Volume 11, Issue 1 (Winter 2023)
PCP 2023, 11(1): 1-8 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hayati M, Ahmadi G, Lotfinia S, Hosseini S M, Mousavi S E. Cognitive Failure and Fear of COVID-19. PCP 2023; 11 (1) :1-8
URL: http://jpcp.uswr.ac.ir/article-1-818-en.html
URL: http://jpcp.uswr.ac.ir/article-1-818-en.html
Marzieh Hayati1 
 , Gholamreza Ahmadi2
, Gholamreza Ahmadi2 
 , Shahab Lotfinia3
, Shahab Lotfinia3 

 , Seyed Morteza Hosseini4
, Seyed Morteza Hosseini4 
 , Seyedeh Elnaz Mousavi *
, Seyedeh Elnaz Mousavi * 

 5
5

 , Gholamreza Ahmadi2
, Gholamreza Ahmadi2 
 , Shahab Lotfinia3
, Shahab Lotfinia3 

 , Seyed Morteza Hosseini4
, Seyed Morteza Hosseini4 
 , Seyedeh Elnaz Mousavi *
, Seyedeh Elnaz Mousavi * 

 5
5
1- Department of Clinical Psychology, Faculty of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran.
2- Department of Psychology, Faculty of Psychology and Educational Sciences, Allameh Tabatabaei University, Tehran, Iran.
3- Department of Clinical Psychology, Faculty of Medicine, Shahid Beheshti University of Medical Science, Tehran, Iran.
4- Quran and Hadith Reasearch Center, Baqiyatallah University of Medical Sciences, Tehran, Iran.
5- Department of Clinical Psychology, School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran. , elnaz48.mousavi@gmail.com
2- Department of Psychology, Faculty of Psychology and Educational Sciences, Allameh Tabatabaei University, Tehran, Iran.
3- Department of Clinical Psychology, Faculty of Medicine, Shahid Beheshti University of Medical Science, Tehran, Iran.
4- Quran and Hadith Reasearch Center, Baqiyatallah University of Medical Sciences, Tehran, Iran.
5- Department of Clinical Psychology, School of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran. , elnaz48.mousavi@gmail.com
Keywords: COVID-19 pandemic, Cognitive neuroscience, Cognitive function, Cognitive test, Memory deficits
Full-Text [PDF 655 kb]
(507 Downloads)
| Abstract (HTML) (1633 Views)
Full-Text: (306 Views)
1. Introduction
Coronavirus disease 2019 (COVID-19) was reported in December 2019 in Wuhan, China (Huang & Zhao, 2020). The World Health Organization (WHO) called the disease a pandemic. The pandemic quickly reached and affected everyone worldwide (Vieira et al., 2020). Fever, dry coughs, and shortness of breath are some of the symptoms of this disease (Moghanibashi-Mansourieh, 2020). According to the statements of WHO, this pandemic has caused fear and panic in many people and has changed many aspects of people’s lives (Kim & Su, 2020). The COVID-19 pandemic has become a global concern (Mamun & Griffiths, 2020), and the public’s concern about getting infected by suspected COVID-19 individuals led to panic in society. Although this has helped in limiting the growing number of patients, it has created fear and anxiety (Sahoo et al., 2020). Also, issues related to the pandemic, such as social distancing, have caused psychological problems, including anxiety, sorrow, concern, rage, irritation, helplessness, and guilt (Mamun & Griffiths, 2020). Even recovered patients cannot be safe from the psychological effects of the pandemic because of the increase in public fear and the decrease in economic and social activities.
Individuals in quarantine are also suspectable to unpleasant emotional experiences, such as fear, anger, depression, and guilt (Kim & Su, 2020).
According to the literature, psychological symptoms, such as anxiety, panic, trauma, psychosis, and suicidal ideation are common during pandemics (Moghanibashi-Mansourieh, 2020). We must pay attention to physical and biopsychosocial aspects. Meanwhile, COVID-19 affects the central nervous system, and these psychiatric complications are the main concern (Kim & Su, 2020). In this regard, the Korean Psychiatric Society proposed telephone counseling sessions be funded by the Korean government. In addition, many mental supportive programs were started by the Taiwanese Society for Nutritional Psychiatry Research (TSNRP: www.tsnpr.org.tw/) (Kim & Su, 2020). These psychological emergency services created because of the COVID-19 crisis indicate the important role of psychological variables in developing the COVID-19 and post-COVID-19 period; accordingly, it is important to address this issue. One major issue with the biological-psychological nature is that paying attention at this stage is the role of cognitive failure in fear and reaction to the COVID-19 virus.
A vital factor of health is cognition (Gonçalves et al., 2011). A defect in this factor can negatively affect emotional processing, social functions, and the quality of life (Etkin et al., 2013). This is because the cognitive regulation of emotion and behavior occurs under the supervision of the prefrontal cortex (Miller & Cohen, 2001). This part is responsible for integrating different functions (Widge et al., 2019) and is known as an important part of the mood and emotion-modulating brain network (Keshvari et al., 2017; Steele & Lawrie, 2004). In addition, various studies have shown a relationship between cognitive failure and vulnerability to stress (Broadbent et al., 1982), neuroticism, the tendency to experience negative emotions (Zufferey et al., 2017), anxiety traits, minor symptoms of psychiatric disorders (Matthews & Wells, 1988; Tirre, 2018), anxiety disorders (Matthews et al., 1990), and phobias (Broadbent et al., 1982). Cognitive failure can lead to the adoption of maladaptive coping strategies in which an individual chooses emotion-oriented solutions as the first strategy (Broadbent et al., 1986). This aggravates the negative predictions of events (Zufferey et al., 2017).
Experts define cognitive failure as the inability to successfully perform tasks that a person can usually perform daily, such as forgetting appointments and not responding to emails unintentionally (Payne & Schnapp, 2014), which can lead to major problems because of interfering with daily activities and distracting people’s concentration. Moreover, this insufficiency is found in non-clinical examples and can cause emotional arousal in these people in critical situations (Carrigan & Barkus, 2016). Cognitive failure increases the chance of depression and anxiety during contagious disease outbreaks (Mirza et al., 2017). Cognitive failure increases the vulnerability to disorders caused by negative emotions, such as anxiety, and is associated with a wide range of emotions, including fear, anger, anxiety, and other emotions (Payne & Schnapp, 2014).
A review article in Iran found that during the COVID-19 pandemic, a decline in people’s mental health can be seen, and the symptoms of worry and fear of infection with this virus have spread to all sections of society (Shahed hagh ghadam et al., 2020), the fear of which is not specific to Iran and has spread in different societies. This frightening issue has led to psychological consequences and many other problems (Nooraei et al., 2020). Another reason for the fear of COVID-19 is patients’ fear of social reactions, disease stigma, and being a disease carrier, which has been ignored because of the current crisis (Jahangasht, 2020). Many people worldwide have developed a fear of catching the virus, leading to psychological fear and stress (Zhu et al., 2020), and ambiguity, thus intensifying the level of anxiety. Since mild cognitive failure has been found in non-clinical samples (Carrigan & Barkus, 2016) and the presence of this impairment will cause negative and maladaptive emotions (Mirza et al., 2017), this research aims to investigate the relationship between cognitive failure and the fear of COVID-19.
2. Participants and Methods
Study participants
A total of 415 people were selected by the available sampling method among the statistical population considered for the present study (residents of Tehran Province, Iran). In this research, we focused on Tehran Province, Iran, as it had a severe prevalence rate of COVID-19 during the questionnaire distribution according to the Ministry of Health’s formal statistics.
Inclusion criteria
The inclusion criteria comprised the ability to read and write, living in Tehran Province, Iran, and being in the age range of 18 to 65 (mental development has occurred until the age of 18 and the decline in cognitive ability because of aging has not yet begun, thus by choosing this age range, the mental ability is measured more accurately).
Exclusion criteria
The exclusion criteria were suffering from dementia, emotional disorders, use of psychiatric medications (along with demographic questions, these criteria were asked in a closed-ended response [yes or no]), and incomplete completion of the questionnaires.
Data collection
In this study, the data was collected online. The questionnaires were designed online and linked to platforms, such as Telegram, Instagram, and WhatsApp. Accordingly, subjects who wanted to participate in the research could answer the questionnaires and send their answers to the researcher. The confidentiality of the participants’ information, the explanation of the research objectives, the explanation of the volunteer participation in the research, and the provision of the results, if desired, were among the ethical principles observed in this research. Data analysis was conducted using the independent t test and stepwise regression.
The questions included demographic information (sex, age, marital status, education level, and living province), history of emotional disorder, dementia, and consumption of psychological drugs. Also, the questionnaires contained questions regarding concerns about COVID-19 news, scoring the participants’ knowledge about COVID-19 signs, and whether their relatives were infected by the virus along with their current situation. The questionnaires were the fear of COVID-19 scale and the cognitive failures questionnaire (CFQ).
Fear of COVID-19 questionnaire
Ahorsu et al. developed the Fear of COVID-19 scale. This scale includes 7 questions with a 5-point Likert scale. The responses are “completely agree”, “agree”, “neither agree nor disagree”, “disagree”, and “completely disagree”. The maximum score is 5, the minimum is 1, and the range of scores of the questionnaire is 7 to 35. Higher scores indicate more fear of COVID-19. This study obtained a Cronbach α of 0.82 and the test-retest reliability was acceptable (Ahorsu et al., 2020).
Cognitive failures questionnaire
Broadbent developed CFQ in 1982. This questionnaire is a self-reporting tool that measures the scores that respondents give to a 25-item cognitive failure questionnaire (Boomsma, 1998). The questionnaire’s subscales include forgetfulness, distractibility, and false triggering (Rast et al., 2009). The scores obtained from the test remain constant over long periods, indicating that the instrument measures cognitive deficits that represent personality traits (as opposed to state-dependent errors). Consequently, this tool does not reflect the change in the cognition of people who experience life-threatening events. The most likely approach is that cognitive failure is not caused by anxiety, but having these defects exposes the individual to the negative effects of experiencing anxiety (Broadbent et al., 1982). Broadbent’s CFQ measures the absence of mindfulness and committing errors in doing simple homework because of inattention. The internal consistency of CFQ was obtained at 0.89 and the test-retest reliability was reported in the range of 0.8 to 0.82 (Baer et al., 2006).
3. Result
Among the total of 430 participants from Tehran Province, Iran, 406 subjects responded to the presented tools completely and the incomplete questionnaire was excluded from the analysis. Among the respondents, 112 (27.6%) were male and 293 (72.2%) were female. Meanwhile, 248 (60%) were married and 50% of the respondents had a Bachelor’s or a Master’s degree. A total of 95% percent of people consistently, often, or sometimes, followed the news related to COVID-19, while only 5% did not follow any news in this regard. The relatives of 77% of the participants had no history of catching the virus, 13.4% had recovered, 5.7% were infected during the study, and 3.9% had died because of COVID-19.
According to Table 1, all variables were in the normal range, and the following histogram diagram confirms the data (Figure 1).
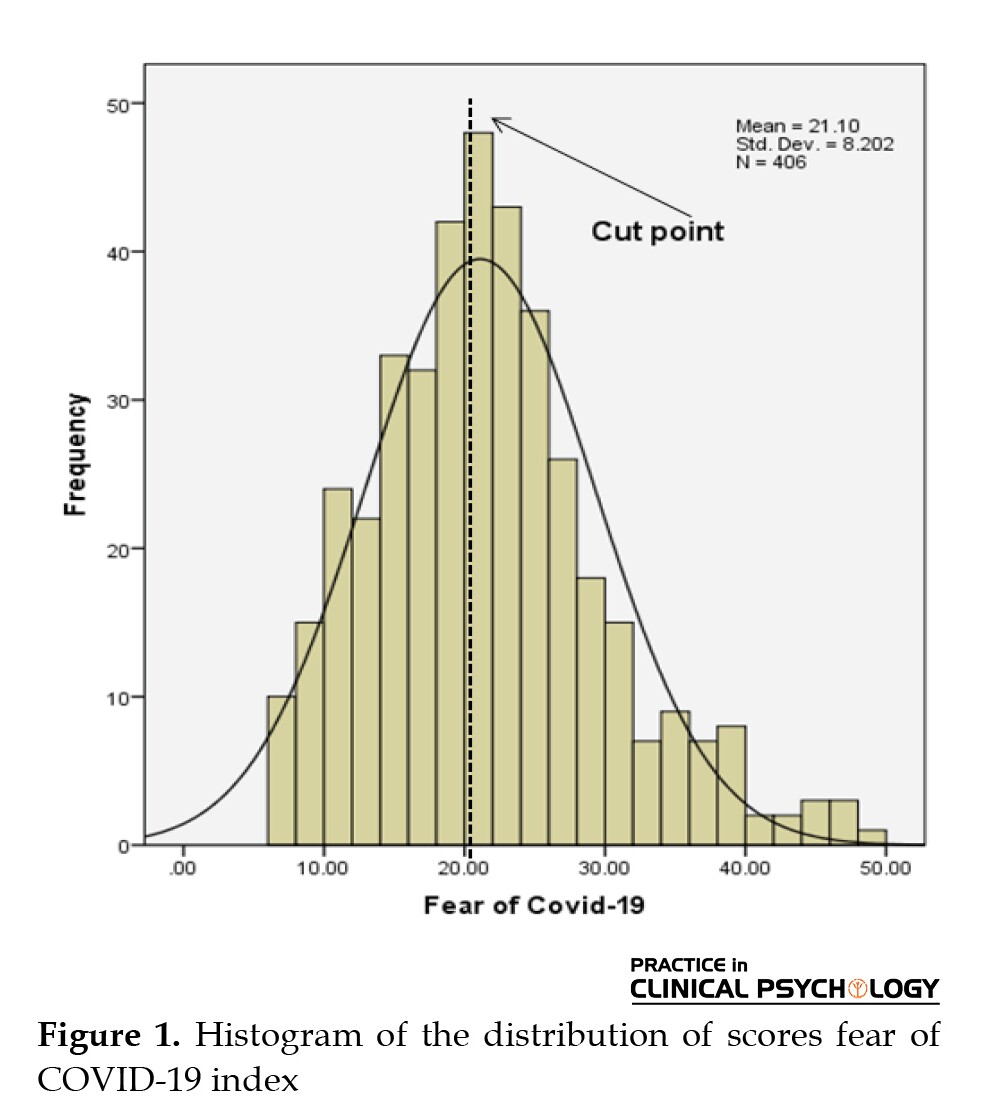
Participants were divided into two levels of low and high fear according to the cutoff point mean.

Then, the subscales of cognitive failure are compared in these two levels (Table 2). Additionally, to predict the fear of COVID-19 according to research variables, at first, the hypotheses related to stepwise regression analysis were tested. In addition to using the distance scale and normal distribution, the output of the Durbin–Watson test (1.89) indicates the presumption of observing the independence of the residuals.

Considering the index higher than 0.01 and the low level of variance inflation factor (VIF) in Table 3, no problem of multiple lines exists as a restriction for applying the regression method. Thus, to predict the fear of COVID-19, the age variables, following the COVID-19 news, and the 3 subscales of memory, distractibility, and false triggering as the predictor variable entered the regression equation.

According to Table 3, among the predictors that entered the regression equation, only the variables of following the news and memory can predict the fear of COVID-19, and other variables were excluded from the equation. Following the news, and memory could predict 14% of the fear of COVID-19 (R2=0.141, adjusted R2=0.137, P<0.01).
According to the β coefficients in Table 4, a negative relationship exists between fear of COVID-19 and following COVID-19 news; however, the relationship between fear of COVID-19 and memory error was positive and significant. Yet, the standard coefficients indicated that even though the effects of both variables were almost identical in changing the dependent variable (β= 0.281; t=5.89; β=-0.286; t=-6.09).

4. Discussion
The growing prevalence of COVID-19 has challenged global public health, leading to a morbid fear of infection in various populations. This research aimed to investigate the relationship between cognitive failure and the fear of COVID-19. The results showed a negative relationship between fear of COVID-19 and following COVID-19 news. This shows that with increasing follow-ups on COVID-19-related news, the fear of COVID-19 decreases. In explaining this finding, due to the nature of the exposure mechanism in this follow-up, people who follow COVID-19 news face negative fears and emotions, and because of the effectiveness of the fear mechanism (Abramowitz et al., 2019; Schäfer et al., 2018; Wannemueller et al., 2018), the fear is reduced. Also, because of the silence, their anxiety is reduced, which leads to the management of stress (Leong et al., 2015; Merz et al., 2014). In addition, gaining this information and exposure reduces ambiguity and uncertainty, and according to research, through this mechanism, the anxiety and fear of COVID-19 are reduced (Hebert & Dugas, 2019; Osmanağaoğlu et al., 2018; Shihata et al., 2017). The finding of this research about reducing fear and ambiguity while exposing stressful situations is the same as the finding of Schafer et al. (Schäfer et al., 2018), Merz et al. (Merz et al., 2014), and Hebert et al. (Hebert & Dugas, 2019).
Based on the results of the regression method in this study, the components of forgetfulness (memory) can predict the fear of COVID-19. Cognitive failure affects people’s mental health. False triggering, distractibility, and memory problems, which are the subscales of cognitive failure, can decrease a person’s mental health (Broadbent et al., 1982). In the current situation, the intervening issue can be considered the prevalence of COVID-19 and the fear of infection with it. In the present study, the forgetfulness subscale was significantly related to fear of COVID-19.
Based on the research literature, high cognitive failures can indicate a general ruminant approach, which may be the rate of vulnerability to negative emotions (Broadbent et al., 1982) and may also be associated with neuroticism (Zufferey et al., 2017) of anxiety traits (Merckelbach et al., 1996) and subsequent intolerance of uncertainty. Therefore, in explaining this finding, people who have shown memory failure do not record information about COVID-19 or suppress the information. This failure in memory causes obsessive-compulsive mental rumination, uncertainty, worry, fear, and anxiety that are associated with the virus; consequently, this uncertainty intolerance and rumination can cause stress or fear of COVID-19 or exacerbate the pre-existing condition. It has been found that cognitive failure is associated with negative emotions, especially stress and anxiety, fear, and neuroticism. That is in line with the finding of Broadbent et al. (Broadbent et al., 1982), Zufferey et al. (Zufferey et al., 2017), Matthews et al. (Matthews et al., 1990), and Mirza et al. (Mirza et al., 2017). Therefore, a relationship exists between cognitive processes that are associated with failure and a wide range of emotions, as well as fear, stress, and anxiety.
The hypothesis of the association of certain moods with errors in cognitive processing has already been proven (Payne & Schnapp, 2014), and mood is related to daily cognitive function (Schnapp, 2007). Negative emotional factors (such as fear, sadness, the feeling of guilt, and hostility) are significantly associated with the scores of distractibility, memory, and false triggering of the CFQ questionnaire as well as the total score of the questionnaire. Meanwhile, fear is one of the negative emotions that is correlated with high scores on the CFQ questionnaire. Thus, regarding the correlation between CFQ scores and negative emotions, one explanation is that the questionnaire measures a feature associated with complaining (or an aspect of neuroticism) that may overlap with experiencing negative emotion. Another explanation is that changes in cognition occur when cognitive resources are challenged by disturbing thoughts caused by stress and trauma (Payne & Schnapp, 2014). Also, experiencing negative emotions can cause susceptible individuals to recall and report more cognitive failures (Fisher et al., 2020).
CFQ is a tool for identifying vulnerable individuals (Payne & Schnapp, 2014). People with high scores in this questionnaire are vulnerable to stress (Matthews & Wells, 1988), and evidence suggests that cognitive failure affects the interpretation of stressful situations. The limitation of the present study was related to convenience sampling which reduces the generalizability of the results. Considering the COVID-19 pandemic conditions, the questionnaires were completed online, and we suggest using objective tools to assess cognitive failure.
5. Conclusion
The results indicate that the component of forgetfulness (memory) can predict the fear of COVID-19, and it is deduced in case of false triggering, distractibility, and memory problems, which are the subscales of cognitive failure and will decrease individuals’ mental health.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences with the Code of Ethics: IR.SBMU.MSP.REC.1400.303.
Funding
This study is supported by Shahid Beheshti University of Medical Sciences.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors report no competing interests to declare.
References
Abramowitz, J. S., Deacon, B. J., & Whiteside, S. P. H. (2019). Exposure therapy for anxiety: Principles and practice. New York: Guilford Publications [Link]
Ahorsu, D. K., Lin, C. Y., Imani, V., Saffari, M., Griffiths, M. D., & Pakpour, A. H. (2020). The fear of COVID-19 scale: Development and initial validation. International Journal of Mental Health and Addiction, 1-9. [DOI:10.1037/t78404-000]
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27-45. [DOI:10.1177/1073191105283504] [PMID]
Boomsma, D. I. (1998). Genetic analysis of cognitive failures (CFQ): A study of Dutch adolescent twins and their parents. European Journal of Personality, 12(5), 321-330. [DOI:10.1002/(SICI)1099-0984(1998090)12:5<321::AID-PER334>3.0.CO;2-5]
Broadbent, D. E., Broadbent, M. H., & Jones, J. L. (1986). Performance correlates of self‐reported cognitive failure and of obsessionality. British Journal of Clinical Psychology, 25(4), 285-299. [DOI:10.1111/j.2044-8260.1986.tb00708.x] [PMID]
Broadbent, D. E., Cooper, P. F., FitzGerald, P., & Parkes, K. R. (1982). The Cognitive Failures Questionnaire (CFQ) and its correlates. British Journal of Clinical Psychology, 21(1), 1-16. [DOI:10.1111/j.2044-8260.1982.tb01421.x] [PMID]
Carrigan, N., & Barkus, E. (2016). A systematic review of cognitive failures in daily life: Healthy populations. Neuroscience & Biobehavioral Reviews, 63, 29-42. [DOI:10.1016/j.neubiorev.2016.01.010] [PMID]
Etkin, A., Gyurak, A., & O’Hara, R. (2013). A neurobiological approach to the cognitive deficits of psychiatric disorders. Dialogues in Clinical Neuroscience, 15(4), 419-429. [PMID] [PMCID]
Fisher, J. E., Zhou, J., Liu, A. G., Fullerton, C. S., Ursano, R. J., & Cozza, S. J. (2020). Effect of comorbid anxiety and depression in complicated grief on perceived cognitive failures. Depression and Anxiety, 37(1), 54-62. [DOI:10.1002/da.22943] [PMID]
Gonçalves, L. C., Vale, R. G., Barata, N. J., Varejão, R. V., & Dantas, E. H. (2011). Flexibility, functional autonomy and quality of life (QoL) in elderly yoga practitioners. Archives of Gerontology and Geriatrics, 53(2), 158-162. [DOI:10.1016/j.archger.2010.10.028] [PMID]
Hebert, E. A., & Dugas, M. J. (2019). Behavioral experiments for intolerance of uncertainty: Challenging the unknown in the treatment of generalized anxiety disorder. Cognitive and Behavioral Practice, 26(2), 421-436. [DOI:10.1016/j.cbpra.2018.07.007]
Huang, Y., & Zhao, N. (2020). Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Research, 288, 112954. [DOI:10.1016/j.psychres.2020.112954] [PMID] [PMCID]
Jahangasht, K. (2020). [Social stigma: The social consequences of covid-19 (Persian)]. Journal of Marine Medicine, 2(1), 59-60. [Link]
Keshvari, F., Heshmati, P., & Ghasemian-Shirvan, E. (2017). [The role of prefrotal cortex in subjective mood: A transcranial direct current stimulation study (Persian)]. Journal of Research in Psychological Health, 11(1), 25-38. [DOI:10.29252/rph.11.1.25]
Kim, S. W., & Su, K. P. (2020). Using psychoneuroimmunity against COVID-19. Brain, Behavior, and Immunity, 87, 4-5. [DOI:10.1016/j.bbi.2020.03.025] [PMID] [PMCID]
Leong, K. C., Goodman, J., & Packard, M. G. (2015). Post-training re-exposure to fear conditioned stimuli enhances memory consolidation and biases rats toward the use of dorsolateral striatum-dependent response learning. Behavioural Brain Research, 291, 195-200. [DOI:10.1016/j.bbr.2015.05.022] [PMID]
Mamun, M. A., & Griffiths, M. D. (2020). First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: Possible suicide prevention strategies. Asian Journal of Psychiatry, 51, 102073. [DOI:10.1016/j.ajp.2020.102073] [PMID] [PMCID]
Matthews, G., Coyle, K., & Craig, A. (1990). Multiple factors of cognitive failure and their relationships with stress vulnerability. Journal of Psychopathology and Behavioral Assessment, 12(1), 49-65. [DOI:10.1007/BF00960453]
Matthews, G., & Wells, A. (1988). Relationships between anxiety, self-consciousness, and cognitive failure. Cognition and Emotion, 2(2), 123-132. [DOI:10.1080/02699938808408069]
Merckelbach, H., Muris, P., Nijman, H., & de Jong, P. J. (1996). Self-reported cognitive failures and neurotic symptomatology. Personality and Individual Differences, 20(6), 715-724. [DOI:10.1016/0191-8869(96)00024-4]
Merz, C. J., Hamacher-Dang, T. C., & Wolf, O. T. (2014). Exposure to stress attenuates fear retrieval in healthy men. Psychoneuroendocrinology, 41, 89-96. [DOI:10.1016/j.psyneuen.2013.12.009] [PMID]
Miller, E. K., & Cohen, J. D. (2001). An integrative theory of prefrontal cortex function. Annual Review of Neuroscience, 24, 167-202. [DOI:10.1146/annurev.neuro.24.1.167] [PMID]
Mirza, S. S., Ikram, M. A., Bos, D., Mihaescu, R., Hofman, A., & Tiemeier, H. (2017). Mild cognitive impairment and risk of depression and anxiety: A population-based study. Alzheimer’s & Dementia, 13(2), 130-139. [DOI:10.1016/j.jalz.2016.06.2361] [PMID]
Moghanibashi-Mansourieh, A. (2020). Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian Journal of Psychiatry, 51, 102076. [PMID] [PMCID]
Nooraei, S., Entezari, M., Hushmandi, K., & Raei, M. (2020). [Stress and anxiety caused by covid-19 in the communities (Persian)]. Journal of Marine Medicine, 2(1), 65-66. [Link]
Osmanağaoğlu, N., Creswell, C., & Dodd, H. F. (2018). Intolerance of Uncertainty, anxiety, and worry in children and adolescents: A meta-analysis. Journal of Affective Disorders, 225, 80-90. [PMID]
Payne, T. W., & Schnapp, M. A. (2014). The relationship between negative affect and reported cognitive failures. Depression Research and Treatment, 2014, 396195. [PMID] [PMCID]
Rast, P., Zimprich, D., Van Boxtel, M., & Jolles, J. (2009). Factor structure and measurement invariance of the cognitive failures questionnaire across the adult life span. Assessment, 16(2), 145-158. [DOI:10.1177/1073191108324440] [PMID]
Sahoo, S., Rani, S., Parveen, S., Pal Singh, A., Mehra, A., & Chakrabarti, S., et al. (2020). Self-harm and COVID-19 pandemic: An emerging concern-A report of 2 cases from India. Asian Journal of Psychiatry, 51, 102104. [PMID] [PMCID]
Schäfer, S. K., Ihmig, F. R., Lara H, K. A., Neurohr, F., Kiefer, S., & Staginnus, M., et al. (2018). Effects of heart rate variability biofeedback during exposure to fear-provoking stimuli within spider-fearful individuals: Study protocol for a randomized controlled trial. Trials, 19(1), 184. [DOI:10.1186/s13063-018-2554-2] [PMID] [PMCID]
Schnapp, M. (2007). Affect and cognitive failures: A comparison of positive and negative mood factors. Kenyon Summer Science Scholars Program, 364. [Link]
Shahed hagh ghadam, H., Fathi Ashtiani, A., Rahnejat, A. M., Ahmadi Tahour Soltani, M., Taghva, A., & Ebrahimi, M. R., et al. (2020). [Psychological consequences and interventions during the covid-19 pandemic: Narrative review (Persian)]. Journal of Marine Medicine, 2(1), 1-11. [DOI:10.30491/2.1.7]
Shihata, S., McEvoy, P. M., & Mullan, B. A. (2017). Pathways from uncertainty to anxiety: An evaluation of a hierarchical model of trait and disorder-specific intolerance of uncertainty on anxiety disorder symptoms. Journal of Anxiety Disorders, 45, 72-79. [DOI:10.1016/j.janxdis.2016.12.001] [PMID]
Steele, J. D., & Lawrie, S. M. (2004). Segregation of cognitive and emotional function in the prefrontal cortex: A stereotactic meta-analysis. Neuroimage, 21(3), 868-875. [DOI:10.1016/j.neuroimage.2003.09.066] [PMID]
Tirre, W. C. (2018). Dimensionality and determinants of self-reported cognitive failures. International Journal of Psychological Research, 11(1), 9-18. [PMID] [PMCID]
Mesa Vieira, C., Franco, O. H., Gómez Restrepo, C., & Abel, T. (2020). COVID-19: The forgotten priorities of the pandemic. Maturitas, 136, 38-41. [PMID] [PMCID]
Wannemueller, A., Moser, D., Kumsta, R., Jöhren, H. P., Adolph, D., & Margraf, J. (2018). Mechanisms, genes and treatment: Experimental fear conditioning, the serotonin transporter gene, and the outcome of a highly standardized exposure-based fear treatment. Behaviour Research and Therapy, 107, 117-126. [DOI:10.1016/j.brat.2018.06.003] [PMID]
Widge, A. S., Zorowitz, S., Basu, I., Paulk, A. C., Cash, S. S., & Eskandar, E. N., et al. (2019). Deep brain stimulation of the internal capsule enhances human cognitive control and prefrontal cortex function. Nature Communications, 10(1), 1536. [PMID] [PMCID]
Zhu, Z., Xu, S., Wang, H., Liu, Z., Wu, J., & Li, G., et al. (2020). COVID-19 in Wuhan: Immediate psychological impact on 5062 health workers. MedRxiv, 1-24. [DOI:10.1101/2020.02.20.20025338]
Zufferey, V., Donati, A., Popp, J., Meuli, R., Rossier, J., & Frackowiak, R., et al. (2017). Neuroticism, depression, and anxiety traits exacerbate the state of cognitive impairment and hippocampal vulnerability to Alzheimer’s disease. Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring, 7, 107-114. [PMID]
Coronavirus disease 2019 (COVID-19) was reported in December 2019 in Wuhan, China (Huang & Zhao, 2020). The World Health Organization (WHO) called the disease a pandemic. The pandemic quickly reached and affected everyone worldwide (Vieira et al., 2020). Fever, dry coughs, and shortness of breath are some of the symptoms of this disease (Moghanibashi-Mansourieh, 2020). According to the statements of WHO, this pandemic has caused fear and panic in many people and has changed many aspects of people’s lives (Kim & Su, 2020). The COVID-19 pandemic has become a global concern (Mamun & Griffiths, 2020), and the public’s concern about getting infected by suspected COVID-19 individuals led to panic in society. Although this has helped in limiting the growing number of patients, it has created fear and anxiety (Sahoo et al., 2020). Also, issues related to the pandemic, such as social distancing, have caused psychological problems, including anxiety, sorrow, concern, rage, irritation, helplessness, and guilt (Mamun & Griffiths, 2020). Even recovered patients cannot be safe from the psychological effects of the pandemic because of the increase in public fear and the decrease in economic and social activities.
Individuals in quarantine are also suspectable to unpleasant emotional experiences, such as fear, anger, depression, and guilt (Kim & Su, 2020).
According to the literature, psychological symptoms, such as anxiety, panic, trauma, psychosis, and suicidal ideation are common during pandemics (Moghanibashi-Mansourieh, 2020). We must pay attention to physical and biopsychosocial aspects. Meanwhile, COVID-19 affects the central nervous system, and these psychiatric complications are the main concern (Kim & Su, 2020). In this regard, the Korean Psychiatric Society proposed telephone counseling sessions be funded by the Korean government. In addition, many mental supportive programs were started by the Taiwanese Society for Nutritional Psychiatry Research (TSNRP: www.tsnpr.org.tw/) (Kim & Su, 2020). These psychological emergency services created because of the COVID-19 crisis indicate the important role of psychological variables in developing the COVID-19 and post-COVID-19 period; accordingly, it is important to address this issue. One major issue with the biological-psychological nature is that paying attention at this stage is the role of cognitive failure in fear and reaction to the COVID-19 virus.
A vital factor of health is cognition (Gonçalves et al., 2011). A defect in this factor can negatively affect emotional processing, social functions, and the quality of life (Etkin et al., 2013). This is because the cognitive regulation of emotion and behavior occurs under the supervision of the prefrontal cortex (Miller & Cohen, 2001). This part is responsible for integrating different functions (Widge et al., 2019) and is known as an important part of the mood and emotion-modulating brain network (Keshvari et al., 2017; Steele & Lawrie, 2004). In addition, various studies have shown a relationship between cognitive failure and vulnerability to stress (Broadbent et al., 1982), neuroticism, the tendency to experience negative emotions (Zufferey et al., 2017), anxiety traits, minor symptoms of psychiatric disorders (Matthews & Wells, 1988; Tirre, 2018), anxiety disorders (Matthews et al., 1990), and phobias (Broadbent et al., 1982). Cognitive failure can lead to the adoption of maladaptive coping strategies in which an individual chooses emotion-oriented solutions as the first strategy (Broadbent et al., 1986). This aggravates the negative predictions of events (Zufferey et al., 2017).
Experts define cognitive failure as the inability to successfully perform tasks that a person can usually perform daily, such as forgetting appointments and not responding to emails unintentionally (Payne & Schnapp, 2014), which can lead to major problems because of interfering with daily activities and distracting people’s concentration. Moreover, this insufficiency is found in non-clinical examples and can cause emotional arousal in these people in critical situations (Carrigan & Barkus, 2016). Cognitive failure increases the chance of depression and anxiety during contagious disease outbreaks (Mirza et al., 2017). Cognitive failure increases the vulnerability to disorders caused by negative emotions, such as anxiety, and is associated with a wide range of emotions, including fear, anger, anxiety, and other emotions (Payne & Schnapp, 2014).
A review article in Iran found that during the COVID-19 pandemic, a decline in people’s mental health can be seen, and the symptoms of worry and fear of infection with this virus have spread to all sections of society (Shahed hagh ghadam et al., 2020), the fear of which is not specific to Iran and has spread in different societies. This frightening issue has led to psychological consequences and many other problems (Nooraei et al., 2020). Another reason for the fear of COVID-19 is patients’ fear of social reactions, disease stigma, and being a disease carrier, which has been ignored because of the current crisis (Jahangasht, 2020). Many people worldwide have developed a fear of catching the virus, leading to psychological fear and stress (Zhu et al., 2020), and ambiguity, thus intensifying the level of anxiety. Since mild cognitive failure has been found in non-clinical samples (Carrigan & Barkus, 2016) and the presence of this impairment will cause negative and maladaptive emotions (Mirza et al., 2017), this research aims to investigate the relationship between cognitive failure and the fear of COVID-19.
2. Participants and Methods
Study participants
A total of 415 people were selected by the available sampling method among the statistical population considered for the present study (residents of Tehran Province, Iran). In this research, we focused on Tehran Province, Iran, as it had a severe prevalence rate of COVID-19 during the questionnaire distribution according to the Ministry of Health’s formal statistics.
Inclusion criteria
The inclusion criteria comprised the ability to read and write, living in Tehran Province, Iran, and being in the age range of 18 to 65 (mental development has occurred until the age of 18 and the decline in cognitive ability because of aging has not yet begun, thus by choosing this age range, the mental ability is measured more accurately).
Exclusion criteria
The exclusion criteria were suffering from dementia, emotional disorders, use of psychiatric medications (along with demographic questions, these criteria were asked in a closed-ended response [yes or no]), and incomplete completion of the questionnaires.
Data collection
In this study, the data was collected online. The questionnaires were designed online and linked to platforms, such as Telegram, Instagram, and WhatsApp. Accordingly, subjects who wanted to participate in the research could answer the questionnaires and send their answers to the researcher. The confidentiality of the participants’ information, the explanation of the research objectives, the explanation of the volunteer participation in the research, and the provision of the results, if desired, were among the ethical principles observed in this research. Data analysis was conducted using the independent t test and stepwise regression.
The questions included demographic information (sex, age, marital status, education level, and living province), history of emotional disorder, dementia, and consumption of psychological drugs. Also, the questionnaires contained questions regarding concerns about COVID-19 news, scoring the participants’ knowledge about COVID-19 signs, and whether their relatives were infected by the virus along with their current situation. The questionnaires were the fear of COVID-19 scale and the cognitive failures questionnaire (CFQ).
Fear of COVID-19 questionnaire
Ahorsu et al. developed the Fear of COVID-19 scale. This scale includes 7 questions with a 5-point Likert scale. The responses are “completely agree”, “agree”, “neither agree nor disagree”, “disagree”, and “completely disagree”. The maximum score is 5, the minimum is 1, and the range of scores of the questionnaire is 7 to 35. Higher scores indicate more fear of COVID-19. This study obtained a Cronbach α of 0.82 and the test-retest reliability was acceptable (Ahorsu et al., 2020).
Cognitive failures questionnaire
Broadbent developed CFQ in 1982. This questionnaire is a self-reporting tool that measures the scores that respondents give to a 25-item cognitive failure questionnaire (Boomsma, 1998). The questionnaire’s subscales include forgetfulness, distractibility, and false triggering (Rast et al., 2009). The scores obtained from the test remain constant over long periods, indicating that the instrument measures cognitive deficits that represent personality traits (as opposed to state-dependent errors). Consequently, this tool does not reflect the change in the cognition of people who experience life-threatening events. The most likely approach is that cognitive failure is not caused by anxiety, but having these defects exposes the individual to the negative effects of experiencing anxiety (Broadbent et al., 1982). Broadbent’s CFQ measures the absence of mindfulness and committing errors in doing simple homework because of inattention. The internal consistency of CFQ was obtained at 0.89 and the test-retest reliability was reported in the range of 0.8 to 0.82 (Baer et al., 2006).
3. Result
Among the total of 430 participants from Tehran Province, Iran, 406 subjects responded to the presented tools completely and the incomplete questionnaire was excluded from the analysis. Among the respondents, 112 (27.6%) were male and 293 (72.2%) were female. Meanwhile, 248 (60%) were married and 50% of the respondents had a Bachelor’s or a Master’s degree. A total of 95% percent of people consistently, often, or sometimes, followed the news related to COVID-19, while only 5% did not follow any news in this regard. The relatives of 77% of the participants had no history of catching the virus, 13.4% had recovered, 5.7% were infected during the study, and 3.9% had died because of COVID-19.
According to Table 1, all variables were in the normal range, and the following histogram diagram confirms the data (Figure 1).
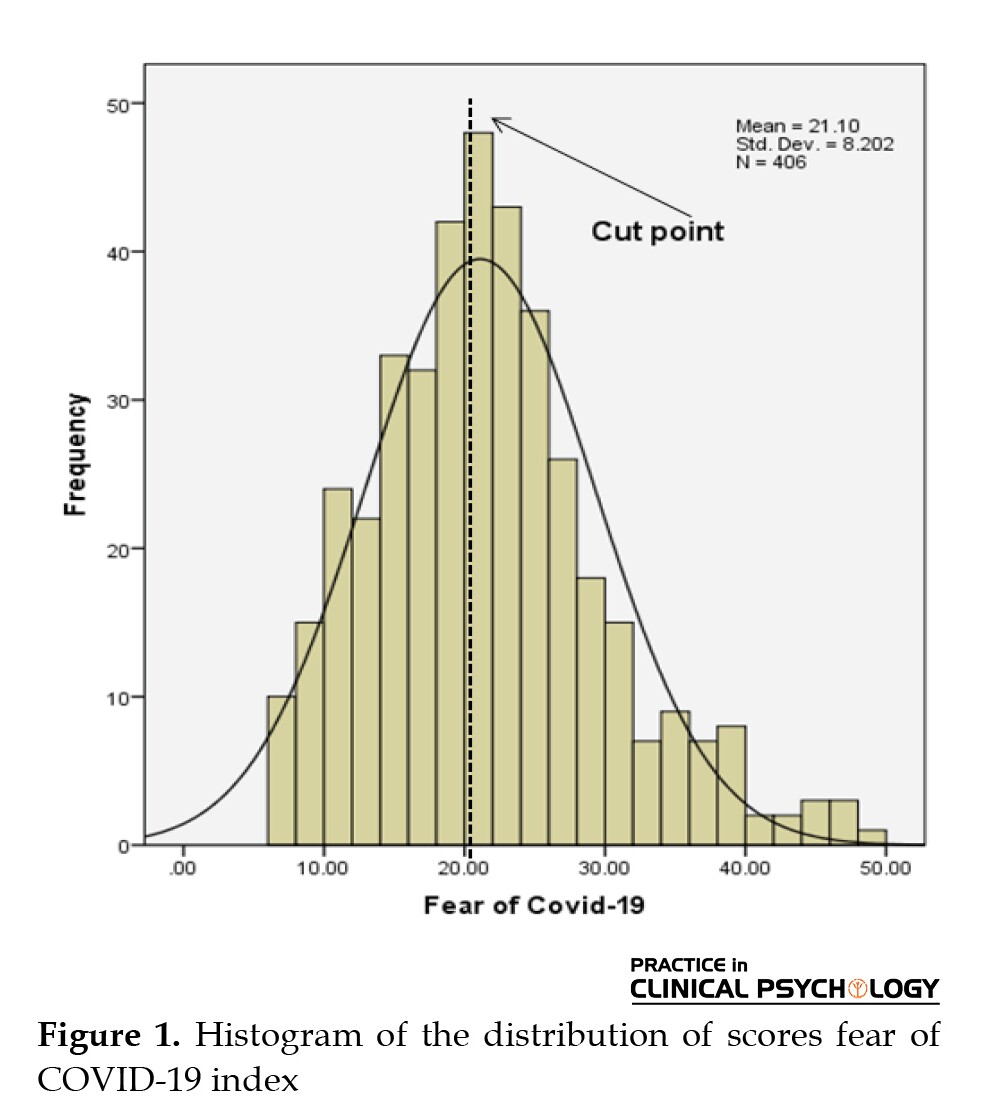
Participants were divided into two levels of low and high fear according to the cutoff point mean.

Then, the subscales of cognitive failure are compared in these two levels (Table 2). Additionally, to predict the fear of COVID-19 according to research variables, at first, the hypotheses related to stepwise regression analysis were tested. In addition to using the distance scale and normal distribution, the output of the Durbin–Watson test (1.89) indicates the presumption of observing the independence of the residuals.

Considering the index higher than 0.01 and the low level of variance inflation factor (VIF) in Table 3, no problem of multiple lines exists as a restriction for applying the regression method. Thus, to predict the fear of COVID-19, the age variables, following the COVID-19 news, and the 3 subscales of memory, distractibility, and false triggering as the predictor variable entered the regression equation.

According to Table 3, among the predictors that entered the regression equation, only the variables of following the news and memory can predict the fear of COVID-19, and other variables were excluded from the equation. Following the news, and memory could predict 14% of the fear of COVID-19 (R2=0.141, adjusted R2=0.137, P<0.01).
According to the β coefficients in Table 4, a negative relationship exists between fear of COVID-19 and following COVID-19 news; however, the relationship between fear of COVID-19 and memory error was positive and significant. Yet, the standard coefficients indicated that even though the effects of both variables were almost identical in changing the dependent variable (β= 0.281; t=5.89; β=-0.286; t=-6.09).

4. Discussion
The growing prevalence of COVID-19 has challenged global public health, leading to a morbid fear of infection in various populations. This research aimed to investigate the relationship between cognitive failure and the fear of COVID-19. The results showed a negative relationship between fear of COVID-19 and following COVID-19 news. This shows that with increasing follow-ups on COVID-19-related news, the fear of COVID-19 decreases. In explaining this finding, due to the nature of the exposure mechanism in this follow-up, people who follow COVID-19 news face negative fears and emotions, and because of the effectiveness of the fear mechanism (Abramowitz et al., 2019; Schäfer et al., 2018; Wannemueller et al., 2018), the fear is reduced. Also, because of the silence, their anxiety is reduced, which leads to the management of stress (Leong et al., 2015; Merz et al., 2014). In addition, gaining this information and exposure reduces ambiguity and uncertainty, and according to research, through this mechanism, the anxiety and fear of COVID-19 are reduced (Hebert & Dugas, 2019; Osmanağaoğlu et al., 2018; Shihata et al., 2017). The finding of this research about reducing fear and ambiguity while exposing stressful situations is the same as the finding of Schafer et al. (Schäfer et al., 2018), Merz et al. (Merz et al., 2014), and Hebert et al. (Hebert & Dugas, 2019).
Based on the results of the regression method in this study, the components of forgetfulness (memory) can predict the fear of COVID-19. Cognitive failure affects people’s mental health. False triggering, distractibility, and memory problems, which are the subscales of cognitive failure, can decrease a person’s mental health (Broadbent et al., 1982). In the current situation, the intervening issue can be considered the prevalence of COVID-19 and the fear of infection with it. In the present study, the forgetfulness subscale was significantly related to fear of COVID-19.
Based on the research literature, high cognitive failures can indicate a general ruminant approach, which may be the rate of vulnerability to negative emotions (Broadbent et al., 1982) and may also be associated with neuroticism (Zufferey et al., 2017) of anxiety traits (Merckelbach et al., 1996) and subsequent intolerance of uncertainty. Therefore, in explaining this finding, people who have shown memory failure do not record information about COVID-19 or suppress the information. This failure in memory causes obsessive-compulsive mental rumination, uncertainty, worry, fear, and anxiety that are associated with the virus; consequently, this uncertainty intolerance and rumination can cause stress or fear of COVID-19 or exacerbate the pre-existing condition. It has been found that cognitive failure is associated with negative emotions, especially stress and anxiety, fear, and neuroticism. That is in line with the finding of Broadbent et al. (Broadbent et al., 1982), Zufferey et al. (Zufferey et al., 2017), Matthews et al. (Matthews et al., 1990), and Mirza et al. (Mirza et al., 2017). Therefore, a relationship exists between cognitive processes that are associated with failure and a wide range of emotions, as well as fear, stress, and anxiety.
The hypothesis of the association of certain moods with errors in cognitive processing has already been proven (Payne & Schnapp, 2014), and mood is related to daily cognitive function (Schnapp, 2007). Negative emotional factors (such as fear, sadness, the feeling of guilt, and hostility) are significantly associated with the scores of distractibility, memory, and false triggering of the CFQ questionnaire as well as the total score of the questionnaire. Meanwhile, fear is one of the negative emotions that is correlated with high scores on the CFQ questionnaire. Thus, regarding the correlation between CFQ scores and negative emotions, one explanation is that the questionnaire measures a feature associated with complaining (or an aspect of neuroticism) that may overlap with experiencing negative emotion. Another explanation is that changes in cognition occur when cognitive resources are challenged by disturbing thoughts caused by stress and trauma (Payne & Schnapp, 2014). Also, experiencing negative emotions can cause susceptible individuals to recall and report more cognitive failures (Fisher et al., 2020).
CFQ is a tool for identifying vulnerable individuals (Payne & Schnapp, 2014). People with high scores in this questionnaire are vulnerable to stress (Matthews & Wells, 1988), and evidence suggests that cognitive failure affects the interpretation of stressful situations. The limitation of the present study was related to convenience sampling which reduces the generalizability of the results. Considering the COVID-19 pandemic conditions, the questionnaires were completed online, and we suggest using objective tools to assess cognitive failure.
5. Conclusion
The results indicate that the component of forgetfulness (memory) can predict the fear of COVID-19, and it is deduced in case of false triggering, distractibility, and memory problems, which are the subscales of cognitive failure and will decrease individuals’ mental health.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences with the Code of Ethics: IR.SBMU.MSP.REC.1400.303.
Funding
This study is supported by Shahid Beheshti University of Medical Sciences.
Authors' contributions
All authors equally contributed to preparing this article.
Conflict of interest
The authors report no competing interests to declare.
References
Abramowitz, J. S., Deacon, B. J., & Whiteside, S. P. H. (2019). Exposure therapy for anxiety: Principles and practice. New York: Guilford Publications [Link]
Ahorsu, D. K., Lin, C. Y., Imani, V., Saffari, M., Griffiths, M. D., & Pakpour, A. H. (2020). The fear of COVID-19 scale: Development and initial validation. International Journal of Mental Health and Addiction, 1-9. [DOI:10.1037/t78404-000]
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27-45. [DOI:10.1177/1073191105283504] [PMID]
Boomsma, D. I. (1998). Genetic analysis of cognitive failures (CFQ): A study of Dutch adolescent twins and their parents. European Journal of Personality, 12(5), 321-330. [DOI:10.1002/(SICI)1099-0984(1998090)12:5<321::AID-PER334>3.0.CO;2-5]
Broadbent, D. E., Broadbent, M. H., & Jones, J. L. (1986). Performance correlates of self‐reported cognitive failure and of obsessionality. British Journal of Clinical Psychology, 25(4), 285-299. [DOI:10.1111/j.2044-8260.1986.tb00708.x] [PMID]
Broadbent, D. E., Cooper, P. F., FitzGerald, P., & Parkes, K. R. (1982). The Cognitive Failures Questionnaire (CFQ) and its correlates. British Journal of Clinical Psychology, 21(1), 1-16. [DOI:10.1111/j.2044-8260.1982.tb01421.x] [PMID]
Carrigan, N., & Barkus, E. (2016). A systematic review of cognitive failures in daily life: Healthy populations. Neuroscience & Biobehavioral Reviews, 63, 29-42. [DOI:10.1016/j.neubiorev.2016.01.010] [PMID]
Etkin, A., Gyurak, A., & O’Hara, R. (2013). A neurobiological approach to the cognitive deficits of psychiatric disorders. Dialogues in Clinical Neuroscience, 15(4), 419-429. [PMID] [PMCID]
Fisher, J. E., Zhou, J., Liu, A. G., Fullerton, C. S., Ursano, R. J., & Cozza, S. J. (2020). Effect of comorbid anxiety and depression in complicated grief on perceived cognitive failures. Depression and Anxiety, 37(1), 54-62. [DOI:10.1002/da.22943] [PMID]
Gonçalves, L. C., Vale, R. G., Barata, N. J., Varejão, R. V., & Dantas, E. H. (2011). Flexibility, functional autonomy and quality of life (QoL) in elderly yoga practitioners. Archives of Gerontology and Geriatrics, 53(2), 158-162. [DOI:10.1016/j.archger.2010.10.028] [PMID]
Hebert, E. A., & Dugas, M. J. (2019). Behavioral experiments for intolerance of uncertainty: Challenging the unknown in the treatment of generalized anxiety disorder. Cognitive and Behavioral Practice, 26(2), 421-436. [DOI:10.1016/j.cbpra.2018.07.007]
Huang, Y., & Zhao, N. (2020). Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Research, 288, 112954. [DOI:10.1016/j.psychres.2020.112954] [PMID] [PMCID]
Jahangasht, K. (2020). [Social stigma: The social consequences of covid-19 (Persian)]. Journal of Marine Medicine, 2(1), 59-60. [Link]
Keshvari, F., Heshmati, P., & Ghasemian-Shirvan, E. (2017). [The role of prefrotal cortex in subjective mood: A transcranial direct current stimulation study (Persian)]. Journal of Research in Psychological Health, 11(1), 25-38. [DOI:10.29252/rph.11.1.25]
Kim, S. W., & Su, K. P. (2020). Using psychoneuroimmunity against COVID-19. Brain, Behavior, and Immunity, 87, 4-5. [DOI:10.1016/j.bbi.2020.03.025] [PMID] [PMCID]
Leong, K. C., Goodman, J., & Packard, M. G. (2015). Post-training re-exposure to fear conditioned stimuli enhances memory consolidation and biases rats toward the use of dorsolateral striatum-dependent response learning. Behavioural Brain Research, 291, 195-200. [DOI:10.1016/j.bbr.2015.05.022] [PMID]
Mamun, M. A., & Griffiths, M. D. (2020). First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: Possible suicide prevention strategies. Asian Journal of Psychiatry, 51, 102073. [DOI:10.1016/j.ajp.2020.102073] [PMID] [PMCID]
Matthews, G., Coyle, K., & Craig, A. (1990). Multiple factors of cognitive failure and their relationships with stress vulnerability. Journal of Psychopathology and Behavioral Assessment, 12(1), 49-65. [DOI:10.1007/BF00960453]
Matthews, G., & Wells, A. (1988). Relationships between anxiety, self-consciousness, and cognitive failure. Cognition and Emotion, 2(2), 123-132. [DOI:10.1080/02699938808408069]
Merckelbach, H., Muris, P., Nijman, H., & de Jong, P. J. (1996). Self-reported cognitive failures and neurotic symptomatology. Personality and Individual Differences, 20(6), 715-724. [DOI:10.1016/0191-8869(96)00024-4]
Merz, C. J., Hamacher-Dang, T. C., & Wolf, O. T. (2014). Exposure to stress attenuates fear retrieval in healthy men. Psychoneuroendocrinology, 41, 89-96. [DOI:10.1016/j.psyneuen.2013.12.009] [PMID]
Miller, E. K., & Cohen, J. D. (2001). An integrative theory of prefrontal cortex function. Annual Review of Neuroscience, 24, 167-202. [DOI:10.1146/annurev.neuro.24.1.167] [PMID]
Mirza, S. S., Ikram, M. A., Bos, D., Mihaescu, R., Hofman, A., & Tiemeier, H. (2017). Mild cognitive impairment and risk of depression and anxiety: A population-based study. Alzheimer’s & Dementia, 13(2), 130-139. [DOI:10.1016/j.jalz.2016.06.2361] [PMID]
Moghanibashi-Mansourieh, A. (2020). Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian Journal of Psychiatry, 51, 102076. [PMID] [PMCID]
Nooraei, S., Entezari, M., Hushmandi, K., & Raei, M. (2020). [Stress and anxiety caused by covid-19 in the communities (Persian)]. Journal of Marine Medicine, 2(1), 65-66. [Link]
Osmanağaoğlu, N., Creswell, C., & Dodd, H. F. (2018). Intolerance of Uncertainty, anxiety, and worry in children and adolescents: A meta-analysis. Journal of Affective Disorders, 225, 80-90. [PMID]
Payne, T. W., & Schnapp, M. A. (2014). The relationship between negative affect and reported cognitive failures. Depression Research and Treatment, 2014, 396195. [PMID] [PMCID]
Rast, P., Zimprich, D., Van Boxtel, M., & Jolles, J. (2009). Factor structure and measurement invariance of the cognitive failures questionnaire across the adult life span. Assessment, 16(2), 145-158. [DOI:10.1177/1073191108324440] [PMID]
Sahoo, S., Rani, S., Parveen, S., Pal Singh, A., Mehra, A., & Chakrabarti, S., et al. (2020). Self-harm and COVID-19 pandemic: An emerging concern-A report of 2 cases from India. Asian Journal of Psychiatry, 51, 102104. [PMID] [PMCID]
Schäfer, S. K., Ihmig, F. R., Lara H, K. A., Neurohr, F., Kiefer, S., & Staginnus, M., et al. (2018). Effects of heart rate variability biofeedback during exposure to fear-provoking stimuli within spider-fearful individuals: Study protocol for a randomized controlled trial. Trials, 19(1), 184. [DOI:10.1186/s13063-018-2554-2] [PMID] [PMCID]
Schnapp, M. (2007). Affect and cognitive failures: A comparison of positive and negative mood factors. Kenyon Summer Science Scholars Program, 364. [Link]
Shahed hagh ghadam, H., Fathi Ashtiani, A., Rahnejat, A. M., Ahmadi Tahour Soltani, M., Taghva, A., & Ebrahimi, M. R., et al. (2020). [Psychological consequences and interventions during the covid-19 pandemic: Narrative review (Persian)]. Journal of Marine Medicine, 2(1), 1-11. [DOI:10.30491/2.1.7]
Shihata, S., McEvoy, P. M., & Mullan, B. A. (2017). Pathways from uncertainty to anxiety: An evaluation of a hierarchical model of trait and disorder-specific intolerance of uncertainty on anxiety disorder symptoms. Journal of Anxiety Disorders, 45, 72-79. [DOI:10.1016/j.janxdis.2016.12.001] [PMID]
Steele, J. D., & Lawrie, S. M. (2004). Segregation of cognitive and emotional function in the prefrontal cortex: A stereotactic meta-analysis. Neuroimage, 21(3), 868-875. [DOI:10.1016/j.neuroimage.2003.09.066] [PMID]
Tirre, W. C. (2018). Dimensionality and determinants of self-reported cognitive failures. International Journal of Psychological Research, 11(1), 9-18. [PMID] [PMCID]
Mesa Vieira, C., Franco, O. H., Gómez Restrepo, C., & Abel, T. (2020). COVID-19: The forgotten priorities of the pandemic. Maturitas, 136, 38-41. [PMID] [PMCID]
Wannemueller, A., Moser, D., Kumsta, R., Jöhren, H. P., Adolph, D., & Margraf, J. (2018). Mechanisms, genes and treatment: Experimental fear conditioning, the serotonin transporter gene, and the outcome of a highly standardized exposure-based fear treatment. Behaviour Research and Therapy, 107, 117-126. [DOI:10.1016/j.brat.2018.06.003] [PMID]
Widge, A. S., Zorowitz, S., Basu, I., Paulk, A. C., Cash, S. S., & Eskandar, E. N., et al. (2019). Deep brain stimulation of the internal capsule enhances human cognitive control and prefrontal cortex function. Nature Communications, 10(1), 1536. [PMID] [PMCID]
Zhu, Z., Xu, S., Wang, H., Liu, Z., Wu, J., & Li, G., et al. (2020). COVID-19 in Wuhan: Immediate psychological impact on 5062 health workers. MedRxiv, 1-24. [DOI:10.1101/2020.02.20.20025338]
Zufferey, V., Donati, A., Popp, J., Meuli, R., Rossier, J., & Frackowiak, R., et al. (2017). Neuroticism, depression, and anxiety traits exacerbate the state of cognitive impairment and hippocampal vulnerability to Alzheimer’s disease. Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring, 7, 107-114. [PMID]
Type of Study: Research |
Subject:
Psychiatry
Received: 2022/03/5 | Accepted: 2022/11/5 | Published: 2023/01/4
Received: 2022/03/5 | Accepted: 2022/11/5 | Published: 2023/01/4
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





