Volume 13, Issue 4 (Autumn 2025)
PCP 2025, 13(4): 287-298 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Abdolloahi M H, Mohammadkhani S, Noury R. Childhood Trauma and Substance Use Tendencies: The Mediating Effects of PTSD, Impulsivity, and Emotion Dysregulation. PCP 2025; 13 (4) :287-298
URL: http://jpcp.uswr.ac.ir/article-1-1028-en.html
URL: http://jpcp.uswr.ac.ir/article-1-1028-en.html
1- Department of Clinical Psychology, Faculty of Psychology and Education, Kharazmi University, Tehran, Iran.
2- Department of Clinical Psychology, Faculty of Psychology and Education, Kharazmi University, Tehran, Iran. ,mohammadkhani@khu.ac.ir
2- Department of Clinical Psychology, Faculty of Psychology and Education, Kharazmi University, Tehran, Iran. ,
Keywords: Adverse childhood experiences (ACEs), Substance use, Impulsive behavior, Emotion regulation, Post-traumatic stress disorder (PTSD)
Full-Text [PDF 702 kb]
(583 Downloads)
| Abstract (HTML) (684 Views)
Materials and Methods
Following recommendations for SEM (Kline, 2010), 815 students from universities in Tehran were initially recruited using non-random sampling. The inclusion criteria included enrollment at a Tehran university between 18 and 70 years old. The exclusion criteria involved incomplete or inconsistent survey responses. Even though the age range in our sample was broad (18-70 years) with a Mean±SD age of 24.89±7.02, we also did not employ stratification or classification analysis based on age because of the sample size and main research focus. Since age can be a factor affecting the variables under analysis, this is one of the limitations of our study. Future research should also consider a more stratified analysis or another detailed age-based control to establish the possible moderating impact of age on the association between childhood trauma, psychological mediators, and substance use.
Procedures
This descriptive-correlational study used an online survey hosted on the Porsline platform, distributed through Telegram channels popular among Tehran University students. Convenience sampling through Telegram channels was utilized because of inaccessibility and resource constraints. This can restrict the generalizability of the results to all students at Tehran University. Future studies should establish methods for probabilistic sampling to be more representative. Participation was voluntary, with no incentives provided, and participants could withdraw at any time. The survey, taking approximately 35 minutes to complete, included measures of childhood trauma, substance use tendencies (SUT), impulsivity, emotional dysregulation, and PTSD symptoms.
Measures
Addiction potential scale
The addiction potential scale (APS) evaluates the tendency to use substances in an individual using 41 questions, five of which are lie scales. The scoring scale is a 4-point Likert scale (0=strongly disagree, 3=strongly agree) (Weed et al., 1992). It was adapted to Iran by Zargar et al. (2008), containing active and passive tendency subscales with a score range of 0-108. The scale’s construct validity was established using a correlation coefficient of 0.45 and the Symptom Checklist-25 (SCL-25) (Zargar et al., 2008). In this study, Cronbach’s α was 0.84, indicating good reliability.
Childhood trauma questionnaire-short form (CTQ-SF)
The CTQ-SF is a 28-item self-report measure to measure five types of child abuse: Emotional neglect, emotional abuse, sexual abuse, physical neglect, and physical abuse (Bernstein et al., 2003). The scale of measurement involved a Likert scale (5-point scale), where 1 (never true) and 5 (often true). The Persian translation, which has been proven valid by Garrusi and Nakhaee (2009), is quite reliable (Cronbach’s α=0.85 in the present study).
Short form of the UPPS-P impulsive behavior scale (SUPPS-P)
The 20-item SUPPS-P estimates five aspects of impulsivity: Sensation seeking, lack of persistence, lack of reflection, positive urgency, and negative urgency (Cyders et al., 2014). The ratings were on a 4-point scale (1=completely agree, 4=completely disagree). The Persian version, which was validated by Jebraeili et al., 2019, and proved to have good reliability (Cronbach’s α=0.80 in this research).
PTSD checklist (PCL-5)
PCL-5 is a self-report scale, comprising 20 questions, assessing how well the symptoms of PTSD are authenticated by the diagnostic and statistical manual of mental disorders, fifth edition (DSM-5) rules, and evaluated on a 5-point Likert scale (0=not at all, 4=excessively) (Weathers et al., 2014). The Persian version exhibited a high reliability rate (Cronbach’s α=0.92 in the current study) (Sadeghi et al., 2016).
Difficulties in emotion regulation scale (DERS)
The DERS is a 36-item instrument used to measure six facets of psychometric instruments: non-acceptance, goals, strategies, impulse, awareness, and clarity of emotional dysregulation (Gratz & Roemer, 2004). The grading scale value of items is 5-point Likert (1=rarely, 5=almost always). The Persian version reflected reliability (Cronbach’s α coefficient of 0.93 in the current study) (Khanzadeh et al., 2012).
Statistical analysis
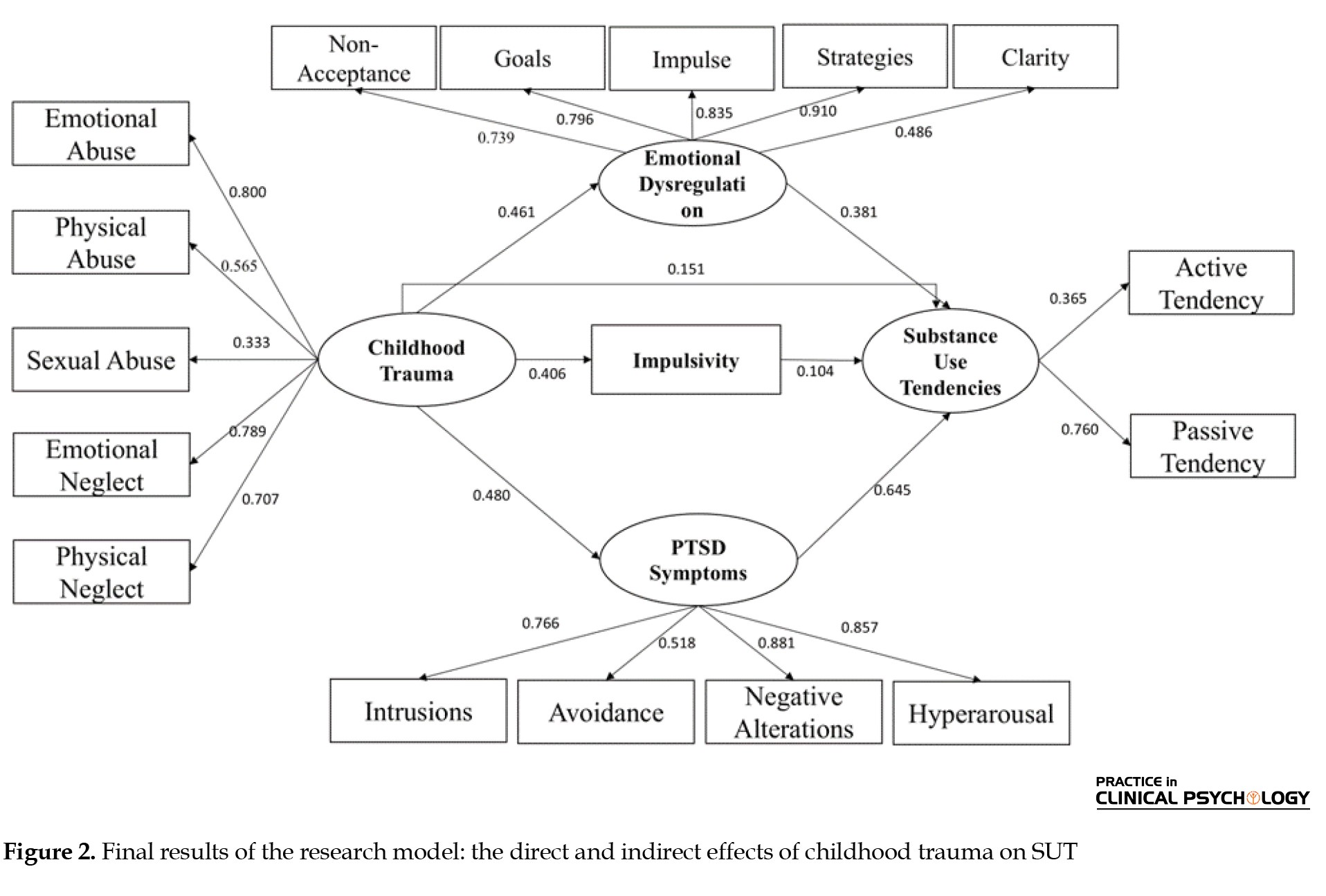
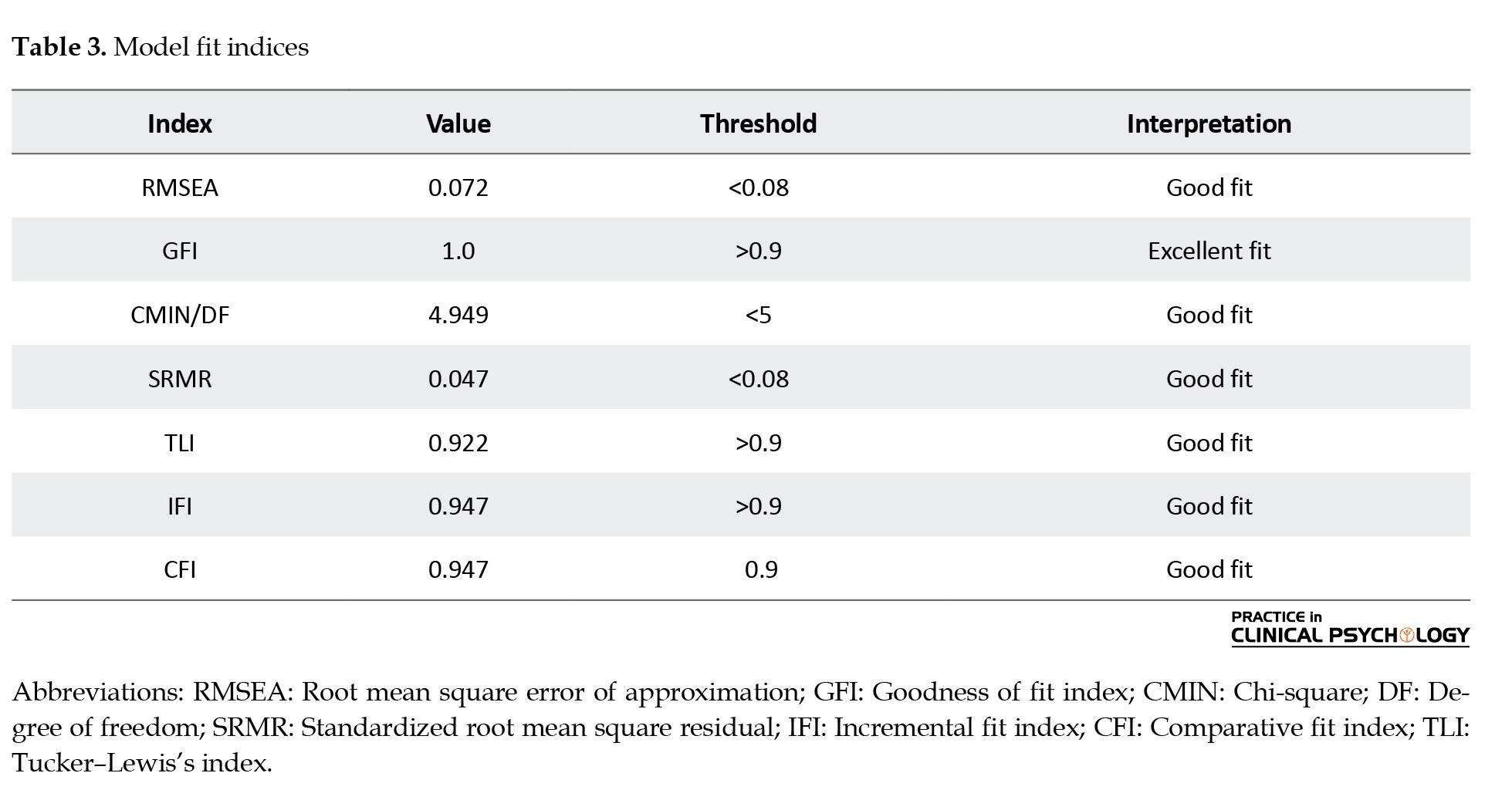
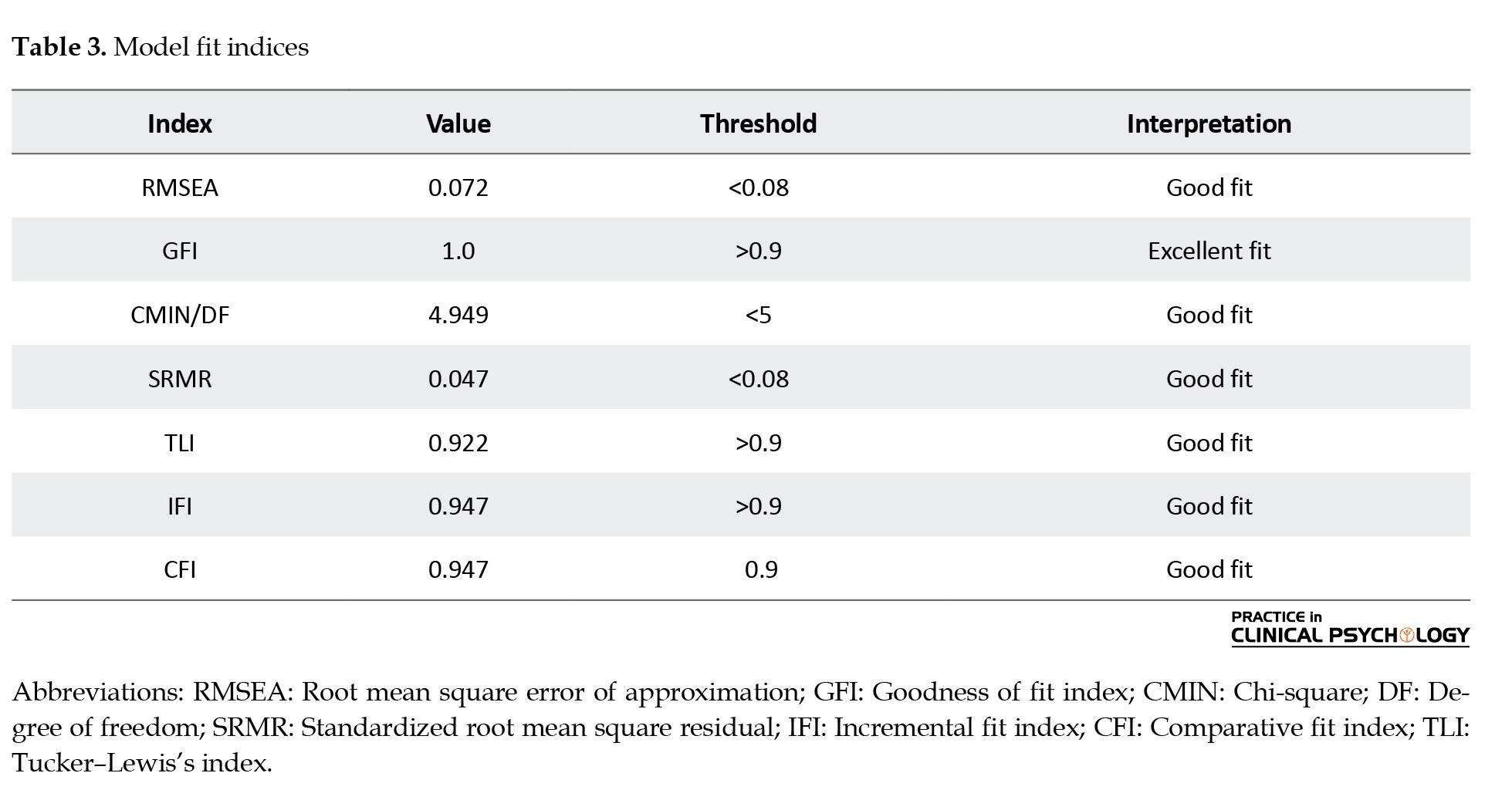
SEM was employed to examine direct and indirect relationships among childhood trauma, impulsivity, emotional dysregulation, PTSD symptoms, and SUT. Descriptive statistics were used to summarize the participant characteristics. To examine the assumption of non-collinearity, the variance inflation factor and tolerance index statistics were used. The tolerance index of the variables was in the range of 0.476 to 0.853, and the variance inflation factor was also in the range of 1.173 to 2.102. Given that none of the values related to the tolerance index were less than 0.01 and none of the values related to the variance inflation factor were more than 10, it was possible to be confident about the assumption of non-collinearity. The present study used a frequency table and a box plot to identify univariate outliers for observable variables. When the values of P1 and P2 in the Amos software output are equal to 0.000, it can be concluded that the respondent is a multivariate outlier (Kline, 2010). After identifying univariate outliers, multivariate outliers were not identified due to the favorable state of model fit. The non-acceptance subscale of DERS was excluded due to low factor loading (<0.3). Pearson’s correlation coefficient was used to assess the relationship between the variables. Model fit was evaluated using the root mean square error of approximation (RMSEA) (<0.08), goodness of fit index (GFI), comparative fit index (CFI), Tucker–Lewis index (TLI), incremental fit index (IFI) (≥0.90), standardized root mean square residual (SRMR) (<0.08), and chi-square/degree of freedom (CMIN/DF) (<5) as thresholds for good fit. Analyses were performed using SPSS software, version 27 and Amos software, version 29. The final outcomes of the research model are presented in Figure 2.
Results
Participant characteristics
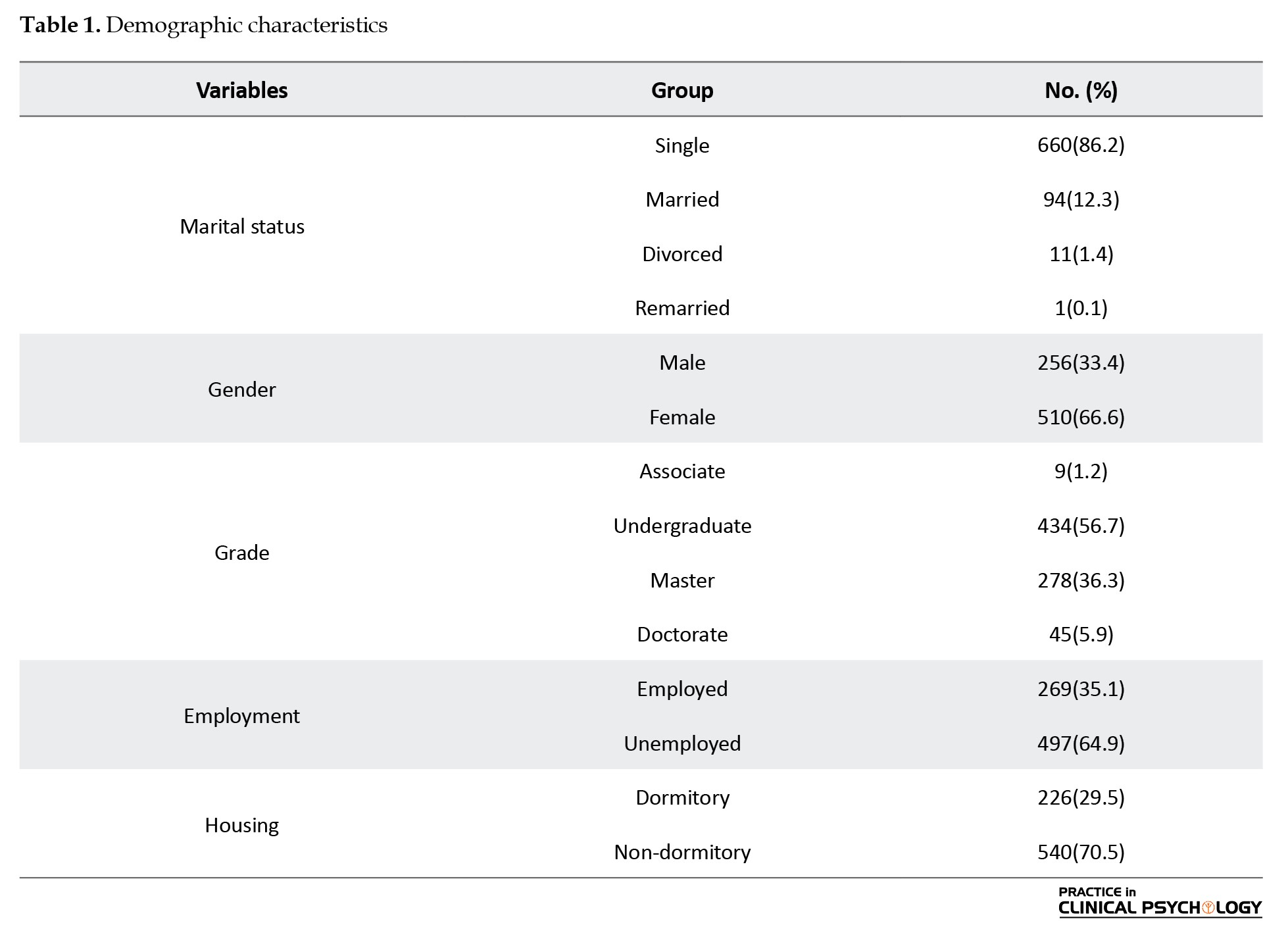
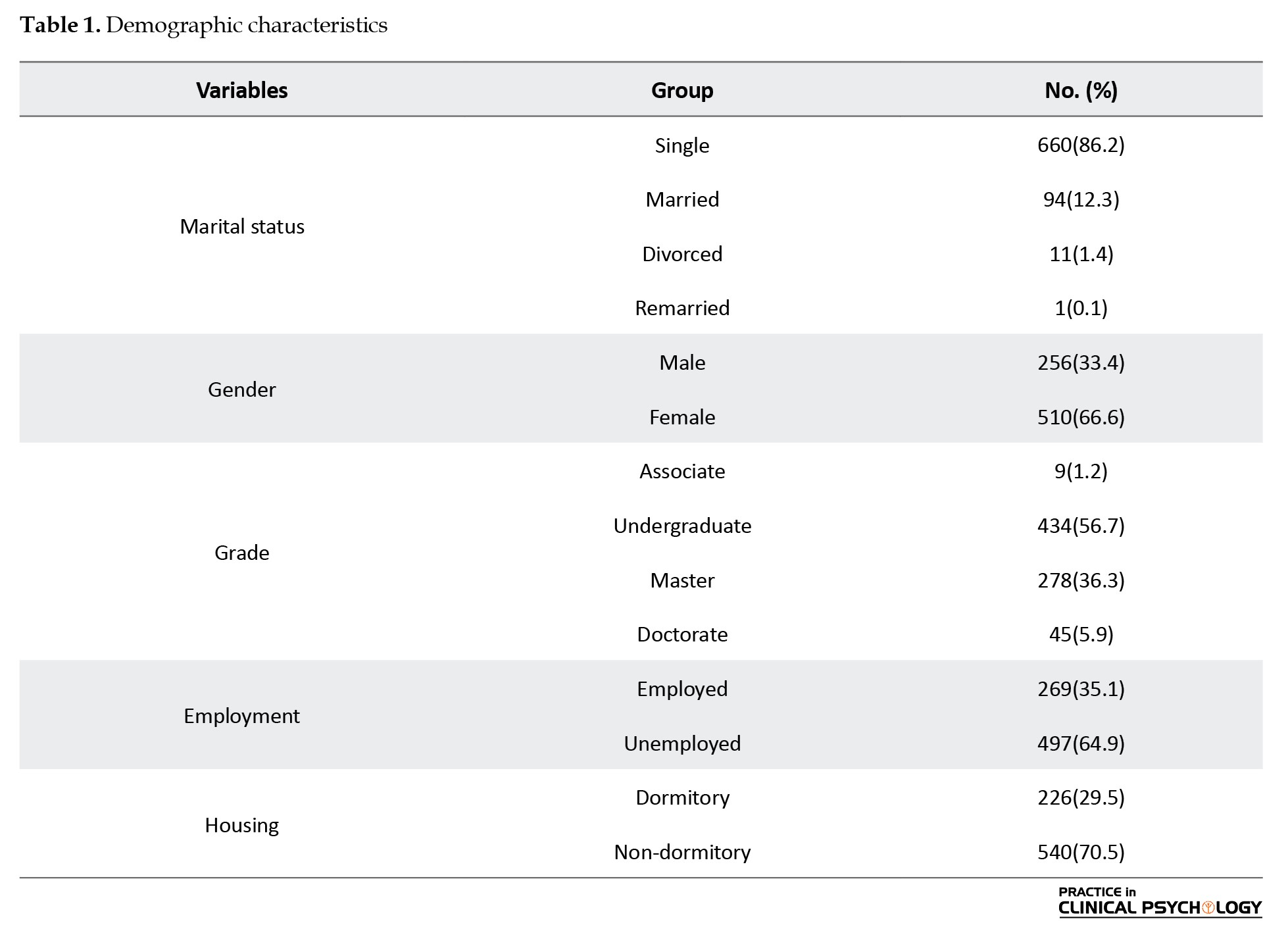
A total of 766 university students from Tehran participated in the study, of whom 510(66.6%) were women and 256(33.4%) were men. The participants were between 18 and 70 years old (Mean±SD 24.89±7.02). The education levels were 1.2%, 56.7%, 36.3%, and 5.9% for associate degrees, undergraduate, master’s, and doctoral programs, respectively. Most participants were single (86.2%), and 12.3% were married. The employment ratio was 35.1% versus 64.9% unemployed. Regarding residence, 29.5% of the respondents lived in boarding hostels, whereas 70.5% lived off-campus (Table 1).
Descriptive statistics and correlations
Descriptive statistics showed that all the variables had good normality (1 skewness and kurtosis ranged between -2 and +2). Significant positive relationships found by Pearson correlations (Table 2) existed between:
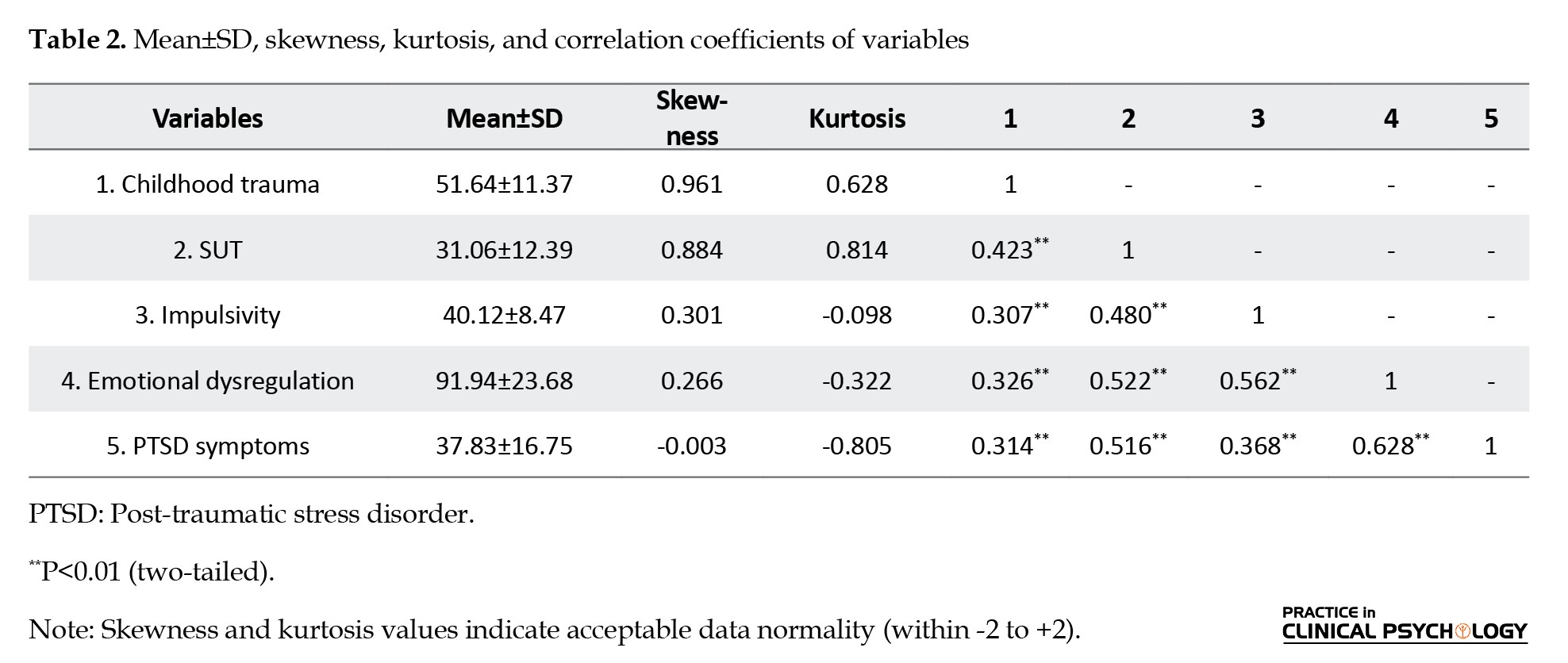
Childhood trauma and SUT (r=0.423), emotional dysregulation and SUT (r=0.522), PTSD symptoms and SUT (r=0.516), and impulsivity and SUT (r=0.480).
To further confirm childhood trauma, PTSD symptoms (r=0.314), emotional dysregulation (r=0.326), and impulsivity (r=0.307) were also positively correlated.
Measurement model
The majority of factor loadings were acceptable, except for non-acceptance, which was part of the DERS, since the factor loading was low (<0.30) to enhance the model’s validity. The critical standardized loadings involved are as follows:
Emotional dysregulation: Strategies (β=0.910, t=24.967), non-acceptance (β=0.739, t=not reported), clarity (β=0.486, t=13.070), goals (β=0.796, t=21.949), and impulse (β=0.835, t=23.079); PTSD symptoms: Negative alterations in cognitions and mood (β=0.881, t=29.130), hyperarousal (β=0.857, t=not reported), and intrusions (β=0.766, t=24.335); childhood trauma: Emotional abuse (β=0.800, t=19.214), sexual abuse (β=0.333, t=8.448), physical neglect (β=0.707, t=not reported), emotional neglect (β=0.789, t=19.027), and physical abuse (β=0.565, t=14.116); SUT: Passive and active tendencies (β=0.760, t=9.419 and β=0.365, t=not reported).
Structural equation modeling (SEM)
The expanded SEM model with cross errors showed good model fit indices (CFI=0.947, RMSEA=0.072, SRMR=0.047; Table 3), and the model seems to be a good representation of the correlates among childhood trauma, emotional dysregulation, impulsivity, PTSD symptoms, and the tendency to abuse substances.
Direct effects
Table 4 presents direct effects from the SEM analysis. All paths were statistically significant (P<0.05):
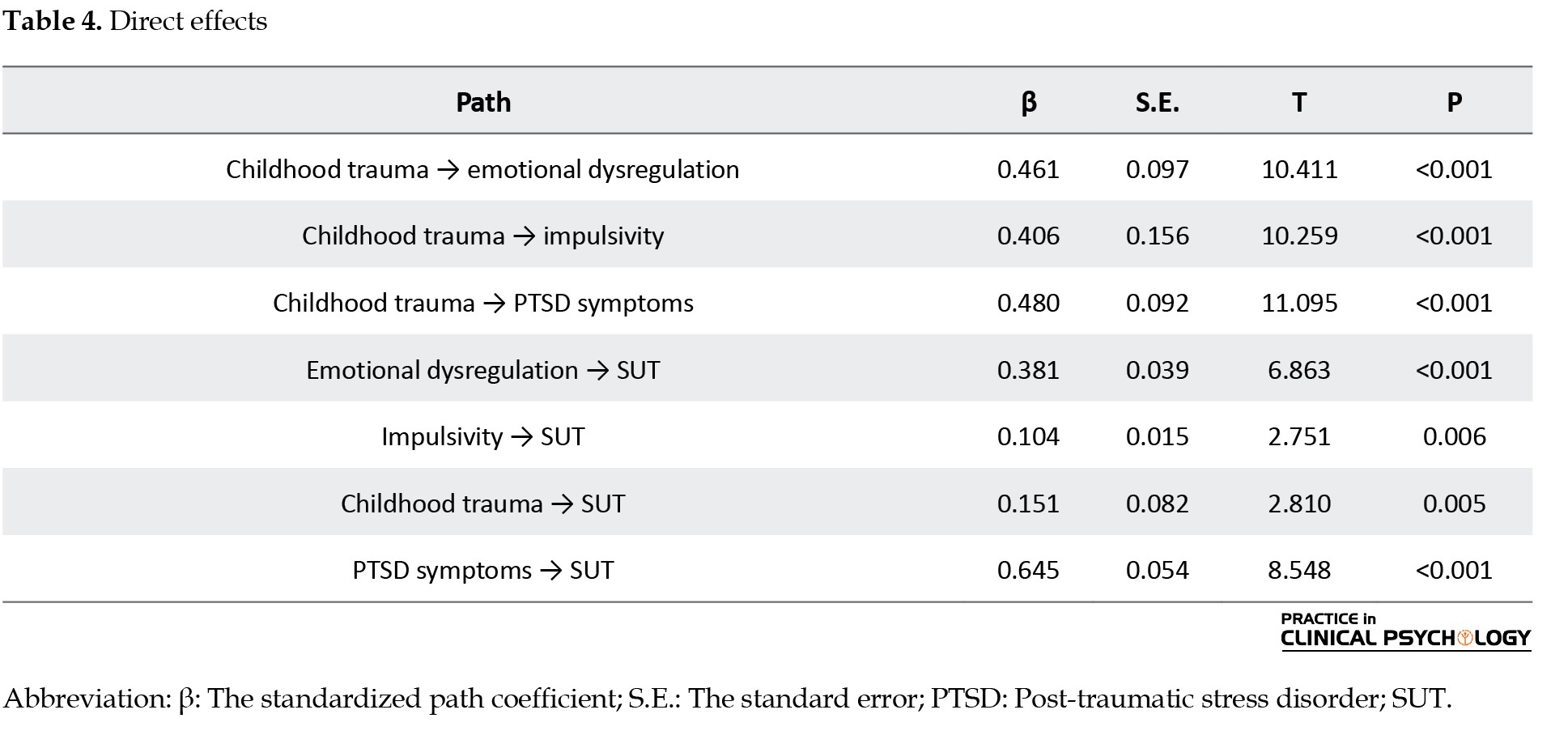
• Childhood trauma to SUT: (β=0.151, SE=0.082, t=2.810, P=0.005)
• Emotional dysregulation to SUT: (β=0.381, SE=0.039, t=6.863, P<0.001)
• Impulsivity to SUT: (β=0.104, SE=0.015, t=2.751, P=0.006)
• PTSD symptoms to SUT: (β=0.645, SE=0.054, t=8.548, P<0.001)
• Childhood trauma to mediators: Emotional dysregulation (β=0.461, SE=0.097, t=10.411, P<0.001), impulsivity (β=0.406, SE=0.156, t=10.259, P<0.001), and PTSD symptoms (β=0.480, SE=0.092, t=11.095, P<0.001).
Summary of results
Overall, the findings suggest that childhood trauma is directly and indirectly (via emotional dysregulation, impulsivity, and PTSD symptoms) related to substance use tendency among Tehran University students. The direct effect of the PTSD symptoms on substance use risk was ranked highest. These facts support the fact that psychological interventions that target the implications of childhood trauma are essential in assisting in substance use vulnerability in this group.
Discussion
The present research will enhance the existing body of knowledge supporting the direct and indirect impacts of childhood trauma on the substance consumption propensity of Iranian university students by examining the mediating variables of emotional dysregulation, impulsivity, and PTSD symptoms. With the help of multi-mediator SEM, its findings support the complexity of psychological mechanisms that connect trauma with maladaptive substance-related outcomes in a distinct sociocultural setting.
Interpretation of findings
As previously stated, the findings sustain a strong direct connection between childhood trauma and trends in substance use (β=0.151, P=0.005) (Odac, 2021; Akcan, 2021). Significant positive correlations between all subdimensions of childhood trauma (physical neglect, emotional abuse, physical abuse, sexual abuse and emotional neglect) and SUT (r=0.423, P<0.01) also confirmed the idea that early childhood traumatic experiences continue to affect psychological functioning and poor coping behaviors that lead to substance abuse (Odacı et al., 2021). Nevertheless, Wang et al. (2020) showed that infancy or prenatal trauma is not significantly correlated with adult male alcohol use disorders, focusing on the timeline of the traumatic event concerning its moderation. The existing disparity demonstrates the necessity of considering the age point of the trauma, as early childhood trauma can have a more significant impact on SUT.
The mediating effects of emotion regulation, impulsivity, and PTSD symptoms were also confirmed. The direct impact of emotional dysregulation on SUT was significant (β=0.381, P<0.001), which concurs with the traumatic childhood findings that poor emotional regulation is a mediator of the relationship between childhood trauma and substance use (Koçak & Cagatay, 2024; Schaefer et al., 2021; Barahmand et al., 2016). Similarly, the relationship between trauma and substance use was mediated by impulsivity (β=0.104, P=0.006), which is in line with the results of studies that mark impulsivity as a neurocognitive mechanism between childhood adversity and substance use (Morris et al., 2020; Hosking & Winstanley, 2011; Brown et al., 2022). The significance of the mediating effect of PTSD symptoms was also found to be the highest (β=0.645, P<0.001), making the self-medication hypothesis, according to which individuals use substances to get rid of the distress caused by traumatic experiences, accurate (Rosenkranz et al., 2014; Patock-Peckham et al., 2020; Park et al., 2019; Hannan et al., 2017).
Comparison with existing literature
The results extrapolate prior studies by combining various mediators (emotional dysregulation, impulsivity, and PTSD symptoms) in one model in a non-psychiatric, culturally high population. This study also shows the importance of these mediators in a non-clinical sample of Iranian students, who, due to cultural circumstances (such as stigma and emotional suppression), might have stronger psychological vulnerabilities (Farnia et al., 2018) than those reported by Wang et al. (2020). This clinical sample that is specific to the types of trauma in addition to characteristics of clinical groups. The high correlation between the presence of emotional dysregulation and substance use found (r=0.522, P<0.01) agrees with what Mandavia et al. (2016) established in their research: emotional dysregulation is an intermediary in the interplay between childhood emotional abuse and lifelong substance use. Similarly, Ramakrishnan et al. (2019) found that positive urgency is an essential dimension between childhood maltreatment and substance use, supporting the mediating performance of impulsivity.
Usually, the presence of PTSD symptoms has a strong mediating impact, confirming previous studies that trauma-induced symptoms are the leading elements in developing substance use as a coping tool (Park et al., 2019; Hannan et al., 2017). This is particularly timely in Iran, where few people can seek mental health assistance, and cultural stigma can exacerbate dependence on substances to address PTSD symptoms (Skidmore et al., 2016).
Conclusion
However, this investigation supports both direct and indirect associations between childhood trauma and SUT among Iranian university students, such as the effects of emotional dysregulation, impulsivity, and PTSD symptoms on SUT. These results move towards understanding the psychological mechanisms that connect an early experience of trauma to substance use and the necessity of guiding interventions that operate on these mediators. Considering emotional dysregulation, impulsivity, and the manifestations of PTSD, especially when implemented in culturally considerate circumstances, prevention and treatment programs can decrease the risks of substance usage and enhance the mental health of survivors of trauma.
Limitations
Despite these contributions, this study has several limitations. The cross-sectional design does not allow for concluding causality and the time sequence. Self-report measures, at least where stigmatized behaviors and experiences are involved, carry the possibility of a recall or social desirability bias that can lead to incorrect downplaying of associations. The sample was national, and only students in Tehran were used; there is low generalizability to other communities in Iran, especially those living in less urban or exposed and less privileged areas. Besides, due to the exclusion of non-trauma diagnoses (anxiety, depression, or other comorbid conditions), other potentially relevant pathways associated with trauma and substance use may have been missed.
Unique contributions
To the best of our knowledge, no research has ever examined such mediating factors of emotional dysregulation, impulsivity, and PTSD symptoms in both dimensions of assessing the trauma and substance use pathway, and the same research on such aspects has never been undertaken, among a large sample of university students in a non-clinical population in Iran. Combining these elements into a single model and placing the study within a non-Western location allows for the addressing of vital gaps in the literature and the bringing forth of cultural specifics that can encourage the development of prevention and intervention strategies.
Direction for future research and recommendations
These conclusions are significant to prevention and intervention. The low to moderate but still significant mediating effects of emotional dysregulation, impulsivity, and PTSD symptoms potentially indicate that policies and strategies to promote substance use risk prevention among survivors of trauma may be implemented. For example, cognitive-behavior therapies aimed at emotional control and impulse control, and trauma-based therapies for PTSD can prove to be especially efficient. Cultural interventions, which would be able to respond to stigma and low access to mental health services, are essential in the Iranian case.
Future research on this topic should use longitudinal designs to demystify causal processes. The study should be replicated among non-student populations and rural groups to increase generalizability. Self-report biases may be decreased by including objective measures, such as clinical interviews or archival records. Also, the analysis of other mental health measures, including mood or anxiety disorders, would provide a more detailed picture of how trauma is connected to drug use.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Review Board of Kharazmi University, Tehran, Iran (Code: (IR.KHU.REC.1403.149). Participants were assured confidentiality.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: All authors; Supervision: Shahram Mohammadkhani and Robabeh Noury; Methodology, investigation, data collection and analysis: Mohammad Hossein Abdolloahi; Writing: Mohammad Hossein Abdolloahi, Shahram Mohammadkhani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all participants in this study.
References
Akcan, G., Öztürk, E., & Erdoğan, B. (2021). The investigation of the mediating role of coping strategies on the relationship between childhood traumas, depression, and alcohol use disorder in university students. Journal of Substance Abuse Treatment, 123, 108305. [DOI:10.1016/j.jsat.2021.108305] [PMID]
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association. [DOI:10.1176/appi.books.9780890425596]
Amin-Esmaeili, M., Rahimi-Movaghar, A., Sharifi, V., Hajebi, A., Radgoodarzi, R., & Mojtabai, R., et al. (2016). Epidemiology of illicit drug use disorders in Iran: Prevalence, correlates, comorbidity and service utilization results from the Iranian mental health survey. Addiction (Abingdon, England), 111(10), 1836–1847. [DOI:10.1111/add.13453] [PMID]
Andersen, S. L., & Teicher, M. H. (2009). Desperately driven and no brakes: Developmental stress exposure and subsequent risk for substance abuse. Neuroscience & Biobehavioral Reviews, 33(4), 516-524. [DOI:10.1016/j.neubiorev.2008.09.009] [PMID]
Banducci, A. N., Hoffman, E. M., Lejuez, C. W., & Koenen, K. C. (2014). The impact of childhood abuse on inpatient substance users: Specific links with risky sex, aggression, and emotion dysregulation. Child Abuse & Neglect, 38(5), 928–938.[DOI:10.1016/j.chiabu.2013.12.007] [PMID]
Barahmand, U., Khazaee, A., & Hashjin, G. S. (2016). Emotion dysregulation mediates between childhood emotional abuse and motives for substance use. Archives of Psychiatric Nursing, 30(6), 653-659. [DOI:10.1016/j.apnu.2016.02.007] [PMID]
Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., & Ahluvalia, T., et al. (2003). Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse & Neglect, 27(2), 169-190. [DOI:10.1016/S0145-2134(02)00541-0] [PMID]
Braquehais, M. D., Oquendo, M. A., Baca-García, E., & Sher, L. (2010). Is impulsivity a link between childhood abuse and suicide?. Comprehensive Psychiatry, 51(2), 121–129. [DOI:10.1016/j.comppsych.2009.05.003] [PMID]
Brown, S., Fite, P. J., & Bortolato, M. (2022). The mediating role of impulsivity in the associations between child maltreatment types and past-month substance use. Child Abuse & Neglect, 128, 105591. [DOI:10.1016/j.chiabu.2022.105591] [PMID]
Cyders, M. A., Littlefield, A. K., Coffey, S., & Karyadi, K. A. (2014). Examination of a short English version of the UPPS-P impulsive behavior scale. Addictive Behaviors, 39(9), 1372-1376. [DOI:10.1016/j.addbeh.2014.02.013] [PMID]
Farnia, V., Mousavi, S. B., Tatari, F., Salemi, S., Golshani, S., & Alikhani, M., et al. (2018). Prevalence of childhood attention-deficit/hyperactivity disorder (ADHD) in methamphetamine dependence: A descriptive study. Iranian Journal of Psychiatry and Behavioral Sciences, 12(4), e61329. [DOI:10.5812/ijpbs.61329]
Garrusi, B., & Nakhaee, N. (2009). Validity and reliability of a Persian version of the childhood trauma questionnaire. Psychological Reports, 104(2), 509-516. [DOI:10.2466/PR0.104.2.509-516] [PMID]
Gratz, K. L., & Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41-54. [DOI:10.1023/B:JOBA.0000007455.08539.94]
Hannan, S. M., Orcutt, H. K., Miron, L. R., & Thompson, K. L. (2017). Childhood sexual abuse and later alcohol-related problems: Investigating the roles of revictimization, PTSD, and drinking motivations among college women. Journal of Interpersonal Violence, 32(14), 2118-2138. [DOI:10.1177/0886260515591276] [PMID]
Hosking, J., & Winstanley, C. A. (2011). Impulsivity as a mediating mechanism between early-life adversity and addiction: Theoretical comment on Lovic et al. (2011). Behavioral Neuroscience, 125(5), 681-686. [DOI:10.1037/a0024612] [PMID]
Jebraeili, H., Moradi, A., & Habibi, M. (2019). Psychometric properties of the Persian short version of the five-factor impulsive behavior scale. Journal of Research and Health, 9(6), 516-524. [DOI:10.32598/jrh.9.6.516]
Keyes, K. M., Shmulewitz, D., Greenstein, E., McLaughlin, K., Wall, M., & Aharonovich, E., et al. (2014). Exposure to the Lebanon war of 2006 and effects on alcohol use disorders: The moderating role of childhood maltreatment. Drug and Alcohol Dependence, 134, 296–303. [DOI:10.1016/j.drugalcdep.2013.10.014] [PMID]
Khantzian, E. J. (1997). The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry, 4(5), 231-244. [DOI:10.3109/10673229709030550] [PMID]
Khanzadeh, M., Saeediyan, M., Hosseinchari, M., & Edrissi, F. (2012). [Factor structure and psychometric properties of the difficulties in emotional regulation scale (Persian)]. International Journal of Behavioral Sciences, 6(1), 87-96. [Link]
Kiburi, S. K., Molebatsi, K., Obondo, A., & Kuria, M. W. (2018). Adverse childhood experiences among patients with substance use disorders at a referral psychiatric hospital in Kenya. BMC Psychiatry, 18(1), 197. [DOI:10.1186/s12888-018-1780-1] [PMID]
Kline, R. B. (2010). Principles and practice of structural equation modeling. New York, NY: The Guilford Press. [Link]
Koçak, Z., & Çağatay, S. E. (2024). Childhood traumas and emotional eating: The mediating role of self-esteem and emotion dysregulation. Current Psychology, 43, 21783–21791. [DOI:10.1007/s12144-024-05953-2]
Lawson, K. M., Back, S. E., Hartwell, K. J., Maria, M. M., & Brady, K. T. (2013). A comparison of trauma profiles among individuals with prescription opioid, nicotine, or cocaine dependence. The American Journal on Addictions, 22(2), 127-131. [DOI:10.1111/j.1521-0391.2013.00319.x] [PMID]
Lovallo, W. R. (2013). Early life adversity reduces stress reactivity and enhances impulsive behavior: Implications for health behaviors. International Journal of Psychophysiology, 90(1), 8-16. [DOI:10.1016/j.ijpsycho.2012.10.006] [PMID]
Mandavia, A., Robinson, G. G., Bradley, B., Ressler, K. J., & Powers, A. (2016). Exposure to childhood abuse and later substance use: Indirect effects of emotion dysregulation and exposure to trauma. Journal of Traumatic Stress, 29(5), 422-429. [DOI:10.1002/jts.22131] [PMID]
Morris, V. L., Huffman, L. G., Naish, K. R., Holshausen, K., Oshri, A., McKinnon, M., & Amlung, M. (2020). Impulsivity as a mediating factor in the association between posttraumatic stress disorder symptoms and substance use. Psychological Trauma: Theory, Research, Practice and Policy, 12(6), 659–668. [DOI:10.1037/tra0000588] [PMID]
Odacı, H., Bülbül, K., & Türkkan, T. (2021). The mediating role of cognitive flexibility in the relationship between traumatic experiences in the childhood period and substance abuse proclivity. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 39(4), 538-554. [DOI:10.1007/s10942-020-00385-w]
Park, T., Thompson, K., Wekerle, C., Al‐Hamdani, M., Smith, S., & Hudson, A., et al. (2019). Posttraumatic stress symptoms and coping motives mediate the association between childhood maltreatment and alcohol problems. Journal of Traumatic Stress, 32(6), 918-926. [DOI:10.1002/jts.22467] [PMID]
Patock-Peckham, J. A., Belton, D. A., D’Ardenne, K., Tein, J. Y., Bauman, D. C., & Infurna, F. J., et al. (2020). Dimensions of childhood trauma and their direct and indirect links to PTSD, impaired control over drinking, and alcohol-related problems. Addictive Behaviors Reports, 12, 100304. [DOI:10.1016/j.abrep.2020.100304] [PMID]
Ramakrishnan, N., McPhee, M., Sosnowski, A., Rajasingaam, V., & Erb, S. (2019). Positive urgency partially mediates the relationship between childhood adversity and problems associated with substance use in an undergraduate population. Addictive Behaviors Reports, 10, 100230. [DOI:10.1016/j.abrep.2019.100230] [PMID]
Rezahosseini, O., Roohbakhsh, A., Tavakolian, V., & Assar, S. (2014). Drug abuse among university students of Rafsanjan, Iran. Iranian Journal of Psychiatry and Behavioral Sciences, 8(2), 81-85. [Link]
Rosenkranz, S. E., Muller, R. T., & Henderson, J. L. (2014). The role of complex PTSD in mediating childhood maltreatment and substance abuse severity among youth seeking substance abuse treatment. Psychological Trauma: Theory, Research, Practice, and Policy, 6(1), 25-33. [DOI:10.1037/a0031920]
Sadeghi, M., Taghva, A., Goudarzi, N., & Rah Nejat, A. M. (2016). Validity and reliability of the Persian version of “post-traumatic stress disorder scale” in war veterans. Iranian Journal of War and Public Health, 8(4), 243-249. [Link]
Schaefer, L. M., Hazzard, V. M., Smith, K. E., Johnson, C. A., Cao, L., & Crosby, R. D., et al. (2021). Examining the roles of emotion dysregulation and impulsivity in the relationship between psychological trauma and substance abuse among women with bulimic-spectrum pathology. Eating Disorders, 29(3), 276–291. [DOI:10.1080/10640266.2021.1891370] [PMID]
Shin, S. H., Lee, S., Jeon, S. M., & Wills, T. A. (2015). Childhood emotional abuse, negative emotion-driven impulsivity, and alcohol use in young adulthood. Child Abuse & Neglect, 50, 94-103. [DOI:10.1016/j.chiabu.2015.02.010] [PMID]
Skidmore, C. R., Kaufman, E. A., & Crowell, S. E. (2016). Substance use among college students. Child and Adolescent Psychiatric Clinics of North America, 25(4), 735-753. [DOI:10.1016/j.chc.2016.06.004] [PMID]
Unicef. (2024). Nearly 400 million young children worldwide regularly experience violent discipline at home. New York: Unicef. [Link]
Wang, L., An, C. X., Song, M., Li, N., Gao, Y. Y., & Zhao, X. C., et al. (2020). Evaluation of childhood traumatic experience as a risk factor for alcohol use disorder in adulthood. BMC Psychiatry, 20(1), 15. [DOI:10.1186/s12888-020-2428-5] [PMID]
Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2014). PTSD checklist for DSM-5 (PCL-5). Cleveland: National Center for PTSD. [Link]
Weed, N. C., Butcher, J. N., McKenna, T., & Ben-Porath, Y. S. (1992). New measures for assessing alcohol and drug abuse with the MMPI-2: The APS and AAS. Journal of Personality Assessment, 58(2), 389–404. [DOI:10.1207/s15327752jpa5802_15] [PMID]
Weiss, N. H., Tull, M. T., Lavender, J., & Gratz, K. L. (2013). Role of emotion dysregulation in the relationship between childhood abuse and probable PTSD in a sample of substance abusers. Child Abuse & Neglect, 37(11), 944–954. [DOI:10.1016/j.chiabu.2013.03.014] [PMID]
Weiss, N. H., Tull, M. T., Viana, A. G., Anestis, M. D., & Gratz, K. L. (2012). Impulsive behaviors as an emotion regulation strategy: Examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders, 26(3), 453–458.[DOI:10.1016/j.janxdis.2012.01.007] [PMID]
White, H. R., & Widom, C. S. (2008). Three potential mediators of the effects of child abuse and neglect on adulthood substance use among women. Journal of Studies on Alcohol and Drugs, 69(3), 337-347. [DOI:10.15288/jsad.2008.69.337] [PMID]
WHO. (2018). Child maltreatment. Geneva: World Health Organization. [Link]
Zargar, Y., Najarian, B., & Naami, A. Z. (2008). [The relationship of some personality variables, religious attitudes, and marital satisfaction with addiction potential in personnel of an industrial factory in Ahvaz (Persian)]. Journal Of Education And Psychology, 15(1), 99-120. [Link]
Full-Text: (215 Views)
Introduction
Substance use is a significant deterrent to the health of the Iranian population because it has more than a million cases among citizens aged 15-64 years (Amin-Esmaeili et al., 2016). University students are one of the vulnerable groups since they have to endure both academic and social stress, and according to the latest surveys, the prevalence of substance use during the last month is reported to be within the range of 0.3-0.9 percent (Rezahosseini et al., 2014). The collectivist nature of Iranian society and the high level of stigma and criminal punishment associated with substance use prevent disclosure and asking people to help, which increases the dangers of lack of treatment in the case of problematic behaviors (Skidmore et al., 2016).
Physical, emotional, and sexual abuse or neglect, known as childhood trauma, are well-established risk factors internationally that lead to substance use later in life (WHO, 2018). About 60 percent of all children below the age of 5, totaling 400 million children, are often physically punished and/or psychologically abused by their parents and caregivers (UNICEF, 2024). Iran is a country where family and social constraints can regularly bottle up the denunciation of an abuse that multiplies the psychological impacts that are not dealt with (Andersen & Teicher, 2009). Adverse childhood experiences (ACEs) were repeatedly associated with elevated substance use in adulthood, although certain traumas (e.g. exposure to war) have shown a dramatic increase in risk (Kiburi et al., 2018; Lawson et al., 2013; Lovallo, 2013; Keyes et al., 2014).
Nonetheless, most studies have been conducted on clinical or substance-using populations, usually in a Western setting, and a major gap remains in non-clinically, culturally dissimilar populations, such as Iranian university students (Skidmore et al., 2016). Moreover, despite the necessity to focus on each psychological mediator individually, such as impulsivity, emotional dysregulation, and post-traumatic stress disorder (PTSD) symptoms, there are very few studies evaluating how these psychological mediators interact in the trauma substance use pathway, even in Iranian samples (Banducci et al., 2014; Weiss et al., 2012; Weiss et al., 2013; Shin et al., 2015; Farnia et al., 2018).
Each of the symptoms of impulsivity, emotional dysregulation, and PTSD could be evaluated as the ways through which childhood trauma predisposes to substance use. Neurocognitive development can be impaired by childhood trauma, which increases impulsivity (Braquehais et al., 2010; Cyders et al., 2014). Another crucial mediator, emotional dysregulation (conceptualization of having issues with handling emotional reactions), also applies. It involves difficulties in emotional recognition, acceptance, and regulation (Gratz & Roemer, 2004). The dysregulation of emotions or the inability to control emotional reactions is especially topical in Iran, where the cultural principles of emotional suppression are supported (Farnia et al., 2018). Both trauma exposure and subsequent substance use are associated with PTSD symptoms, such as re-experiencing, avoidance, and hyperarousal, which may be due to self-medication (Khantzian, 1997; White & Widom, 2008; APA, 2013).
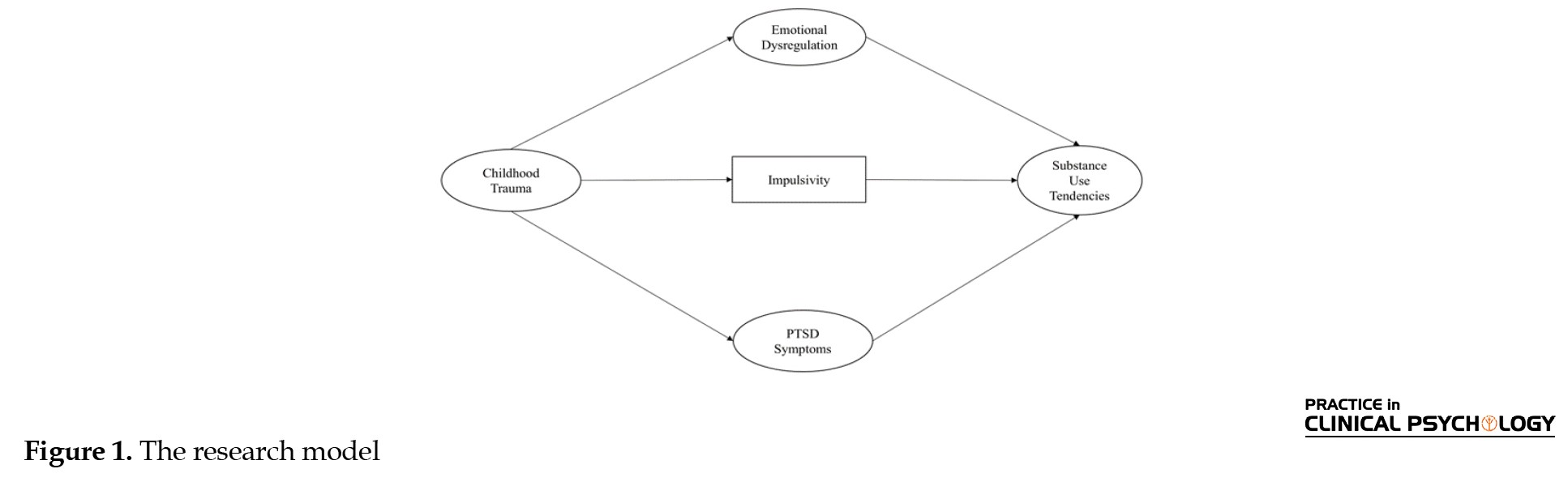
Thus, this study fills a considerable research gap by simultaneously exploring the mediating influence of impulsivity, emotional dysregulation, and symptoms of posttraumatic stress disorder on the relationship between childhood trauma and substance use in Iranian university students, a non-clinical population exposed to specific cultural and academic stressors. Through structural equation modeling (SEM), this study will help describe the direct and indirect paths and provide valuable information for identifying and early intervention in young people regarding culture-specific measures (Kline, 2010). The proposed theoretical model is shown in Figure 1.
Substance use is a significant deterrent to the health of the Iranian population because it has more than a million cases among citizens aged 15-64 years (Amin-Esmaeili et al., 2016). University students are one of the vulnerable groups since they have to endure both academic and social stress, and according to the latest surveys, the prevalence of substance use during the last month is reported to be within the range of 0.3-0.9 percent (Rezahosseini et al., 2014). The collectivist nature of Iranian society and the high level of stigma and criminal punishment associated with substance use prevent disclosure and asking people to help, which increases the dangers of lack of treatment in the case of problematic behaviors (Skidmore et al., 2016).
Physical, emotional, and sexual abuse or neglect, known as childhood trauma, are well-established risk factors internationally that lead to substance use later in life (WHO, 2018). About 60 percent of all children below the age of 5, totaling 400 million children, are often physically punished and/or psychologically abused by their parents and caregivers (UNICEF, 2024). Iran is a country where family and social constraints can regularly bottle up the denunciation of an abuse that multiplies the psychological impacts that are not dealt with (Andersen & Teicher, 2009). Adverse childhood experiences (ACEs) were repeatedly associated with elevated substance use in adulthood, although certain traumas (e.g. exposure to war) have shown a dramatic increase in risk (Kiburi et al., 2018; Lawson et al., 2013; Lovallo, 2013; Keyes et al., 2014).
Nonetheless, most studies have been conducted on clinical or substance-using populations, usually in a Western setting, and a major gap remains in non-clinically, culturally dissimilar populations, such as Iranian university students (Skidmore et al., 2016). Moreover, despite the necessity to focus on each psychological mediator individually, such as impulsivity, emotional dysregulation, and post-traumatic stress disorder (PTSD) symptoms, there are very few studies evaluating how these psychological mediators interact in the trauma substance use pathway, even in Iranian samples (Banducci et al., 2014; Weiss et al., 2012; Weiss et al., 2013; Shin et al., 2015; Farnia et al., 2018).
Each of the symptoms of impulsivity, emotional dysregulation, and PTSD could be evaluated as the ways through which childhood trauma predisposes to substance use. Neurocognitive development can be impaired by childhood trauma, which increases impulsivity (Braquehais et al., 2010; Cyders et al., 2014). Another crucial mediator, emotional dysregulation (conceptualization of having issues with handling emotional reactions), also applies. It involves difficulties in emotional recognition, acceptance, and regulation (Gratz & Roemer, 2004). The dysregulation of emotions or the inability to control emotional reactions is especially topical in Iran, where the cultural principles of emotional suppression are supported (Farnia et al., 2018). Both trauma exposure and subsequent substance use are associated with PTSD symptoms, such as re-experiencing, avoidance, and hyperarousal, which may be due to self-medication (Khantzian, 1997; White & Widom, 2008; APA, 2013).
Thus, this study fills a considerable research gap by simultaneously exploring the mediating influence of impulsivity, emotional dysregulation, and symptoms of posttraumatic stress disorder on the relationship between childhood trauma and substance use in Iranian university students, a non-clinical population exposed to specific cultural and academic stressors. Through structural equation modeling (SEM), this study will help describe the direct and indirect paths and provide valuable information for identifying and early intervention in young people regarding culture-specific measures (Kline, 2010). The proposed theoretical model is shown in Figure 1.
Materials and Methods
Following recommendations for SEM (Kline, 2010), 815 students from universities in Tehran were initially recruited using non-random sampling. The inclusion criteria included enrollment at a Tehran university between 18 and 70 years old. The exclusion criteria involved incomplete or inconsistent survey responses. Even though the age range in our sample was broad (18-70 years) with a Mean±SD age of 24.89±7.02, we also did not employ stratification or classification analysis based on age because of the sample size and main research focus. Since age can be a factor affecting the variables under analysis, this is one of the limitations of our study. Future research should also consider a more stratified analysis or another detailed age-based control to establish the possible moderating impact of age on the association between childhood trauma, psychological mediators, and substance use.
Procedures
This descriptive-correlational study used an online survey hosted on the Porsline platform, distributed through Telegram channels popular among Tehran University students. Convenience sampling through Telegram channels was utilized because of inaccessibility and resource constraints. This can restrict the generalizability of the results to all students at Tehran University. Future studies should establish methods for probabilistic sampling to be more representative. Participation was voluntary, with no incentives provided, and participants could withdraw at any time. The survey, taking approximately 35 minutes to complete, included measures of childhood trauma, substance use tendencies (SUT), impulsivity, emotional dysregulation, and PTSD symptoms.
Measures
Addiction potential scale
The addiction potential scale (APS) evaluates the tendency to use substances in an individual using 41 questions, five of which are lie scales. The scoring scale is a 4-point Likert scale (0=strongly disagree, 3=strongly agree) (Weed et al., 1992). It was adapted to Iran by Zargar et al. (2008), containing active and passive tendency subscales with a score range of 0-108. The scale’s construct validity was established using a correlation coefficient of 0.45 and the Symptom Checklist-25 (SCL-25) (Zargar et al., 2008). In this study, Cronbach’s α was 0.84, indicating good reliability.
Childhood trauma questionnaire-short form (CTQ-SF)
The CTQ-SF is a 28-item self-report measure to measure five types of child abuse: Emotional neglect, emotional abuse, sexual abuse, physical neglect, and physical abuse (Bernstein et al., 2003). The scale of measurement involved a Likert scale (5-point scale), where 1 (never true) and 5 (often true). The Persian translation, which has been proven valid by Garrusi and Nakhaee (2009), is quite reliable (Cronbach’s α=0.85 in the present study).
Short form of the UPPS-P impulsive behavior scale (SUPPS-P)
The 20-item SUPPS-P estimates five aspects of impulsivity: Sensation seeking, lack of persistence, lack of reflection, positive urgency, and negative urgency (Cyders et al., 2014). The ratings were on a 4-point scale (1=completely agree, 4=completely disagree). The Persian version, which was validated by Jebraeili et al., 2019, and proved to have good reliability (Cronbach’s α=0.80 in this research).
PTSD checklist (PCL-5)
PCL-5 is a self-report scale, comprising 20 questions, assessing how well the symptoms of PTSD are authenticated by the diagnostic and statistical manual of mental disorders, fifth edition (DSM-5) rules, and evaluated on a 5-point Likert scale (0=not at all, 4=excessively) (Weathers et al., 2014). The Persian version exhibited a high reliability rate (Cronbach’s α=0.92 in the current study) (Sadeghi et al., 2016).
Difficulties in emotion regulation scale (DERS)
The DERS is a 36-item instrument used to measure six facets of psychometric instruments: non-acceptance, goals, strategies, impulse, awareness, and clarity of emotional dysregulation (Gratz & Roemer, 2004). The grading scale value of items is 5-point Likert (1=rarely, 5=almost always). The Persian version reflected reliability (Cronbach’s α coefficient of 0.93 in the current study) (Khanzadeh et al., 2012).
Statistical analysis
SEM was employed to examine direct and indirect relationships among childhood trauma, impulsivity, emotional dysregulation, PTSD symptoms, and SUT. Descriptive statistics were used to summarize the participant characteristics. To examine the assumption of non-collinearity, the variance inflation factor and tolerance index statistics were used. The tolerance index of the variables was in the range of 0.476 to 0.853, and the variance inflation factor was also in the range of 1.173 to 2.102. Given that none of the values related to the tolerance index were less than 0.01 and none of the values related to the variance inflation factor were more than 10, it was possible to be confident about the assumption of non-collinearity. The present study used a frequency table and a box plot to identify univariate outliers for observable variables. When the values of P1 and P2 in the Amos software output are equal to 0.000, it can be concluded that the respondent is a multivariate outlier (Kline, 2010). After identifying univariate outliers, multivariate outliers were not identified due to the favorable state of model fit. The non-acceptance subscale of DERS was excluded due to low factor loading (<0.3). Pearson’s correlation coefficient was used to assess the relationship between the variables. Model fit was evaluated using the root mean square error of approximation (RMSEA) (<0.08), goodness of fit index (GFI), comparative fit index (CFI), Tucker–Lewis index (TLI), incremental fit index (IFI) (≥0.90), standardized root mean square residual (SRMR) (<0.08), and chi-square/degree of freedom (CMIN/DF) (<5) as thresholds for good fit. Analyses were performed using SPSS software, version 27 and Amos software, version 29. The final outcomes of the research model are presented in Figure 2.
Results
Participant characteristics
A total of 766 university students from Tehran participated in the study, of whom 510(66.6%) were women and 256(33.4%) were men. The participants were between 18 and 70 years old (Mean±SD 24.89±7.02). The education levels were 1.2%, 56.7%, 36.3%, and 5.9% for associate degrees, undergraduate, master’s, and doctoral programs, respectively. Most participants were single (86.2%), and 12.3% were married. The employment ratio was 35.1% versus 64.9% unemployed. Regarding residence, 29.5% of the respondents lived in boarding hostels, whereas 70.5% lived off-campus (Table 1).
Descriptive statistics and correlations
Descriptive statistics showed that all the variables had good normality (1 skewness and kurtosis ranged between -2 and +2). Significant positive relationships found by Pearson correlations (Table 2) existed between:
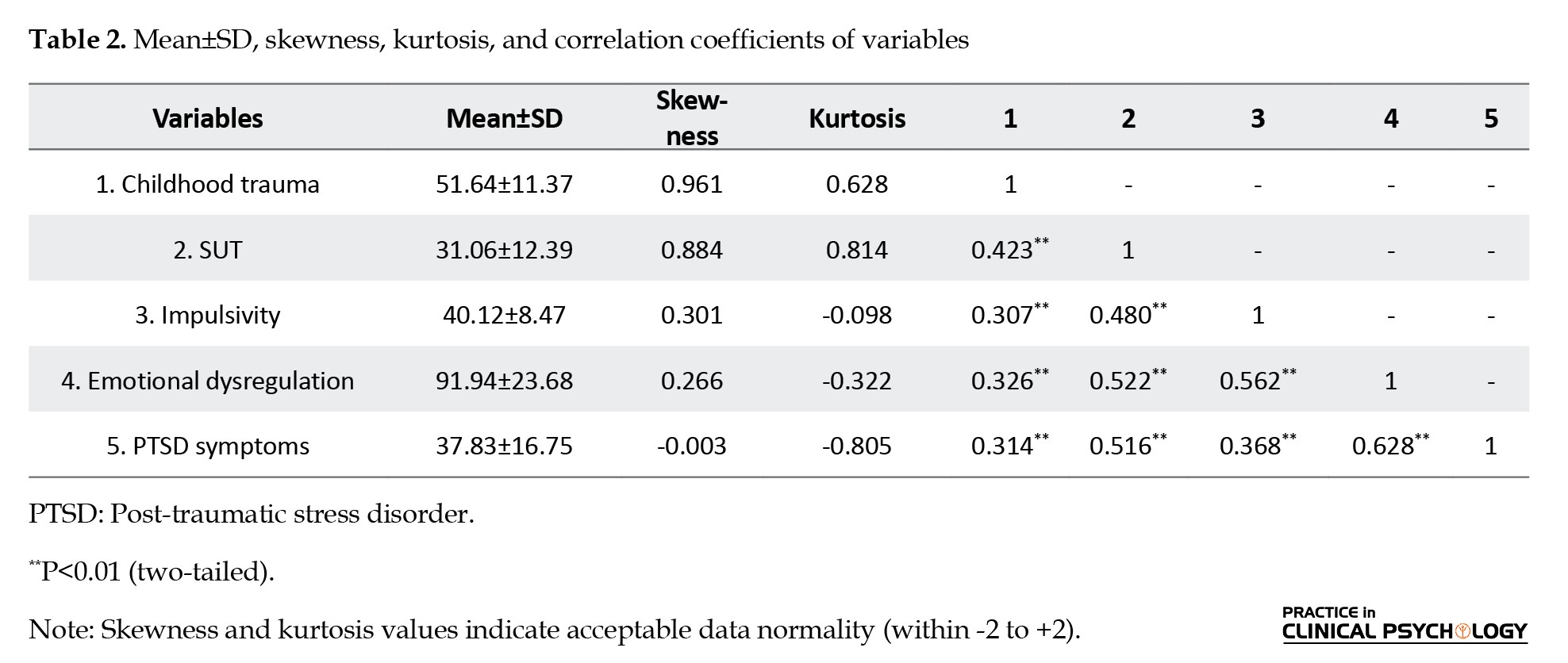
Childhood trauma and SUT (r=0.423), emotional dysregulation and SUT (r=0.522), PTSD symptoms and SUT (r=0.516), and impulsivity and SUT (r=0.480).
To further confirm childhood trauma, PTSD symptoms (r=0.314), emotional dysregulation (r=0.326), and impulsivity (r=0.307) were also positively correlated.
Measurement model
The majority of factor loadings were acceptable, except for non-acceptance, which was part of the DERS, since the factor loading was low (<0.30) to enhance the model’s validity. The critical standardized loadings involved are as follows:
Emotional dysregulation: Strategies (β=0.910, t=24.967), non-acceptance (β=0.739, t=not reported), clarity (β=0.486, t=13.070), goals (β=0.796, t=21.949), and impulse (β=0.835, t=23.079); PTSD symptoms: Negative alterations in cognitions and mood (β=0.881, t=29.130), hyperarousal (β=0.857, t=not reported), and intrusions (β=0.766, t=24.335); childhood trauma: Emotional abuse (β=0.800, t=19.214), sexual abuse (β=0.333, t=8.448), physical neglect (β=0.707, t=not reported), emotional neglect (β=0.789, t=19.027), and physical abuse (β=0.565, t=14.116); SUT: Passive and active tendencies (β=0.760, t=9.419 and β=0.365, t=not reported).
Structural equation modeling (SEM)
The expanded SEM model with cross errors showed good model fit indices (CFI=0.947, RMSEA=0.072, SRMR=0.047; Table 3), and the model seems to be a good representation of the correlates among childhood trauma, emotional dysregulation, impulsivity, PTSD symptoms, and the tendency to abuse substances.
Direct effects
Table 4 presents direct effects from the SEM analysis. All paths were statistically significant (P<0.05):
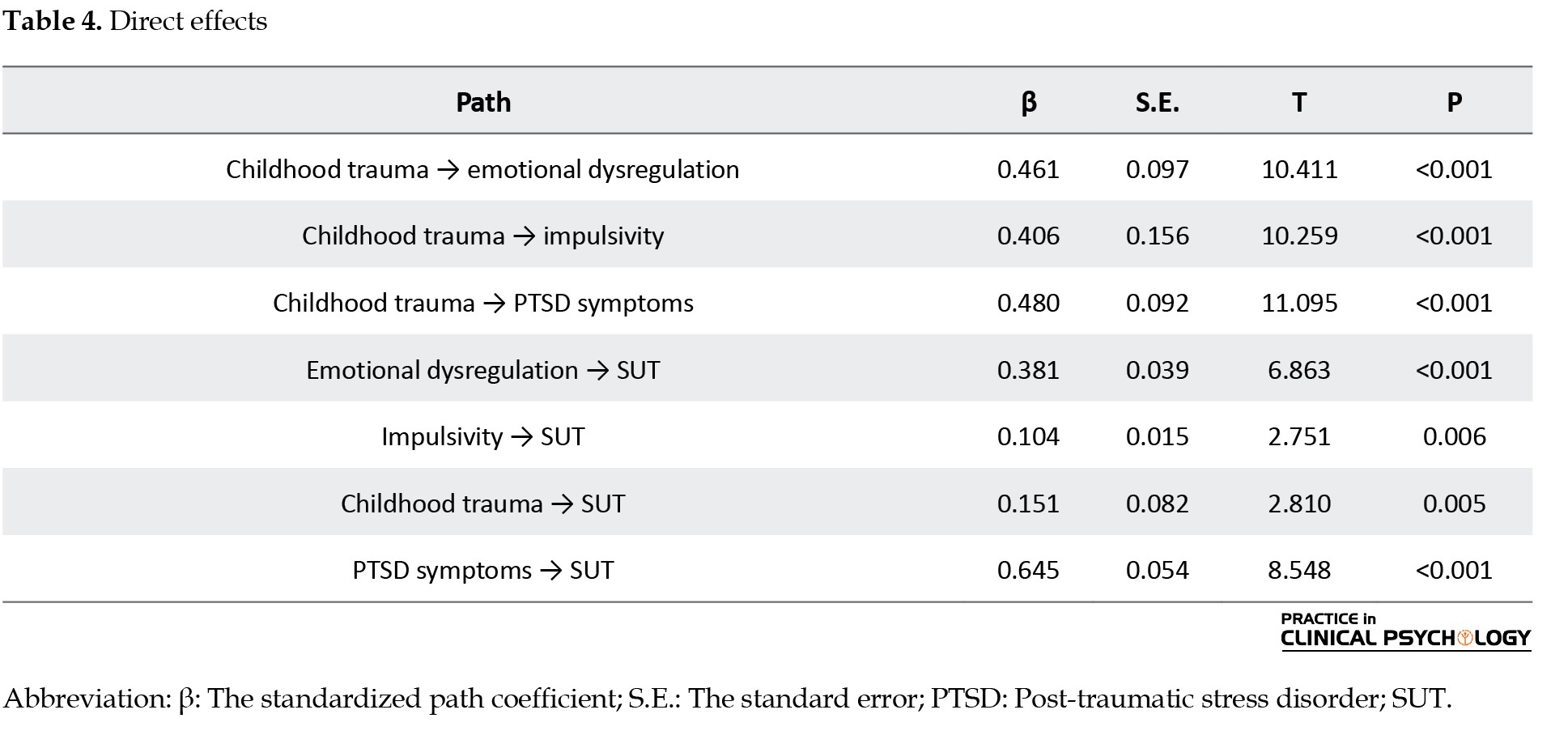
• Childhood trauma to SUT: (β=0.151, SE=0.082, t=2.810, P=0.005)
• Emotional dysregulation to SUT: (β=0.381, SE=0.039, t=6.863, P<0.001)
• Impulsivity to SUT: (β=0.104, SE=0.015, t=2.751, P=0.006)
• PTSD symptoms to SUT: (β=0.645, SE=0.054, t=8.548, P<0.001)
• Childhood trauma to mediators: Emotional dysregulation (β=0.461, SE=0.097, t=10.411, P<0.001), impulsivity (β=0.406, SE=0.156, t=10.259, P<0.001), and PTSD symptoms (β=0.480, SE=0.092, t=11.095, P<0.001).
Summary of results
Overall, the findings suggest that childhood trauma is directly and indirectly (via emotional dysregulation, impulsivity, and PTSD symptoms) related to substance use tendency among Tehran University students. The direct effect of the PTSD symptoms on substance use risk was ranked highest. These facts support the fact that psychological interventions that target the implications of childhood trauma are essential in assisting in substance use vulnerability in this group.
Discussion
The present research will enhance the existing body of knowledge supporting the direct and indirect impacts of childhood trauma on the substance consumption propensity of Iranian university students by examining the mediating variables of emotional dysregulation, impulsivity, and PTSD symptoms. With the help of multi-mediator SEM, its findings support the complexity of psychological mechanisms that connect trauma with maladaptive substance-related outcomes in a distinct sociocultural setting.
Interpretation of findings
As previously stated, the findings sustain a strong direct connection between childhood trauma and trends in substance use (β=0.151, P=0.005) (Odac, 2021; Akcan, 2021). Significant positive correlations between all subdimensions of childhood trauma (physical neglect, emotional abuse, physical abuse, sexual abuse and emotional neglect) and SUT (r=0.423, P<0.01) also confirmed the idea that early childhood traumatic experiences continue to affect psychological functioning and poor coping behaviors that lead to substance abuse (Odacı et al., 2021). Nevertheless, Wang et al. (2020) showed that infancy or prenatal trauma is not significantly correlated with adult male alcohol use disorders, focusing on the timeline of the traumatic event concerning its moderation. The existing disparity demonstrates the necessity of considering the age point of the trauma, as early childhood trauma can have a more significant impact on SUT.
The mediating effects of emotion regulation, impulsivity, and PTSD symptoms were also confirmed. The direct impact of emotional dysregulation on SUT was significant (β=0.381, P<0.001), which concurs with the traumatic childhood findings that poor emotional regulation is a mediator of the relationship between childhood trauma and substance use (Koçak & Cagatay, 2024; Schaefer et al., 2021; Barahmand et al., 2016). Similarly, the relationship between trauma and substance use was mediated by impulsivity (β=0.104, P=0.006), which is in line with the results of studies that mark impulsivity as a neurocognitive mechanism between childhood adversity and substance use (Morris et al., 2020; Hosking & Winstanley, 2011; Brown et al., 2022). The significance of the mediating effect of PTSD symptoms was also found to be the highest (β=0.645, P<0.001), making the self-medication hypothesis, according to which individuals use substances to get rid of the distress caused by traumatic experiences, accurate (Rosenkranz et al., 2014; Patock-Peckham et al., 2020; Park et al., 2019; Hannan et al., 2017).
Comparison with existing literature
The results extrapolate prior studies by combining various mediators (emotional dysregulation, impulsivity, and PTSD symptoms) in one model in a non-psychiatric, culturally high population. This study also shows the importance of these mediators in a non-clinical sample of Iranian students, who, due to cultural circumstances (such as stigma and emotional suppression), might have stronger psychological vulnerabilities (Farnia et al., 2018) than those reported by Wang et al. (2020). This clinical sample that is specific to the types of trauma in addition to characteristics of clinical groups. The high correlation between the presence of emotional dysregulation and substance use found (r=0.522, P<0.01) agrees with what Mandavia et al. (2016) established in their research: emotional dysregulation is an intermediary in the interplay between childhood emotional abuse and lifelong substance use. Similarly, Ramakrishnan et al. (2019) found that positive urgency is an essential dimension between childhood maltreatment and substance use, supporting the mediating performance of impulsivity.
Usually, the presence of PTSD symptoms has a strong mediating impact, confirming previous studies that trauma-induced symptoms are the leading elements in developing substance use as a coping tool (Park et al., 2019; Hannan et al., 2017). This is particularly timely in Iran, where few people can seek mental health assistance, and cultural stigma can exacerbate dependence on substances to address PTSD symptoms (Skidmore et al., 2016).
Conclusion
However, this investigation supports both direct and indirect associations between childhood trauma and SUT among Iranian university students, such as the effects of emotional dysregulation, impulsivity, and PTSD symptoms on SUT. These results move towards understanding the psychological mechanisms that connect an early experience of trauma to substance use and the necessity of guiding interventions that operate on these mediators. Considering emotional dysregulation, impulsivity, and the manifestations of PTSD, especially when implemented in culturally considerate circumstances, prevention and treatment programs can decrease the risks of substance usage and enhance the mental health of survivors of trauma.
Limitations
Despite these contributions, this study has several limitations. The cross-sectional design does not allow for concluding causality and the time sequence. Self-report measures, at least where stigmatized behaviors and experiences are involved, carry the possibility of a recall or social desirability bias that can lead to incorrect downplaying of associations. The sample was national, and only students in Tehran were used; there is low generalizability to other communities in Iran, especially those living in less urban or exposed and less privileged areas. Besides, due to the exclusion of non-trauma diagnoses (anxiety, depression, or other comorbid conditions), other potentially relevant pathways associated with trauma and substance use may have been missed.
Unique contributions
To the best of our knowledge, no research has ever examined such mediating factors of emotional dysregulation, impulsivity, and PTSD symptoms in both dimensions of assessing the trauma and substance use pathway, and the same research on such aspects has never been undertaken, among a large sample of university students in a non-clinical population in Iran. Combining these elements into a single model and placing the study within a non-Western location allows for the addressing of vital gaps in the literature and the bringing forth of cultural specifics that can encourage the development of prevention and intervention strategies.
Direction for future research and recommendations
These conclusions are significant to prevention and intervention. The low to moderate but still significant mediating effects of emotional dysregulation, impulsivity, and PTSD symptoms potentially indicate that policies and strategies to promote substance use risk prevention among survivors of trauma may be implemented. For example, cognitive-behavior therapies aimed at emotional control and impulse control, and trauma-based therapies for PTSD can prove to be especially efficient. Cultural interventions, which would be able to respond to stigma and low access to mental health services, are essential in the Iranian case.
Future research on this topic should use longitudinal designs to demystify causal processes. The study should be replicated among non-student populations and rural groups to increase generalizability. Self-report biases may be decreased by including objective measures, such as clinical interviews or archival records. Also, the analysis of other mental health measures, including mood or anxiety disorders, would provide a more detailed picture of how trauma is connected to drug use.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Review Board of Kharazmi University, Tehran, Iran (Code: (IR.KHU.REC.1403.149). Participants were assured confidentiality.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Authors' contributions
Conceptualization: All authors; Supervision: Shahram Mohammadkhani and Robabeh Noury; Methodology, investigation, data collection and analysis: Mohammad Hossein Abdolloahi; Writing: Mohammad Hossein Abdolloahi, Shahram Mohammadkhani.
Conflict of interest
The authors declared no conflict of interest.
Acknowledgments
The authors thank all participants in this study.
References
Akcan, G., Öztürk, E., & Erdoğan, B. (2021). The investigation of the mediating role of coping strategies on the relationship between childhood traumas, depression, and alcohol use disorder in university students. Journal of Substance Abuse Treatment, 123, 108305. [DOI:10.1016/j.jsat.2021.108305] [PMID]
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association. [DOI:10.1176/appi.books.9780890425596]
Amin-Esmaeili, M., Rahimi-Movaghar, A., Sharifi, V., Hajebi, A., Radgoodarzi, R., & Mojtabai, R., et al. (2016). Epidemiology of illicit drug use disorders in Iran: Prevalence, correlates, comorbidity and service utilization results from the Iranian mental health survey. Addiction (Abingdon, England), 111(10), 1836–1847. [DOI:10.1111/add.13453] [PMID]
Andersen, S. L., & Teicher, M. H. (2009). Desperately driven and no brakes: Developmental stress exposure and subsequent risk for substance abuse. Neuroscience & Biobehavioral Reviews, 33(4), 516-524. [DOI:10.1016/j.neubiorev.2008.09.009] [PMID]
Banducci, A. N., Hoffman, E. M., Lejuez, C. W., & Koenen, K. C. (2014). The impact of childhood abuse on inpatient substance users: Specific links with risky sex, aggression, and emotion dysregulation. Child Abuse & Neglect, 38(5), 928–938.[DOI:10.1016/j.chiabu.2013.12.007] [PMID]
Barahmand, U., Khazaee, A., & Hashjin, G. S. (2016). Emotion dysregulation mediates between childhood emotional abuse and motives for substance use. Archives of Psychiatric Nursing, 30(6), 653-659. [DOI:10.1016/j.apnu.2016.02.007] [PMID]
Bernstein, D. P., Stein, J. A., Newcomb, M. D., Walker, E., Pogge, D., & Ahluvalia, T., et al. (2003). Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse & Neglect, 27(2), 169-190. [DOI:10.1016/S0145-2134(02)00541-0] [PMID]
Braquehais, M. D., Oquendo, M. A., Baca-García, E., & Sher, L. (2010). Is impulsivity a link between childhood abuse and suicide?. Comprehensive Psychiatry, 51(2), 121–129. [DOI:10.1016/j.comppsych.2009.05.003] [PMID]
Brown, S., Fite, P. J., & Bortolato, M. (2022). The mediating role of impulsivity in the associations between child maltreatment types and past-month substance use. Child Abuse & Neglect, 128, 105591. [DOI:10.1016/j.chiabu.2022.105591] [PMID]
Cyders, M. A., Littlefield, A. K., Coffey, S., & Karyadi, K. A. (2014). Examination of a short English version of the UPPS-P impulsive behavior scale. Addictive Behaviors, 39(9), 1372-1376. [DOI:10.1016/j.addbeh.2014.02.013] [PMID]
Farnia, V., Mousavi, S. B., Tatari, F., Salemi, S., Golshani, S., & Alikhani, M., et al. (2018). Prevalence of childhood attention-deficit/hyperactivity disorder (ADHD) in methamphetamine dependence: A descriptive study. Iranian Journal of Psychiatry and Behavioral Sciences, 12(4), e61329. [DOI:10.5812/ijpbs.61329]
Garrusi, B., & Nakhaee, N. (2009). Validity and reliability of a Persian version of the childhood trauma questionnaire. Psychological Reports, 104(2), 509-516. [DOI:10.2466/PR0.104.2.509-516] [PMID]
Gratz, K. L., & Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41-54. [DOI:10.1023/B:JOBA.0000007455.08539.94]
Hannan, S. M., Orcutt, H. K., Miron, L. R., & Thompson, K. L. (2017). Childhood sexual abuse and later alcohol-related problems: Investigating the roles of revictimization, PTSD, and drinking motivations among college women. Journal of Interpersonal Violence, 32(14), 2118-2138. [DOI:10.1177/0886260515591276] [PMID]
Hosking, J., & Winstanley, C. A. (2011). Impulsivity as a mediating mechanism between early-life adversity and addiction: Theoretical comment on Lovic et al. (2011). Behavioral Neuroscience, 125(5), 681-686. [DOI:10.1037/a0024612] [PMID]
Jebraeili, H., Moradi, A., & Habibi, M. (2019). Psychometric properties of the Persian short version of the five-factor impulsive behavior scale. Journal of Research and Health, 9(6), 516-524. [DOI:10.32598/jrh.9.6.516]
Keyes, K. M., Shmulewitz, D., Greenstein, E., McLaughlin, K., Wall, M., & Aharonovich, E., et al. (2014). Exposure to the Lebanon war of 2006 and effects on alcohol use disorders: The moderating role of childhood maltreatment. Drug and Alcohol Dependence, 134, 296–303. [DOI:10.1016/j.drugalcdep.2013.10.014] [PMID]
Khantzian, E. J. (1997). The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry, 4(5), 231-244. [DOI:10.3109/10673229709030550] [PMID]
Khanzadeh, M., Saeediyan, M., Hosseinchari, M., & Edrissi, F. (2012). [Factor structure and psychometric properties of the difficulties in emotional regulation scale (Persian)]. International Journal of Behavioral Sciences, 6(1), 87-96. [Link]
Kiburi, S. K., Molebatsi, K., Obondo, A., & Kuria, M. W. (2018). Adverse childhood experiences among patients with substance use disorders at a referral psychiatric hospital in Kenya. BMC Psychiatry, 18(1), 197. [DOI:10.1186/s12888-018-1780-1] [PMID]
Kline, R. B. (2010). Principles and practice of structural equation modeling. New York, NY: The Guilford Press. [Link]
Koçak, Z., & Çağatay, S. E. (2024). Childhood traumas and emotional eating: The mediating role of self-esteem and emotion dysregulation. Current Psychology, 43, 21783–21791. [DOI:10.1007/s12144-024-05953-2]
Lawson, K. M., Back, S. E., Hartwell, K. J., Maria, M. M., & Brady, K. T. (2013). A comparison of trauma profiles among individuals with prescription opioid, nicotine, or cocaine dependence. The American Journal on Addictions, 22(2), 127-131. [DOI:10.1111/j.1521-0391.2013.00319.x] [PMID]
Lovallo, W. R. (2013). Early life adversity reduces stress reactivity and enhances impulsive behavior: Implications for health behaviors. International Journal of Psychophysiology, 90(1), 8-16. [DOI:10.1016/j.ijpsycho.2012.10.006] [PMID]
Mandavia, A., Robinson, G. G., Bradley, B., Ressler, K. J., & Powers, A. (2016). Exposure to childhood abuse and later substance use: Indirect effects of emotion dysregulation and exposure to trauma. Journal of Traumatic Stress, 29(5), 422-429. [DOI:10.1002/jts.22131] [PMID]
Morris, V. L., Huffman, L. G., Naish, K. R., Holshausen, K., Oshri, A., McKinnon, M., & Amlung, M. (2020). Impulsivity as a mediating factor in the association between posttraumatic stress disorder symptoms and substance use. Psychological Trauma: Theory, Research, Practice and Policy, 12(6), 659–668. [DOI:10.1037/tra0000588] [PMID]
Odacı, H., Bülbül, K., & Türkkan, T. (2021). The mediating role of cognitive flexibility in the relationship between traumatic experiences in the childhood period and substance abuse proclivity. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 39(4), 538-554. [DOI:10.1007/s10942-020-00385-w]
Park, T., Thompson, K., Wekerle, C., Al‐Hamdani, M., Smith, S., & Hudson, A., et al. (2019). Posttraumatic stress symptoms and coping motives mediate the association between childhood maltreatment and alcohol problems. Journal of Traumatic Stress, 32(6), 918-926. [DOI:10.1002/jts.22467] [PMID]
Patock-Peckham, J. A., Belton, D. A., D’Ardenne, K., Tein, J. Y., Bauman, D. C., & Infurna, F. J., et al. (2020). Dimensions of childhood trauma and their direct and indirect links to PTSD, impaired control over drinking, and alcohol-related problems. Addictive Behaviors Reports, 12, 100304. [DOI:10.1016/j.abrep.2020.100304] [PMID]
Ramakrishnan, N., McPhee, M., Sosnowski, A., Rajasingaam, V., & Erb, S. (2019). Positive urgency partially mediates the relationship between childhood adversity and problems associated with substance use in an undergraduate population. Addictive Behaviors Reports, 10, 100230. [DOI:10.1016/j.abrep.2019.100230] [PMID]
Rezahosseini, O., Roohbakhsh, A., Tavakolian, V., & Assar, S. (2014). Drug abuse among university students of Rafsanjan, Iran. Iranian Journal of Psychiatry and Behavioral Sciences, 8(2), 81-85. [Link]
Rosenkranz, S. E., Muller, R. T., & Henderson, J. L. (2014). The role of complex PTSD in mediating childhood maltreatment and substance abuse severity among youth seeking substance abuse treatment. Psychological Trauma: Theory, Research, Practice, and Policy, 6(1), 25-33. [DOI:10.1037/a0031920]
Sadeghi, M., Taghva, A., Goudarzi, N., & Rah Nejat, A. M. (2016). Validity and reliability of the Persian version of “post-traumatic stress disorder scale” in war veterans. Iranian Journal of War and Public Health, 8(4), 243-249. [Link]
Schaefer, L. M., Hazzard, V. M., Smith, K. E., Johnson, C. A., Cao, L., & Crosby, R. D., et al. (2021). Examining the roles of emotion dysregulation and impulsivity in the relationship between psychological trauma and substance abuse among women with bulimic-spectrum pathology. Eating Disorders, 29(3), 276–291. [DOI:10.1080/10640266.2021.1891370] [PMID]
Shin, S. H., Lee, S., Jeon, S. M., & Wills, T. A. (2015). Childhood emotional abuse, negative emotion-driven impulsivity, and alcohol use in young adulthood. Child Abuse & Neglect, 50, 94-103. [DOI:10.1016/j.chiabu.2015.02.010] [PMID]
Skidmore, C. R., Kaufman, E. A., & Crowell, S. E. (2016). Substance use among college students. Child and Adolescent Psychiatric Clinics of North America, 25(4), 735-753. [DOI:10.1016/j.chc.2016.06.004] [PMID]
Unicef. (2024). Nearly 400 million young children worldwide regularly experience violent discipline at home. New York: Unicef. [Link]
Wang, L., An, C. X., Song, M., Li, N., Gao, Y. Y., & Zhao, X. C., et al. (2020). Evaluation of childhood traumatic experience as a risk factor for alcohol use disorder in adulthood. BMC Psychiatry, 20(1), 15. [DOI:10.1186/s12888-020-2428-5] [PMID]
Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., & Schnurr, P. P. (2014). PTSD checklist for DSM-5 (PCL-5). Cleveland: National Center for PTSD. [Link]
Weed, N. C., Butcher, J. N., McKenna, T., & Ben-Porath, Y. S. (1992). New measures for assessing alcohol and drug abuse with the MMPI-2: The APS and AAS. Journal of Personality Assessment, 58(2), 389–404. [DOI:10.1207/s15327752jpa5802_15] [PMID]
Weiss, N. H., Tull, M. T., Lavender, J., & Gratz, K. L. (2013). Role of emotion dysregulation in the relationship between childhood abuse and probable PTSD in a sample of substance abusers. Child Abuse & Neglect, 37(11), 944–954. [DOI:10.1016/j.chiabu.2013.03.014] [PMID]
Weiss, N. H., Tull, M. T., Viana, A. G., Anestis, M. D., & Gratz, K. L. (2012). Impulsive behaviors as an emotion regulation strategy: Examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders, 26(3), 453–458.[DOI:10.1016/j.janxdis.2012.01.007] [PMID]
White, H. R., & Widom, C. S. (2008). Three potential mediators of the effects of child abuse and neglect on adulthood substance use among women. Journal of Studies on Alcohol and Drugs, 69(3), 337-347. [DOI:10.15288/jsad.2008.69.337] [PMID]
WHO. (2018). Child maltreatment. Geneva: World Health Organization. [Link]
Zargar, Y., Najarian, B., & Naami, A. Z. (2008). [The relationship of some personality variables, religious attitudes, and marital satisfaction with addiction potential in personnel of an industrial factory in Ahvaz (Persian)]. Journal Of Education And Psychology, 15(1), 99-120. [Link]
Type of Study: Original Research Article |
Subject:
Substance abuse and dependence
Received: 2025/01/23 | Accepted: 2025/03/17 | Published: 2025/10/1
Received: 2025/01/23 | Accepted: 2025/03/17 | Published: 2025/10/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |