovic, M., Soldatovic, I., Bjekic, M., & Sipetic-Grujicic, S. (2019). Adolescents' self perceived acne-related beliefs: from myth to science. Anais Brasileiros de Dermatologia, 94(6), 684–690. [DOI:10.1016/j.abd.2019.02.005] [PMID]
Misery L. (2011). Consequences of psychological distress in adolescents with acne. The Journal of investigative dermatology, 131(2), 290–292. [DOI: 10.1038/jid.2010.375] [PMID]
Nie, P., Zhao, K., Ma, D., Liu, H., Amin, S., & Yasin, I. (2024). Global climate change, mental health, and socio-economic stressors: Toward Sustainable Interventions across Regions. Sustainability, 16(19), 8693. [DOI:10.3390/su16198693]
Picardi, A., Mazzotti, E., & Pasquini, P. (2006). Prevalence and correlates of suicidal ideation among patients with skin disease. Journal of the American Academy of Dermatology, 54(3), 420–426. [DOI:10.1016/j.jaad.2005.11.1103] [PMID]
Sutaria, A. H., Masood, S., Saleh, H. M., & Schlessinger, J. (2023). Acne Vulgaris. In StatPearls. StatPearls Publishing. [PMID]
Williams, H. C., Dellavalle, R. P., & Garner, S. (2012). Acne vulgaris. Lancet (London, England), 379(9813), 361–372. [DOI:10.1016/S0140-6736(11)60321-8] [PMID]
Young, J. E., Klosko, J. S., & Weishaar, M. E (2008). Schema therapy: A practitioner”s guide. New York: Guilford Press. [Link]
Zouboulis, C. C., & Böhm, M. (2004). Neuroendocrine regulation of sebocytes -- a pathogenetic link between stress and acne. Experimental Dermatology, 13 (Suppl 4), 31–35. [DOI:10.1111/j.1600-0625.2004.00254.x] [PMID]
Zouboulis, C. C., Eady, A., Philpott, M., Goldsmith, L. A., Orfanos, C., Cunliffe, W. C., & Rosenfield, R. (2005). What is the pathogenesis of acne? Experimental Dermatology, 14(2), 143–152. [DOI:10.1111/j.0906-6705.2005.0285a.x] [PMID]
Acne vulgaris, commonly referred to as “teenage acne,” is a chronic inflammatory skin disease classified as a psychosomatic disorder. It affects approximately 9.4% of the global population (Ding et al., 2024). As the third most prevalent dermatological condition worldwide, it primarily manifests during adolescence and early adulthood, particularly in the second and third decades of life. The prevalence of this skin condition is estimated to be approximately 80%–85% (Marković et al., 2019).
Acne results from the clogging of skin pores due to excess oil (sebum) and dead skin cells. It can appear on the face, neck, chest, back, or shoulders, which are areas rich in sebaceous (oil) glands (Bhambri & Del Rosso, 2009). Research indicates that facial acne is significantly more common than acne on other body regions. The prevalence rates are reported to be 91% for facial acne, 54% for back acne, and 36% for chest acne. Approximately 20% of individuals experience severe acne, which can lead to permanent scarring (Sutaria & Schlessinger, 2020).
The clinical presentation of acne varies and includes papules (small red bumps), pustules (pus-filled lesions), cysts (painful pus-filled lumps beneath the skin), nodules (large painful lumps under the skin), whiteheads (closed clogged pores), and blackheads (open clogged pores where the sebum oxidizes upon exposure to air and darkens) (Ding et al., 2024).
The four primary physical causes of acne are as follows: (1) sebum overproduction, (2) accumulation of dead skin cells, (3) clogged hair follicles, and (4) bacterial infection. Hair follicles are connected to sebaceous glands that secrete sebum to lubricate the skin and hair. When excessive sebum and dead cells accumulate, they form a soft plug that creates an ideal environment for bacterial growth. Infected clogged pores trigger skin inflammation. If the clogged pore remains closed, it forms a whitehead; if open, a blackhead forms. Red pimples with white centers result from inflamed or infected follicles, while deeper blockages may develop into cysts (William & Delavar, 2012).
Psychosomatic skin disorders, such as nail biting, trichotillomania, psychogenic pruritus, dermatitis, urticaria, burning sensations, and exaggerated pain responses, are common conditions encountered by dermatologists (Bhambri & Del Rosso, 2009). Halvorsen et al. (2011) found that psychological stress plays a significant role in the development of acne, often arising from daily life events or as a consequence of having acne itself.
Stress contributes to the physiological processes of acne through biochemical pathways. Sebaceous glands have specific receptors for stress-related hormones, including corticotropin-releasing hormone, melanocortins, neuropeptide Y, and beta-endorphins. When these hormones bind to their receptors, they trigger the release of pro-inflammatory cytokines, stimulating sebaceous glands and exacerbating acne (Zouboulis et al., 2005; Zoulis & Bomm, 2004; Magin et al., 2008). Under stress, the production of corticosteroids and adrenal androgens increases, worsening acne symptoms.
The psychological impact of acne is profound. Many individuals, especially adolescents, experience heightened anxiety, depression, and diminished self-esteem. Acne can also interfere with the formation of one’s identity and personal development. These mental health challenges are often intensified by the social stigma associated with visible skin conditions (Ding et al., 2024).
Mental health and acne: Theoretical foundations and the role of schema therapy
The American Psychological Association (APA) defines mental health as a state in which individuals can cope appropriately with life challenges and utilize their emotional and psychological capacities to enhance their quality of life (QoL) and achieve success. According to the National Institute of Mental Health (NIMH), mental health involves a balance of cognitive, emotional, and behavioral functioning, enabling individuals to learn, manage stress, establish relationships, and adapt effectively to changes. The World Health Organization (WHO) describes mental health as a state in which an individual recognizes their own abilities, can cope with normal life stressors, work productively, and contribute to their community (Jain et al., 2024).
Although individuals live in objective (external) environments, they respond to events based on their subjective (internal) perceptions. Therefore, mental health is considered a key indicator of QoL (Dolan & Cautesous, 2014). It encompasses emotional responses to life events, psychological states, and judgments about satisfaction in areas such as marriage, work, and personal development (Nie et al., 2024).
Acne can inflict invisible psychological harm, significantly undermining self-esteem, particularly among women. Despite its psychological consequences, only a minority of acne sufferers seek psychological treatment (Galatino & Berson, 2018). Given the psychological underpinnings and the role of emotional conflict in such disorders, solely physiological treatments are often insufficient, highlighting the need for psychological interventions. This has led dermatologists and mental health professionals to collaborate on psychosomatic dermatology research and treatment (Behnam et al., 2010).
Dermatological lesions of acne, especially facial acne, which is the most prevalent, not only cause physical discomfort but also have negative psychosocial impacts on interpersonal interactions. Since acne often begins in adolescence, a period marked by heightened sensitivity to physical appearance, its presence can result in deeper psychological damage (Ding et al., 2024). This may initiate a psychosomatic cycle, where stress and emotional disturbances exacerbate acne symptoms and lead to chronic conditions, eventually contributing to the emergence of mental disorders, such as anxiety and depression. This, in turn, reinforces the cycle of psychosomatic dysfunction. Studies have shown that anxiety and stress delay wound healing by approximately 40% and are recognized as key factors in prolonging acne symptoms (Halvorsen, 2011).
Psychodermatological patients often present with comorbid conditions, including obsessive-compulsive personality disorder, body dysmorphic disorder, obsessive thoughts related to oily skin, eating disorders, substance abuse, trichotillomania, and borderline personality disorder (Picardi et al., 2006). Acne may trigger psychological distress and is frequently associated with psychiatric disorders (Misery, 2011). Halvorsen et al. (2011) found that self-image disturbances in acne patients are often more severe than what clinical evaluations reveal. Acne vulgaris can lead to suicidal ideation, mental health issues, and emotional isolation, particularly in adolescents. The risk of suicide attempts is two to three times higher in individuals with severe acne, making it a potential independent risk factor for suicidal thoughts, especially in males.
From a theoretical standpoint, psychological distress is closely linked to frequent use of immature defense mechanisms. These mechanisms involve higher levels of reality distortion and may result in maladaptive behavior, making individuals more vulnerable to mental disorders. In contrast, adaptive defenses involve lower levels of distortion and lead to healthier stress responses. Numerous psychodynamic studies have supported this hypothesis (Békés et al., 2023).
Attractiveness is a highly valued trait in many cultures, often associated with skin appearance and the absence of blemishes. Self-esteem and personal identity are critical developmental tasks for adolescents and young adults. A visible and potentially stigmatizing skin condition can lead to social rejection, interpersonal difficulties, and reduced perceived sexual or professional competence, all of which negatively impact self-perception (Magin et al., 2008). Adolescents’ perceptions of acne are often shaped by misconceptions and negative stereotypes (Marković et al., 2019).
According to Hank W. Bass, patients’ responses to acne are influenced by visibility, lesion location, sex, age, disease chronicity, childhood experiences, sensitivity to appearance, emotional difficulties, and self-confidence (Koblenzer, 2005). Adverse childhood experiences can foster a negative self-image and diminish self-worth, making individuals more susceptible to acne-related psychological challenges during adolescence and early adulthood (Koblenzer, 2005).
Research indicates that self-perception in patients with acne is a stronger predictor of psychosocial issues than the actual severity of acne (Pavaris et al., 2006). Magin et al. identified self-consciousness and embarrassment as key psychological factors among acne sufferers. These individuals often perceive themselves as targets of ridicule or judgment (Magin et al. 2006; Magin et al., 2008).
According to Young et al. (2008), schemas are deep, stable beliefs individuals form about themselves and the world, shaped by early life experiences. Schemas act as cognitive frameworks through which individuals interpret themselves and their environment (Leahy, 2013). Young et al. identified a specific category of schemas, early maladaptive schemas (EMS), which are core psychological themes driving emotional disorders (Young et al., 2008). These schemas consist of recurring memories, emotions, cognitions, and bodily sensations that guide behavior and are rooted in early developmental experiences (Bamber, 2023).
EMS are pervasive patterns originating in childhood or adolescence, often dysfunctional, and are related to one’s sense of self and relationships with others (Young, 2008). In schema therapy, particular attention is given to these dysfunctional themes, especially in patients with personality disorders and chronic psychological issues who may not respond well to traditional cognitive-behavioral approaches (Askari, 2025). Depending on the patient’s needs, schema therapy may be short-term, medium-term, or long-term. In the cognitive domain, a schema serves as a structure formed from experience and reality that helps individuals interpret their experiences (Young et al., 2008).
Schema therapy has been effective in treating persistent depression and anxiety, eating disorders, marital problems, and difficulties in maintaining close relationships. It has also been applied in criminal populations and in relapse prevention among individuals with substance use disorders (Young, 2008).
Theoretical and empirical background
EMS is correlated with various psychiatric symptoms, including somatization, obsessive-compulsive tendencies, anxiety, depression, and paranoid ideation. In particular, schemas, such as abandonment, vulnerability to harm and illness, self-sacrifice, and emotional inhibition, have been identified as significant predictors of anxiety and depression (Ahmadpanah et al., 2017).
A study by Shahmoradi demonstrated the effectiveness of schema therapy in modifying maladaptive schemas in patients with psoriasis, a chronic, recurrent inflammatory skin condition (Shahmoradi et al., 2018). In another study, Shahamat (2011) examined the predictive value of EMS on psychological symptoms such as somatization, anxiety, and depression in university students. The results indicated a significant relationship between EMS and these symptoms, with the defect/shame schema being a strong predictor of all three. Furthermore, specific schemas significantly predicted different aspects of psychological dysfunction.
Shahmoradi et al. (2018) also found that both schema therapy and mindfulness-based cognitive therapy were effective in reducing maladaptive schemas and enhancing mental health in patients with vitiligo. Vitiligo is an acquired skin disorder characterized by melanocyte loss in the epidermis, mucous membranes, and other tissues. It often presents considerable aesthetic and psychological challenges, resulting in significant psychosocial consequences. Notably, this study reported no significant difference in treatment efficacy between the two therapeutic approaches.
In another study, Hassanvand et al. (2014) investigated the predictive role of EMS in social anxiety symptoms (fear, avoidance, and physiological discomfort). The findings revealed significant correlations between EMS and all three symptoms. Specifically, the schema of social isolation/alienation significantly predicted fear, avoidance, and physiological distress. Moreover, certain schemas significantly predicted the variance in each symptom.
Alipour et al. (2013) demonstrated the efficacy of group cognitive-behavioral therapy, closely related to schema therapy, in improving the mental health of patients with psoriasis.
Coping styles refer to a set of cognitive, emotional, and behavioral patterns that individuals use to manage and reduce psychological stress. These styles can evolve over time and across various life situations, playing a vital role in mental health and personal adjustment (Askari, 2025). The use of effective problem- and emotion-focused coping strategies can reduce stress, improve psychological well-being, and enhance life satisfaction. One of the primary objectives of therapy is to assist individuals in identifying and modifying maladaptive coping styles, replacing them with more adaptive and effective styles (Maleki, 2023).
Dehesh found that schema therapy was effective in improving anger management styles (both internal and external), increasing the use of mature defense mechanisms, and reducing the use of immature and neurotic defenses among women on the verge of divorce. In another study, Arab Amiri and Khodabakhshi examined the role of EMS in coping styles and found positive correlations between EMS and maladaptive coping patterns. Their results indicated that emotional inhibition, entitlement/grandiosity, enmeshment, unrelenting standards, excessive self-criticism, and insufficient self-control were positively associated with fear of cancer recurrence (Arab Amiri & Khodabakhshi, 2021).
Furthermore, Abdolkhani (2016), in a study on cancer patients in Shiraz, found that psychological well-being could be predicted through all three categories of defense mechanisms: mature, immature, and neurotic.
Research question
Given these findings, the present study seeks to answer the following question: Is schema therapy effective in improving defense mechanisms and enhancing the mental health of individuals suffering from acne vulgaris?
Materials and Methods
This study employed a quasi-experimental design with pre-test, post-test, and control groups. The study population consisted of patients diagnosed with acne vulgaris who attended dermatology clinics in northeastern Tehran in 2024. Using purposive sampling, 28 individuals were selected and randomly assigned to two groups of 14 participants each (total: 28 individuals). The experimental group consisted of six men and eight women, while the control group included nine men and five women.
The inclusion criteria for participation included age between 15 and 25 years, completion of at least middle school education, presence of facial acne symptoms, and absence of any diagnosed physical or psychiatric disorders.
At baseline (pre-test), both groups completed the symptom checklist-90 (SCL-90) and the defense style questionnaire (DSQ-40). The experimental group then underwent 12 group schema therapy sessions over six weeks (two sessions per week). Upon completion of the intervention, the same questionnaires were administered to both groups for post-testing.
The SCL-90 is one of the most widely used diagnostic tools in psychiatry. This self-report inventory consists of 90 items that assess psychological symptoms across nine dimensions: Somatization, obsessive-compulsive symptoms, depression, anxiety, hostility, phobic anxiety, paranoid ideation, psychoticism, and interpersonal sensitivity. The instrument was originally developed by Derogatis et al. in 1973 and revised in 1976 based on clinical experience and psychometric analyses.
The defense style questionnaire-40 (DSQ-40), developed by Andrews et al. in 1993 based on revisions of earlier versions, was standardized for use in Iran by Heidari Nasab (2006). This questionnaire contains 40 items rated on a 9-point Likert scale (ranging from “strongly disagree” to “strongly agree”) and assesses 20 defense mechanisms across three main defense styles: mature, neurotic, and immature. Each of the 20 defense mechanisms is evaluated using two statements.
Mature defenses include suppression, sublimation, humor, and anticipation.
Neurotic defenses include reaction formation, idealization, rationalization, and pseudo-altruism.
Immature defenses include projection, passive hostility, acting out, displacement, denial, autistic fantasy, devaluation, somatization, splitting, omnipotence, and isolation.
Besharat et al. (2019) reported Cronbach’s α coefficients for mature, neurotic, and immature defense styles as 0.75, 0.74, and 0.73, respectively. The test re-test reliability over a two-week interval was 0.82. Heidari Nasab et al. (2007) also reported satisfactory construct validity, comparable to the original version.
The schema therapy intervention consisted of 12 group sessions conducted over six weeks, with two one-hour sessions per week. Table 1 presents a detailed session plan (not included here).
Results
Table 2 presents the descriptive statistics for each variable, separated by experimental and control groups, for the participants.
Schema therapy protocol based on Young’s therapeutic model
Prior to conducting the covariance analysis, the necessary assumptions for using this method, including the normal distribution of scores (assessed via the Kolmogorov-Smirnov test), homogeneity of variances (assessed via Levene’s test), and homogeneity of regression slopes (assessed through covariance analysis), were evaluated and confirmed for all research variables at the 0.05 significance level.
The results indicated that, after controlling for the pre-test scores (i.e. accounting for the covariate effect of the pre-test), a significant difference was observed between the experimental and control groups in terms of defense mechanisms and psychological well-being. Therefore, the effectiveness of schema therapy in improving the defensive styles and psychological health of individuals with acne was confirmed (F=4.60, P<0.001).
Table 3 presents a summary of the multivariate analysis of covariance (MANCOVA) results, analyzed at an alpha level of 0.05.
Discussion
This study aimed to investigate the effectiveness of schema therapy in improving defense mechanisms and psychological well-being among individuals with acne vulgaris. The results indicated that schema therapy can positively impact defense styles and mental health in patients suffering from this dermatological condition. Based on these findings, schema therapy had a significant effect on the subscales of interpersonal sensitivity, hostility, and paranoid ideation (as components of psychological well-being). The eta squared values revealed that schema therapy explained 25% of the variance in interpersonal sensitivity, 28% in hostility, and 24% in paranoid ideation.
According to Magin et al. (2008), psychological responses to acne are closely associated with factors such as heightened sensitivity to appearance, emotional difficulties, and self-esteem issues. Individuals with acne often perceive others as mocking or belittling them, and factors such as self-awareness and shame play a crucial role in the psychological challenges they face. These findings are consistent with those of prior studies by Shahamat (2011), Hassanvand et al. (2014), Alipour et al. (2013), Khoshnood et al. (2013), Gojani et al. (2017), and Shahmoradi et al. (2018). For example, Shahamat’s study indicated that EMS, particularly the defectiveness/shame schema, significantly predicted somatization, anxiety, and depression (Shahamat, 2011). Similarly, Hassanvand’s research demonstrated that maladaptive schemas predict avoidance and social anxiety (Hassanvand et al., 2014).
These results can be explained by the therapeutic mechanism of schema therapy, which targets EMS and dysfunctional cognitive patterns. By facilitating cognitive restructuring and replacing maladaptive beliefs with healthier alternatives, schema therapy appears to improve the emotional and affective dimensions of maladaptive schemas. This process leads to notable improvements in interpersonal sensitivity, hostility, and paranoid ideation among acne patients.
Although the current study did not find significant differences between the experimental and control groups in the subscales of somatization, depression, phobic anxiety, general anxiety, obsessive-compulsive symptoms, and psychoticism, the descriptive data (Table 2) showed noticeable reductions in post-test mean scores for these variables. The lack of statistical significance, despite meaningful mean differences, may be attributed to the short duration and compressed format of the schema therapy intervention. It seems likely that certain symptoms, particularly phobic anxiety, obsessive-compulsive traits, and psychoticism, are deeply rooted and more resistant to change, potentially requiring longer-term or more intensive schema-based interventions.
The findings also support the effectiveness of schema therapy in enhancing mature defense mechanisms and reducing neurotic defense styles in individuals with acne vulgaris. Eta squared (η²) values showed that 35% of the variance in mature defense styles and 27% of the variance in neurotic defense styles were accounted for by schema therapy. These results align with studies by Arab Amiri and Khodabakhshi (2021), Abdolkhani (2016), and Dehesh (2015). Abdolkhani’s research showed that all three defense styles (mature, immature, and neurotic) significantly predicted psychological well-being (Abdolkhani, 2016). Prior research supports the notion that the use of more mature defense mechanisms and fewer neurotic styles are positively related to better mental health. Dehesh’s study further emphasized the effectiveness of schema therapy in reducing neurotic and immature defense styles while promoting mature defenses among women on the verge of divorce (Dehesh, 2015).
Conclusion
The present study demonstrated that schema therapy is an effective psychological intervention for patients with acne vulgaris, leading to improvements in both mental health and defense mechanisms. The therapy can significantly reduce interpersonal sensitivity, hostility, and paranoid ideation while enhancing the use of mature defense mechanisms and reducing neurotic mechanisms. Although it had no significant effect on some mental symptoms, such as depression, somatization, and anxiety, the observed numerical reductions suggest that longer or more intensive interventions may further enhance outcomes. Overall, the findings highlight the importance of integrating schema therapy into psychosomatic and dermatological care, as it not only alleviates psychological distress but also promotes healthier coping strategies and a better quality of life for individuals affected by acne vulgaris.
Ethical Considerations
Compliance with ethical guidelines
All ethical principles are considered in this article. The participants were informed of the purpose of the research and its implementation stages. They were also assured about the confidentiality of their information and were free to leave the study whenever they wished, and if desired, the research results would be available to them. A written consent has been obtained from the subjects. principles of the Helsinki Convention was also observed.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The author declared no conflict of interest.
Acknowledgments
The author would like to thank all those who contributed to the data collection.
References
Abdolkhani, M., & Moen, L. (2016). [Relationship between defense styles and quality of life with psychological well-being of patients with cancer in Shiraz (Persian)]. Paper presented at: 4national Conference on Counseling and Mental Health, Qochan, Iran, 3 May, 2016. [Link]
Ahmadpanah, M., Astinsadaf, S., Akhondi, A., Haghighi, M., Sadeghi Bahmani, D., & Nazaribadie, M., et al. (2017). Early maladaptive schemas of emotional deprivation, social isolation, shame and abandonment are related to a history of suicide attempts among patients with major depressive disorders. Comprehensive Psychiatry, 77, 71–79. [DOI:10.1016/j.comppsych.2017.05.008] [PMID]
Alipour, A., Hossein, Z., Seyyed Naser, E., & Hassan, A. (2013). [The impact of group cognitive behavioral therapy on the disease severity and mental health of psoriasis patients (Persian)]. Journal of Dermatology and Cosmetic, 4 (4), 196-204. [Link]
Askari, A. (2015). [New concepts of schema therapy the 6 coping styles (Persian)]. Tehran: Arjmand Publishing. [Link]
Bamber, M. R. (2023). Schema Therapy for Occupational Stress [H. Hamidpour & H. Zirak, Persian trans.).Tehran: Arjomand Publications. [Link]
Behnam, B., Taheri, R., Sadat Hashemi, S. M., & Nesari-Rad Motlagh, M. (2010). [Frequency of psychopathological manifestations in psoriatic patients in Semnan city, central part of Iran (Persian)]. Journal of Fundamentals of Mental Health, 12(3), 604-611. [Link]
Besharat, M. A., Khadem, H., Zarei, V., & Motavalli Haghi, S. A. (2019). Predicting anxiety symptoms based on confrontation with existential issues: The moderating role of defense mechanisms. PCP, 7(4) :235-244. [DOI: 10.32598/jpcp.7.4.235]
Bhambri, S., Del Rosso, J. Q., & Bhambri, A. (2009). Pathogenesis of acne vulgaris: recent advances. Journal of Drugs in Dermatology : JDD, 8(7), 615–618. [PMID]
Békés, V., Starrs, C. J., Perry, J. C., Prout, T. A., Conversano, C., & Di Giuseppe, M. (2023). Defense mechanisms are associated with mental health symptoms across six countries. Research in Psychotherapy (Milano), 26(3), 729. [DOI:10.4081/ripppo.2023.729] [PMID]
Dahesh, M. (2015). [Investigating the effectiveness of schema therapy on anger management styles, defense mechanisms and determining the dominant schemas of women on the verge of divorce (Persian)] [MA thesis]. Kurdistan: University of Kurdistan. [Link]
Ding, R., He, Y., Wu, Q., & Lin, T. (2024). Quality of life in patients with acne vulgaris: An observational study. International Journal of Dermatology and Venereology, 7, E155-E182. [Link]
Dolan, P., Kavetsos, G., & Vlaev, I. (2014). The happiness workout. Social Indicators Research, 119(3), 1363-1377. [DOI:10.1007/s11205-013-0543-0]
Gallitano, S. M., & Berson, D. S. (2017). How acne bumps cause the blues: The influence of acne vulgaris on self-esteem. International Journal of Women's Dermatology, 4(1), 12–17.[DOI:10.1016/j.ijwd.2017.10.004] [PMID]
Gojani, P. J., Masjedi, M., Khaleghipour, S., & Behzadi, E. (2017). Effects of the schema therapy and mindfulness on the maladaptive schemas hold by the psoriasis patients with the psychopathology symptoms. Advanced biomedical research, 6(1), 4. [DOI:10.4103/2277-9175.190988]
Halvorsen, J. A., Stern, R. S., Dalgard, F., Thoresen, M., Bjertness, E., & Lien, L. (2011). Suicidal ideation, mental health problems, and social impairment are increased in adolescents with acne: A population-based study. Journal of Investigative Dermatology, 131(2), 363–370. [DOI:10.1038/jid.2010.264] [PMID]
Hassanvand, A. M., Hassanvand, A. A., & Ghadampour, M. (2014). [The prediction of social anxiety symptoms (fear, avoidance, physiological arousal) on the basis of early maladaptive dchemas (Persian)]. The Journal of Modern Psychological Researches, 8(32): 89-110. [Link]
Heidari Nasab, L., Mansouri, M., Azadfallah, P., & Shaieeri, M. (2007). Validity and reliability of defens style questionaire (DSQ-40) in Iranian Samples. Clinical Psychology and Personality, 5(1), 11-26.[Link]
Jain, S., Pillai, P., & Mathias, K. (2024). Opening up the 'black-box': what strategies do community mental health workers use to address the social dimensions of mental health? Social Psychiatry and Psychiatric Epidemiology, 59(3), 493–502.[DOI:10.1007/s00127-023-02582-1] [PMID]
Shahamat, F. (2011). [Predicting General Health Symptoms (Somatization, anxiety, depression) from Early Maladaptive Schemas (Persian)]. Journal of Modern Psychological Researches, 5(20), 103-124. [Link]
Shahmoradi, Z., Khaleghipour, S., & Masjedi, M. (2009). [Comparing effectiveness of “schema therapy” and “mindfulness- based cognitive therapy” on maladaptive schemas and general health in patients with Vitiligo (Persian)]. Journal of Health Promotion Management, 7 (6), 42-52. [Link]
Leahy, R. (2013). Scheme emotional therapy (H, Zirak., & R, Azadi, Persian trans). Tehran: Arjomand Publications. [Link]
Maleki, M. (2023). [Coping styles (Persian)]. Gorgan: Noroouzi Publications. [Link]
Magin, P., Adams, J., Heading, G., Pond, D., & Smith, W. (2006). Psychological sequelae of acne vulgaris: Results of a qualitative study. Canadian Family Physician Medecin de Famille Canadien, 52(8), 978–979. [PMID]
Magin, P., Adams, J., Heading, G., Pond, D., & Smith, W. (2008). Experiences of appearance-related teasing and bullying in skin diseases and their psychological sequelae: Results of a qualitative study. Scandinavian Journal of Caring Sciences, 22(3), 430–436. [DOI:10.1111/j.1471-6712.2007.00547.x] [PMID]
Markovic, M., Soldatovic, I., Bjekic, M., & Sipetic-Grujicic, S. (2019). Adolescents' self perceived acne-related beliefs: from myth to science. Anais Brasileiros de Dermatologia, 94(6), 684–690. [DOI:10.1016/j.abd.2019.02.005] [PMID]
Misery L. (2011). Consequences of psychological distress in adolescents with acne. The Journal of investigative dermatology, 131(2), 290–292. [DOI: 10.1038/jid.2010.375] [PMID]
Nie, P., Zhao, K., Ma, D., Liu, H., Amin, S., & Yasin, I. (2024). Global climate change, mental health, and socio-economic stressors: Toward Sustainable Interventions across Regions. Sustainability, 16(19), 8693. [DOI:10.3390/su16198693]
Picardi, A., Mazzotti, E., & Pasquini, P. (2006). Prevalence and correlates of suicidal ideation among patients with skin disease. Journal of the American Academy of Dermatology, 54(3), 420–426. [DOI:10.1016/j.jaad.2005.11.1103] [PMID]
Sutaria, A. H., Masood, S., Saleh, H. M., & Schlessinger, J. (2023). Acne Vulgaris. In StatPearls. StatPearls Publishing. [PMID]
Williams, H. C., Dellavalle, R. P., & Garner, S. (2012). Acne vulgaris. Lancet (London, England), 379(9813), 361–372. [DOI:10.1016/S0140-6736(11)60321-8] [PMID]
Young, J. E., Klosko, J. S., & Weishaar, M. E (2008). Schema therapy: A practitioner”s guide. New York: Guilford Press. [Link]
Zouboulis, C. C., & Böhm, M. (2004). Neuroendocrine regulation of sebocytes -- a pathogenetic link between stress and acne. Experimental Dermatology, 13 (Suppl 4), 31–35. [DOI:10.1111/j.1600-0625.2004.00254.x] [PMID]
Zouboulis, C. C., Eady, A., Philpott, M., Goldsmith, L. A., Orfanos, C., Cunliffe, W. C., & Rosenfield, R. (2005). What is the pathogenesis of acne? Experimental Dermatology, 14(2), 143–152. [DOI:10.1111/j.0906-6705.2005.0285a.x] [PMID]
Type of Study: Original Research Article |
Subject:
Cognitive behavioral
Received: 2025/07/4 | Accepted: 2025/08/25 | Published: 2025/10/27
Received: 2025/07/4 | Accepted: 2025/08/25 | Published: 2025/10/27
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |