Volume 13, Issue 4 (Autumn 2025)
PCP 2025, 13(4): 299-308 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Alavizadeh S A, demehri F, afshani A, sadri S. Predicting Childhood OCD Symptoms: The Mediating Effect of Self-concept on Religiosity, Guilt, and Parental Perfectionism. PCP 2025; 13 (4) :299-308
URL: http://jpcp.uswr.ac.ir/article-1-1038-en.html
URL: http://jpcp.uswr.ac.ir/article-1-1038-en.html
1- Department of Psychology, Faculty of Humanities, Science and Arts University, Yazd, Iran.
2- Department of Psychology, Faculty of Humanities, Science and Arts University, Yazd, Iran. ,demehri@sau.ac.ir
3- Department of Sociology, Faculty of Social Sciences, Yazd University, Yazd, Iran.
2- Department of Psychology, Faculty of Humanities, Science and Arts University, Yazd, Iran. ,
3- Department of Sociology, Faculty of Social Sciences, Yazd University, Yazd, Iran.
Full-Text [PDF 752 kb]
(47 Downloads)
| Abstract (HTML) (124 Views)
Full-Text: (24 Views)
Introduction
Recent research has highlighted the significant role of family dynamics in children’s development, including parent-child relationships, academic achievement, motivation, well-being, and mental health (Draženović et al., 2023). Globally, approximately one in six children and adolescents experience mental disorders, with obsessive-compulsive disorder (OCD) being particularly prevalent (WHO, 2024). OCD in children is characterized by persistent, distressing thoughts and behaviors that interfere with daily functioning (Wichers et al., 2023). Among parental factors, religious adherence has emerged as a significant and influential factor. While it can promote positive outcomes such as resilience, well-being, and prosocial behaviors, it may also elicit feelings of guilt when individuals perceive themselves as failing to meet ethical or religious standards (Abramowitz & Buchholz, 2020; Bukhori et al., 2022; Tamrchi et al., 2024). Religious adherence is a multidimensional construct encompassing several components, such as religious beliefs, practices, experiences, and identity (Aman et al., 2021; Bôas & Nakasu, 2021). Additionally, religious individuals often experience feelings of guilt due to their religious beliefs and values, as well as the ethical principles inherent in their religions, even for the smallest actions that contradict these principles (Federico et al., 2021).
Parental guilt and perfectionism, defined as a tendency to set excessively high standards and criticize oneself or one’s children, can impact children’s emotional and cognitive development (Lavrijsen et al., 2021; Vanzhula et al., 2021). In the context of motherhood, guilt can arise from various situations, which may have both positive and negative effects on the mother’s mental and emotional health (Bastin et al., 2021; Kalmijn et al., 2019). When children are exposed to the excessive and unrealistic demands of their perfectionist parents, they tend to exhibit more obsessive behavior in their tasks (Hu et al., 2023). Perfectionistic mothers may excessively criticize themselves and their children, leading to feelings of inadequacy and low self-esteem (Curran & Hill, 2022). One study reported that perfectionism showed no significant predictive value for self-evaluation (Azizi et al., 2017). This can significantly challenge a child’s self-concept. Self-concept in children refers to their understanding of themselves, including their beliefs, values, and attitudes regarding their abilities, traits, and experiences (Bardone-Cone et al., 2022). Children’s self-concept is influenced by their caregivers’ responses to their behavior, and cultural values and beliefs can impact and shape children’s self-concept (Celikel & Çoban, 2022; Papadopoulos, 2021). A positive self-concept is associated with resilience, higher self-esteem, and better academic outcomes (Aivalioti & Pezirkianidis, 2020; Möller et al., 2020).
Furthermore, studies in diverse cultural contexts, such as Tiwari et al.’s (2024) work, show that joint versus nuclear families play a protective role in children’s well-being during stressful periods, emphasizing the influence of parental and familial environments on child mental health. Research findings indicate that unwanted intrusive thoughts are universally reported, with cross-cultural variations in their content, appraisal, and management significantly influencing the severity of obsessive-compulsive symptoms. These differences underscore the crucial role of cultural factors in the manifestation of OCD (Shams et al., 2020). Despite these findings, the mechanisms through which parental religious adherence, guilt, and perfectionism contribute to obsessive symptoms in children remain unexplored. Thus, the present study aimed to examine whether obsessive symptoms in children can be predicted by parental religious adherence, guilt, and perfectionism, with children’s self-concept serving as a mediating factor. By addressing this gap, this study provides theoretical insights into the cognitive-emotional pathways linking family influences to OCD risk in children and informs family-based interventions to promote mental health.
Materials and Methods
Design and participants
This fundamental correlational study employed structural equation modeling (SEM). The target population consisted of approximately 750 students aged 10-12 years and their mothers in Yazd Province, as determined by the Ministry of Education. According to Morgan’s table, the required sample size was 256 participants. Ultimately, 256 questionnaires were distributed (both online and paper formats), of which 240 were returned complete and valid, yielding a response rate of 93.7%. Participants were selected through voluntary convenience sampling, which may have limited the generalizability of the results. A call for participation was issued in cooperation with the Ministry of Education, and eligible families who expressed interest were invited to complete questionnaires.
Inclusion and exclusion criteria
The inclusion criteria included the willingness and informed consent of mothers and children, children aged 10–12 years, and the absence of parental psychiatric medication use. The exclusion criteria were applied through screening questions at the beginning of the survey. Children with a history of parental divorce, intellectual disability, or psychological disorders, such as attention deficit hyperactivity disorder (ADHD), depression, or anxiety, were excluded.
Study instrument
The obsessive beliefs questionnaire for children and adolescents (Coles et al., 2010), is a 44-item measure developed by the obsessive compulsive cognitions working group to assess core belief domains of responsibility/threat, perfectionism/certainty, and importance/control of thoughts. It was developed for individuals aged 8-18 years. The items were scored on a Likert scale ranging from “completely disagree” to “completely agree.”. In this questionnaire, the highest possible score an individual can obtain is 220, and the lowest possible score is 44. A score close to 220 indicates high obsessive-compulsive tendencies, while a score close to 44 indicates low obsessive-compulsive tendencies. The original version demonstrated excellent psychometric properties, including high internal consistency (Cronbach’s α>0.90 for the total score), good test re-test reliability, and strong construct validity, as evidenced by significant correlations with measures of OCD symptoms. The Persian 38-item adaptation, validated in Iran by Halvaiepour et al. (2013) maintained good reliability (α=0.85) and convergent validity. The reliability of the scale was assessed using Cronbach’s α for its four subscales, yielding the following results: overestimation of threat (α=0.87), perfectionism (α=0.81), responsibility (α=0.74), and over-importance of thoughts (α=0.72). Furthermore, the four-factor structure of the questionnaire was confirmed through factor analysis, supporting its construct validity.
The religious adherence questionnaire (Ahmadi et al., 2022), a 60-item self-report measure developed and validated by Janbozorgi (2009) within an Iranian context, is designed to assess the degree of Islamic religious adherence. Responses are recorded on a four-point Likert scale ranging from “completely agree” to “completely disagree.” The instrument comprises three subscales: Religious adherence, non-adherence, and ambivalence. It demonstrated strong internal consistency, with a Cronbach’s α of 0.81 for the total scale and ranging from 0.69 to 0.88 for the subscales. Furthermore, its validity is supported by a significant correlation of 0.47 with the Allport religious orientation scale, indicating acceptable convergent validity (Ahmadi et al., 2022).
The guilt questionnaire (Kugler & Jones, 1992), a 45-item scale measuring three dimensions of guilt (trait guilt, state guilt, and moral standards), was employed to assess guilt proneness. Scores between 45 and 90 indicate a low level of guilt, suggesting minimal tendencies toward guilt-related responses. Scores ranging from 90 to 135 reflect a moderate level of guilt, representing average or situational guilt experiences. Finally, a score above 135 signifies a high level of guilt, with pronounced and potentially pervasive feelings of guilt across various contexts. The scale has demonstrated strong psychometric properties internationally, with high internal consistency (Cronbach’s α=0.87) and established construct validity. Its validity and reliability have also been confirmed for use in Iranian populations, with studies reporting excellent internal consistency (Cronbach’s α up to 0.91 for the full scale) and a confirmed three-factor structure, supporting its use in this cultural context (Demehri et al., 2021).
Frost multidimensional perfectionism scale (Frost et al., 1990), a 35-item instrument, was used to assess multidimensional perfectionism, encompassing factors, such as concern over mistakes, personal standards, parental expectations, and self-critical evaluation. The scale has demonstrated excellent internal consistency in its original validation (Cronbach’s α=0.91) and strong construct validity, as evidenced by significant correlations with related psychological measures (Frost et al., 1990). Its reliability and validity have also been established in Iranian contexts, with studies reporting comparable high internal consistency (e.g. Cronbach’s α ranging from 0.85 to 0.93 for subscales) and a confirmed multifactorial structure, supporting its appropriateness for use in this population (Farrokhi et al., 2013).
The Piers-Harris children’s self-concept scale (Piers, 2002), an 80-item self-report measure, is designed to assess children’s self-concept across six domains: Behavior, intellectual and scholastic status, physical appearance, anxiety, sociability, and happiness. The responses to the questions in this test will be “yes” or “no.” The items are scored in both positive and negative directions to accurately reflect the assessed dimensions. The Persian version of this scale has been translated and validated for use among Iranian children, demonstrating excellent internal consistency (Cronbach’s α=0.92) and strong convergent validity with other measures of self-concept. In the present study, participants responded to items in a yes/no format, with higher scores reflecting a more positive self-concept (Mostafa Bashi & Shaker Dioulagh, 2019).
Data collection procedure
Ethical approval was obtained from the relevant university committee and the Ministry of Education. At the beginning of the questionnaires, the study’s ethical principles, including voluntary participation and confidentiality of responses, were clearly explained. Demographic questions were presented first, followed by the study measures. Participants were instructed to read items carefully and answer as completely as possible. Incomplete questionnaires were excluded from the final analyses. Additionally, to minimize response bias, anonymity was assured, and both online and paper versions were made available to accommodate participants’ preferences. Data were analyzed using SEM in AMOS software, version 24. Prior to analysis, assumptions of normality and multicollinearity were examined. Model fit was evaluated using indices, such as CMIN/degree of freedom (df), root mean square error of approximation (RMSEA), normal fit index (NFI), Tucker-Lewis index (TLI), incremental fit index (IFI), and comparative fit index (CFI).
Data analysis
Data were analyzed using SPSS software, version 22. Descriptive statistics, including measures of dispersion (variance) and central tendency (Mean±SD), were employed. In inferential statistics, AMOS. SEM assessed relationships among variables, with indices, such as RMSEA (≤0.08) and CFI (≥0.9), determining model fit.
Results
According to the findings of the study, the Mean±SD of the variables were as follows: religious commitment: (100.96±12.45), obsessive-compulsive symptoms: (133.18±18.89), perfectionism: (84.56±10.23), guilt: (130.26±17.24), and self-concept: (24.77±6.44). Before proceeding to the examination and analysis of the research hypotheses, the correlation coefficients of various variables were reviewed. The findings in Table 1 show a significant negative relationship between religious adherence and self-concept and obsessive symptoms (P<0.001).
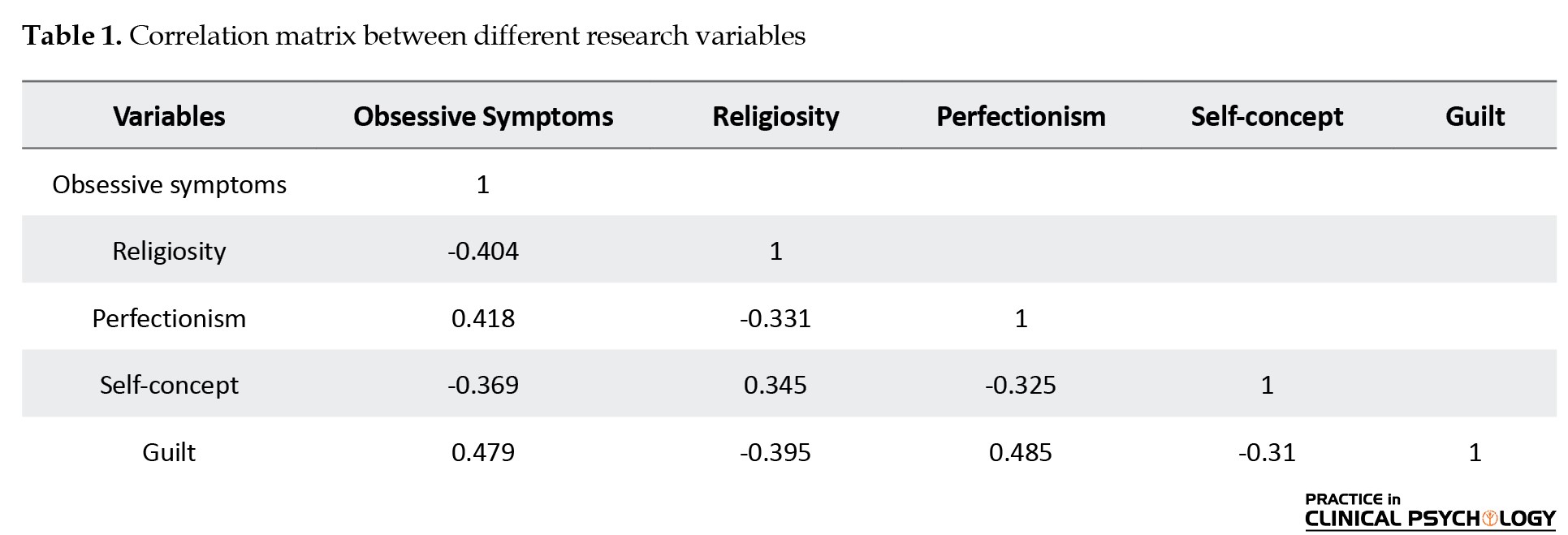
However, a significant positive relationship was found between guilt feelings and perfectionism with obsessive symptoms (P<0.001).
The model is presented with unstandardized estimates in Figure 1 and with standardized estimates in Figure 2.
Recent research has highlighted the significant role of family dynamics in children’s development, including parent-child relationships, academic achievement, motivation, well-being, and mental health (Draženović et al., 2023). Globally, approximately one in six children and adolescents experience mental disorders, with obsessive-compulsive disorder (OCD) being particularly prevalent (WHO, 2024). OCD in children is characterized by persistent, distressing thoughts and behaviors that interfere with daily functioning (Wichers et al., 2023). Among parental factors, religious adherence has emerged as a significant and influential factor. While it can promote positive outcomes such as resilience, well-being, and prosocial behaviors, it may also elicit feelings of guilt when individuals perceive themselves as failing to meet ethical or religious standards (Abramowitz & Buchholz, 2020; Bukhori et al., 2022; Tamrchi et al., 2024). Religious adherence is a multidimensional construct encompassing several components, such as religious beliefs, practices, experiences, and identity (Aman et al., 2021; Bôas & Nakasu, 2021). Additionally, religious individuals often experience feelings of guilt due to their religious beliefs and values, as well as the ethical principles inherent in their religions, even for the smallest actions that contradict these principles (Federico et al., 2021).
Parental guilt and perfectionism, defined as a tendency to set excessively high standards and criticize oneself or one’s children, can impact children’s emotional and cognitive development (Lavrijsen et al., 2021; Vanzhula et al., 2021). In the context of motherhood, guilt can arise from various situations, which may have both positive and negative effects on the mother’s mental and emotional health (Bastin et al., 2021; Kalmijn et al., 2019). When children are exposed to the excessive and unrealistic demands of their perfectionist parents, they tend to exhibit more obsessive behavior in their tasks (Hu et al., 2023). Perfectionistic mothers may excessively criticize themselves and their children, leading to feelings of inadequacy and low self-esteem (Curran & Hill, 2022). One study reported that perfectionism showed no significant predictive value for self-evaluation (Azizi et al., 2017). This can significantly challenge a child’s self-concept. Self-concept in children refers to their understanding of themselves, including their beliefs, values, and attitudes regarding their abilities, traits, and experiences (Bardone-Cone et al., 2022). Children’s self-concept is influenced by their caregivers’ responses to their behavior, and cultural values and beliefs can impact and shape children’s self-concept (Celikel & Çoban, 2022; Papadopoulos, 2021). A positive self-concept is associated with resilience, higher self-esteem, and better academic outcomes (Aivalioti & Pezirkianidis, 2020; Möller et al., 2020).
Furthermore, studies in diverse cultural contexts, such as Tiwari et al.’s (2024) work, show that joint versus nuclear families play a protective role in children’s well-being during stressful periods, emphasizing the influence of parental and familial environments on child mental health. Research findings indicate that unwanted intrusive thoughts are universally reported, with cross-cultural variations in their content, appraisal, and management significantly influencing the severity of obsessive-compulsive symptoms. These differences underscore the crucial role of cultural factors in the manifestation of OCD (Shams et al., 2020). Despite these findings, the mechanisms through which parental religious adherence, guilt, and perfectionism contribute to obsessive symptoms in children remain unexplored. Thus, the present study aimed to examine whether obsessive symptoms in children can be predicted by parental religious adherence, guilt, and perfectionism, with children’s self-concept serving as a mediating factor. By addressing this gap, this study provides theoretical insights into the cognitive-emotional pathways linking family influences to OCD risk in children and informs family-based interventions to promote mental health.
Materials and Methods
Design and participants
This fundamental correlational study employed structural equation modeling (SEM). The target population consisted of approximately 750 students aged 10-12 years and their mothers in Yazd Province, as determined by the Ministry of Education. According to Morgan’s table, the required sample size was 256 participants. Ultimately, 256 questionnaires were distributed (both online and paper formats), of which 240 were returned complete and valid, yielding a response rate of 93.7%. Participants were selected through voluntary convenience sampling, which may have limited the generalizability of the results. A call for participation was issued in cooperation with the Ministry of Education, and eligible families who expressed interest were invited to complete questionnaires.
Inclusion and exclusion criteria
The inclusion criteria included the willingness and informed consent of mothers and children, children aged 10–12 years, and the absence of parental psychiatric medication use. The exclusion criteria were applied through screening questions at the beginning of the survey. Children with a history of parental divorce, intellectual disability, or psychological disorders, such as attention deficit hyperactivity disorder (ADHD), depression, or anxiety, were excluded.
Study instrument
The obsessive beliefs questionnaire for children and adolescents (Coles et al., 2010), is a 44-item measure developed by the obsessive compulsive cognitions working group to assess core belief domains of responsibility/threat, perfectionism/certainty, and importance/control of thoughts. It was developed for individuals aged 8-18 years. The items were scored on a Likert scale ranging from “completely disagree” to “completely agree.”. In this questionnaire, the highest possible score an individual can obtain is 220, and the lowest possible score is 44. A score close to 220 indicates high obsessive-compulsive tendencies, while a score close to 44 indicates low obsessive-compulsive tendencies. The original version demonstrated excellent psychometric properties, including high internal consistency (Cronbach’s α>0.90 for the total score), good test re-test reliability, and strong construct validity, as evidenced by significant correlations with measures of OCD symptoms. The Persian 38-item adaptation, validated in Iran by Halvaiepour et al. (2013) maintained good reliability (α=0.85) and convergent validity. The reliability of the scale was assessed using Cronbach’s α for its four subscales, yielding the following results: overestimation of threat (α=0.87), perfectionism (α=0.81), responsibility (α=0.74), and over-importance of thoughts (α=0.72). Furthermore, the four-factor structure of the questionnaire was confirmed through factor analysis, supporting its construct validity.
The religious adherence questionnaire (Ahmadi et al., 2022), a 60-item self-report measure developed and validated by Janbozorgi (2009) within an Iranian context, is designed to assess the degree of Islamic religious adherence. Responses are recorded on a four-point Likert scale ranging from “completely agree” to “completely disagree.” The instrument comprises three subscales: Religious adherence, non-adherence, and ambivalence. It demonstrated strong internal consistency, with a Cronbach’s α of 0.81 for the total scale and ranging from 0.69 to 0.88 for the subscales. Furthermore, its validity is supported by a significant correlation of 0.47 with the Allport religious orientation scale, indicating acceptable convergent validity (Ahmadi et al., 2022).
The guilt questionnaire (Kugler & Jones, 1992), a 45-item scale measuring three dimensions of guilt (trait guilt, state guilt, and moral standards), was employed to assess guilt proneness. Scores between 45 and 90 indicate a low level of guilt, suggesting minimal tendencies toward guilt-related responses. Scores ranging from 90 to 135 reflect a moderate level of guilt, representing average or situational guilt experiences. Finally, a score above 135 signifies a high level of guilt, with pronounced and potentially pervasive feelings of guilt across various contexts. The scale has demonstrated strong psychometric properties internationally, with high internal consistency (Cronbach’s α=0.87) and established construct validity. Its validity and reliability have also been confirmed for use in Iranian populations, with studies reporting excellent internal consistency (Cronbach’s α up to 0.91 for the full scale) and a confirmed three-factor structure, supporting its use in this cultural context (Demehri et al., 2021).
Frost multidimensional perfectionism scale (Frost et al., 1990), a 35-item instrument, was used to assess multidimensional perfectionism, encompassing factors, such as concern over mistakes, personal standards, parental expectations, and self-critical evaluation. The scale has demonstrated excellent internal consistency in its original validation (Cronbach’s α=0.91) and strong construct validity, as evidenced by significant correlations with related psychological measures (Frost et al., 1990). Its reliability and validity have also been established in Iranian contexts, with studies reporting comparable high internal consistency (e.g. Cronbach’s α ranging from 0.85 to 0.93 for subscales) and a confirmed multifactorial structure, supporting its appropriateness for use in this population (Farrokhi et al., 2013).
The Piers-Harris children’s self-concept scale (Piers, 2002), an 80-item self-report measure, is designed to assess children’s self-concept across six domains: Behavior, intellectual and scholastic status, physical appearance, anxiety, sociability, and happiness. The responses to the questions in this test will be “yes” or “no.” The items are scored in both positive and negative directions to accurately reflect the assessed dimensions. The Persian version of this scale has been translated and validated for use among Iranian children, demonstrating excellent internal consistency (Cronbach’s α=0.92) and strong convergent validity with other measures of self-concept. In the present study, participants responded to items in a yes/no format, with higher scores reflecting a more positive self-concept (Mostafa Bashi & Shaker Dioulagh, 2019).
Data collection procedure
Ethical approval was obtained from the relevant university committee and the Ministry of Education. At the beginning of the questionnaires, the study’s ethical principles, including voluntary participation and confidentiality of responses, were clearly explained. Demographic questions were presented first, followed by the study measures. Participants were instructed to read items carefully and answer as completely as possible. Incomplete questionnaires were excluded from the final analyses. Additionally, to minimize response bias, anonymity was assured, and both online and paper versions were made available to accommodate participants’ preferences. Data were analyzed using SEM in AMOS software, version 24. Prior to analysis, assumptions of normality and multicollinearity were examined. Model fit was evaluated using indices, such as CMIN/degree of freedom (df), root mean square error of approximation (RMSEA), normal fit index (NFI), Tucker-Lewis index (TLI), incremental fit index (IFI), and comparative fit index (CFI).
Data analysis
Data were analyzed using SPSS software, version 22. Descriptive statistics, including measures of dispersion (variance) and central tendency (Mean±SD), were employed. In inferential statistics, AMOS. SEM assessed relationships among variables, with indices, such as RMSEA (≤0.08) and CFI (≥0.9), determining model fit.
Results
According to the findings of the study, the Mean±SD of the variables were as follows: religious commitment: (100.96±12.45), obsessive-compulsive symptoms: (133.18±18.89), perfectionism: (84.56±10.23), guilt: (130.26±17.24), and self-concept: (24.77±6.44). Before proceeding to the examination and analysis of the research hypotheses, the correlation coefficients of various variables were reviewed. The findings in Table 1 show a significant negative relationship between religious adherence and self-concept and obsessive symptoms (P<0.001).
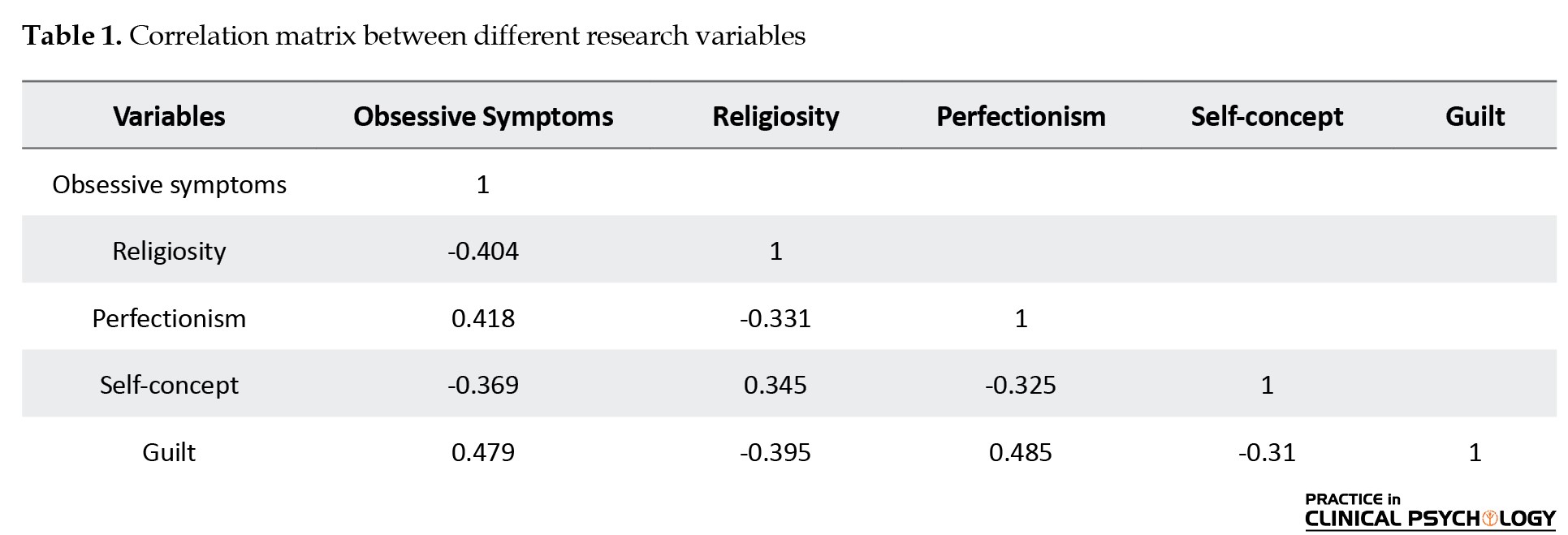
However, a significant positive relationship was found between guilt feelings and perfectionism with obsessive symptoms (P<0.001).
The model is presented with unstandardized estimates in Figure 1 and with standardized estimates in Figure 2.
A covariance-based SEM approach was used to test the research hypotheses. Figure 2 shows the estimates for the overall model fit indices and main parameters.
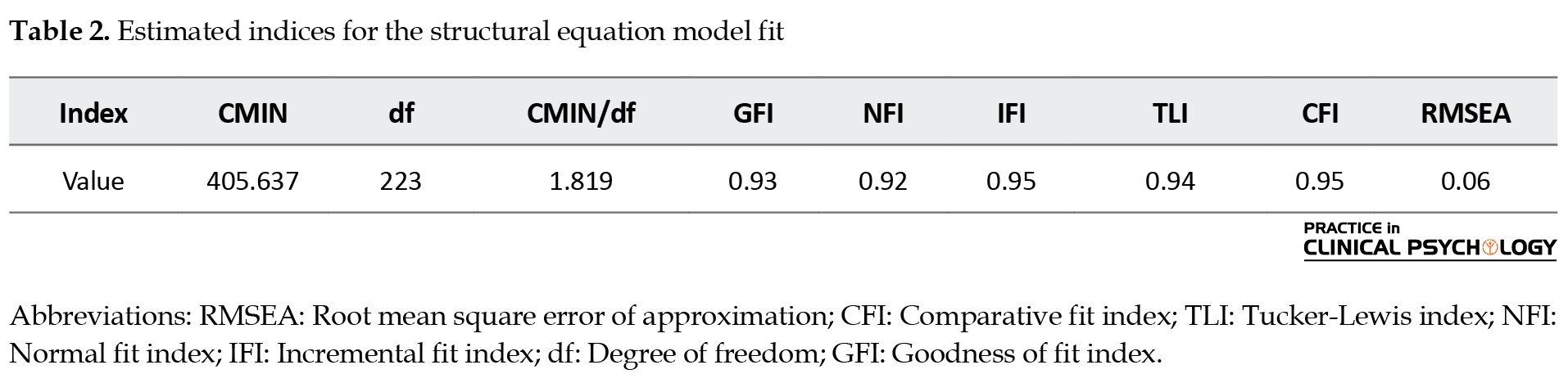
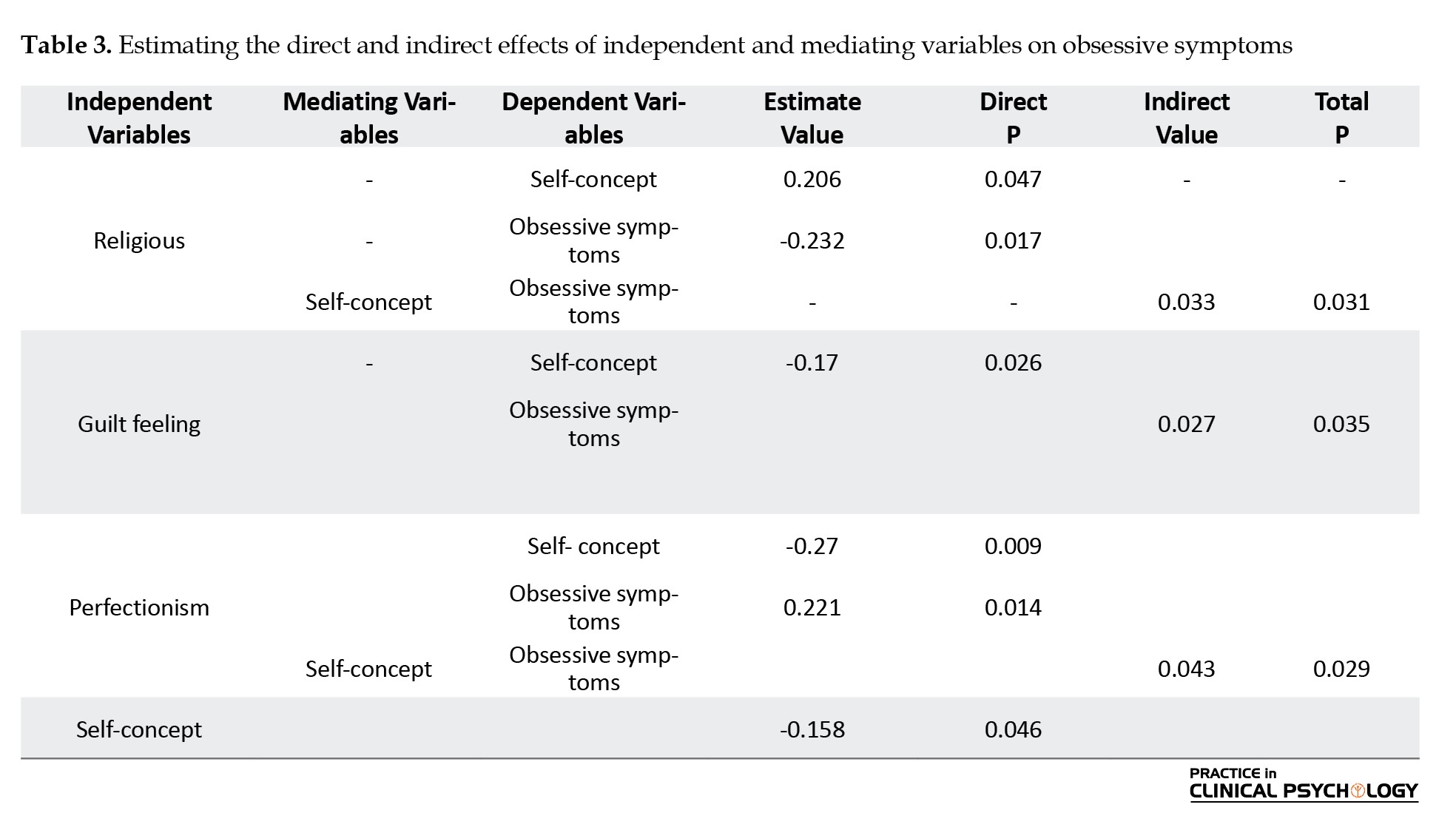
A confirmatory factor analysis was conducted to evaluate the proposed structural model. Model fit was assessed using multiple indices, including χ²/df, RMSEA, GFI, TLI, NFI, CFI, and IFI. While there is no absolute cutoff for χ²/df, smaller values indicate a better fit, with values below 3 generally considered acceptable. An RMSEA ≤0.08 indicates a good fit, whereas values ≥0.1 suggest a poor fit. For GFI, NFI, IFI, TLI, and CFI, values ≥0.9 are considered indicative of adequate fit. As shown in Table 2, all fit indices for the proposed model fell within the acceptable range, demonstrating that the model fit the data well.
These results support the hypothesized relationships and provide confidence in the model’s structural validity.
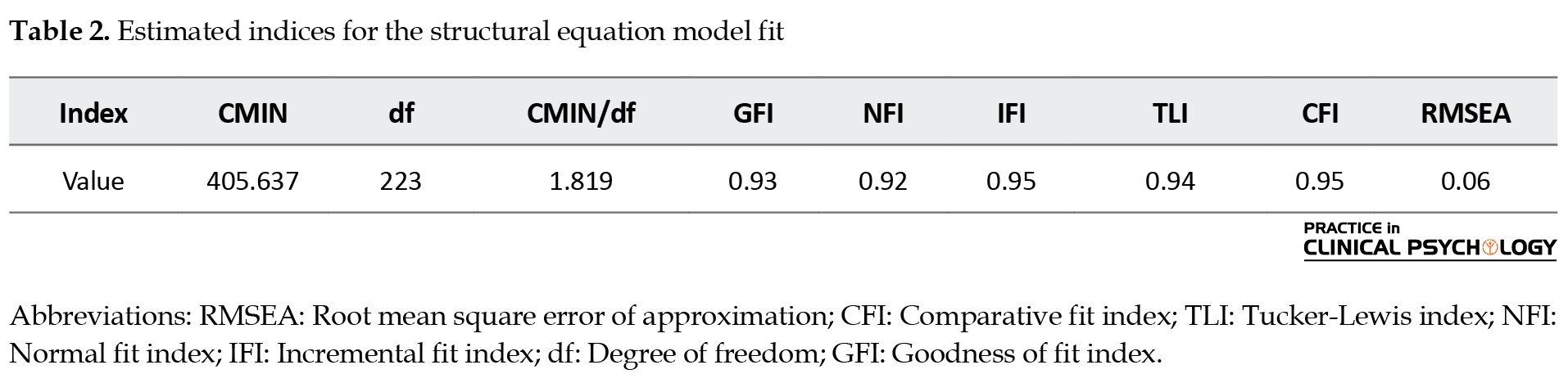
To calculate the direct, indirect, and total effects of the independent and mediator variables on the dependent variable, the bootstrapping method was used in AMOS software. Table 3 presents the results.
Based on the estimated values, the effects of parental factors and self-concept on obsessive-compulsive symptoms in children were examined. Religious commitment had a positive and significant effect on self-concept (γ=0.206, P<0.05), suggesting that higher parental religious commitment is associated with a stronger self-concept in children. It also showed a negative and significant direct effect on obsessive symptoms (γ=-0.232, P<0.05), indicating that greater religious commitment is related to fewer obsessive-compulsive symptoms. Guilt feelings had a negative effect on self-concept (γ=-0.170, P<0.05) and a positive effect on obsessive symptoms (γ=0.312, P<0.01), implying that higher parental guilt is associated with lower self-concept and higher obsessive symptoms. Perfectionism showed a negative relationship with self-concept (γ=-0.270, P<0.01), indicating that children of more perfectionistic parents tend to have lower self-concepts. Self-concept had a negative effect on obsessive symptoms (β=-0.158, P<0.05), highlighting its protective role, as children with higher self-concept experience fewer obsessive-compulsive symptoms. The Sobel test was conducted to examine the mediating role of self-concept. The results indicated that the mediating effect of self-concept between religious commitment and obsessive symptoms was significant (Sobel statistic =-2.82, P<0.01), confirming that self-concept partially mediated this relationship.
Discussion
The results indicate several significant effects of parental factors on children’s self-concept and obsessive-compulsive symptoms. Parental religious commitment positively influenced children’s self-concept and negatively affected obsessive symptoms, suggesting that shared values, emotional support, and coping strategies in religious families foster resilience and a sense of meaning. This finding aligns with previous research (Bôas & Nakasu, 2021; Bukhori et al., 2022) and highlights the potential of family-based spiritual and moral guidance in promoting children’s psychological well-being. In practical terms, communities and schools can encourage family involvement in value-based programs to support children’s mental health. Conversely, parental guilt negatively impacted children’s self-concept and positively predicted obsessive symptoms, highlighting how a guilt-laden environment can promote self-criticism and obsessive rumination, consistent with psychoanalytic theory (Gomez-Ortiz & Roldán-Barrios, 2021). This underscores the importance of educating parents about the psychological consequences of excessive guilt and providing community-based support for parental-emotional regulation. This suggests that parental religious commitment may reduce the likelihood of obsessive behaviors in children by providing emotional and spiritual support, coping strategies a stronger sense of self and meaning in life (White et al., 2021).
Parental perfectionism also negatively affects self-concept and increases obsessive symptoms, reflecting how unrealistic parental expectations contribute to anxiety and fear of failure in children. These findings suggest that interventions targeting parental perfectionism, such as parenting workshops and counseling, could reduce children’s risk of obsessive behaviors. The high demands and unrealistic expectations set by perfectionistic parents can create anxiety and fear of failure, leading children to develop obsessive behaviors (Choe et al., 2020).
Self-concept was a key mediator in these relationships. It buffered the negative effects of parental guilt and perfectionism and enhanced the protective influence of religious commitment on obsessive symptoms, emphasizing the role of children’s self-perception in shaping mental health outcomes (Celikel & Çoban, 2022). Interventions aimed at strengthening self-concept through school programs, community activities, or family-centered therapy may have a broad impact on mitigating obsessive tendencies. Cultural specificity is particularly important: The observed patterns reflect the social and religious contexts of Yazd Province, where family dynamics and religious practices uniquely shape children’s experiences and self-perception. These findings highlight the need for culturally sensitive approaches in psychological interventions and community programs to effectively support child mental health. These findings highlight the importance of addressing both supportive and detrimental parental factors in interventions aimed at promoting children’s mental health. Cultural specificity should be considered, as the observed patterns reflect the social and religious context of Yazd, Iran. Furthermore, self-concept mediated the effects of parental guilt and perfectionism on obsessive symptoms, highlighting the importance of self-perception in understanding how parental behaviors and emotions influence children’s mental health outcomes. These findings underscore the significant role of self-concept as a mediator in the relationship between parental religious commitment, guilt, perfectionism, and children’s obsessive symptoms. They highlight the importance of parental influence and self-perception in understanding and addressing childhood obsessive-compulsive symptoms. Future research should explore intervention strategies aimed at improving self-concept to mitigate the adverse effects of parental guilt and perfectionism while leveraging the protective aspects of this commitment.
Conclusion
This study highlights the intricate interplay between parental religious adherence, guilt, and perfectionism in shaping children’s self-concept and obsessive-compulsive symptoms. The findings emphasize the protective role of a positive self-concept fostered by parental support and religious values, as well as the detrimental impact of parental guilt and perfectionism. Addressing these parental factors in therapeutic settings, such as through family-centered counseling or parent-training programs, can enhance children’s mental health and resilience. Future research should expand these findings to diverse cultural and social contexts to examine universal and culture-specific patterns and develop targeted, culturally sensitive interventions. Ultimately, this work underscores the importance of fostering a supportive and value-oriented family environment to mitigate obsessive-compulsive tendencies in children.
Limitations and future research
The study focused on a specific cultural and geographical context (Yazd, Iran), limiting the generalizability of the findings to other populations and cultural settings. Also, the correlational nature of the study prevents causal inferences about the relationships between variables. In addition, the study did not account for fathers’ specific influences separately, which may provide unique insights into children’s self-concept and obsessive symptoms. Future research should expand these findings to diverse cultural and social contexts to examine the universality and specificity of parental influences on children’s self-concept and obsessive-compulsive symptoms. Researchers should adopt longitudinal designs to investigate causal relationships and track developmental changes over time. Moreover, studies should explore targeted, culturally sensitive interventions, such as family-centered counseling, parent-training programs, or school-based self-concept enhancement activities, to mitigate the negative effects of parental guilt and perfectionism while leveraging the protective role of religious commitment in this context.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Science and Culture, Tehran, Iran (Code: IR.ACECR.USC.REC.1403.122). Participation in the study was voluntary and confidential, and informed consent was obtained from the students.
Funding
This article was extracted from the master’s thesis of Samin Alsadat Alavizadeh, approved by the Science and Arts University, Yazd, Iran. This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, supervision and writing: Farangis Demehri; Methodology and investigation: Alireza Afshani and Shamim Sadri; Data collection and analysis: Samin Alsadat Alavizadeh, Farangis Demehri, and Shamim Sadri.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely thank the participating children and their families for their valuable contributions to this study. The authors are also grateful to the University of Science and Art in Yazd Province for their support in facilitating data collection.
References
Abramowitz, J. S., & Buchholz, J. L. (2020). Spirituality/religion and obsessive-compulsive-related disorders. In D. H. Rosmarin& H. G. Koenig (Eds.), Handbook of spirituality, religion, and mental health (pp. 61-78). Massachusetts: Academic Press [DOI:10.1016/B978-0-12-816766-3.00004-5]
Ahmadi, M., Khalatbari, J., Aghayousefi, A., & Janbozorgi, M. (2022). The effect of the variables of multidimensional spiritual pattern on obsessive-compulsive disorder with the mediation of dysfunctional beliefs. Studies in Islam and Psychology, 16(31), 129-153. [DOI:10.30471/psy.2022.8982.2059]
Aivalioti, I., & Pezirkianidis, C. (2020). The role of family resilience on parental well-being and resilience levels. Psychology, 11(11), 1705-1728. [DOI:10.4236/psych.2020.1111108]
Aman, J., Abbas, J., Lela, U., & Shi, G. (2021). Religious affiliation, daily spirituals, and private religious factors promote marital commitment among married couples: Does religiosity help people amid the COVID-19 crisis? Frontiers in Psychology, 12, 657400. [DOI:10.3389/fpsyg.2021.657400] [PMID]
Azizi, S., Garoosi Farshi, M. T., Poursharifi, H., & Farazmand, S. (2017). Effects of personality traits and perfectionism in predicting core self-evaluations of women with trichotillomania and healthy women. Practice in Clinical Psychology, 5(2), 123-132. [DOI:10.18869/acadpub.jpcp.5.2.123]
Bardone-Cone, A. M., White, J. P., Thompson, K. A., Zucker, N., Watson, H. J., & Bulik, C. M. (2022). Examination of perfectionism and self-concept constructs across stages of eating disorder recovery in men: An exploratory study. Eating Behaviors, 46, 101658. [DOI:10.1016/j.eatbeh.2022.101658] [PMID]
Bastin, C., Rakesh, D., Harrison, B. J., Davey, C. G., Allen, N. B., & Muller, S., et al. (2021). Feelings of shame and guilt are associated with distinct neural activation in youth. Biological Psychology, 159, 108025. [DOI:10.1016/j.biopsycho.2021.108025] [PMID]
Bôas, G., & Nakasu, M. V. P. (2021). Association between resilience, religiosity and therapeutic adherence in patients undergoing hemodialysis. Revista de Medicina, 100(2), 119-127. [DOI:10.11606/issn.1679-9836.v100i2p119-127]
Bukhori, B., Hidayanti, E., & Situmorang, D. D. B. (2022). Religious coping strategies for people with HIV/AIDS (PLWHA) Muslims in Indonesia: A qualitative study with a telling-the-stories. Heliyon, 8(12), e12208. [DOI:10.1016/j.heliyon.2022.e12208] [PMID]
Celikel, B., & Çoban, A. E. (2022). Self-concept with cross-cultural perspective: 36-72-month-old preschool children in Turkey and Germany. Frontiers in Psychology, 13, 821074.[DOI:10.3389/fpsyg.2022.821074] [PMID]
Choe, S. Y., Lee, J. O., & Read, S. J. (2020). Self‐concept as a mechanism through which parental psychological control impairs empathy development from adolescence to emerging adulthood. Social Development, 29(3), 713-731. [DOI:10.1111/sode.12431]
Coles, M. E., Wolters, L. H., Sochting, I., de Haan, E., Pietrefesa, A. S., & Whiteside, S. P. (2010). Development and initial validation of the obsessive belief questionnaire-child version (OBQ-CV). Depression and Anxiety, 27(10), 982–991.[DOI:10.1002/da.20702] [PMID]
Curran, T., & Hill, A. P. (2022). Young people’s perceptions of their parents’ expectations and criticism are increasing over time: Implications for perfectionism. Psychological Bulletin, 148(1-2), 107-128. [DOI:10.1037/bul0000347] [PMID]
Demehri, F., Rostami, M., & Saeidmanesh, M. S. (2021). [The effectiveness of compassion therapy on guilt, perfectionism and imperfection schema in the children of law enforcement unit (Persian)]. Military Psychology, 12(48), 59-74. [Link]
Draženović, M., Vukušić Rukavina, T., & Machala Poplašen, L. (2023). Impact of social media use on mental health within adolescent and student populations during COVID-19 pandemic. International Journal of Environmental Research and Public Health, 20(4), 3392. [DOI: 10.3390/ijerph20043392] [PMID]
Farrokhi, A., Motesharee, E., Zeyd Abadi, R., Aghasi, S., & Parsa, G. R. (2013). [Validity and reliability of the Persian version of sport perfectionism scale in Iranian athletes (Persian)]. Journal of Sports and Motor Development and Learning, 5(1), 55-76. [DOI:10.22059/jmlm.2013.35004]
Federico, C. M., de Zavala, A. G., & Baran, T. (2021). Collective narcissism, in-group satisfaction, and solidarity in the face of COVID-19. Social Psychological and Personality Science, 12(6), 1071-1081. [DOI:10.1177/1948550620963655]
Frost, R. O., Marten, P., Lahart, C., & Rosenblate, R. (1990). The dimensions of perfectionism. Cognitive Therapy and Research, 14(5), 449-468. [DOI:10.1007/BF01172967]
Gómez-Ortiz, O., & Roldán-Barrios, A. (2021). Work-family guilt in spanish parents: analysis of the measurement, antecedents and outcomes from a gender perspective. International Journal of Environmental Research and Public Health, 18(15), 8229. [DOI:10.3390/ijerph18158229] [PMID]
Halvaiepour, Z., Khormaei, F., Khanzadeh, M., & Nosratabadi, M. (2013). [Validation of the Persian version of obsessive beliefs questionnaire-child and teenager version in group of Iranian adolescents (Persian)]. The Journal of Shahid Sadoughi University of Medical Sciences, 21(3), 319-329. [Link]
Hu, P., Liang, P., Liu, X., Ouyang, Y., & Wang, J. (2023). Parenting styles and obsessive-compulsive symptoms in college students: the mediating role of perfectionism. Frontiers in Psychiatry, 14, 1126689. [DOI:10.3389/fpsyt.2023.1126689] [PMID]
Janbozorgi, M. (2009). [Construction and validity of religious adherence test on the basis of the statements of Quran and Nahjul Balaghah (Persian)]. Studies in Islam and Psychology, 3(5), 79-105. [Link]
Kalmijn, M., de Leeuw, S. G., Hornstra, M., Ivanova, K., van Gaalen, R., & van Houdt, K. (2019). Family complexity into adulthood: The central role of mothers in shaping intergenerational ties. American Sociological Review, 84(5), 876-904. [DOI:10.1177/0003122419871959]
Kugler, K., & Jones, W. H. (1992). On conceptualizing and assessing guilt. Journal of Personality and Social Psychology, 62(2), 318-327. [Link]
Lavrijsen, J., Soenens, B., Vansteenkiste, M., & Verschueren, K. (2021). Is intelligence related to perfectionism? Multidimensional perfectionism and parental antecedents among adolescents across varying levels of cognitive ability. Journal of Personality, 89(4), 652–671. [DOI:10.1111/jopy.12606] [PMID]
Möller, J., Zitzmann, S., Helm, F., Machts, N., & Wolff, F. (2020). A meta-analysis of relations between achievement and self-concept. Review of Educational Research, 90(3), 376-419. [DOI:10.3102/0034654320919354]
Mostafa Bashi, A., & Shaker Dioulagh, A. (2019). [Comparison of behavioral problems, self-concept and emotional control in low-hearing and Low-visibility people in the city of Boukan (Persian)]. Rooyesh-e-Ravanshenasi Journal(RRJ), 8(6), 165-172. [Link]
World Health Organization. (2024). Working for a brighter, healthier future: how WHO improves health and promotes well-being for the world’s adolescents. Geneva: World Health Organization. [Link]
Papadopoulos, D. (2021). Examining the relationships among cognitive ability, domain-specific self-concept, and behavioral self-esteem of gifted children aged 5-6 years: A cross-sectional study. Behavioral Sciences, 11(7), 93. [DOI:10.3390/bs11070093] [PMID]
Piers, E. V. (2002). Piers-Harris children’s self-concept scale. Los Angeles: Western Psychological Services. [Link]
Shams, G., Abasi, I., & Youssefi, Y. (2020). Cultural issues in understanding obsessive-compulsive disorder: Nature, appraisals, and control strategies of unwanted intrusive thoughts in Iranian Nonclinical Population. Practice in Clinical Psychology, 8(2), 73-84. [DOI:10.32598/jpcp.8.2.98.5]
Tamrchi, S., Rabiee, M., & Dolatshahi, B. (2024). Investigating parenting styles and relationship obsessive-compulsive disorder symptoms: The mediating role of alexithymia. Practice in Clinical Psychology, 12(2), 165-178. [DOI:10.32598/jpcp.12.2.932.1]
Tiwari, G. K., Tiwari, R. P., Pandey, R., Ray, B., Dwivedi, A., & Sharma, D. N., et al. (2024). Perceived life outcomes of Indian children during the early phase of the COVID-19 lockdown: The protective roles of joint and nuclear families. Journal of Research and Health, 14(1), 43-54. [DOI: 10.32598/JRH.14.1.1992.4]
Vanzhula, I. A., Kinkel-Ram, S. S., & Levinson, C. A. (2021). Perfectionism and difficulty controlling thoughts bridge eating disorder and obsessive-compulsive disorder symptoms: A network analysis. Journal of Affective Disorders, 283, 302-309. [DOI:10.1016/j.jad.2021.01.083] [PMID]
White, C. J., Baimel, A., & Norenzayan, A. (2021). How cultural learning and cognitive biases shape religious beliefs. Current Opinion in Psychology, 40, 34-39. [DOI:10.1016/j.copsyc.2020.07.033] [PMID]
Wichers, R. H., van der Wouw, L. C., Brouwer, M. E., Lok, A., & Bockting, C. L. H. (2023). Psychotherapy for co-occurring symptoms of depression, anxiety and obsessive-compulsive disorder in children and adults with autism spectrum disorder: A systematic review and meta-analysis. Psychological Medicine, 53(1), 17–33. [DOI:10.1017/S0033291722003415] [PMID]
A confirmatory factor analysis was conducted to evaluate the proposed structural model. Model fit was assessed using multiple indices, including χ²/df, RMSEA, GFI, TLI, NFI, CFI, and IFI. While there is no absolute cutoff for χ²/df, smaller values indicate a better fit, with values below 3 generally considered acceptable. An RMSEA ≤0.08 indicates a good fit, whereas values ≥0.1 suggest a poor fit. For GFI, NFI, IFI, TLI, and CFI, values ≥0.9 are considered indicative of adequate fit. As shown in Table 2, all fit indices for the proposed model fell within the acceptable range, demonstrating that the model fit the data well.
These results support the hypothesized relationships and provide confidence in the model’s structural validity.
To calculate the direct, indirect, and total effects of the independent and mediator variables on the dependent variable, the bootstrapping method was used in AMOS software. Table 3 presents the results.
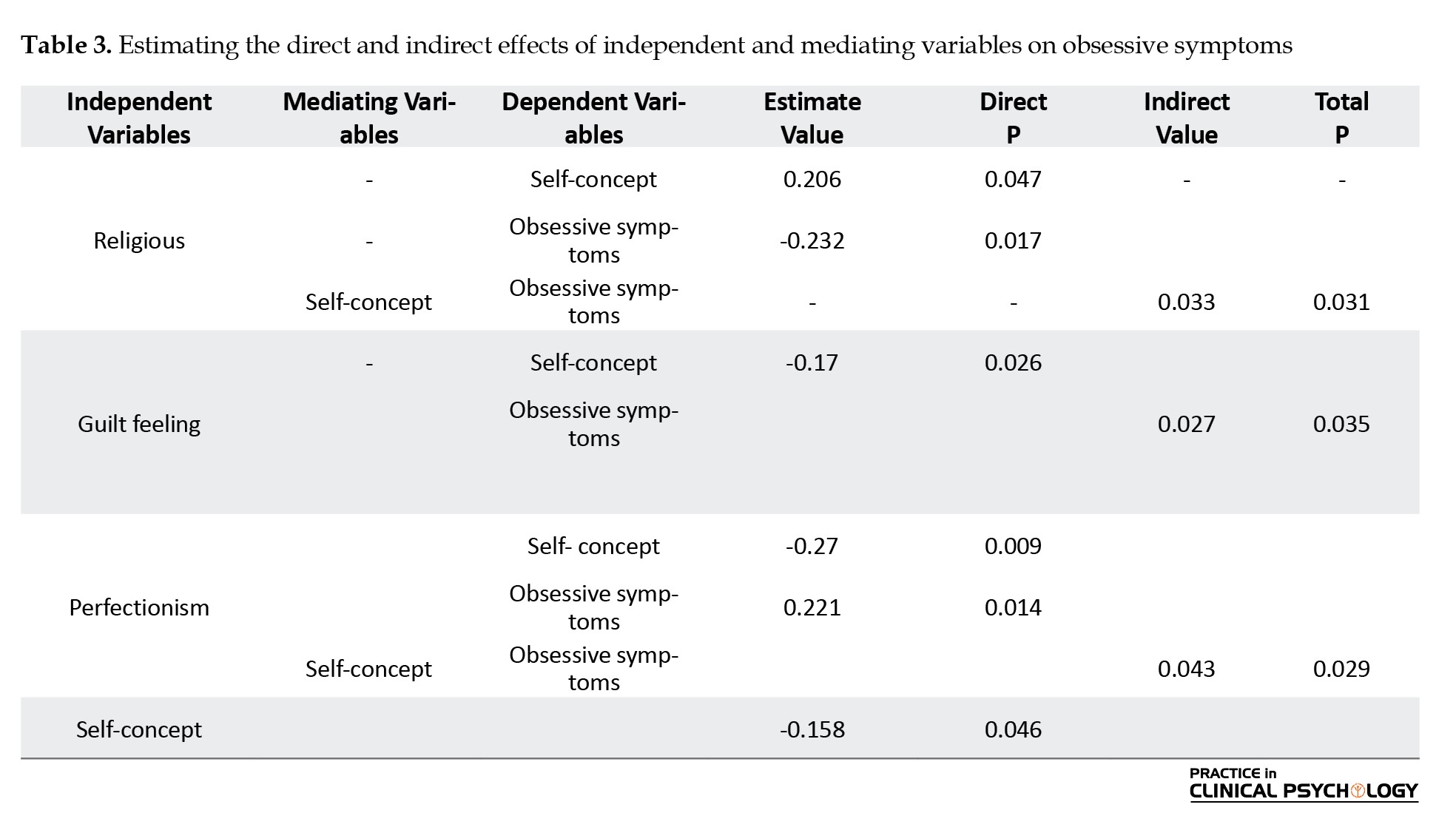
Based on the estimated values, the effects of parental factors and self-concept on obsessive-compulsive symptoms in children were examined. Religious commitment had a positive and significant effect on self-concept (γ=0.206, P<0.05), suggesting that higher parental religious commitment is associated with a stronger self-concept in children. It also showed a negative and significant direct effect on obsessive symptoms (γ=-0.232, P<0.05), indicating that greater religious commitment is related to fewer obsessive-compulsive symptoms. Guilt feelings had a negative effect on self-concept (γ=-0.170, P<0.05) and a positive effect on obsessive symptoms (γ=0.312, P<0.01), implying that higher parental guilt is associated with lower self-concept and higher obsessive symptoms. Perfectionism showed a negative relationship with self-concept (γ=-0.270, P<0.01), indicating that children of more perfectionistic parents tend to have lower self-concepts. Self-concept had a negative effect on obsessive symptoms (β=-0.158, P<0.05), highlighting its protective role, as children with higher self-concept experience fewer obsessive-compulsive symptoms. The Sobel test was conducted to examine the mediating role of self-concept. The results indicated that the mediating effect of self-concept between religious commitment and obsessive symptoms was significant (Sobel statistic =-2.82, P<0.01), confirming that self-concept partially mediated this relationship.
Discussion
The results indicate several significant effects of parental factors on children’s self-concept and obsessive-compulsive symptoms. Parental religious commitment positively influenced children’s self-concept and negatively affected obsessive symptoms, suggesting that shared values, emotional support, and coping strategies in religious families foster resilience and a sense of meaning. This finding aligns with previous research (Bôas & Nakasu, 2021; Bukhori et al., 2022) and highlights the potential of family-based spiritual and moral guidance in promoting children’s psychological well-being. In practical terms, communities and schools can encourage family involvement in value-based programs to support children’s mental health. Conversely, parental guilt negatively impacted children’s self-concept and positively predicted obsessive symptoms, highlighting how a guilt-laden environment can promote self-criticism and obsessive rumination, consistent with psychoanalytic theory (Gomez-Ortiz & Roldán-Barrios, 2021). This underscores the importance of educating parents about the psychological consequences of excessive guilt and providing community-based support for parental-emotional regulation. This suggests that parental religious commitment may reduce the likelihood of obsessive behaviors in children by providing emotional and spiritual support, coping strategies a stronger sense of self and meaning in life (White et al., 2021).
Parental perfectionism also negatively affects self-concept and increases obsessive symptoms, reflecting how unrealistic parental expectations contribute to anxiety and fear of failure in children. These findings suggest that interventions targeting parental perfectionism, such as parenting workshops and counseling, could reduce children’s risk of obsessive behaviors. The high demands and unrealistic expectations set by perfectionistic parents can create anxiety and fear of failure, leading children to develop obsessive behaviors (Choe et al., 2020).
Self-concept was a key mediator in these relationships. It buffered the negative effects of parental guilt and perfectionism and enhanced the protective influence of religious commitment on obsessive symptoms, emphasizing the role of children’s self-perception in shaping mental health outcomes (Celikel & Çoban, 2022). Interventions aimed at strengthening self-concept through school programs, community activities, or family-centered therapy may have a broad impact on mitigating obsessive tendencies. Cultural specificity is particularly important: The observed patterns reflect the social and religious contexts of Yazd Province, where family dynamics and religious practices uniquely shape children’s experiences and self-perception. These findings highlight the need for culturally sensitive approaches in psychological interventions and community programs to effectively support child mental health. These findings highlight the importance of addressing both supportive and detrimental parental factors in interventions aimed at promoting children’s mental health. Cultural specificity should be considered, as the observed patterns reflect the social and religious context of Yazd, Iran. Furthermore, self-concept mediated the effects of parental guilt and perfectionism on obsessive symptoms, highlighting the importance of self-perception in understanding how parental behaviors and emotions influence children’s mental health outcomes. These findings underscore the significant role of self-concept as a mediator in the relationship between parental religious commitment, guilt, perfectionism, and children’s obsessive symptoms. They highlight the importance of parental influence and self-perception in understanding and addressing childhood obsessive-compulsive symptoms. Future research should explore intervention strategies aimed at improving self-concept to mitigate the adverse effects of parental guilt and perfectionism while leveraging the protective aspects of this commitment.
Conclusion
This study highlights the intricate interplay between parental religious adherence, guilt, and perfectionism in shaping children’s self-concept and obsessive-compulsive symptoms. The findings emphasize the protective role of a positive self-concept fostered by parental support and religious values, as well as the detrimental impact of parental guilt and perfectionism. Addressing these parental factors in therapeutic settings, such as through family-centered counseling or parent-training programs, can enhance children’s mental health and resilience. Future research should expand these findings to diverse cultural and social contexts to examine universal and culture-specific patterns and develop targeted, culturally sensitive interventions. Ultimately, this work underscores the importance of fostering a supportive and value-oriented family environment to mitigate obsessive-compulsive tendencies in children.
Limitations and future research
The study focused on a specific cultural and geographical context (Yazd, Iran), limiting the generalizability of the findings to other populations and cultural settings. Also, the correlational nature of the study prevents causal inferences about the relationships between variables. In addition, the study did not account for fathers’ specific influences separately, which may provide unique insights into children’s self-concept and obsessive symptoms. Future research should expand these findings to diverse cultural and social contexts to examine the universality and specificity of parental influences on children’s self-concept and obsessive-compulsive symptoms. Researchers should adopt longitudinal designs to investigate causal relationships and track developmental changes over time. Moreover, studies should explore targeted, culturally sensitive interventions, such as family-centered counseling, parent-training programs, or school-based self-concept enhancement activities, to mitigate the negative effects of parental guilt and perfectionism while leveraging the protective role of religious commitment in this context.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the University of Science and Culture, Tehran, Iran (Code: IR.ACECR.USC.REC.1403.122). Participation in the study was voluntary and confidential, and informed consent was obtained from the students.
Funding
This article was extracted from the master’s thesis of Samin Alsadat Alavizadeh, approved by the Science and Arts University, Yazd, Iran. This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization, supervision and writing: Farangis Demehri; Methodology and investigation: Alireza Afshani and Shamim Sadri; Data collection and analysis: Samin Alsadat Alavizadeh, Farangis Demehri, and Shamim Sadri.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors sincerely thank the participating children and their families for their valuable contributions to this study. The authors are also grateful to the University of Science and Art in Yazd Province for their support in facilitating data collection.
References
Abramowitz, J. S., & Buchholz, J. L. (2020). Spirituality/religion and obsessive-compulsive-related disorders. In D. H. Rosmarin& H. G. Koenig (Eds.), Handbook of spirituality, religion, and mental health (pp. 61-78). Massachusetts: Academic Press [DOI:10.1016/B978-0-12-816766-3.00004-5]
Ahmadi, M., Khalatbari, J., Aghayousefi, A., & Janbozorgi, M. (2022). The effect of the variables of multidimensional spiritual pattern on obsessive-compulsive disorder with the mediation of dysfunctional beliefs. Studies in Islam and Psychology, 16(31), 129-153. [DOI:10.30471/psy.2022.8982.2059]
Aivalioti, I., & Pezirkianidis, C. (2020). The role of family resilience on parental well-being and resilience levels. Psychology, 11(11), 1705-1728. [DOI:10.4236/psych.2020.1111108]
Aman, J., Abbas, J., Lela, U., & Shi, G. (2021). Religious affiliation, daily spirituals, and private religious factors promote marital commitment among married couples: Does religiosity help people amid the COVID-19 crisis? Frontiers in Psychology, 12, 657400. [DOI:10.3389/fpsyg.2021.657400] [PMID]
Azizi, S., Garoosi Farshi, M. T., Poursharifi, H., & Farazmand, S. (2017). Effects of personality traits and perfectionism in predicting core self-evaluations of women with trichotillomania and healthy women. Practice in Clinical Psychology, 5(2), 123-132. [DOI:10.18869/acadpub.jpcp.5.2.123]
Bardone-Cone, A. M., White, J. P., Thompson, K. A., Zucker, N., Watson, H. J., & Bulik, C. M. (2022). Examination of perfectionism and self-concept constructs across stages of eating disorder recovery in men: An exploratory study. Eating Behaviors, 46, 101658. [DOI:10.1016/j.eatbeh.2022.101658] [PMID]
Bastin, C., Rakesh, D., Harrison, B. J., Davey, C. G., Allen, N. B., & Muller, S., et al. (2021). Feelings of shame and guilt are associated with distinct neural activation in youth. Biological Psychology, 159, 108025. [DOI:10.1016/j.biopsycho.2021.108025] [PMID]
Bôas, G., & Nakasu, M. V. P. (2021). Association between resilience, religiosity and therapeutic adherence in patients undergoing hemodialysis. Revista de Medicina, 100(2), 119-127. [DOI:10.11606/issn.1679-9836.v100i2p119-127]
Bukhori, B., Hidayanti, E., & Situmorang, D. D. B. (2022). Religious coping strategies for people with HIV/AIDS (PLWHA) Muslims in Indonesia: A qualitative study with a telling-the-stories. Heliyon, 8(12), e12208. [DOI:10.1016/j.heliyon.2022.e12208] [PMID]
Celikel, B., & Çoban, A. E. (2022). Self-concept with cross-cultural perspective: 36-72-month-old preschool children in Turkey and Germany. Frontiers in Psychology, 13, 821074.[DOI:10.3389/fpsyg.2022.821074] [PMID]
Choe, S. Y., Lee, J. O., & Read, S. J. (2020). Self‐concept as a mechanism through which parental psychological control impairs empathy development from adolescence to emerging adulthood. Social Development, 29(3), 713-731. [DOI:10.1111/sode.12431]
Coles, M. E., Wolters, L. H., Sochting, I., de Haan, E., Pietrefesa, A. S., & Whiteside, S. P. (2010). Development and initial validation of the obsessive belief questionnaire-child version (OBQ-CV). Depression and Anxiety, 27(10), 982–991.[DOI:10.1002/da.20702] [PMID]
Curran, T., & Hill, A. P. (2022). Young people’s perceptions of their parents’ expectations and criticism are increasing over time: Implications for perfectionism. Psychological Bulletin, 148(1-2), 107-128. [DOI:10.1037/bul0000347] [PMID]
Demehri, F., Rostami, M., & Saeidmanesh, M. S. (2021). [The effectiveness of compassion therapy on guilt, perfectionism and imperfection schema in the children of law enforcement unit (Persian)]. Military Psychology, 12(48), 59-74. [Link]
Draženović, M., Vukušić Rukavina, T., & Machala Poplašen, L. (2023). Impact of social media use on mental health within adolescent and student populations during COVID-19 pandemic. International Journal of Environmental Research and Public Health, 20(4), 3392. [DOI: 10.3390/ijerph20043392] [PMID]
Farrokhi, A., Motesharee, E., Zeyd Abadi, R., Aghasi, S., & Parsa, G. R. (2013). [Validity and reliability of the Persian version of sport perfectionism scale in Iranian athletes (Persian)]. Journal of Sports and Motor Development and Learning, 5(1), 55-76. [DOI:10.22059/jmlm.2013.35004]
Federico, C. M., de Zavala, A. G., & Baran, T. (2021). Collective narcissism, in-group satisfaction, and solidarity in the face of COVID-19. Social Psychological and Personality Science, 12(6), 1071-1081. [DOI:10.1177/1948550620963655]
Frost, R. O., Marten, P., Lahart, C., & Rosenblate, R. (1990). The dimensions of perfectionism. Cognitive Therapy and Research, 14(5), 449-468. [DOI:10.1007/BF01172967]
Gómez-Ortiz, O., & Roldán-Barrios, A. (2021). Work-family guilt in spanish parents: analysis of the measurement, antecedents and outcomes from a gender perspective. International Journal of Environmental Research and Public Health, 18(15), 8229. [DOI:10.3390/ijerph18158229] [PMID]
Halvaiepour, Z., Khormaei, F., Khanzadeh, M., & Nosratabadi, M. (2013). [Validation of the Persian version of obsessive beliefs questionnaire-child and teenager version in group of Iranian adolescents (Persian)]. The Journal of Shahid Sadoughi University of Medical Sciences, 21(3), 319-329. [Link]
Hu, P., Liang, P., Liu, X., Ouyang, Y., & Wang, J. (2023). Parenting styles and obsessive-compulsive symptoms in college students: the mediating role of perfectionism. Frontiers in Psychiatry, 14, 1126689. [DOI:10.3389/fpsyt.2023.1126689] [PMID]
Janbozorgi, M. (2009). [Construction and validity of religious adherence test on the basis of the statements of Quran and Nahjul Balaghah (Persian)]. Studies in Islam and Psychology, 3(5), 79-105. [Link]
Kalmijn, M., de Leeuw, S. G., Hornstra, M., Ivanova, K., van Gaalen, R., & van Houdt, K. (2019). Family complexity into adulthood: The central role of mothers in shaping intergenerational ties. American Sociological Review, 84(5), 876-904. [DOI:10.1177/0003122419871959]
Kugler, K., & Jones, W. H. (1992). On conceptualizing and assessing guilt. Journal of Personality and Social Psychology, 62(2), 318-327. [Link]
Lavrijsen, J., Soenens, B., Vansteenkiste, M., & Verschueren, K. (2021). Is intelligence related to perfectionism? Multidimensional perfectionism and parental antecedents among adolescents across varying levels of cognitive ability. Journal of Personality, 89(4), 652–671. [DOI:10.1111/jopy.12606] [PMID]
Möller, J., Zitzmann, S., Helm, F., Machts, N., & Wolff, F. (2020). A meta-analysis of relations between achievement and self-concept. Review of Educational Research, 90(3), 376-419. [DOI:10.3102/0034654320919354]
Mostafa Bashi, A., & Shaker Dioulagh, A. (2019). [Comparison of behavioral problems, self-concept and emotional control in low-hearing and Low-visibility people in the city of Boukan (Persian)]. Rooyesh-e-Ravanshenasi Journal(RRJ), 8(6), 165-172. [Link]
World Health Organization. (2024). Working for a brighter, healthier future: how WHO improves health and promotes well-being for the world’s adolescents. Geneva: World Health Organization. [Link]
Papadopoulos, D. (2021). Examining the relationships among cognitive ability, domain-specific self-concept, and behavioral self-esteem of gifted children aged 5-6 years: A cross-sectional study. Behavioral Sciences, 11(7), 93. [DOI:10.3390/bs11070093] [PMID]
Piers, E. V. (2002). Piers-Harris children’s self-concept scale. Los Angeles: Western Psychological Services. [Link]
Shams, G., Abasi, I., & Youssefi, Y. (2020). Cultural issues in understanding obsessive-compulsive disorder: Nature, appraisals, and control strategies of unwanted intrusive thoughts in Iranian Nonclinical Population. Practice in Clinical Psychology, 8(2), 73-84. [DOI:10.32598/jpcp.8.2.98.5]
Tamrchi, S., Rabiee, M., & Dolatshahi, B. (2024). Investigating parenting styles and relationship obsessive-compulsive disorder symptoms: The mediating role of alexithymia. Practice in Clinical Psychology, 12(2), 165-178. [DOI:10.32598/jpcp.12.2.932.1]
Tiwari, G. K., Tiwari, R. P., Pandey, R., Ray, B., Dwivedi, A., & Sharma, D. N., et al. (2024). Perceived life outcomes of Indian children during the early phase of the COVID-19 lockdown: The protective roles of joint and nuclear families. Journal of Research and Health, 14(1), 43-54. [DOI: 10.32598/JRH.14.1.1992.4]
Vanzhula, I. A., Kinkel-Ram, S. S., & Levinson, C. A. (2021). Perfectionism and difficulty controlling thoughts bridge eating disorder and obsessive-compulsive disorder symptoms: A network analysis. Journal of Affective Disorders, 283, 302-309. [DOI:10.1016/j.jad.2021.01.083] [PMID]
White, C. J., Baimel, A., & Norenzayan, A. (2021). How cultural learning and cognitive biases shape religious beliefs. Current Opinion in Psychology, 40, 34-39. [DOI:10.1016/j.copsyc.2020.07.033] [PMID]
Wichers, R. H., van der Wouw, L. C., Brouwer, M. E., Lok, A., & Bockting, C. L. H. (2023). Psychotherapy for co-occurring symptoms of depression, anxiety and obsessive-compulsive disorder in children and adults with autism spectrum disorder: A systematic review and meta-analysis. Psychological Medicine, 53(1), 17–33. [DOI:10.1017/S0033291722003415] [PMID]
Type of Study: Original Research Article |
Subject:
Family and group therapy
Received: 2025/03/1 | Accepted: 2025/05/23 | Published: 2025/10/1
Received: 2025/03/1 | Accepted: 2025/05/23 | Published: 2025/10/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |