Volume 7, Issue 2 (Spring 2019)
PCP 2019, 7(2): 125-136 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kiani A, Ramezani S, Atadokht A. Predicting Suicidality and Addictions Among University Students Based on Adverse Childhood Experiences and Exposure to Family Members’ and Friends’ Suicide. PCP 2019; 7 (2) :125-136
URL: http://jpcp.uswr.ac.ir/article-1-623-en.html
URL: http://jpcp.uswr.ac.ir/article-1-623-en.html
1- Department of Counseling, Faculty of Education and Psychology, University of Mohaghegh Ardabili, Ardabili, Iran. , ahmadreza_kiani@yahoo.com
2- Department of Counseling, Faculty of Education and Psychology, University of Mohaghegh Ardabili, Ardabili, Iran.
3- Department of Psychology, Faculty of Education and Psychology, University of Mohaghegh Ardabili, Ardabili, Iran.
2- Department of Counseling, Faculty of Education and Psychology, University of Mohaghegh Ardabili, Ardabili, Iran.
3- Department of Psychology, Faculty of Education and Psychology, University of Mohaghegh Ardabili, Ardabili, Iran.
Full-Text [PDF 695 kb]
(1589 Downloads)
| Abstract (HTML) (3381 Views)
Full-Text: (1603 Views)
1. Introduction
uicide is the second leading cause of mortality in youth and adolescents, aged 15 to 29 years, throughout the world (Ma, Batterham, Calear, & Han, 2016). Also, 20-25 non-fatal suicide attempts occur for every one successful suicide (Maltsberger, 2003). Entrance to college can be stressful for students because this period involves a transition from adolescence to adulthood (Arnett, 2000). Therefore, they are at high risk for suicidal ideation (SI), planning, and attempts (Eskin et al. 2016). Approximately one out of four to six college students have reported some form of SI during college education (Mortier et al. 2018). In recent years, the prevalence of suicide in Iran has increased, and calls for special attention (Kiani Chelmardi, Rashid, Honarmand, & Tamook, 2018). Research suggests that the suicide rate is approximately 10 in 100000 people in Iran in the past two decades (Hassanian- Moghaddam & Zamani, 2017).
Adverse Childhood Experiences (ACEs) are among the factors that have a critical impact on suicide. The researchers have shown that ACEs are correlated with mental health problems in children and adolescents (Oladeji, Makanjuola, & Gureje, 2010) and especially with suicide. The ACEs include emotional, physical, and sexual abuse; emotional and physical neglect; witnessing domestic violence; parental separation or divorce; and living with a substance-abusing, mentally ill, or criminal household member (Schilling, Aseltine, & Gore, 2007). To date, the ACEs studies have repeatedly shown that traumatic and stressful childhood events increase the likelihood of myriad adolescent risk behaviors, such as regular smoking by the age 14 (Anda et al., 1999), attempted suicide and use of illicit drugs (Dube et al., 2003).
Some retrospective studies have investigated the effect of various ACEs, as risk factors for psychiatric disorders with suicidal behavior in adulthood (Chapman et al., 2004). For instance, one study has shown that women who were exposed to sexual abuse before the age 16, have the probability of taking suicide attempts, some time in their lives, and 18 times more than women without such experiences. Also, a higher number of ACEs significantly increases suicide risk throughout the lifespan. For example, people with three ACEs are 8 times more likely to take a suicide attempt in childhood or adolescent. Various research observations support the effect of ACEs on the biological and mental development of children and adolescents and show that brain development is probably influenced by ACEs (Sher, 2017).
Another factor that can increase the risk of suicidality is witnessing others’ suicide and self-harm behaviors. Dhingra, Boduszek, & O’Connor (2016) research indicates that witnessing suicide and not being afraid of death has a positive relationship with a suicide attempt. Here, Joiner’s term of “acquired capability” is proposed, that is a volitional moderator. This concept refers to a person’s ability for enacting suicide desire or utilizing fatal self-injury that is increased by exposure and habituation to self-injury behaviors (Van Orden, Witte, Gordon, Bender, & Joiner. 2008). In O’Conner’s model of suicide, shifting suicide thoughts to behavior is affected by enacting behavior that includes access to lethal means, acquired capability (fearless about death and lack of sensitivity to pain), and witnessing others’ self-harm behaviors and impulsivity (Dhingra et al., 2016). It means that exposure to friends’ or family members’ suicide attempts can increase the capacity for suicide, and subsequently, this higher capacity leads to losing the fear of death and lacking sensitivity to pain.
Drug addiction; as a social, mental, and health problem; is a crisis in the 21st century. It is also one of the most important triggering factors of high-risk behaviors (Dehshiri & Moosavi, 2015). Death statistics throughout the world due to drug and substance abuse calls for excessive attention of health professions (Becker, & Fiellin, 2017). Studies show that alcohol and substance addicts attempt to commit suicide 5 to 10 times more than normal people (Voss et al., 2012). Research has shown that children and adolescents affected by parental drug use have more drug problems (Hill, Tessner, McDermott, 2011). With regard to substance use problems, their records often show an early onset of substance use (Rothman, Edwards, Heeren, Hingson, 2008), increased binge drinking rates (Weitzman & Wechsler, 2000), and higher risk of developing substance use disorders at a younger age than their peers (Hussong, Bauer, & Chassin, 2008). Approximately 33% to 40% of all children with an addicted parent will develop a substance use disorder themselves (Parolin, Simonelli, Mapelli, Sacco, Cristofalo, 2016).
ACEs are the main factors in the tendency toward addiction (Quinn et al., 2016). Retrospective self-report data have shown that ACEs are key factors in the etiology of illegal drugs abuse (Anda et al., 2006) and can be responsible for half to two-thirds of problems related to the substance abuse in adulthood (Dube et al., 2003).
In 1998, Keiser and CDC foundation reported that people who suffered from three or more ACEs, are more likely involved in substance abuse, domestic violence, and suicide attempt and are also more likely involved in taking divorce, catching diabetes, being obese, catching cancer and heart disease. More recent studies found a definite relationship between ACEs and substance abuse. For example, one study in 2016 showed a clear relationship between the number of childhood traumatic experiences and an increase in the risk of substance abuse in adulthood. People who reported five or more ACEs were exposed to substance abuse, and their likelihood of using injective drugs was three times more than normal people (Quinn et al., 2016). Another study indicates that above 80% of patients that were searching for a treatment of drug abuse, experienced at least one type of childhood traumas and two-thirds of them had witnessed violence in childhood (Tsavoussis, Stawicki, Stoicea, & Papadimos, 2014). In Iran, addiction was recognized as an important medical and social emergency. Despite the huge therapeutic cost, which spends each year, the government has not attained any success in reducing or controlling addiction.
In 2001, it was reported that 1.5 million people in Iran had substance dependency (Yasamy et al., 2001). This number has increased to 10 million by now. Opioid use and opium, in particular, were the most common abuse disorder among Iranian students in 2016 (Amin‐Esmaeili et al., 2016). Unfortunately, there has not been a transparent understanding of the etiology and incidence of addiction phenomena in our country. Besides, suicide is a serious public health concern that needs more attention in Iran, as its rate is increasing, especially among the 15-24 years old group. This group has the highest rate of suicide per 100000 people in Iran (Veisani, Delpisheh, Mohamadian, Valizadeh, 2018). Although previous studies have investigated drug abuse in Iran (Kabir et al., 2018), no study is available on the impact of ACEs on drug abuse behaviors, particularly among university students.
As mentioned earlier, suicide and addiction are the two most important risk behaviors among Iranian students, and ACEs certainly play an essential part in creating these two phenomena. However, no research has been carried out to highlight the most important role of ACEs on high-risk behaviors such as suicide and addiction, in adolescents in Iran. Therefore, acquiring in-depth knowledge and designing prevention strategies for suicide and addiction is an important issue in our society, especially for college students who are more vulnerable to suicide (Rashid, Khorramdel, Gholami, & Senobar, 2016) and addiction (Kabir et al., 2018). Considering that suicide and addiction are really serious social harms, this research aims to predict suicidality and addiction (substance, alcohol, cigarette, psychoactive drugs) among Iranian university students based on adverse childhood experiences and witnessing others’ suicide.
2. Methods
The study procedure is cross-sectional. The statistical community included all students of the University of Mohaghegh Ardabili, Ardabil City, Iran, in 2017.
As our community comprised about 12000 students, based on Cochran’s sample size formula and considering the power of generalization, a sample of 500 people was selected by convenience sampling method. The inclusion criteria included being 18-45 years old, studying at university, and being interested in participating in the research. Ethical consideration included information confidentiality, informed consent, and right of being aware of research output. In the procedure, first, the researcher referred to the classrooms and described the purpose of research, the importance of suicide, and then explained the informed consent and confidentiality. After that, he asked the potential participants to complete the questionnaires and returned them to the researcher. The researcher also said to the participants that they could return the questionnaire if they were not interested in completing it. In the next step, the obtained data were entered in SPSS and analyzed by Pearson correlation and regression analyses. In this study, we used the following measures:
Depressive Symptom-Suicidality Subscale (DSI-SS) assesses the frequency and intensity of suicidal thoughts at the current time. Overall scores of answers evaluate the severity of suicide ideation ranging from 0 to 3 (for the present study; Mean±SD=1.01±1.096). Two studies reported the excellent internal consistency, convergent validity, and ability to differentiate attempters and non-attempters in the general population (Joiner, Pfaff, & Acres, 2002; Von Glischinski, Teismann, Prinz, Gebauer, & Hirschfeld, 2016). The original study (Joiner et al., 2002) proposed the cut-off point of three, but later von Glischinski et al. (2016) stated that the best cut-off point for the general population is 2.
Adverse Childhood Experiences (ACE) were assessed by the ACE questionnaire (Anda, Butchart, Felitti, & Brown, 2010) which addresses 10 individual ACEs under three categories: 1. Abuse: Emotional, physical, and sexual abuse; 2. Neglect: Emotional and physical neglect; and 3. Household dysfunction: Parental separation/ divorce, violence against mother, household substance abuse, household mental illness and incarceration of household member. The ACE questionnaire is a reliable and valid measure of childhood adversity that has been used extensively in large-scale ACE studies (Centers for Disease Control and Prevention NCfIPaC, 2014). All questions about ACEs pertained to the respondents’ first 18 years of life and were binary (Yes or No). Out of these, a dichotomous variable was created to reflect exposure to any ACE, and similar variables were created to reflect any exposure to each ACE subtype (abuse, neglect, household dysfunction). One of the questions, for example, is: “while you were growing up, during your first 18 years of life, did a parent or other adult in the household often or very often push, grab, slab, or throw something at you? or ever hit you so hard that you had marks or were injured? Yes ___ No___”.
In this part, 4 questions are asked: “During the last month, how many times did you use cigarette or tobacco?”, “During the last month, how many times did you use alcohol or its derivatives?”, “During the last month, how many times did you use substance?”, “During the last month, how many times did you use psychoactive drugs (such as cannabis, Ritalin, or street drugs)?” Responses are rated from 0 to 3. (0= Not at all; 1=one time in several weeks; 2=More than one time in several days; 3=Every day). The higher score indicates higher use of that substance.
Exposure to Suicidal Behavior (ESB) was the other scale. Based on Dhingra et al. (2016) and O’Connor, Rasmussen, & Hawton (2012) research, two items were used to find out about the likelihood of individual’s exposure to family members’ or friends’ suicide or self-injurious behaviors. Questions were “Has anyone among your close friends/your family members ever attempted suicide or deliberately harmed himself or herself?”. In O’Connor, Armitage, & Gray (2006) research, the Cronbach’s α for the scale was 0.92 and in the current research, it was 0.83.
3. Results
Descriptive data
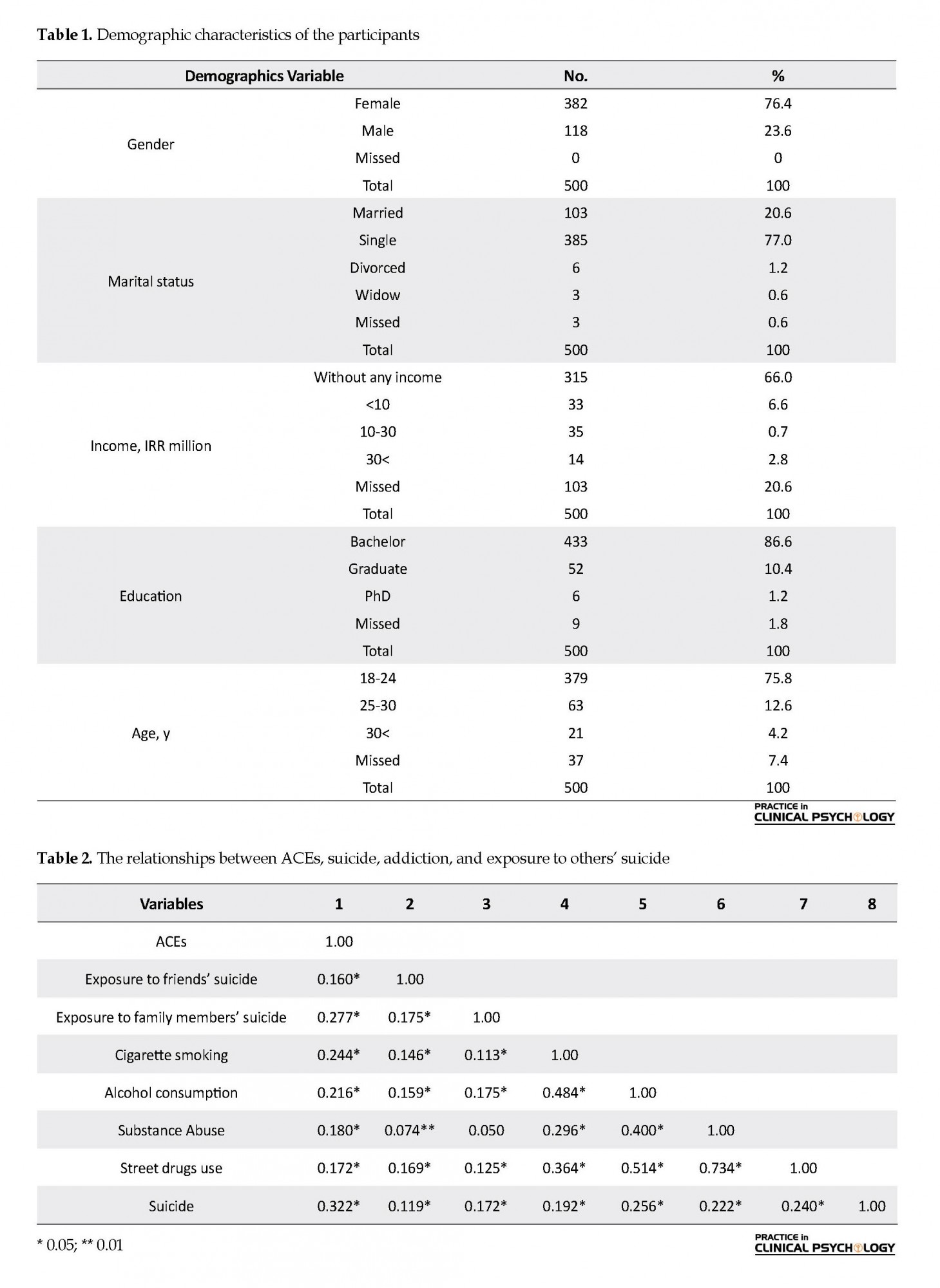
First, Table 1 presents the demographic information of the participants. Then, the correlation between research variables was assessed, and finally, the regression models were used to predict suicide and addition based on adverse childhood experiences and exposure to family members’ or friends’ suicide.
According to Table 1, most participants was female (n=382), single (n=385), without any income (n=315), studying bachelor’ degree (n=433), and aged between 18 and 24 years (n=379). Table 2 presents the relationships between the research variables. Table 2 presents the associations between ACEs, suicide, addiction, and exposure to suicide. As shown in Table 2, ACEs had significant correlation with suicide (r=0.322), cigarette smoking (r=0.244), alcohol consumption (r=0.216), substance abuse (r=0.180), and street drugs (r= 0.172) (P<0.01). Besides, the relationship between suicide and exposure to friends’ suicide (r=0.119) and exposure to family members’ suicide (r=0.172) was significant. Exposure to friends’ suicide had significant correlation with cigarette smoking (r=0.146), alcohol consumption (r=0.159), substance abuse (r=0.074), and street drugs use (r=0.169). However, there was no significant correlation between exposure to family members’ suicide with substance abuse (r=0.050). Summary of regression analyses for predicting suicide based on ACEs and exposure to family member’s and friends’ suicide are presented in Table 3. As noted in Table 3, ACEs and exposure to family members’ and friends’ suicide can predict suicide, and these two variables can explain 14% variance of suicide. According to Table 4, of the 3 variables (exposure to family members’ suicide, exposure to friends’ suicide, and ACEs), ACEs variable (t=6.617, β=0.235) can predict suicide significantly.
uicide is the second leading cause of mortality in youth and adolescents, aged 15 to 29 years, throughout the world (Ma, Batterham, Calear, & Han, 2016). Also, 20-25 non-fatal suicide attempts occur for every one successful suicide (Maltsberger, 2003). Entrance to college can be stressful for students because this period involves a transition from adolescence to adulthood (Arnett, 2000). Therefore, they are at high risk for suicidal ideation (SI), planning, and attempts (Eskin et al. 2016). Approximately one out of four to six college students have reported some form of SI during college education (Mortier et al. 2018). In recent years, the prevalence of suicide in Iran has increased, and calls for special attention (Kiani Chelmardi, Rashid, Honarmand, & Tamook, 2018). Research suggests that the suicide rate is approximately 10 in 100000 people in Iran in the past two decades (Hassanian- Moghaddam & Zamani, 2017).
Adverse Childhood Experiences (ACEs) are among the factors that have a critical impact on suicide. The researchers have shown that ACEs are correlated with mental health problems in children and adolescents (Oladeji, Makanjuola, & Gureje, 2010) and especially with suicide. The ACEs include emotional, physical, and sexual abuse; emotional and physical neglect; witnessing domestic violence; parental separation or divorce; and living with a substance-abusing, mentally ill, or criminal household member (Schilling, Aseltine, & Gore, 2007). To date, the ACEs studies have repeatedly shown that traumatic and stressful childhood events increase the likelihood of myriad adolescent risk behaviors, such as regular smoking by the age 14 (Anda et al., 1999), attempted suicide and use of illicit drugs (Dube et al., 2003).
Some retrospective studies have investigated the effect of various ACEs, as risk factors for psychiatric disorders with suicidal behavior in adulthood (Chapman et al., 2004). For instance, one study has shown that women who were exposed to sexual abuse before the age 16, have the probability of taking suicide attempts, some time in their lives, and 18 times more than women without such experiences. Also, a higher number of ACEs significantly increases suicide risk throughout the lifespan. For example, people with three ACEs are 8 times more likely to take a suicide attempt in childhood or adolescent. Various research observations support the effect of ACEs on the biological and mental development of children and adolescents and show that brain development is probably influenced by ACEs (Sher, 2017).
Another factor that can increase the risk of suicidality is witnessing others’ suicide and self-harm behaviors. Dhingra, Boduszek, & O’Connor (2016) research indicates that witnessing suicide and not being afraid of death has a positive relationship with a suicide attempt. Here, Joiner’s term of “acquired capability” is proposed, that is a volitional moderator. This concept refers to a person’s ability for enacting suicide desire or utilizing fatal self-injury that is increased by exposure and habituation to self-injury behaviors (Van Orden, Witte, Gordon, Bender, & Joiner. 2008). In O’Conner’s model of suicide, shifting suicide thoughts to behavior is affected by enacting behavior that includes access to lethal means, acquired capability (fearless about death and lack of sensitivity to pain), and witnessing others’ self-harm behaviors and impulsivity (Dhingra et al., 2016). It means that exposure to friends’ or family members’ suicide attempts can increase the capacity for suicide, and subsequently, this higher capacity leads to losing the fear of death and lacking sensitivity to pain.
Drug addiction; as a social, mental, and health problem; is a crisis in the 21st century. It is also one of the most important triggering factors of high-risk behaviors (Dehshiri & Moosavi, 2015). Death statistics throughout the world due to drug and substance abuse calls for excessive attention of health professions (Becker, & Fiellin, 2017). Studies show that alcohol and substance addicts attempt to commit suicide 5 to 10 times more than normal people (Voss et al., 2012). Research has shown that children and adolescents affected by parental drug use have more drug problems (Hill, Tessner, McDermott, 2011). With regard to substance use problems, their records often show an early onset of substance use (Rothman, Edwards, Heeren, Hingson, 2008), increased binge drinking rates (Weitzman & Wechsler, 2000), and higher risk of developing substance use disorders at a younger age than their peers (Hussong, Bauer, & Chassin, 2008). Approximately 33% to 40% of all children with an addicted parent will develop a substance use disorder themselves (Parolin, Simonelli, Mapelli, Sacco, Cristofalo, 2016).
ACEs are the main factors in the tendency toward addiction (Quinn et al., 2016). Retrospective self-report data have shown that ACEs are key factors in the etiology of illegal drugs abuse (Anda et al., 2006) and can be responsible for half to two-thirds of problems related to the substance abuse in adulthood (Dube et al., 2003).
In 1998, Keiser and CDC foundation reported that people who suffered from three or more ACEs, are more likely involved in substance abuse, domestic violence, and suicide attempt and are also more likely involved in taking divorce, catching diabetes, being obese, catching cancer and heart disease. More recent studies found a definite relationship between ACEs and substance abuse. For example, one study in 2016 showed a clear relationship between the number of childhood traumatic experiences and an increase in the risk of substance abuse in adulthood. People who reported five or more ACEs were exposed to substance abuse, and their likelihood of using injective drugs was three times more than normal people (Quinn et al., 2016). Another study indicates that above 80% of patients that were searching for a treatment of drug abuse, experienced at least one type of childhood traumas and two-thirds of them had witnessed violence in childhood (Tsavoussis, Stawicki, Stoicea, & Papadimos, 2014). In Iran, addiction was recognized as an important medical and social emergency. Despite the huge therapeutic cost, which spends each year, the government has not attained any success in reducing or controlling addiction.
In 2001, it was reported that 1.5 million people in Iran had substance dependency (Yasamy et al., 2001). This number has increased to 10 million by now. Opioid use and opium, in particular, were the most common abuse disorder among Iranian students in 2016 (Amin‐Esmaeili et al., 2016). Unfortunately, there has not been a transparent understanding of the etiology and incidence of addiction phenomena in our country. Besides, suicide is a serious public health concern that needs more attention in Iran, as its rate is increasing, especially among the 15-24 years old group. This group has the highest rate of suicide per 100000 people in Iran (Veisani, Delpisheh, Mohamadian, Valizadeh, 2018). Although previous studies have investigated drug abuse in Iran (Kabir et al., 2018), no study is available on the impact of ACEs on drug abuse behaviors, particularly among university students.
As mentioned earlier, suicide and addiction are the two most important risk behaviors among Iranian students, and ACEs certainly play an essential part in creating these two phenomena. However, no research has been carried out to highlight the most important role of ACEs on high-risk behaviors such as suicide and addiction, in adolescents in Iran. Therefore, acquiring in-depth knowledge and designing prevention strategies for suicide and addiction is an important issue in our society, especially for college students who are more vulnerable to suicide (Rashid, Khorramdel, Gholami, & Senobar, 2016) and addiction (Kabir et al., 2018). Considering that suicide and addiction are really serious social harms, this research aims to predict suicidality and addiction (substance, alcohol, cigarette, psychoactive drugs) among Iranian university students based on adverse childhood experiences and witnessing others’ suicide.
2. Methods
The study procedure is cross-sectional. The statistical community included all students of the University of Mohaghegh Ardabili, Ardabil City, Iran, in 2017.
As our community comprised about 12000 students, based on Cochran’s sample size formula and considering the power of generalization, a sample of 500 people was selected by convenience sampling method. The inclusion criteria included being 18-45 years old, studying at university, and being interested in participating in the research. Ethical consideration included information confidentiality, informed consent, and right of being aware of research output. In the procedure, first, the researcher referred to the classrooms and described the purpose of research, the importance of suicide, and then explained the informed consent and confidentiality. After that, he asked the potential participants to complete the questionnaires and returned them to the researcher. The researcher also said to the participants that they could return the questionnaire if they were not interested in completing it. In the next step, the obtained data were entered in SPSS and analyzed by Pearson correlation and regression analyses. In this study, we used the following measures:
Depressive Symptom-Suicidality Subscale (DSI-SS) assesses the frequency and intensity of suicidal thoughts at the current time. Overall scores of answers evaluate the severity of suicide ideation ranging from 0 to 3 (for the present study; Mean±SD=1.01±1.096). Two studies reported the excellent internal consistency, convergent validity, and ability to differentiate attempters and non-attempters in the general population (Joiner, Pfaff, & Acres, 2002; Von Glischinski, Teismann, Prinz, Gebauer, & Hirschfeld, 2016). The original study (Joiner et al., 2002) proposed the cut-off point of three, but later von Glischinski et al. (2016) stated that the best cut-off point for the general population is 2.
Adverse Childhood Experiences (ACE) were assessed by the ACE questionnaire (Anda, Butchart, Felitti, & Brown, 2010) which addresses 10 individual ACEs under three categories: 1. Abuse: Emotional, physical, and sexual abuse; 2. Neglect: Emotional and physical neglect; and 3. Household dysfunction: Parental separation/ divorce, violence against mother, household substance abuse, household mental illness and incarceration of household member. The ACE questionnaire is a reliable and valid measure of childhood adversity that has been used extensively in large-scale ACE studies (Centers for Disease Control and Prevention NCfIPaC, 2014). All questions about ACEs pertained to the respondents’ first 18 years of life and were binary (Yes or No). Out of these, a dichotomous variable was created to reflect exposure to any ACE, and similar variables were created to reflect any exposure to each ACE subtype (abuse, neglect, household dysfunction). One of the questions, for example, is: “while you were growing up, during your first 18 years of life, did a parent or other adult in the household often or very often push, grab, slab, or throw something at you? or ever hit you so hard that you had marks or were injured? Yes ___ No___”.
In this part, 4 questions are asked: “During the last month, how many times did you use cigarette or tobacco?”, “During the last month, how many times did you use alcohol or its derivatives?”, “During the last month, how many times did you use substance?”, “During the last month, how many times did you use psychoactive drugs (such as cannabis, Ritalin, or street drugs)?” Responses are rated from 0 to 3. (0= Not at all; 1=one time in several weeks; 2=More than one time in several days; 3=Every day). The higher score indicates higher use of that substance.
Exposure to Suicidal Behavior (ESB) was the other scale. Based on Dhingra et al. (2016) and O’Connor, Rasmussen, & Hawton (2012) research, two items were used to find out about the likelihood of individual’s exposure to family members’ or friends’ suicide or self-injurious behaviors. Questions were “Has anyone among your close friends/your family members ever attempted suicide or deliberately harmed himself or herself?”. In O’Connor, Armitage, & Gray (2006) research, the Cronbach’s α for the scale was 0.92 and in the current research, it was 0.83.
3. Results
Descriptive data
First, Table 1 presents the demographic information of the participants. Then, the correlation between research variables was assessed, and finally, the regression models were used to predict suicide and addition based on adverse childhood experiences and exposure to family members’ or friends’ suicide.
According to Table 1, most participants was female (n=382), single (n=385), without any income (n=315), studying bachelor’ degree (n=433), and aged between 18 and 24 years (n=379). Table 2 presents the relationships between the research variables. Table 2 presents the associations between ACEs, suicide, addiction, and exposure to suicide. As shown in Table 2, ACEs had significant correlation with suicide (r=0.322), cigarette smoking (r=0.244), alcohol consumption (r=0.216), substance abuse (r=0.180), and street drugs (r= 0.172) (P<0.01). Besides, the relationship between suicide and exposure to friends’ suicide (r=0.119) and exposure to family members’ suicide (r=0.172) was significant. Exposure to friends’ suicide had significant correlation with cigarette smoking (r=0.146), alcohol consumption (r=0.159), substance abuse (r=0.074), and street drugs use (r=0.169). However, there was no significant correlation between exposure to family members’ suicide with substance abuse (r=0.050). Summary of regression analyses for predicting suicide based on ACEs and exposure to family member’s and friends’ suicide are presented in Table 3. As noted in Table 3, ACEs and exposure to family members’ and friends’ suicide can predict suicide, and these two variables can explain 14% variance of suicide. According to Table 4, of the 3 variables (exposure to family members’ suicide, exposure to friends’ suicide, and ACEs), ACEs variable (t=6.617, β=0.235) can predict suicide significantly.
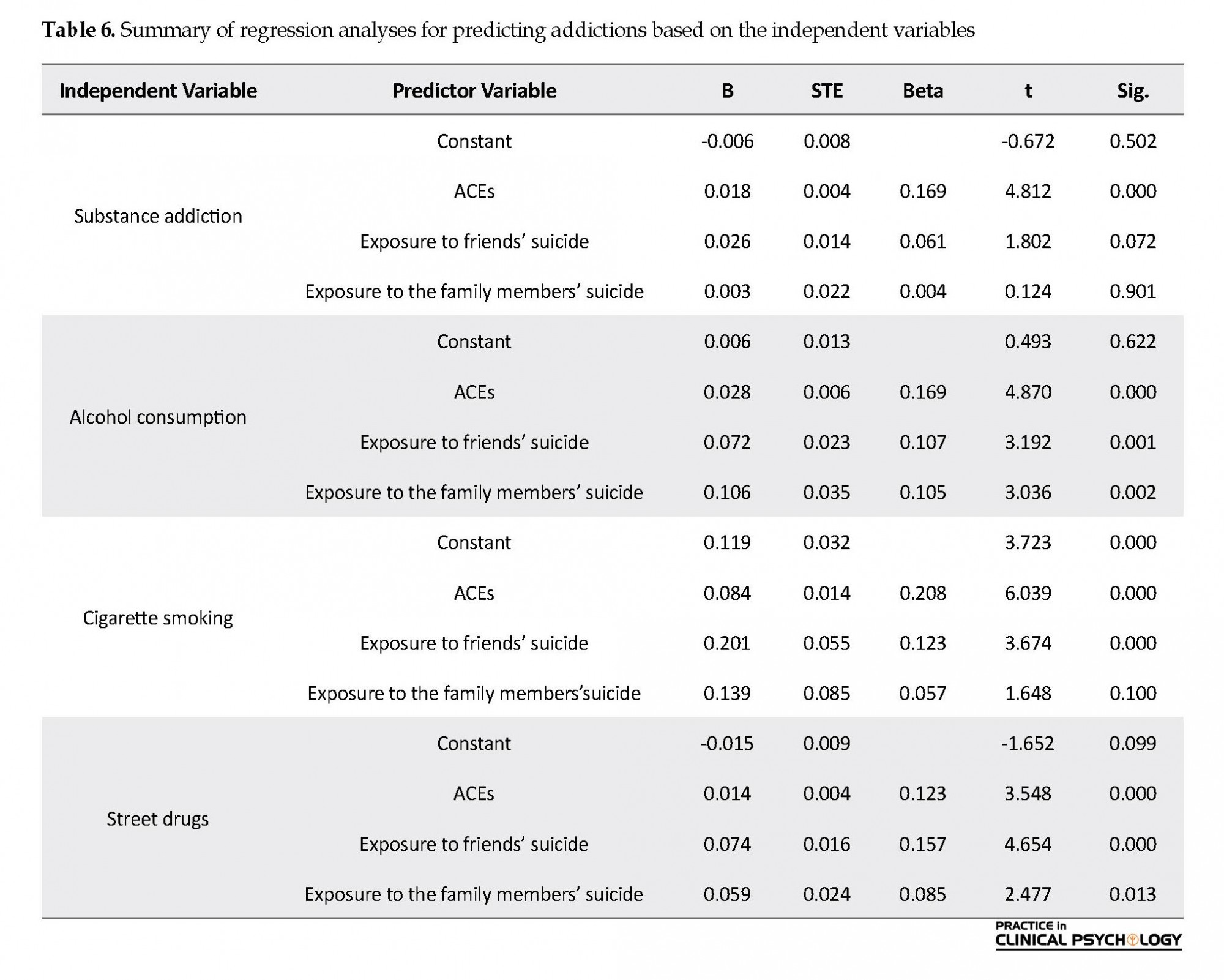
As presented in Table 5, ACEs and exposure to friends’ and family members’ suicide can explain addiction and 3% of substance abuse variance, 6% of alcohol consumption variance, 7% of cigarette smoking, and 5% of street drugs variance. Regression coefficients of predictor variable show that ACEs (t=4.812, β=0.169) and exposure to friends’ suicide (t=1.802, β= 0.061) can significantly predict substance addiction, however, the role of ACEs is more significant. All 3 variables of ACEs (t=4.870, β=0.169), exposure to friends’ suicide (t=3.192, β=0.107), and exposure to family members’ suicide (t=3.036, β=0.105) can predict alcohol consumption, but ACEs also play a more important role. In terms of cigarette smoking, ACEs (t=6.039, β=0.208), and exposure to friends’ suicide (t=3.674, β=0.123) are influential, but again, the role of ACEs is more significant. ACEs (t=3.548, β=0.123), exposure to friends’ suicide (t=4-654, β=0.157), and exposure to family members’ suicide (t=2.477, β=0.157) play a role in predicting street drugs addiction Table 6.
4. Discussion
This research aimed to predict suicidality and addiction (substance, alcohol, cigarette, psychoactive drugs) among college students based on ACEs and exposure to others’ suicide. Our findings have shown that ACEs can predict suicide among students. This finding is in line with Lipschitz et al. (1999), and Chapman et al. (2004) findings. Adolescents’ suicidal behaviors are affected by genetic, psychological, cognitive, and social factors, with particular risks related to childhood adversities (Miller, Esposito-Smythers, Weismoore, & Renshaw. 2013). A strong graded relationship has been reported between the number of adverse experiences in childhood and self-reports of cigarette smoking, alcoholism, drug abuse, obesity, attempted suicide, and sexual promiscuity in later life (Anda et al., 1999).
This research aimed to predict suicidality and addiction (substance, alcohol, cigarette, psychoactive drugs) among college students based on ACEs and exposure to others’ suicide. Our findings have shown that ACEs can predict suicide among students. This finding is in line with Lipschitz et al. (1999), and Chapman et al. (2004) findings. Adolescents’ suicidal behaviors are affected by genetic, psychological, cognitive, and social factors, with particular risks related to childhood adversities (Miller, Esposito-Smythers, Weismoore, & Renshaw. 2013). A strong graded relationship has been reported between the number of adverse experiences in childhood and self-reports of cigarette smoking, alcoholism, drug abuse, obesity, attempted suicide, and sexual promiscuity in later life (Anda et al., 1999).
Based on this finding, we can infer that experiencing adversity in childhood, especially in the absence of supportive factors, impairs the development of executive functions and distort physiological responses to stress (Shonkoff, 2016), leading to unhealthy coping behavior, disorder in physical, mental, and behavioral health, less hope for life (Brown et al., 2009), losing life opportunities (such as educational, professional and financial chance) (Font, Maguire-Jack, 2016), and finally higher likelihood of suicide. Evidence shows that brain development is influenced by ACEs (Sher, 2015). Thus, experiencing adversity can change and impair developmental, emotional, social, cognitive, neural, and behavioral processes in people, and ultimately lead to suicidal attempts.
Another finding of this research is that ACEs can predict addiction tendency among students. This result is consistent with Anda et al. (1999) conclusion. Maltreatment in childhood may cause adults to adopt risky behaviors in a variety of domains, including smoking (Anda et al., 1999), alcohol abuse, and illicit drug use (Thompson, Potter, Sanderson, Maibach, 1997).
In a study, the subjects with four or more adverse childhood events, were nearly five times more prone to depressive episodes in the 12 last months, twice as likely to smoke cigarettes, more than seven times as likely to consider themselves an “alcoholic”, and 12 times as likely to have attempted suicide (Reavis et al., 2013). Thus, a strong graded relationship exists between the number of adverse events an individual suffers in childhood and experiencing physical disease, mental disorder, and substance abuse in adulthood. In this research, the correlation between ACEs and cigarette addiction was more than other types of addictions.
About this relationship, it should be said that smoking is an accessible and easy target which is highly acceptable among people. In addition, in low-income societies like our country, smoking cigarette costs less than other types of addiction. Consequently, society does not condemn it. In contrast, addictions to substance, alcohol, or street drugs are banned in Iran, and people prefer to use smoke instead. In conclusion, participants of this study can quickly disclose about smoking, and it has not any legal consequences, but unveiling other addictions may have legal and social consequences, and the participants prefer not to report it in the questionnaire.
But about exposure to friends’ or family members’ suicide, it should be said that it has a significant correlation with suicide. It means that witnessing friends’ or family members’ suicide, increase the likelihood of witness’ suicide in the future. Dhingra et al. (2016) reported that exposure to family members’ and friends’ suicide or self-injurious behavior and fearlessness about death are related to suicide among college student samples. One study (Mars et al., 2018) reported that witnessing family members’ and or friends’ self-harm was higher among attempters than those who have suicidal ideations. However, exposure to friends’ self-harm was more related to attempt suicide than exposure to family members’ self-harm. Dhingra et al. (2016) stated that two of the volitional covariates, namely exposure to and fearlessness about death, were directly related to suicide attempts. Witnessing the suicidal behavior of others (family or friends) is a social volitional model with an established relationship with the suicide risk (O’Connor et al., 2012).
There are several potential mechanisms that explain this relationship. For example, the suicidal behavior of others may increase the modeling or imitating a loved one’s suicidal behavior. Witnessing suicide may also increase the salience and cognitive accessibility of suicide such that individuals are more likely to attempt suicide when they encounter stressors. Finally, we should say that witnessing suicide can trigger suicide attempt in multiple ways: first, the role of social learning, in which a person learns and imitates with observing other’ self-harm or suicide, and may enact it in the future. Second, watching others’ suicides affect the person’s cognitive process and distort it. As such, this stressful experience disrupts the personal balance in stressful situations and impair emotional and cognitive functioning in that situation. In this research, exposure to friends’ or family members’ suicide has a significant relationship with addictions
About predictions, it should be said that witnessing suicide has a significant direct relationship with suicide, but with entering ACEs to model, this relationship reduces in favor of ACEs, and ACEs has got more power for predicting suicide. Research has shown that later risk factor in life, such as victimization by peers and sexual violence can affect forming suicide ideation and suicide attempt (Ports et al., 2017), whereas the effect of ACEs is more than exposures and people in the process of ACEs are exposed to maltreatment and adversity, to anticipating the ACEs strength will be more that exposures alone.
These results enrich our understanding of the impact of ACEs and child maltreatment on adult behavior and have clear implications for mental health policymakers, suggesting the importance of screening for mental health problems and suicidality among adversity-exposed people. Furthermore, accessible and useful child and adolescent mental health services and suicide prevention services may be essential components in reducing students’ suicidality. These findings may be helpful for practitioners in university, health, and social services and non-governmental organizations, in identifying students who may be at risk of a suicide attempt. Using strategies such as cognitive behavioral intervention can help individuals in controlling their stress and using proper coping style when encountering with the stressful event, and subsequently, reduce the likelihood of self-injury or suicidal behavior. Concerning ACEs, we strongly need to inform society and especially parents about the effect of early life years’ experiences on later life behaviors and educate families about true and secure behavior with children. We can do these with teaching parenting skills to parents.
The results of this study are subject to certain limitations. Responses were based on self-reports. The percentage of students disclosing ACEs is lower than real life ACEs and therefore may be subject to under-reporting. Future research may help address these issues by including more objective measures such as laboratory results and clinical diagnosis. A potential weakness of studies with retrospective reporting of childhood experiences is the possibility of recall bias. The ACEs questionnaire was derived from other cultures, while in our country, other indicators such as war can be seen as ACEs. Therefore, designing a new ACE questionnaire based on our culture is a useful idea. Finally, ACEs in the early years of life are the main factor for risky behaviors in later life, including suicide and addiction. Therefore, awareness of this mechanism can help us in reducing this problem, promoting health, and decreasing the burden of the health system at the personal, family, society level.
Based on these findings, we can conclude that adverse childhood experiences play an important and essential role in suicidality and addiction, and we should prevent these experiences by working on the family.
Ethical Considerations
Compliance with ethical guidelines
Ethical issues such as confidentiality of the participants’ information, written consent of the participants and non-intervention were observed.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization, methodology, investigation, writing oiginal draft, supervision, writing review & editing: Ahmadreza Kiani; Funding acquisition: Akbar Atadokht; Resources: Shokoufe Ramezani.
Conflict of interest
The authors declared no conflict of interest.
References
Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C. H., et al. (2006). The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience, 256(3), 174-86. [DOI: 10.1007/s00406-005-0624-4]
Arnett, J. J. (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469-80. [PMID: 10842426]
Amin‐Esmaeili, M., Rahimi‐Movaghar, A., Sharifi, V., Hajebi, A., Radgoodarzi, R., Mojtabai, R., et al. (2016). Epidemiology of illicit drug use disorders in Iran: prevalence, correlates, comorbidity, and service utilization results from the Iranian Mental Health Survey. Addiction, 111(10), 1836-47. [DOI:10.4178/epih.e2018030] [PMID] [PMCID]
Anda, R. F., Butchart, A., Felitti, V. J., & Brown, D. W. (2010). Building a framework for global surveillance of the public health implications of adverse childhood experiences. American Journal of preventive medicine, 39(1), 93-8. [DOI:10.1016/j.amepre.2010.03.015] [PMID]
Anda, R. F., Croft, J. B., Felitti, V. J., Nordenberg, D., Giles, W. H., Williamson, D. F., et al. (1999). Adverse childhood experiences and smoking during adolescence and adulthood. JAMA, 282(17), 1652-8. [DOI:10.1001/jama.282.17.1652] [PMID]
Becker, W. C., & Fiellin, D. A. (2017). Abuse-deterrent opioid formulations-putting the potential benefits into perspective. New England Journal of Medicine, 376(22), 2103-5. [DOI:10.1056/NEJMp1701553] [PMID]
Brown, D. W., Anda, R. F., Tiemeier, H., Felitti, V. J., Edwards, V. J., Croft, J. B., et al. (2009). Adverse childhood experiences and the risk of premature mortality. American Journal of Preventive Medicine, 37(5), 389-96. [DOI:10.1016/j.amepre.2009.06.021]
Chapman, D. P., Whitfield, C. L., Felitti, V. J., Dube, S. R., Edwards, V. J., & Anda, R. F. (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders, 82(2), 217-25. [DOI:10.1016/j.jad.2003.12.013] [PMID]
Dehshiri, G., & Mousavi, S. F. (2015). Potential for drug abuse: The predictive role of parenting styles, stress and type D personality (Persian)]. Research on Addiction, 9(33), 91-106.
Dhingra, K., Boduszek, D., & O’Connor, R. C. (2016). A structural test of the integrated motivational-volitional model of suicidal behavior. Psychiatry Research, 239, 169-78. [DOI:10.1016/j.psychres.2016.03.023] [PMID]
Dube, S. R., Anda, R. F., Felitti, V. J., Chapman, D. P., Williamson, D. F., & Giles, W. H. (2001). Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. The Journal of the American Medical Association, 286(24), 3089-96. [DOI:10.1001/jama.286.24.3089] [PMID]
Dube, S. R., Felitti, V. J., Dong, M., Chapman, D. P., Giles, W. H., & Anda, R. F. (2003). Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics, 111(3), 564-72. [DOI:10.1542/peds.111.3.564] [PMID]
Eskin, M., Sun, J. M., Abuidhail, J., Yoshimasu, K., Kujan, O., Janghorbani, et al. (2016). Suicidal behavior and psychological distress in university students: A 12-nation Study. Journal Archives of Suicide Research, 20(3), 369–88. [DOI/10.1080/13811118.2015.1054055]
Font, S. A., & Maguire-Jack, K. (2016). Pathways from childhood abuse and other adversities to adult health risks: the role of adult socioeconomic conditions. Child Abuse & Neglect, 51, 390-9. [DOI:10.1016/j.chiabu.2015.05.013] [PMID] [PMCID]
Hassanian-Moghaddam, H., & Zamani, N. (2017). Suicide in Iran: The facts and the figures from nationwide reports. Iranian Journal of Psychiatry, 12(1), 73-7. [PMID] [PMCID]
Hill, S. Y., Tessner, K. D., & McDermott, M. D. (2011). Psychopathology in offspring from families of alcohol dependent female probands: A prospective study. Journal of Psychiatric Research, 45(3), 285-94. [DOI:10.1016/j.jpsychires.2010.08.005] [PMID] [PMCID]
Hussong, A., Bauer, D., & Chassin, L. (2008). Telescoped trajectories from alcohol initiation to disorder in children of alcoholic parents. Journal of Abnormal Psychology, 117(1):63-78.[DOI:10.1037/0021-843X.117.1.63] [PMID] [PMCID]
Joiner Jr, T. E., Pfaff, J. J., & Acres, J. G. (2002). A brief screening tool for suicidal symptoms in adolescents and young adults in general health settings: Reliability and validity data from the Australian national general practice youth suicide prevention project. Behavior Research and Therapy, 40(4), 471-81. [DOI:10.1016/S0005-7967(01)00017-1]
Kabir, K., Bahari, A., Hajizadeh, M., Allahverdipour, H., Tarrahi, M. J., Fakhari, A., et al. (2018). Substance abuse behaviors among university freshmen in Iran: A latent class analysis. Epidemiology and Health, 40, e2018030. [DOI:10.4178/epih.e2018030] [PMID] [PMCID]
Kiani Chelmardi, A.R., Rashid, S., Honarmand, P., & Tamook, F. (2018). [structural test of the interpersonal theory of suicide model in students (Persian)]. Contemporary Psychology, Biannual. Journal of the Iranian Psychological Association, 13(1), 50-61. [DOI: 10.32598/bjcp.13.1.50]
Ma, J., Batterham, P. J., Calear, A. L., & Han, J. (2016). A systematic review of the predictions of the interpersonal-psychological theory of suicidal behavior. Clinical Psychology Review, 46, 34-45. [DOI:10.1016/j.cpr.2016.04.008] [PMID]
Maltsberger, J. T. (2003). Reducing suicide: A national imperative. The Journal of Nervous and Mental Disease, 191(9), 623-4. [DOI:10.1097/01.nmd.0000087330.14485.41]
Mars, B., Heron, J., Klonsky, E. D., Moran, P., O'Connor, R. C., Tilling, K., et al. (2019). What distinguishes adolescents with suicidal thoughts from those who have attempted suicide? A population-based birth cohort study. Journal of Child Psychology and Psychiatry, 60(1), 91-9. [DOI:10.1111/jcpp.12878] [PMID] [PMCID]
Miller, A. B., Esposito-Smythers, C., Weismoore, J. T., & Renshaw, K. D. (2013). The relation between child maltreatment and adolescent suicidal behavior: A systematic review and critical examination of the literature. Clinical Child and Family Psychology Review, 16(2), 146-72. [DOI:10.1007/s10567-013-0131-5] [PMID] [PMCID]
Mortier, P., Cuijpers, P., Kiekens, G., Auerbach, R. P., Demyttenaere, K., Green, J. G., et al. (2018). The prevalence of suicidal thoughts and behaviours among college students: a metaanalysis. Psychological Medicine, 48(4), 554–65. [DOI:10.1017/S0033291717002215]
Lipschitz, D. S., Winegar, R. K., Nicolaou, A. L., Hartnick, E., Wolfson, M., & Southwick, S. M. (1999). Perceived abuse and neglect as risk factors for suicidal behavior in adolescent inpatients. The Journal of Nervous and Mental Disease, 187(1), 32-9.
O’connor, R. C., Armitage, C. J., & Gray, L. (2006). The role of clinical and social cognitive variables in parasuicide. British Journal of Clinical Psychology, 45(4), 465-81. [DOI:10.1348/014466505X82315] [PMID]
O’connor, R. C., Rasmussen, S., & Hawton, K. (2012). Distinguishing adolescents who think about self-harm from those who engage in self-harm. The British Journal of Psychiatry, 200(4), 330-5. [DOI:10.1192/bjp.bp.111.097808] [PMID]
Oladeji, B. D., Makanjuola, V. A., & Gureje, O. (2010). Family-related adverse childhood experiences as risk factors for psychiatric disorders in Nigeria. The British Journal of Psychiatry, 196(3), 186-91. [DOI:10.1192/bjp.bp.109.063677] [PMID] [PMCID]
Parolin, M., Simonelli, A., Mapelli, D., Sacco, M., & Cristofalo, P. (2016). Parental substance abuse as an early traumatic event. Preliminary findings on neuropsychological and personality functioning in young drug addicts exposed to drugs early. Frontiers in Psychology, 7(887), 1-15. [DOI:10.3389/fpsyg.2016.00887]
Ports, K. A., Merrick, M. T., Stone, D. M., Wilkins, N. J., Reed, J., Ebin, J., et al. (2017). Adverse childhood experiences and suicide risk: Toward comprehensive prevention. American Journal of Preventive Medicine, 53(3), 400-3. [DOI:10.1016/j.amepre.2017.03.015] [PMID] [PMCID]
Quinn, K., Boone, L., Scheidell, J. D., Mateu-Gelabert, P., McGorray, S. P., Beharie, N., et al. (2016). The relationships of childhood trauma and adulthood prescription pain reliever misuse and injection drug use. Drug and Alcohol Dependence, 169, 190-8. [DOI:10.1016/j.drugalcdep.2016.09.021] [PMID] [PMCID]
Rashid, S., Khorramdel, K., Gholami, F., & Senobar, L. (2016). The relationship between interpersonal psychological theory of suicide constructs (loneliness, perceived social support, thwarted belongingness and burdensomeness) and suicidal behavior among Iranian students. Health Education & Health Promotion, 4(2), 35-48.
Reavis, J. A., Looman, J., Franco, K. A., & Rojas, B. (2013). Adverse childhood experiences and adult criminality: How long must we live before we possess our own lives?. The Permanente Journal, 17(2), 44-8. [DOI:10.7812/TPP/12-072]
Rothman, E. F., Edwards, E. M., Heeren, T., & Hingson, R. W. (2008). Adverse childhood experiences predict earlier age of drinking onset: Results from a representative US sample of current or former drinkers. Pediatrics, 122(2), e298-e304. [DOI:10.1542/peds.2007-3412] [PMID]
Schilling, E. A., Aseltine, R. H., & Gore, S. (2007). Adverse childhood experiences and mental health in young adults: a longitudinal survey. BMC Public Health, 7, 30. [DOI:10.1186/1471-2458-7-30] [PMID] [PMCID]
Sher, L. (2017). Commentary: Adverse childhood experiences and risk for Suicidal Behavior in male Iraq and Afghanistan Veterans Seeking PtSD treatment. Frontiers in Public Health, 5(72), 1-3. [DOI:10.3389/fpubh.2017.00072]
Shonkoff, J. P. (2016). Capitalizing on advances in science to reduce the health consequences of early childhood adversity. JAMA Pediatrics, 170(10), 1003-7. [DOI:10.1001/jamapediatrics.2016.1559] [PMID]
Thompson, N. J., Potter, J. S., Sanderson, C. A., & Maibach, E.W. (1997). The relationship between sexual abuse and HIV risk behaviors among heterosexual adult female STD patients. Child Abuse & Neglect, 21(2):149-56. [DOI:10.1016/S0145-2134(96)00140-8]
Tsavoussis, A., Stawicki, S., Stoicea, N., & Papadimos, T. J. (2014). Child-witnessed domestic violence and its adverse effects on brain development: a call for societal self-examination and awareness. Frontiers in Public Health, 2, 178. [DOI:10.3389/fpubh.2014.00178] [PMID] [PMCID]
Van Orden, K. A., Witte, T. K., Gordon, K. H., Bender, T. W., & Joiner Jr, T. E. (2008). Suicidal desire and the capability for suicide: Tests of the interpersonal-psychological theory of suicidal behavior among adults. Journal of Consulting and Clinical Psychology, 76(1), 72-83. [DOI:10.1037/0022-006X.76.1.72] [PMID]
Veisani, Y., Delpisheh, A., Mohamadian, F., & Valizadeh, R. (2018). Trends of suicide attempts and completed suicide in Ilam province of Iran; A demographic analysis study. Bulletin of Emergency & Trauma, 6(3), 245-8. [DOI:10.29252/beat-060310] [PMID] [PMCID]
von Glischinski, M., Teismann, T., Prinz, S., Gebauer, J. E., & Hirschfeld, G. (2016). Depressive symptom inventory suicidality subscale: Optimal cut points for clinical and non‐clinical samples. Clinical Psychology & Psychotherapy, 23(6), 543-9. [DOI:10.1002/cpp.2007] [PMID]
Voss, W. D., Kaufman, E., O’Connor, S. S., Comtois, K. A., Conner, K. R., & Ries, R. K. (2013). Preventing addiction-related suicide: A pilot study. Journal of Substance Abuse Treatment, 44(5), 565-9. [DOI:10.1016/j.jsat.2012.10.006] [PMID] [PMCID]
Weitzman, E. R., & Wechsler, H. (2000). Alcohol use, abuse, and related problems among children of problem drinkers: findings from a national survey of college alcohol use. The Journal of Nervous and Mental Disease, 188(3), 148-54. [DOI:10.1097/00005053-200003000-00004] [PMID]
Yasamy, M. T., Shahmohammadi, D., Bagheri Yazdi, S. A., Layeghi, H., Bolhari, J., Razzaghi, E. M., et al. (2001). Mental health in the Islamic Republic of Iran: Achievements and areas of need. EMHJ-Eastern Mediterranean Health Journal, 7(3), 381-91. [PMID]
In a study, the subjects with four or more adverse childhood events, were nearly five times more prone to depressive episodes in the 12 last months, twice as likely to smoke cigarettes, more than seven times as likely to consider themselves an “alcoholic”, and 12 times as likely to have attempted suicide (Reavis et al., 2013). Thus, a strong graded relationship exists between the number of adverse events an individual suffers in childhood and experiencing physical disease, mental disorder, and substance abuse in adulthood. In this research, the correlation between ACEs and cigarette addiction was more than other types of addictions.
About this relationship, it should be said that smoking is an accessible and easy target which is highly acceptable among people. In addition, in low-income societies like our country, smoking cigarette costs less than other types of addiction. Consequently, society does not condemn it. In contrast, addictions to substance, alcohol, or street drugs are banned in Iran, and people prefer to use smoke instead. In conclusion, participants of this study can quickly disclose about smoking, and it has not any legal consequences, but unveiling other addictions may have legal and social consequences, and the participants prefer not to report it in the questionnaire.
But about exposure to friends’ or family members’ suicide, it should be said that it has a significant correlation with suicide. It means that witnessing friends’ or family members’ suicide, increase the likelihood of witness’ suicide in the future. Dhingra et al. (2016) reported that exposure to family members’ and friends’ suicide or self-injurious behavior and fearlessness about death are related to suicide among college student samples. One study (Mars et al., 2018) reported that witnessing family members’ and or friends’ self-harm was higher among attempters than those who have suicidal ideations. However, exposure to friends’ self-harm was more related to attempt suicide than exposure to family members’ self-harm. Dhingra et al. (2016) stated that two of the volitional covariates, namely exposure to and fearlessness about death, were directly related to suicide attempts. Witnessing the suicidal behavior of others (family or friends) is a social volitional model with an established relationship with the suicide risk (O’Connor et al., 2012).
There are several potential mechanisms that explain this relationship. For example, the suicidal behavior of others may increase the modeling or imitating a loved one’s suicidal behavior. Witnessing suicide may also increase the salience and cognitive accessibility of suicide such that individuals are more likely to attempt suicide when they encounter stressors. Finally, we should say that witnessing suicide can trigger suicide attempt in multiple ways: first, the role of social learning, in which a person learns and imitates with observing other’ self-harm or suicide, and may enact it in the future. Second, watching others’ suicides affect the person’s cognitive process and distort it. As such, this stressful experience disrupts the personal balance in stressful situations and impair emotional and cognitive functioning in that situation. In this research, exposure to friends’ or family members’ suicide has a significant relationship with addictions
About predictions, it should be said that witnessing suicide has a significant direct relationship with suicide, but with entering ACEs to model, this relationship reduces in favor of ACEs, and ACEs has got more power for predicting suicide. Research has shown that later risk factor in life, such as victimization by peers and sexual violence can affect forming suicide ideation and suicide attempt (Ports et al., 2017), whereas the effect of ACEs is more than exposures and people in the process of ACEs are exposed to maltreatment and adversity, to anticipating the ACEs strength will be more that exposures alone.
These results enrich our understanding of the impact of ACEs and child maltreatment on adult behavior and have clear implications for mental health policymakers, suggesting the importance of screening for mental health problems and suicidality among adversity-exposed people. Furthermore, accessible and useful child and adolescent mental health services and suicide prevention services may be essential components in reducing students’ suicidality. These findings may be helpful for practitioners in university, health, and social services and non-governmental organizations, in identifying students who may be at risk of a suicide attempt. Using strategies such as cognitive behavioral intervention can help individuals in controlling their stress and using proper coping style when encountering with the stressful event, and subsequently, reduce the likelihood of self-injury or suicidal behavior. Concerning ACEs, we strongly need to inform society and especially parents about the effect of early life years’ experiences on later life behaviors and educate families about true and secure behavior with children. We can do these with teaching parenting skills to parents.
The results of this study are subject to certain limitations. Responses were based on self-reports. The percentage of students disclosing ACEs is lower than real life ACEs and therefore may be subject to under-reporting. Future research may help address these issues by including more objective measures such as laboratory results and clinical diagnosis. A potential weakness of studies with retrospective reporting of childhood experiences is the possibility of recall bias. The ACEs questionnaire was derived from other cultures, while in our country, other indicators such as war can be seen as ACEs. Therefore, designing a new ACE questionnaire based on our culture is a useful idea. Finally, ACEs in the early years of life are the main factor for risky behaviors in later life, including suicide and addiction. Therefore, awareness of this mechanism can help us in reducing this problem, promoting health, and decreasing the burden of the health system at the personal, family, society level.
Based on these findings, we can conclude that adverse childhood experiences play an important and essential role in suicidality and addiction, and we should prevent these experiences by working on the family.
Ethical Considerations
Compliance with ethical guidelines
Ethical issues such as confidentiality of the participants’ information, written consent of the participants and non-intervention were observed.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
Conceptualization, methodology, investigation, writing oiginal draft, supervision, writing review & editing: Ahmadreza Kiani; Funding acquisition: Akbar Atadokht; Resources: Shokoufe Ramezani.
Conflict of interest
The authors declared no conflict of interest.
References
Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C. H., et al. (2006). The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience, 256(3), 174-86. [DOI: 10.1007/s00406-005-0624-4]
Arnett, J. J. (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55(5), 469-80. [PMID: 10842426]
Amin‐Esmaeili, M., Rahimi‐Movaghar, A., Sharifi, V., Hajebi, A., Radgoodarzi, R., Mojtabai, R., et al. (2016). Epidemiology of illicit drug use disorders in Iran: prevalence, correlates, comorbidity, and service utilization results from the Iranian Mental Health Survey. Addiction, 111(10), 1836-47. [DOI:10.4178/epih.e2018030] [PMID] [PMCID]
Anda, R. F., Butchart, A., Felitti, V. J., & Brown, D. W. (2010). Building a framework for global surveillance of the public health implications of adverse childhood experiences. American Journal of preventive medicine, 39(1), 93-8. [DOI:10.1016/j.amepre.2010.03.015] [PMID]
Anda, R. F., Croft, J. B., Felitti, V. J., Nordenberg, D., Giles, W. H., Williamson, D. F., et al. (1999). Adverse childhood experiences and smoking during adolescence and adulthood. JAMA, 282(17), 1652-8. [DOI:10.1001/jama.282.17.1652] [PMID]
Becker, W. C., & Fiellin, D. A. (2017). Abuse-deterrent opioid formulations-putting the potential benefits into perspective. New England Journal of Medicine, 376(22), 2103-5. [DOI:10.1056/NEJMp1701553] [PMID]
Brown, D. W., Anda, R. F., Tiemeier, H., Felitti, V. J., Edwards, V. J., Croft, J. B., et al. (2009). Adverse childhood experiences and the risk of premature mortality. American Journal of Preventive Medicine, 37(5), 389-96. [DOI:10.1016/j.amepre.2009.06.021]
Chapman, D. P., Whitfield, C. L., Felitti, V. J., Dube, S. R., Edwards, V. J., & Anda, R. F. (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders, 82(2), 217-25. [DOI:10.1016/j.jad.2003.12.013] [PMID]
Dehshiri, G., & Mousavi, S. F. (2015). Potential for drug abuse: The predictive role of parenting styles, stress and type D personality (Persian)]. Research on Addiction, 9(33), 91-106.
Dhingra, K., Boduszek, D., & O’Connor, R. C. (2016). A structural test of the integrated motivational-volitional model of suicidal behavior. Psychiatry Research, 239, 169-78. [DOI:10.1016/j.psychres.2016.03.023] [PMID]
Dube, S. R., Anda, R. F., Felitti, V. J., Chapman, D. P., Williamson, D. F., & Giles, W. H. (2001). Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. The Journal of the American Medical Association, 286(24), 3089-96. [DOI:10.1001/jama.286.24.3089] [PMID]
Dube, S. R., Felitti, V. J., Dong, M., Chapman, D. P., Giles, W. H., & Anda, R. F. (2003). Childhood abuse, neglect, and household dysfunction and the risk of illicit drug use: the adverse childhood experiences study. Pediatrics, 111(3), 564-72. [DOI:10.1542/peds.111.3.564] [PMID]
Eskin, M., Sun, J. M., Abuidhail, J., Yoshimasu, K., Kujan, O., Janghorbani, et al. (2016). Suicidal behavior and psychological distress in university students: A 12-nation Study. Journal Archives of Suicide Research, 20(3), 369–88. [DOI/10.1080/13811118.2015.1054055]
Font, S. A., & Maguire-Jack, K. (2016). Pathways from childhood abuse and other adversities to adult health risks: the role of adult socioeconomic conditions. Child Abuse & Neglect, 51, 390-9. [DOI:10.1016/j.chiabu.2015.05.013] [PMID] [PMCID]
Hassanian-Moghaddam, H., & Zamani, N. (2017). Suicide in Iran: The facts and the figures from nationwide reports. Iranian Journal of Psychiatry, 12(1), 73-7. [PMID] [PMCID]
Hill, S. Y., Tessner, K. D., & McDermott, M. D. (2011). Psychopathology in offspring from families of alcohol dependent female probands: A prospective study. Journal of Psychiatric Research, 45(3), 285-94. [DOI:10.1016/j.jpsychires.2010.08.005] [PMID] [PMCID]
Hussong, A., Bauer, D., & Chassin, L. (2008). Telescoped trajectories from alcohol initiation to disorder in children of alcoholic parents. Journal of Abnormal Psychology, 117(1):63-78.[DOI:10.1037/0021-843X.117.1.63] [PMID] [PMCID]
Joiner Jr, T. E., Pfaff, J. J., & Acres, J. G. (2002). A brief screening tool for suicidal symptoms in adolescents and young adults in general health settings: Reliability and validity data from the Australian national general practice youth suicide prevention project. Behavior Research and Therapy, 40(4), 471-81. [DOI:10.1016/S0005-7967(01)00017-1]
Kabir, K., Bahari, A., Hajizadeh, M., Allahverdipour, H., Tarrahi, M. J., Fakhari, A., et al. (2018). Substance abuse behaviors among university freshmen in Iran: A latent class analysis. Epidemiology and Health, 40, e2018030. [DOI:10.4178/epih.e2018030] [PMID] [PMCID]
Kiani Chelmardi, A.R., Rashid, S., Honarmand, P., & Tamook, F. (2018). [structural test of the interpersonal theory of suicide model in students (Persian)]. Contemporary Psychology, Biannual. Journal of the Iranian Psychological Association, 13(1), 50-61. [DOI: 10.32598/bjcp.13.1.50]
Ma, J., Batterham, P. J., Calear, A. L., & Han, J. (2016). A systematic review of the predictions of the interpersonal-psychological theory of suicidal behavior. Clinical Psychology Review, 46, 34-45. [DOI:10.1016/j.cpr.2016.04.008] [PMID]
Maltsberger, J. T. (2003). Reducing suicide: A national imperative. The Journal of Nervous and Mental Disease, 191(9), 623-4. [DOI:10.1097/01.nmd.0000087330.14485.41]
Mars, B., Heron, J., Klonsky, E. D., Moran, P., O'Connor, R. C., Tilling, K., et al. (2019). What distinguishes adolescents with suicidal thoughts from those who have attempted suicide? A population-based birth cohort study. Journal of Child Psychology and Psychiatry, 60(1), 91-9. [DOI:10.1111/jcpp.12878] [PMID] [PMCID]
Miller, A. B., Esposito-Smythers, C., Weismoore, J. T., & Renshaw, K. D. (2013). The relation between child maltreatment and adolescent suicidal behavior: A systematic review and critical examination of the literature. Clinical Child and Family Psychology Review, 16(2), 146-72. [DOI:10.1007/s10567-013-0131-5] [PMID] [PMCID]
Mortier, P., Cuijpers, P., Kiekens, G., Auerbach, R. P., Demyttenaere, K., Green, J. G., et al. (2018). The prevalence of suicidal thoughts and behaviours among college students: a metaanalysis. Psychological Medicine, 48(4), 554–65. [DOI:10.1017/S0033291717002215]
Lipschitz, D. S., Winegar, R. K., Nicolaou, A. L., Hartnick, E., Wolfson, M., & Southwick, S. M. (1999). Perceived abuse and neglect as risk factors for suicidal behavior in adolescent inpatients. The Journal of Nervous and Mental Disease, 187(1), 32-9.
O’connor, R. C., Armitage, C. J., & Gray, L. (2006). The role of clinical and social cognitive variables in parasuicide. British Journal of Clinical Psychology, 45(4), 465-81. [DOI:10.1348/014466505X82315] [PMID]
O’connor, R. C., Rasmussen, S., & Hawton, K. (2012). Distinguishing adolescents who think about self-harm from those who engage in self-harm. The British Journal of Psychiatry, 200(4), 330-5. [DOI:10.1192/bjp.bp.111.097808] [PMID]
Oladeji, B. D., Makanjuola, V. A., & Gureje, O. (2010). Family-related adverse childhood experiences as risk factors for psychiatric disorders in Nigeria. The British Journal of Psychiatry, 196(3), 186-91. [DOI:10.1192/bjp.bp.109.063677] [PMID] [PMCID]
Parolin, M., Simonelli, A., Mapelli, D., Sacco, M., & Cristofalo, P. (2016). Parental substance abuse as an early traumatic event. Preliminary findings on neuropsychological and personality functioning in young drug addicts exposed to drugs early. Frontiers in Psychology, 7(887), 1-15. [DOI:10.3389/fpsyg.2016.00887]
Ports, K. A., Merrick, M. T., Stone, D. M., Wilkins, N. J., Reed, J., Ebin, J., et al. (2017). Adverse childhood experiences and suicide risk: Toward comprehensive prevention. American Journal of Preventive Medicine, 53(3), 400-3. [DOI:10.1016/j.amepre.2017.03.015] [PMID] [PMCID]
Quinn, K., Boone, L., Scheidell, J. D., Mateu-Gelabert, P., McGorray, S. P., Beharie, N., et al. (2016). The relationships of childhood trauma and adulthood prescription pain reliever misuse and injection drug use. Drug and Alcohol Dependence, 169, 190-8. [DOI:10.1016/j.drugalcdep.2016.09.021] [PMID] [PMCID]
Rashid, S., Khorramdel, K., Gholami, F., & Senobar, L. (2016). The relationship between interpersonal psychological theory of suicide constructs (loneliness, perceived social support, thwarted belongingness and burdensomeness) and suicidal behavior among Iranian students. Health Education & Health Promotion, 4(2), 35-48.
Reavis, J. A., Looman, J., Franco, K. A., & Rojas, B. (2013). Adverse childhood experiences and adult criminality: How long must we live before we possess our own lives?. The Permanente Journal, 17(2), 44-8. [DOI:10.7812/TPP/12-072]
Rothman, E. F., Edwards, E. M., Heeren, T., & Hingson, R. W. (2008). Adverse childhood experiences predict earlier age of drinking onset: Results from a representative US sample of current or former drinkers. Pediatrics, 122(2), e298-e304. [DOI:10.1542/peds.2007-3412] [PMID]
Schilling, E. A., Aseltine, R. H., & Gore, S. (2007). Adverse childhood experiences and mental health in young adults: a longitudinal survey. BMC Public Health, 7, 30. [DOI:10.1186/1471-2458-7-30] [PMID] [PMCID]
Sher, L. (2017). Commentary: Adverse childhood experiences and risk for Suicidal Behavior in male Iraq and Afghanistan Veterans Seeking PtSD treatment. Frontiers in Public Health, 5(72), 1-3. [DOI:10.3389/fpubh.2017.00072]
Shonkoff, J. P. (2016). Capitalizing on advances in science to reduce the health consequences of early childhood adversity. JAMA Pediatrics, 170(10), 1003-7. [DOI:10.1001/jamapediatrics.2016.1559] [PMID]
Thompson, N. J., Potter, J. S., Sanderson, C. A., & Maibach, E.W. (1997). The relationship between sexual abuse and HIV risk behaviors among heterosexual adult female STD patients. Child Abuse & Neglect, 21(2):149-56. [DOI:10.1016/S0145-2134(96)00140-8]
Tsavoussis, A., Stawicki, S., Stoicea, N., & Papadimos, T. J. (2014). Child-witnessed domestic violence and its adverse effects on brain development: a call for societal self-examination and awareness. Frontiers in Public Health, 2, 178. [DOI:10.3389/fpubh.2014.00178] [PMID] [PMCID]
Van Orden, K. A., Witte, T. K., Gordon, K. H., Bender, T. W., & Joiner Jr, T. E. (2008). Suicidal desire and the capability for suicide: Tests of the interpersonal-psychological theory of suicidal behavior among adults. Journal of Consulting and Clinical Psychology, 76(1), 72-83. [DOI:10.1037/0022-006X.76.1.72] [PMID]
Veisani, Y., Delpisheh, A., Mohamadian, F., & Valizadeh, R. (2018). Trends of suicide attempts and completed suicide in Ilam province of Iran; A demographic analysis study. Bulletin of Emergency & Trauma, 6(3), 245-8. [DOI:10.29252/beat-060310] [PMID] [PMCID]
von Glischinski, M., Teismann, T., Prinz, S., Gebauer, J. E., & Hirschfeld, G. (2016). Depressive symptom inventory suicidality subscale: Optimal cut points for clinical and non‐clinical samples. Clinical Psychology & Psychotherapy, 23(6), 543-9. [DOI:10.1002/cpp.2007] [PMID]
Voss, W. D., Kaufman, E., O’Connor, S. S., Comtois, K. A., Conner, K. R., & Ries, R. K. (2013). Preventing addiction-related suicide: A pilot study. Journal of Substance Abuse Treatment, 44(5), 565-9. [DOI:10.1016/j.jsat.2012.10.006] [PMID] [PMCID]
Weitzman, E. R., & Wechsler, H. (2000). Alcohol use, abuse, and related problems among children of problem drinkers: findings from a national survey of college alcohol use. The Journal of Nervous and Mental Disease, 188(3), 148-54. [DOI:10.1097/00005053-200003000-00004] [PMID]
Yasamy, M. T., Shahmohammadi, D., Bagheri Yazdi, S. A., Layeghi, H., Bolhari, J., Razzaghi, E. M., et al. (2001). Mental health in the Islamic Republic of Iran: Achievements and areas of need. EMHJ-Eastern Mediterranean Health Journal, 7(3), 381-91. [PMID]
Type of Study: Research |
Subject:
Cognitive behavioral
Received: 2018/09/21 | Accepted: 2019/02/8 | Published: 2019/04/1
Received: 2018/09/21 | Accepted: 2019/02/8 | Published: 2019/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |