Volume 6, Issue 3 (Summer 2018)
PCP 2018, 6(3): 175-182 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mohammadi Z, Pourshahbaz A, Poshtmashhadi M, Dolatshahi B, Barati F, Zarei M. Psychometric Properties of the Young Mania Rating Scale as a Mania Severity Measure in Patients With Bipolar I Disorder. PCP 2018; 6 (3) :175-182
URL: http://jpcp.uswr.ac.ir/article-1-552-en.html
URL: http://jpcp.uswr.ac.ir/article-1-552-en.html
Zahra Mohammadi * 
 1, Abbas Pourshahbaz2
1, Abbas Pourshahbaz2 

 , Marjan Poshtmashhadi2
, Marjan Poshtmashhadi2 

 , Behrooz Dolatshahi2
, Behrooz Dolatshahi2 

 , Fatemeh Barati2
, Fatemeh Barati2 
 , Majid Zarei2
, Majid Zarei2 


 1, Abbas Pourshahbaz2
1, Abbas Pourshahbaz2 

 , Marjan Poshtmashhadi2
, Marjan Poshtmashhadi2 

 , Behrooz Dolatshahi2
, Behrooz Dolatshahi2 

 , Fatemeh Barati2
, Fatemeh Barati2 
 , Majid Zarei2
, Majid Zarei2 

1- Department of Clinical Psychology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran , zahra.mohammadi412@gmail.com
2- Department of Clinical Psychology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
2- Department of Clinical Psychology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
Full-Text [PDF 617 kb]
(5210 Downloads)
| Abstract (HTML) (8145 Views)
Full-Text: (5440 Views)
1. Introduction
Bipolar I disorder is a condition, in which the patient experiences one or several manic episodes and may (but not necessarily) experience one or several major depressive episodes. Therefore, the mere presence of mania symptoms is sufficient for the diagnosis of bipolar I disorder (Sadock & Sadock, 2011).
The 12-month prevalence of bipolar I disorder in the USA is estimated to be 0.6% while that in 11 countries has been found to be 0–0.6% (American Psychiatric Association, 2013). Despite lower prevalence rates in comparison with the other mental disorders, such as major depressive disorder and anxiety disorders, bipolar I disorder may lead to functional degradation (Sadock & Sadock, 2011; Torres et al., 2018). Bipolar I disorder reduces the quality of life of patients (Van der Voort et al., 2015), and simultaneously imposes a financial burden on patients, families, and the society (Sammarco, 2016). The direct costs for the treatment of bipolar disorder include the costs of professional services, hospitalization, and medication, and the indirect costs are related to providing care for patients and loss of productivity. 33.5–65.2% of the overall costs for the treatment of patients with bipolar disorder are associated with hospitalization, which is one of the costliest aspects of bipolar disorder constituting about 50% of these medical costs.
Several studies have shown that the annual cost for the treatment of a patient with bipolar disorder is about $12764 and that for an ordinary patient is about $1340. Overall, patients with bipolar disorder utilize about 3-4-fold more healthcare resources than the patients with other disorders (Bergeson et al., 2012). As a result, despite similar education as their peers in the general population, patients with bipolar I disorder experience a considerable decline in the career position, which reduces their socioeconomic status (Sadock & Sadock, 2011). Therefore, correct diagnosis of the disorder, accurate estimation of its severity, and providing timely treatment are crucial for the treatment of bipolar I disorder. On the other hand, lack of appropriate and prompt treatment can lead to a high frequency of episodes, prolonged duration of each episode, and lack of appropriate response to treatment (Birmaher, 2013; Enderami, Monesi, & Zarghami, 2017). Therefore, using instruments that assess the symptoms continually from normal to severe provides an opportunity to identify the patients at the risk of developing the disorder and administer early interventions. One of the most common scales designed to assess the severity of mania symptoms is the Young Mania Rating Scale (YMRS) is developed based on the descriptions provided for the primary symptoms of mania. The YMRS assessed the severity of the mania symptoms according to the patient’s subjective report of their clinical state and also the clinician’s observations during the interview. In an initial study, Young found reliability coefficients ranging from 0.41 (appearance) to 0.85 (thought-language disorders), a total inert-rater reliability coefficient of 0.93, and inter-rater reliabilities ranging from 0.66 (aggressive-destructive behavior) to 0.95 (sleep). In order to assess the validity, the YMRS scores were compared to those on the Petterson and Beigel Scales; a correlation coefficient of 0.71 was observed between YMRS and Beigel Scale and 0.89 between YMRS and Petterson Scale (Miller, Johnson, & Eisner, 2009).
This questionnaire has been translated into several languages. Studies on psychometric properties of the Thai, French, Turkish, and Spanish versions of the YMRS indicated acceptable validity and reliability of the scale and its applicability for assessing the severity of the mania symptoms (Kongsakon & Bhatanaprabhabhan, 2005; Favre et al., 2003; Karadağ, Oral, Yalcin, & Erten, 2002; Colom et al, 2002). In Iran, the standardization of this scale on a sample of 120 manic patients indicated Cronbach’s alpha coefficient of 0.75, diagnostic validity of total scores and group membership of 0.31, and concurrent validity of YMRS with bipolar depression rating scale of 0.74 (Ebrahimi, Kheyr, Nasiri, & Barnamanesh, 2017). In the present study, none of the patients were reported in the manic or depressive phases of bipolar disorder during interviews. Given that the main objective of the present study was to determine the number of mania factors according to the dimensional model of DSM-5, the necessity of examining the psychometric characteristics of the YMRS in patients with bipolar I disorder in the manic phase becomes clear.
2. Methods
This cross-sectional study included all patients in the manic phase of bipolar I disorder from the Razi Psychiatric Hospital and Taleghani Hospital, and the general population of Tehran in 2016-2017 served as the control. This population consisted of a total of 97 patients in the manic phase of bipolar I disorder, and 160 healthy individuals were selected using a purposive sampling method and examined according to the inclusion and exclusion criteria. Due to attrition, 65 patients and 145 healthy individuals were included in the statistical analysis (Cronbach’s alpha coefficient, ROC curve, Pearson’s correlation coefficient, and confirmatory and exploratory factor analysis).
The inclusion criteria were as follows: diagnosis of bipolar I disorder based on clinical interviews for the patient group, absence of mental disorders for the controls, age 18–65 years, and ability to understand the questions. The exclusion criteria were as follows: drug abuse or addiction, mental retardation, severe physical disorders, and lack of willingness to participate in the study at any time. First, the medical records of the patients who were diagnosed with bipolar I disorder by a psychiatrist were examined with respect to the inclusion and exclusion criteria. Subsequently, the patients were examined using the SCID-I to verify the diagnosis of bipolar I disorder. If the diagnosis was confirmed based on SCID-I, the patient was included in the statistical analysis, or else excluded from the study. For the control group, healthy individuals, who had no history of severe mental or physical illness requiring pharmacological or psychological treatment, were selected from the general population. Then, the demographic information of the participants was collected, followed by YMRS. Before collecting the data, the study objectives were explained to the patients and healthy participants. All participants were reassured about confidential of their personal information. In addition, the participants were allowed to quit the study at any time. Data collection instruments are as following:
Structured clinical interview for DSM-IV axis I disorders (SCID-I) is a semi-structural clinical interview for axis 1 disorders, developed by Spitzer et al., (1988) (Segal, Kabacoff, Hersen, Van Hasselt, & Ryan, 1995). The clinical version of SCID-I only includes disorders that are commonly encountered in clinics. The research version of the SCID-I is comprised of axis I disorder with complete details and is useful in studies that require highly accurate details. The research version is considerably longer than the clinical version as it includes the coding of several diagnostic subgroups, severity ratings, course specifiers for many disorders, and features that are useful for diagnosis in research studies (Mohammad-Khani, Jahani Tabesh, & Tamanaie-far, 2013). The kappa coefficient for this interview was reported in the range of 0.53 (dysthymia) to 0.90 (major depressive disorder) (Segal et al., 1995). In Iran, the kappa coefficients >0.4 have been reported for all diagnoses except for anxiety disorders, and specificity has been found to be >0.85 for a majority of the diagnoses and >0.90 for half of this number, indicating that specificity is acceptable, but sensitivity is slightly low (Amini et al., 2008). The SCID-I-CV was used in the present study.
Young Mania Rating Scale (YMRS) comprised of eleven items that encompassed the main symptoms of the manic episode in terms of mood, mobility, sexual desire, sleep, irritability, speech, flight of ideas, grandiosity, aggressive behaviors, appearance, and one item that assesses the patient’s insight. Seven items were rated on a severity scale ranging from 0–4, and the four other items (irritability, speech, thought content, and aggressive-destructive behaviors) weighing twice the other items were rated on a scale ranging from 0–8. The administration time for the YMRS was 15–30 min (Bull, 2017).
The study data were analyzed using Cronbach’s alpha coefficient, ROC curve, Pearson’s correlation coefficient, exploratory and confirmatory factor analysis. All analyses were performed using SPSS version 23 and AMOS.
3. Results
A total of 144 women with an average age of 32.25 (SD=9.57) years and 66 men with an average age of 31.16 (SD=9.92) years participated in the present study. 63.8% of the patients were single, 28.1% were married, and 8.1% were divorced or widowed. In addition, 12.4% were illiterate or had elementary school education, 12.9% had middle school or high school education, 17.6% had a high school diploma, and 57.1% had a college education.
The Cronbach’s alpha coefficient was used to examine the internal consistency of YMRS. A Cronbach’s alpha of 0.72 was detected for the total scale. Among the scale items, thought content, insight, and thought-language disorder showed high reliability, and their exclusion reduced the Cronbach’s alpha level; however, irritability, aggression, and mobility have low reliabilities, and removing them did not reduce the Cronbach’s alpha level.
The ROC curve was used to examine the cut-off point, sensitivity, and specificity of YMRS (Figure 1). According to the ROC curve, the appropriate cut-off point for YMRS is 12.5, at which, the sensitivity and specificity coefficients were 0.93 and 0.96, respectively. Therefore, at this point, the YMRS correctly identifies 93% and incorrectly identifies 4% of the respondents as having mania. Nevertheless, YRMS detected 56 bipolar patients with mania (true positive), 6 healthy individuals with mania (false positive), 139 healthy individuals as healthy (true negative), and 9 bipolar patients as healthy (false negative) (Table 1).
Bipolar I disorder is a condition, in which the patient experiences one or several manic episodes and may (but not necessarily) experience one or several major depressive episodes. Therefore, the mere presence of mania symptoms is sufficient for the diagnosis of bipolar I disorder (Sadock & Sadock, 2011).
The 12-month prevalence of bipolar I disorder in the USA is estimated to be 0.6% while that in 11 countries has been found to be 0–0.6% (American Psychiatric Association, 2013). Despite lower prevalence rates in comparison with the other mental disorders, such as major depressive disorder and anxiety disorders, bipolar I disorder may lead to functional degradation (Sadock & Sadock, 2011; Torres et al., 2018). Bipolar I disorder reduces the quality of life of patients (Van der Voort et al., 2015), and simultaneously imposes a financial burden on patients, families, and the society (Sammarco, 2016). The direct costs for the treatment of bipolar disorder include the costs of professional services, hospitalization, and medication, and the indirect costs are related to providing care for patients and loss of productivity. 33.5–65.2% of the overall costs for the treatment of patients with bipolar disorder are associated with hospitalization, which is one of the costliest aspects of bipolar disorder constituting about 50% of these medical costs.
Several studies have shown that the annual cost for the treatment of a patient with bipolar disorder is about $12764 and that for an ordinary patient is about $1340. Overall, patients with bipolar disorder utilize about 3-4-fold more healthcare resources than the patients with other disorders (Bergeson et al., 2012). As a result, despite similar education as their peers in the general population, patients with bipolar I disorder experience a considerable decline in the career position, which reduces their socioeconomic status (Sadock & Sadock, 2011). Therefore, correct diagnosis of the disorder, accurate estimation of its severity, and providing timely treatment are crucial for the treatment of bipolar I disorder. On the other hand, lack of appropriate and prompt treatment can lead to a high frequency of episodes, prolonged duration of each episode, and lack of appropriate response to treatment (Birmaher, 2013; Enderami, Monesi, & Zarghami, 2017). Therefore, using instruments that assess the symptoms continually from normal to severe provides an opportunity to identify the patients at the risk of developing the disorder and administer early interventions. One of the most common scales designed to assess the severity of mania symptoms is the Young Mania Rating Scale (YMRS) is developed based on the descriptions provided for the primary symptoms of mania. The YMRS assessed the severity of the mania symptoms according to the patient’s subjective report of their clinical state and also the clinician’s observations during the interview. In an initial study, Young found reliability coefficients ranging from 0.41 (appearance) to 0.85 (thought-language disorders), a total inert-rater reliability coefficient of 0.93, and inter-rater reliabilities ranging from 0.66 (aggressive-destructive behavior) to 0.95 (sleep). In order to assess the validity, the YMRS scores were compared to those on the Petterson and Beigel Scales; a correlation coefficient of 0.71 was observed between YMRS and Beigel Scale and 0.89 between YMRS and Petterson Scale (Miller, Johnson, & Eisner, 2009).
This questionnaire has been translated into several languages. Studies on psychometric properties of the Thai, French, Turkish, and Spanish versions of the YMRS indicated acceptable validity and reliability of the scale and its applicability for assessing the severity of the mania symptoms (Kongsakon & Bhatanaprabhabhan, 2005; Favre et al., 2003; Karadağ, Oral, Yalcin, & Erten, 2002; Colom et al, 2002). In Iran, the standardization of this scale on a sample of 120 manic patients indicated Cronbach’s alpha coefficient of 0.75, diagnostic validity of total scores and group membership of 0.31, and concurrent validity of YMRS with bipolar depression rating scale of 0.74 (Ebrahimi, Kheyr, Nasiri, & Barnamanesh, 2017). In the present study, none of the patients were reported in the manic or depressive phases of bipolar disorder during interviews. Given that the main objective of the present study was to determine the number of mania factors according to the dimensional model of DSM-5, the necessity of examining the psychometric characteristics of the YMRS in patients with bipolar I disorder in the manic phase becomes clear.
2. Methods
This cross-sectional study included all patients in the manic phase of bipolar I disorder from the Razi Psychiatric Hospital and Taleghani Hospital, and the general population of Tehran in 2016-2017 served as the control. This population consisted of a total of 97 patients in the manic phase of bipolar I disorder, and 160 healthy individuals were selected using a purposive sampling method and examined according to the inclusion and exclusion criteria. Due to attrition, 65 patients and 145 healthy individuals were included in the statistical analysis (Cronbach’s alpha coefficient, ROC curve, Pearson’s correlation coefficient, and confirmatory and exploratory factor analysis).
The inclusion criteria were as follows: diagnosis of bipolar I disorder based on clinical interviews for the patient group, absence of mental disorders for the controls, age 18–65 years, and ability to understand the questions. The exclusion criteria were as follows: drug abuse or addiction, mental retardation, severe physical disorders, and lack of willingness to participate in the study at any time. First, the medical records of the patients who were diagnosed with bipolar I disorder by a psychiatrist were examined with respect to the inclusion and exclusion criteria. Subsequently, the patients were examined using the SCID-I to verify the diagnosis of bipolar I disorder. If the diagnosis was confirmed based on SCID-I, the patient was included in the statistical analysis, or else excluded from the study. For the control group, healthy individuals, who had no history of severe mental or physical illness requiring pharmacological or psychological treatment, were selected from the general population. Then, the demographic information of the participants was collected, followed by YMRS. Before collecting the data, the study objectives were explained to the patients and healthy participants. All participants were reassured about confidential of their personal information. In addition, the participants were allowed to quit the study at any time. Data collection instruments are as following:
Structured clinical interview for DSM-IV axis I disorders (SCID-I) is a semi-structural clinical interview for axis 1 disorders, developed by Spitzer et al., (1988) (Segal, Kabacoff, Hersen, Van Hasselt, & Ryan, 1995). The clinical version of SCID-I only includes disorders that are commonly encountered in clinics. The research version of the SCID-I is comprised of axis I disorder with complete details and is useful in studies that require highly accurate details. The research version is considerably longer than the clinical version as it includes the coding of several diagnostic subgroups, severity ratings, course specifiers for many disorders, and features that are useful for diagnosis in research studies (Mohammad-Khani, Jahani Tabesh, & Tamanaie-far, 2013). The kappa coefficient for this interview was reported in the range of 0.53 (dysthymia) to 0.90 (major depressive disorder) (Segal et al., 1995). In Iran, the kappa coefficients >0.4 have been reported for all diagnoses except for anxiety disorders, and specificity has been found to be >0.85 for a majority of the diagnoses and >0.90 for half of this number, indicating that specificity is acceptable, but sensitivity is slightly low (Amini et al., 2008). The SCID-I-CV was used in the present study.
Young Mania Rating Scale (YMRS) comprised of eleven items that encompassed the main symptoms of the manic episode in terms of mood, mobility, sexual desire, sleep, irritability, speech, flight of ideas, grandiosity, aggressive behaviors, appearance, and one item that assesses the patient’s insight. Seven items were rated on a severity scale ranging from 0–4, and the four other items (irritability, speech, thought content, and aggressive-destructive behaviors) weighing twice the other items were rated on a scale ranging from 0–8. The administration time for the YMRS was 15–30 min (Bull, 2017).
The study data were analyzed using Cronbach’s alpha coefficient, ROC curve, Pearson’s correlation coefficient, exploratory and confirmatory factor analysis. All analyses were performed using SPSS version 23 and AMOS.
3. Results
A total of 144 women with an average age of 32.25 (SD=9.57) years and 66 men with an average age of 31.16 (SD=9.92) years participated in the present study. 63.8% of the patients were single, 28.1% were married, and 8.1% were divorced or widowed. In addition, 12.4% were illiterate or had elementary school education, 12.9% had middle school or high school education, 17.6% had a high school diploma, and 57.1% had a college education.
The Cronbach’s alpha coefficient was used to examine the internal consistency of YMRS. A Cronbach’s alpha of 0.72 was detected for the total scale. Among the scale items, thought content, insight, and thought-language disorder showed high reliability, and their exclusion reduced the Cronbach’s alpha level; however, irritability, aggression, and mobility have low reliabilities, and removing them did not reduce the Cronbach’s alpha level.
The ROC curve was used to examine the cut-off point, sensitivity, and specificity of YMRS (Figure 1). According to the ROC curve, the appropriate cut-off point for YMRS is 12.5, at which, the sensitivity and specificity coefficients were 0.93 and 0.96, respectively. Therefore, at this point, the YMRS correctly identifies 93% and incorrectly identifies 4% of the respondents as having mania. Nevertheless, YRMS detected 56 bipolar patients with mania (true positive), 6 healthy individuals with mania (false positive), 139 healthy individuals as healthy (true negative), and 9 bipolar patients as healthy (false negative) (Table 1).
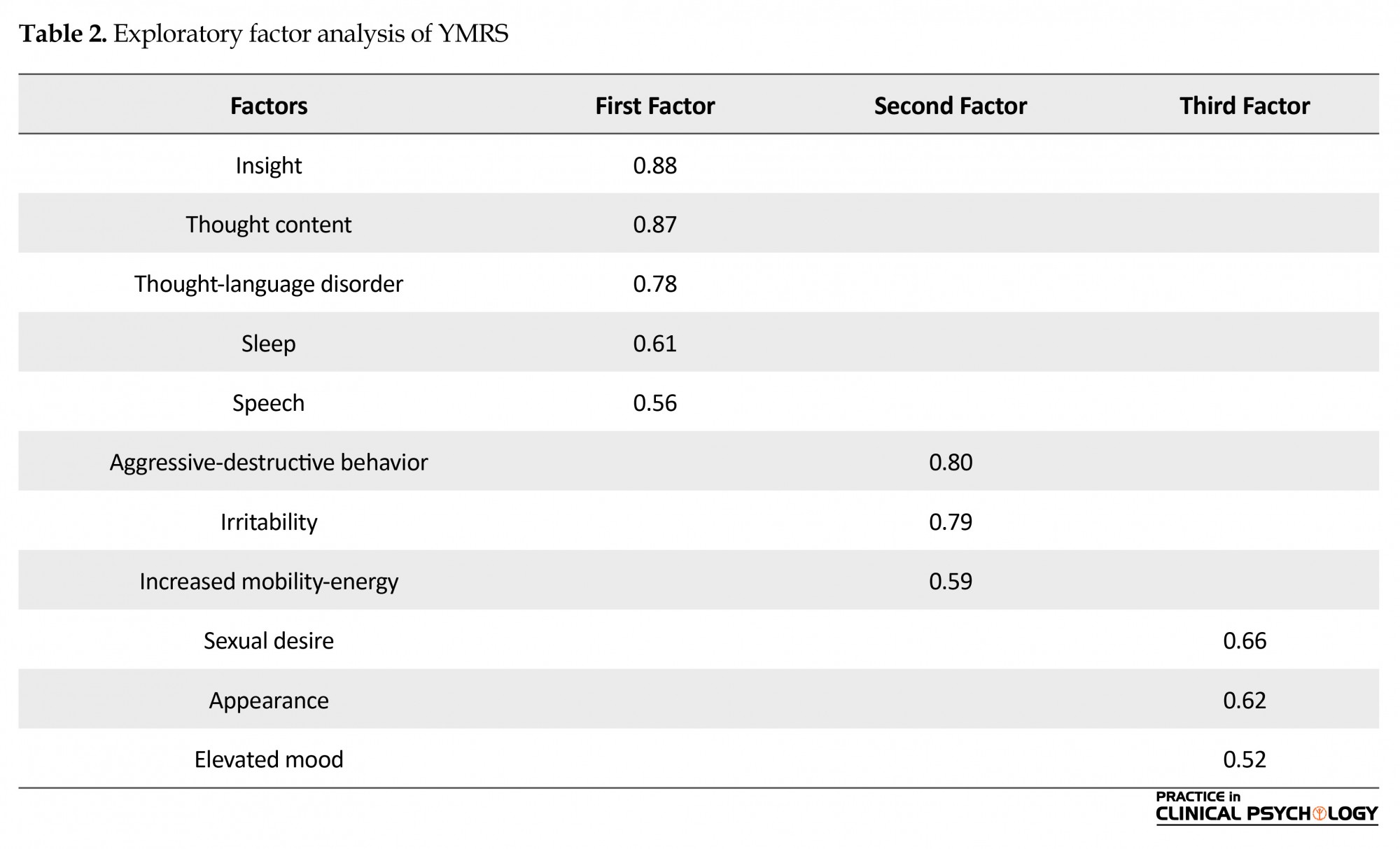
In the process of Exploratory Factor Analysis (EFA), first, the KMO coefficient was used to assess the adequacy of the sample size. A KMO of 0.73 (>0.7) indicated the adequacy of sample size for factor analysis. According to the EFA results, the first factor included five items: insight, thought content, thought-language disorder, sleep, and speech; the second factor included three items: aggressive-destructive behavior, irritability, and increased mobility-energy; the third factor included three items: sexual desire, appearance, and elevated mood. The EFA results are presented in Table 2. According to CFA, the goodness-of-fit indices, including chi-Square, Root-Mean-Square Error (RMSE), Comparative Fit Index (CFI), and Normed Fit Index (NFI) indicated a good fit of the model with the data (Table 3, Figure 2).
4. Discussion
The present study was aimed at examining the psychometric properties of the YMRS. The study findings indicated that the YMRS had good internal consistency as that of an index of reliability. This finding was consistent with those Karadağ et al. (2002). According to the analysis of item reliability, if the items related to irritability and aggressive-destructive behavior are removed and the energy level increased, the internal consistency of the scale improves. Given the nature of the study sample consisting of hospitalized patients in psychiatric wards, the participants would not answer these items, as manic patients with high irritability, aggression, and energy are usually admitted to the emergency department.
Regarding distinguishing the patients with bipolar disorder from controls, the ROC curve showed that the best cut-off point for the YMRS was 12.5 with 93% and 96% sensitivity and specificity, respectively. This finding was in line with those of Turkoz, Fu, Bossie, Sheehan, & Alphs (2013), thereby indicating that YMRS is useful in screening bipolar patients in the manic phase. The present results also indicated a high agreement between psychiatric interview and YMRS in diagnosing mental disorders, which might be attributed to the psychiatric interview and YMRS based on the diagnostic criteria of DSM, indicating an empirical approach (Trull & Prinstein, 2012).
The CFA revealed a three-factor structure for the YMRS which is consistent with the multidimensional structure of mania reported previously (Hanwella & Silva, 2011). The first factor consists of insight, thought content, thought-language disorder, sleep, and speech. This factor can be labeled as “psychotic mania” because, in YMRS, most psychotic features are categorized under “thought content,” assessing grandiosity, paranoia, attributional beliefs, hallucinations, and delusions. Therefore, the first factor can be regarded as representing a severe form of mania.
The second factor consists of aggressive-destructive behavior, irritability, and increased mobility-energy. One of the most important findings of this study was identifying a factor, known as “irritable mania” that is neither included as a distinct category in DSM-5 nor ICD-10. However, there is lack of evidence to support this finding. The third factor includes sexual desire, appearance, and elevated mood. Most previous studies identified an elevated mood, hypersexuality, and grandiosity as core features of mania (Gupta, Sinha, Praharaj, & Gandotra, 2009). The scale used in the present study (YMRS) did not have a distinct item, such as grandiosity, and grandiosity along with delusions and hallucinations were was categorized as “thought content” that was not loaded on this factor.
Overall, the study results showed that the YMRS exhibited appropriate psychometric properties in assessing the severity of mania symptoms in patients with bipolar disorder, and its use is recommended for the following reasons: 1. Good validity and reliability; 2. Short, easy-to-use; and 3. Cost-effective instrument. The items have been selected such that they reflect the main symptoms of the manic phase of bipolar disorder based on the DSM criteria.
Despite the advantages mentioned above, the present study had some limitations. The YMRS is a self-report scale, and therefore, the scores on the scale may alter according to the severity of symptoms and the level of psychological disturbance. In addition, the patient group only included 65 hospitalized patients. Thus, future studies are also suggested to examine outpatients and use larger samples. Finally, owing to small sample size, caution should be exercised in interpreting the study results. In summary, mania has three dimensions: psychotic mania, irritable mania, and a third factor that is the core of mania included elevated mood, sexual desire, and appearance.
Ethical Considerations
Compliance with ethical guidelines
All participants were reassured about confidential of their personal information. In addition, the participants were allowed to quit the study at any time.
Funding
This paper is an outcome of the first author’s Master’s thesis work on clinical psychology from the University of Social Welfare and Rehabilitation Sciences.
Conflict of interests
All authors certify that this manuscript has neither been published in whole nor in part nor being considered for publication elsewhere. The authors have no conflicts of interest to declare.
References
The present study was aimed at examining the psychometric properties of the YMRS. The study findings indicated that the YMRS had good internal consistency as that of an index of reliability. This finding was consistent with those Karadağ et al. (2002). According to the analysis of item reliability, if the items related to irritability and aggressive-destructive behavior are removed and the energy level increased, the internal consistency of the scale improves. Given the nature of the study sample consisting of hospitalized patients in psychiatric wards, the participants would not answer these items, as manic patients with high irritability, aggression, and energy are usually admitted to the emergency department.
Regarding distinguishing the patients with bipolar disorder from controls, the ROC curve showed that the best cut-off point for the YMRS was 12.5 with 93% and 96% sensitivity and specificity, respectively. This finding was in line with those of Turkoz, Fu, Bossie, Sheehan, & Alphs (2013), thereby indicating that YMRS is useful in screening bipolar patients in the manic phase. The present results also indicated a high agreement between psychiatric interview and YMRS in diagnosing mental disorders, which might be attributed to the psychiatric interview and YMRS based on the diagnostic criteria of DSM, indicating an empirical approach (Trull & Prinstein, 2012).
The CFA revealed a three-factor structure for the YMRS which is consistent with the multidimensional structure of mania reported previously (Hanwella & Silva, 2011). The first factor consists of insight, thought content, thought-language disorder, sleep, and speech. This factor can be labeled as “psychotic mania” because, in YMRS, most psychotic features are categorized under “thought content,” assessing grandiosity, paranoia, attributional beliefs, hallucinations, and delusions. Therefore, the first factor can be regarded as representing a severe form of mania.
The second factor consists of aggressive-destructive behavior, irritability, and increased mobility-energy. One of the most important findings of this study was identifying a factor, known as “irritable mania” that is neither included as a distinct category in DSM-5 nor ICD-10. However, there is lack of evidence to support this finding. The third factor includes sexual desire, appearance, and elevated mood. Most previous studies identified an elevated mood, hypersexuality, and grandiosity as core features of mania (Gupta, Sinha, Praharaj, & Gandotra, 2009). The scale used in the present study (YMRS) did not have a distinct item, such as grandiosity, and grandiosity along with delusions and hallucinations were was categorized as “thought content” that was not loaded on this factor.
Overall, the study results showed that the YMRS exhibited appropriate psychometric properties in assessing the severity of mania symptoms in patients with bipolar disorder, and its use is recommended for the following reasons: 1. Good validity and reliability; 2. Short, easy-to-use; and 3. Cost-effective instrument. The items have been selected such that they reflect the main symptoms of the manic phase of bipolar disorder based on the DSM criteria.
Despite the advantages mentioned above, the present study had some limitations. The YMRS is a self-report scale, and therefore, the scores on the scale may alter according to the severity of symptoms and the level of psychological disturbance. In addition, the patient group only included 65 hospitalized patients. Thus, future studies are also suggested to examine outpatients and use larger samples. Finally, owing to small sample size, caution should be exercised in interpreting the study results. In summary, mania has three dimensions: psychotic mania, irritable mania, and a third factor that is the core of mania included elevated mood, sexual desire, and appearance.
Ethical Considerations
Compliance with ethical guidelines
All participants were reassured about confidential of their personal information. In addition, the participants were allowed to quit the study at any time.
Funding
This paper is an outcome of the first author’s Master’s thesis work on clinical psychology from the University of Social Welfare and Rehabilitation Sciences.
Conflict of interests
All authors certify that this manuscript has neither been published in whole nor in part nor being considered for publication elsewhere. The authors have no conflicts of interest to declare.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). New York: American Psychiatric Association. [DOI:10.1176/appi.books.9780890425596]
- Amini, H., Sharifi, V., Asadi, S., Mohammadi, M. R., Kaviani, H., Semnani, Y., et al. (2008). Validity of the Iranian version of the structured clinical interview for DSM-IV (SCID-I) in the diagnosis of psychiatric disorders. Payesh, 7(1), 49-57.
- Bergeson, J. G., Kalsekar, I., Jing, Y., You, M., Forbes, R. A., & Hebden, T. (2012). Medical care costs and hospitalization in patients with bipolar disorder treated with atypical antipsychotics. American Health & Drug Benefits, 5(6), 379-86. [PMID] [PMCID]
- Birmaher, B. (2013). Bipolar disorder in children and adolescents. Child and Adolescent Mental Health, 18(3), 140–148.[DOI:10.1111/camh.12021] [PMID] [PMCID]
- Bull, P. (2017). Rating scales and safety measurements in bipolar disorder and schizophrenia–a reference guide. Psychopharmacology Bulletin, 47(3), 77-109. [PMID] [PMCID]
- Colom, F., Vieta, E., Martínez-Arán, A., Garcia-Garcia, M., Reinares, M., Torrent, C., et al. (2002). [Spanish version of a scale for the assessment of mania: validity and reliability of the Young Mania Rating Scale (Spanish)]. Medicina Clínica, 119(10), 366–71. [DOI:10.1016/S0025-7753(02)73419-2]
- Ebrahimi, A., Kheyr, Z., Nasiri, H., & Barnamanesh, A. (2017). [Reliability, validity, factor and discrimination power analysis of young mania rating scale among unipolar, bipolar depression and healthy people (Persian)]. Jundishapur Scientific Medical Journal, 16(3), 333-44.
- Enderami, A., Monesi, F., & Zarghami, M. (2017). One-year follow-up of patients with a diagnosis of first episode psychosis. Materia Socio Medica, 29(1), 21. [DOI:10.5455/msm.2017.29.21-25] [PMID] [PMCID]
- Favre, S., Aubry, J., Gex-Fabry, M., Ragama-Pardos, E., McQuillan, A., & Bertschy, G. (2003). Translation and validation of a French version of the Young Mania Rating Scale (YMRS). L’Encephale, 29(6), 499-505. [PMID]
- Gupta, S. C., Sinha, V. K., Praharaj, S. K., & Gandotra, S. (2009). Factor structure of manic symptoms. Australian & New Zealand Journal of Psychiatry, 43(12), 1141–6.[DOI:10.3109/00048670903279853] [PMID]
- Hanwella, R., & de Silva, V. A. (2011). Signs and symptoms of acute mania: a factor analysis. BMC Psychiatry, 11(1), 137.[DOI:10.1186/1471-244X-11-137] [PMID] [PMCID]
- Karadağ, F., Oral, T., Yalcin, F. A., & Erten E. (2002). [Reliability and validity of Turkish translation of young mania rating scale (Turkish)]. Turkish Journal of Psychiatry, 13(2), 107-14. [PMID]
- Kongsakon, R., & Bhatanaprabhabhan, D. (2005). Validity and reliability of the Young Mania Rating Scale: Thai version. Journal of the Medical Association of Thailand, 88(11), 1598-604. [PMID]
- Miller, C. J., Johnson, S. L., & Eisner, L. (2009). Assessment tools for adult bipolar disorder. Clinical Psychology: Science and Practice, 16(2), 188–201. [DOI:10.1111/j.1468-2850.2009.01158.x]
- Mohammad-Khani P. J. M., Jahani Tabesh, A., & Tamanaie-far, S. (2013). [Structured clinical interview for DSM-IV-TR (Persian)]. Tehran: Danjeh Publication.
- Sadock BJ, Sadock VA. (2011). Kaplan and Sadock’s synopsis of psychiatry: Behavioral sciences/clinical psychiatry. Philadelphia, Pennsylvania: Lippincott Williams & Wilkins.
- Sammarco, A. (2016). Women’s health issues across the life cycle. Burlington, Massachusetts: Jones & Bartlett Publishers.
- Segal, D. L., Kabacoff, R. I., Hersen, M., Van Hasselt, V. B., & Ryan, C. (1995). Update on the reliability of diagnosis in older psychiatric outpatients using the Structured Clinical Interview for DSM-III-R. Journal of Clinical Geropsychology, 1(4), 313-21.
- Torres, I., Garriga, M., Sole, B., Bonnín, C. M., Corrales, M., Jiménez, E., et al. (2018). Functional impairment in adult bipolar disorder with ADHD. Journal of Affective Disorders. 227, 117-25. [DOI:10.1016/j.jad.2017.09.037] [PMID]
- Trull, T., & Prinstein, M. (2012). Clinical psychology. Belmont: Wadsworth Publishing.
- Turkoz, I., Fu, D. J., Bossie, C. A., Sheehan, J. J., & Alphs, L. (2013). Relationship between the clinical global impression of severity for schizoaffective disorder scale and established mood scales for mania and depression. Journal of Affective Disorders, 150(1), 17–22. [DOI:10.1016/j.jad.2013.01.047] [PMID]
- Van der Voort, T. Y. G., van Meijel, B., Hoogendoorn, A. W., Goossens, P. J. J., Beekman, A. T. F., & Kupka, R. W. (2015). Collaborative care for patients with bipolar disorder: Effects on functioning and quality of life. Journal of Affective Disorders, 179, 14–22. [DOI:10.1016/j.jad.2015.03.005] [PMID]
Type of Study: Research |
Subject:
Psychometric
Received: 2018/02/17 | Accepted: 2018/05/12 | Published: 2018/07/1
Received: 2018/02/17 | Accepted: 2018/05/12 | Published: 2018/07/1
References
1. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). New York: American Psychiatric Association. [DOI:10.1176/appi.books.9780890425596] [DOI:10.1176/appi.books.9780890425596]
2. Amini, H., Sharifi, V., Asadi, S., Mohammadi, M. R., Kaviani, H., Semnani, Y., et al. (2008). Validity of the Iranian version of the structured clinical interview for DSM-IV (SCID-I) in the diagnosis of psychiatric disorders. Payesh, 7(1), 49-57.
3. Bergeson, J. G., Kalsekar, I., Jing, Y., You, M., Forbes, R. A., & Hebden, T. (2012). Medical care costs and hospitalization in patients with bipolar disorder treated with atypical antipsychotics. American Health & Drug Benefits, 5(6), 379-86. [PMID] [PMCID] [PMID] [PMCID]
4. Birmaher, B. (2013). Bipolar disorder in children and adolescents. Child and Adolescent Mental Health, 18(3), 140–148.[DOI:10.1111/camh.12021] [PMID] [PMCID] [DOI:10.1111/camh.12021]
5. Bull, P. (2017). Rating scales and safety measurements in bipolar disorder and schizophrenia–a reference guide. Psychopharmacology Bulletin, 47(3), 77-109. [PMID] [PMCID]
6. Colom, F., Vieta, E., Martínez-Arán, A., Garcia-Garcia, M., Reinares, M., Torrent, C., et al. (2002). [Spanish version of a scale for the assessment of mania: validity and reliability of the Young Mania Rating Scale (Spanish)]. Medicina Clínica, 119(10), 366–71. [DOI:10.1016/S0025-7753(02)73419-2] [DOI:10.1016/S0025-7753(02)73419-2]
7. Ebrahimi, A., Kheyr, Z., Nasiri, H., & Barnamanesh, A. (2017). [Reliability, validity, factor and discrimination power analysis of young mania rating scale among unipolar, bipolar depression and healthy people (Persian)]. Jundishapur Scientific Medical Journal, 16(3), 333-44.
8. Enderami, A., Monesi, F., & Zarghami, M. (2017). One-year follow-up of patients with a diagnosis of first episode psychosis. Materia Socio Medica, 29(1), 21. [DOI:10.5455/msm.2017.29.21-25] [PMID] [PMCID] [DOI:10.5455/msm.2017.29.21-25]
9. Favre, S., Aubry, J., Gex-Fabry, M., Ragama-Pardos, E., McQuillan, A., & Bertschy, G. (2003). Translation and validation of a French version of the Young Mania Rating Scale (YMRS). L'Encephale, 29(6), 499-505. [PMID] [PMID]
10. Gupta, S. C., Sinha, V. K., Praharaj, S. K., & Gandotra, S. (2009). Factor structure of manic symptoms. Australian & New Zealand Journal of Psychiatry, 43(12), 1141–6.[DOI:10.3109/00048670903279853] [PMID] [DOI:10.3109/00048670903279853]
11. Hanwella, R., & de Silva, V. A. (2011). Signs and symptoms of acute mania: a factor analysis. BMC Psychiatry, 11(1), 137.[DOI:10.1186/1471-244X-11-137] [PMID] [PMCID] [DOI:10.1186/1471-244X-11-137]
12. Karadağ, F., Oral, T., Yalcin, F. A., & Erten E. (2002). [Reliability and validity of Turkish translation of young mania rating scale (Turkish)]. Turkish Journal of Psychiatry, 13(2), 107-14. [PMID] [PMID]
13. Kongsakon, R., & Bhatanaprabhabhan, D. (2005). Validity and reliability of the Young Mania Rating Scale: Thai version. Journal of the Medical Association of Thailand, 88(11), 1598-604. [PMID] [PMID]
14. Miller, C. J., Johnson, S. L., & Eisner, L. (2009). Assessment tools for adult bipolar disorder. Clinical Psychology: Science and Practice, 16(2), 188–201. [DOI:10.1111/j.1468-2850.2009.01158.x] [DOI:10.1111/j.1468-2850.2009.01158.x]
15. Mohammad-Khani P. J. M., Jahani Tabesh, A., & Tamanaie-far, S. (2013). [Structured clinical interview for DSM-IV-TR (Persian)]. Tehran: Danjeh Publication.
16. Sadock BJ, Sadock VA. (2011). Kaplan and Sadock's synopsis of psychiatry: Behavioral sciences/clinical psychiatry. Philadelphia, Pennsylvania: Lippincott Williams & Wilkins.
17. Sammarco, A. (2016). Women's health issues across the life cycle. Burlington, Massachusetts: Jones & Bartlett Publishers.
18. Segal, D. L., Kabacoff, R. I., Hersen, M., Van Hasselt, V. B., & Ryan, C. (1995). Update on the reliability of diagnosis in older psychiatric outpatients using the Structured Clinical Interview for DSM-III-R. Journal of Clinical Geropsychology, 1(4), 313-21.
19. Torres, I., Garriga, M., Sole, B., Bonnín, C. M., Corrales, M., Jiménez, E., et al. (2018). Functional impairment in adult bipolar disorder with ADHD. Journal of Affective Disorders. 227, 117-25. [DOI:10.1016/j.jad.2017.09.037] [PMID] [DOI:10.1016/j.jad.2017.09.037]
20. Trull, T., & Prinstein, M. (2012). Clinical psychology. Belmont: Wadsworth Publishing.
21. Turkoz, I., Fu, D. J., Bossie, C. A., Sheehan, J. J., & Alphs, L. (2013). Relationship between the clinical global impression of severity for schizoaffective disorder scale and established mood scales for mania and depression. Journal of Affective Disorders, 150(1), 17–22. [DOI:10.1016/j.jad.2013.01.047] [PMID] [DOI:10.1016/j.jad.2013.01.047]
22. Van der Voort, T. Y. G., van Meijel, B., Hoogendoorn, A. W., Goossens, P. J. J., Beekman, A. T. F., & Kupka, R. W. (2015). Collaborative care for patients with bipolar disorder: Effects on functioning and quality of life. Journal of Affective Disorders, 179, 14–22. [DOI:10.1016/j.jad.2015.03.005] [PMID] [DOI:10.1016/j.jad.2015.03.005]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |