Volume 6, Issue 3 (Summer 2018)
PCP 2018, 6(3): 153-158 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Lotfi M, Amini M, Fathi A, Karami A, Ghiasi S, Sadeghi S. Cognitive Emotion Regulation Strategies in Prisoners With Borderline Personality Disorder. PCP 2018; 6 (3) :153-158
URL: http://jpcp.uswr.ac.ir/article-1-530-en.html
URL: http://jpcp.uswr.ac.ir/article-1-530-en.html
1- Department of Mental Health, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran.
2- Addiction Department, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran. , amini.mh@iums.ac.ir
3- Department of Criminal Law and Criminology, Tehran Prisons Office, Tehran, Iran.
4- Department of Psychology, Tehran Prisons office, Tehran, Iran.
5- Department of Clinical Psychology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
2- Addiction Department, School of Behavioral Sciences and Mental Health (Tehran Institute of Psychiatry), Iran University of Medical Sciences, Tehran, Iran. , amini.mh@iums.ac.ir
3- Department of Criminal Law and Criminology, Tehran Prisons Office, Tehran, Iran.
4- Department of Psychology, Tehran Prisons office, Tehran, Iran.
5- Department of Clinical Psychology, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran.
Full-Text [PDF 708 kb]
(2453 Downloads)
| Abstract (HTML) (5057 Views)
Full-Text: (1514 Views)
1. Introduction
Borderline Personality Disorder (BPD) is one of the most serious mental problems, and approximately prevalent in 1-2% of the general population (Morey, 2017). This disorder is characterized by the extreme instability of affect, mood, behavior, object relations, and self-concept (Bender, Morey, & Skodol, 2011). Patients with BPD are on the neurosis and psychosis border. These patients always seem to be in a critical state, and mood swing is a commonly observed symptom (Sadock, Kaplan, & Sadock, 2015). BPD is associated with comorbidity with other psychiatric disorders, thus leading to 10% suicide rate in people with BPD, which is quite high (Maj, 2010). BPD is the most common personality disorder diagnosed in clinical settings. Nearly, 15 to 50% of hospitalized patients and 11% of outpatient patients have been diagnosed with symptoms of BPD (American Psychiatric Association, 2000). Chronic and intense dysphoria, mood reactivity or affective lability, cognitive problems, recurrent suicidal attempts, behavior or gestures of self-mutilation, etc., are seen in patients suffering from BPD (Bender et al., 2011; Millon, Grossman, Millon, Meagher, & Ramnath, 2004). These signs and symptoms are emotion-based reactions. Researchers have increasingly come to view emotional impairments and dysregulations as the core features of BPD (Doering et al., 2013; Hutsebaut, Feenstra, & Kamphuis, 2016; Hutsebaut, Kamphuis, Feenstra, Weekers, & De Saeger, 2017; Jablensky, 2010).
The Emotional Dysregulation (ED) refers to emotional responses that are weakly modulated (Morey, 2017). These responses are often different from the usual and accepted ones. Some of the EDs in people with BPD include emotional disturbance, intense and suddenly occurred anger, aggressive behaviors, such as destroying objects, attacks on others and self-harm. Such reactions can lead to behavioral problems and affect the social interactions and individual’s relationships (Doering et al., 2013). Based on the theory of emotion regulation, if the individual with BPD who are healthy and adaptive can easily regulate his/her emotions or he/she can act healthy and adaptive (Morey, 2017; Skodol et al., 2011). Therefore, emphasis has been laid upon emotion regulation training as a treatment option for BPD, which presents clear implications in cognitive-behavior therapy used in treating BPD.
Despite the essential role of emotional disturbances in theoretical accounts of BPD (Bateman & Fonagy, 2010; Goldberg, 2010), most of the studies indicated a significant relationship between emotion regulation strategies and BPD symptoms (Lotfi, Amini, Fathi, Karami, & Ghiasi, 2014; Putnam & Silk, 2005). In addition, many studies have focused on two commonly used strategies for down-regulating emotions (Gratz, Rosenthal, Tull, Lejuez, & Gunderson, 2006; Gunderson et al., 2011) and few have examined cognitive emotion regulation strategies specifically. Moreover, although previous studies (Gratz et al., 2006; Kim, Sharp, & Carbone, 2014; Koenigsberg et al., 2010; Lotfi et al., 2014) have found that the features of BPD have a negative correlation with the adaptive strategies and a positive correlation with the maladaptive strategies of cognitive emotion regulation, and BPD is associated with low levels of acceptance and cognitive reappraisal, and high levels of rumination, catastrophizing suppression and avoidance, there is not a large amount of research about adaptive and maladaptive cognitive emotion regulation strategies in BPD. Also, most of the studies were done on non-clinical participants. So, the purpose of this study was to examine the cognitive emotion regulation strategies among prisoners with BPD and compare them with the normal population. In other words, the main aim of this study was to achieve the patterns of cognitive emotion regulation strategies between prisoners with BPD.
2. Methods
This study was a cross-sectional study. Ninety prisoners with BPD and 92 non-clinical individuals participated in this study. Given that the CERQ has 9 strategies and statistically at least 10 participants are required to investigate each of the strategies, the initial sample was 90. However, to increase the power of statistical analysis, 182 samples were selected using purposive and convenience sampling procedure for prisoners and non-clinical individuals, respectively. Non-clinical participants were selected from two university students in Tehran. Participants were paired based on their age and gender. All participants were male. Subjects aged 18 to 50 years, with guidance school degree of study and higher were selected. Inclusion criteria were guidance school and higher education and having symptoms of BPD (for prisoners). The exclusion criteria included having any history of head trauma, serious mental disorders, such as schizophrenia, bipolar disorder, etc., and showing no interesting to participate in the study.
Structured Clinical Interview for DSM-IV-II (SCID-II) and its versions are the one of the most comprehensive of the structured diagnostic interviews which is available (First, Gibbon, & Spitzer, 1997; Groth-Marnat, 2009). Due to the high accuracy of the diagnostic criteria and high clinical utility since the codification, translation and adaption to different languages, the SCID-II and SCID-PQ have been translated into Farsi and adapted with the Iranian culture (Mohammadkhani, Jokar, Jahani-tabesh, & Tamannaei-far, 2011). The test-retest reliability of the SCID-II and its internal consistency refers to intermediate results. For example, its test-retest consistency for diagnosis was between 0.40 and 0.86 with a mean of xxx (First, et al., 1997). Due to the fact that SCID has been made based on DSM, it seems to have good validity.
Cognitive Emotion Regulation Questionnaire (CERQ) (Garnefski & Kraaij, 2007) is a 36-item scale measuring the strategies of cognitive emotion regulation. These strategies essentially refer to how someone actually thinks about situations, when experiencing threatening or stressful life events. The questionnaire consists of 9 subscales, scored on a 5-point Likert scale (1: never to 5: always). The strategies that were evaluated by CERQ are as follows: Catastrophizing, putting into perspective, self-blame, other blame, rumination, positive reappraisal, positive refocusing, acceptance and planning. The CERQ has shown excellent reliability and validity (Garnefski & Kraaij, 2007). In Iranian sample, Yousefi reported good reliability score of 0.82. Cronbach’s alpha value ranged from 0.65 (acceptance) to 0.81 (self-blame).
In the data gathering process, three MSc. graduates in clinical psychology were trained in the SCID-II interview, who then interviewed the participants and asked them to complete the CERQ. In order to uphold the principles of research ethics at first, the purpose of the research and its process was explained, and the participants were allowed to leave the study whenever they want. The data were analyzed by independent t test and correlation coefficient via SPSS-16 software.
3. Results
Independent t test was used to compare the age difference between the prisoners and non-clinical groups. The results showed that there was not any significant difference in age (M=0.29, SD=0.37, P=0.71) between prisoners/BPD (M=1.33, SD=0.51) and non-clinical group (M=1.30, SD=0.53). Also, independent t-test was used to compare the means of variables (Table 1). Means and standard deviations showed that there was a significant differences between prisoners/BPD and non-clinical group in self-blame; t(180)=4.60, P=0.00, other blame; t(180)=8.35, P=0.00, rumination; t(180)=17.28, P=0.00, catastrophizing; t(180)=7.20, P=0.00, putting into perspective; t(180)=-4.80, P=0.00, positive refocusing; t(180)=5.19, P=0.00, positive reappraisal; t(180)=-6.80, P=0.00, acceptance; t(180)=-4.64, P=0.00, and planning; t(180)=-3.26, P=0.00.
Borderline Personality Disorder (BPD) is one of the most serious mental problems, and approximately prevalent in 1-2% of the general population (Morey, 2017). This disorder is characterized by the extreme instability of affect, mood, behavior, object relations, and self-concept (Bender, Morey, & Skodol, 2011). Patients with BPD are on the neurosis and psychosis border. These patients always seem to be in a critical state, and mood swing is a commonly observed symptom (Sadock, Kaplan, & Sadock, 2015). BPD is associated with comorbidity with other psychiatric disorders, thus leading to 10% suicide rate in people with BPD, which is quite high (Maj, 2010). BPD is the most common personality disorder diagnosed in clinical settings. Nearly, 15 to 50% of hospitalized patients and 11% of outpatient patients have been diagnosed with symptoms of BPD (American Psychiatric Association, 2000). Chronic and intense dysphoria, mood reactivity or affective lability, cognitive problems, recurrent suicidal attempts, behavior or gestures of self-mutilation, etc., are seen in patients suffering from BPD (Bender et al., 2011; Millon, Grossman, Millon, Meagher, & Ramnath, 2004). These signs and symptoms are emotion-based reactions. Researchers have increasingly come to view emotional impairments and dysregulations as the core features of BPD (Doering et al., 2013; Hutsebaut, Feenstra, & Kamphuis, 2016; Hutsebaut, Kamphuis, Feenstra, Weekers, & De Saeger, 2017; Jablensky, 2010).
The Emotional Dysregulation (ED) refers to emotional responses that are weakly modulated (Morey, 2017). These responses are often different from the usual and accepted ones. Some of the EDs in people with BPD include emotional disturbance, intense and suddenly occurred anger, aggressive behaviors, such as destroying objects, attacks on others and self-harm. Such reactions can lead to behavioral problems and affect the social interactions and individual’s relationships (Doering et al., 2013). Based on the theory of emotion regulation, if the individual with BPD who are healthy and adaptive can easily regulate his/her emotions or he/she can act healthy and adaptive (Morey, 2017; Skodol et al., 2011). Therefore, emphasis has been laid upon emotion regulation training as a treatment option for BPD, which presents clear implications in cognitive-behavior therapy used in treating BPD.
Despite the essential role of emotional disturbances in theoretical accounts of BPD (Bateman & Fonagy, 2010; Goldberg, 2010), most of the studies indicated a significant relationship between emotion regulation strategies and BPD symptoms (Lotfi, Amini, Fathi, Karami, & Ghiasi, 2014; Putnam & Silk, 2005). In addition, many studies have focused on two commonly used strategies for down-regulating emotions (Gratz, Rosenthal, Tull, Lejuez, & Gunderson, 2006; Gunderson et al., 2011) and few have examined cognitive emotion regulation strategies specifically. Moreover, although previous studies (Gratz et al., 2006; Kim, Sharp, & Carbone, 2014; Koenigsberg et al., 2010; Lotfi et al., 2014) have found that the features of BPD have a negative correlation with the adaptive strategies and a positive correlation with the maladaptive strategies of cognitive emotion regulation, and BPD is associated with low levels of acceptance and cognitive reappraisal, and high levels of rumination, catastrophizing suppression and avoidance, there is not a large amount of research about adaptive and maladaptive cognitive emotion regulation strategies in BPD. Also, most of the studies were done on non-clinical participants. So, the purpose of this study was to examine the cognitive emotion regulation strategies among prisoners with BPD and compare them with the normal population. In other words, the main aim of this study was to achieve the patterns of cognitive emotion regulation strategies between prisoners with BPD.
2. Methods
This study was a cross-sectional study. Ninety prisoners with BPD and 92 non-clinical individuals participated in this study. Given that the CERQ has 9 strategies and statistically at least 10 participants are required to investigate each of the strategies, the initial sample was 90. However, to increase the power of statistical analysis, 182 samples were selected using purposive and convenience sampling procedure for prisoners and non-clinical individuals, respectively. Non-clinical participants were selected from two university students in Tehran. Participants were paired based on their age and gender. All participants were male. Subjects aged 18 to 50 years, with guidance school degree of study and higher were selected. Inclusion criteria were guidance school and higher education and having symptoms of BPD (for prisoners). The exclusion criteria included having any history of head trauma, serious mental disorders, such as schizophrenia, bipolar disorder, etc., and showing no interesting to participate in the study.
Structured Clinical Interview for DSM-IV-II (SCID-II) and its versions are the one of the most comprehensive of the structured diagnostic interviews which is available (First, Gibbon, & Spitzer, 1997; Groth-Marnat, 2009). Due to the high accuracy of the diagnostic criteria and high clinical utility since the codification, translation and adaption to different languages, the SCID-II and SCID-PQ have been translated into Farsi and adapted with the Iranian culture (Mohammadkhani, Jokar, Jahani-tabesh, & Tamannaei-far, 2011). The test-retest reliability of the SCID-II and its internal consistency refers to intermediate results. For example, its test-retest consistency for diagnosis was between 0.40 and 0.86 with a mean of xxx (First, et al., 1997). Due to the fact that SCID has been made based on DSM, it seems to have good validity.
Cognitive Emotion Regulation Questionnaire (CERQ) (Garnefski & Kraaij, 2007) is a 36-item scale measuring the strategies of cognitive emotion regulation. These strategies essentially refer to how someone actually thinks about situations, when experiencing threatening or stressful life events. The questionnaire consists of 9 subscales, scored on a 5-point Likert scale (1: never to 5: always). The strategies that were evaluated by CERQ are as follows: Catastrophizing, putting into perspective, self-blame, other blame, rumination, positive reappraisal, positive refocusing, acceptance and planning. The CERQ has shown excellent reliability and validity (Garnefski & Kraaij, 2007). In Iranian sample, Yousefi reported good reliability score of 0.82. Cronbach’s alpha value ranged from 0.65 (acceptance) to 0.81 (self-blame).
In the data gathering process, three MSc. graduates in clinical psychology were trained in the SCID-II interview, who then interviewed the participants and asked them to complete the CERQ. In order to uphold the principles of research ethics at first, the purpose of the research and its process was explained, and the participants were allowed to leave the study whenever they want. The data were analyzed by independent t test and correlation coefficient via SPSS-16 software.
3. Results
Independent t test was used to compare the age difference between the prisoners and non-clinical groups. The results showed that there was not any significant difference in age (M=0.29, SD=0.37, P=0.71) between prisoners/BPD (M=1.33, SD=0.51) and non-clinical group (M=1.30, SD=0.53). Also, independent t-test was used to compare the means of variables (Table 1). Means and standard deviations showed that there was a significant differences between prisoners/BPD and non-clinical group in self-blame; t(180)=4.60, P=0.00, other blame; t(180)=8.35, P=0.00, rumination; t(180)=17.28, P=0.00, catastrophizing; t(180)=7.20, P=0.00, putting into perspective; t(180)=-4.80, P=0.00, positive refocusing; t(180)=5.19, P=0.00, positive reappraisal; t(180)=-6.80, P=0.00, acceptance; t(180)=-4.64, P=0.00, and planning; t(180)=-3.26, P=0.00.
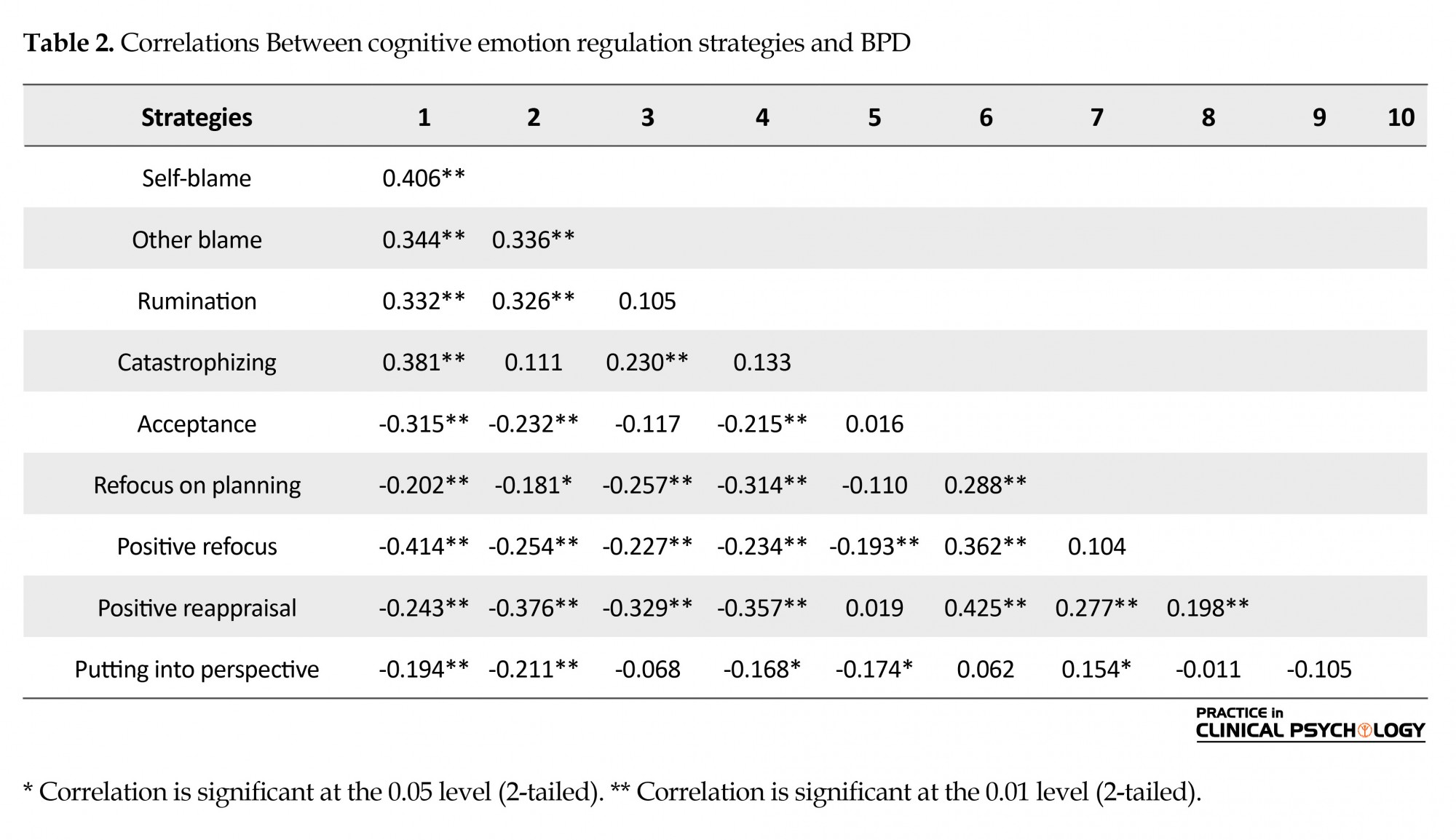
Table 2 displays the bivariate correlations between cognitive emotion regulation strategies and BPD. As expected, there was a robust association between BPD symptoms and emotion regulation strategies. The self-blame, catastrophizing, other blame and rumination strategies exhibited the largest associations with BPD (rs=0.40, 0.38, 0.34 and 0.33, respectively). Also, BPD was significantly and negatively associated with the positive strategies such as positive refocus, acceptance and positive reappraisal (rs=-0.41, -0.24, -0.31 respectively).
4. Discussion
The present study aimed at investigating the relationship between cognitive emotion regulation and BPD. In particular, the purpose of the study was to investigate whether cognitive-emotional regulation can provide additional information about the dimensions of emotional regulation in people with BPD and whether there are other dimensions of emotional regulation strategies, such as negative affect, depression and anxiety in these individuals.
The results showed that there was a significant difference between the two groups in negative and cognitive emotion regulation strategies. Results also suggested that cognitive emotional regulation present a robust and unique relationship with BPD symptoms.
Emotional dysregulation resulting from impulse control difficulties and limited access to emotion regulation strategies showed the strongest relationship to BPD, and the cognitive emotion regulation can be defined as a set of conscious strategies that a person uses to deal with emotionally arousing information. Although it has been shown that people with BPD have responses to stress such as rumination, catastrophizing and self-blame, generally associated with more emotional problems, but responses such as a positive reappraisal have been shown to be associated with fewer problems.
Findings supported that in addition to emotion regulation, cognitive emotion regulation strategies is an important feature of BPD. Moreover, results suggested that the assessment of cognitive emotion regulation strategies adds unique information to our knowledge of BPD psychopathology beyond that assessed by other measures of negative emotionality. As, showing self-blame, catastrophizing, other blame and rumination strategies exhibited the largest associations with BPD, and positive strategies such as positive refocus, acceptance and positive reappraisal have been shown to be fewer (or negative) related to BPD. These findings are in accordance with findings in general population samples, adolescents and patients with depression and anxiety (Hopwood et al., 2011; Hutsebaut et al., 2016; Katschnig, 2010; Morey, 2017; Skodol et al., 2011).
Overall, the present study helps to understand cognitive emotional regulation as an essential feature of BPD (Bateman & Fonagy, 2010). However, the study also had limitations, and future research is needed to overcome it. The main limitation of this study primarily relates to the nature of the sample, in which the sample was chosen from the population of prisoners, and all the participants were male with a relatively smaller sample size. Hence, further research is needed on a larger sample, including both male and female, and consisting of a clinical population. The other limitation was the use of self-report tools. It is advisable to use neuropsychological and neurophysiologic instruments to investigate the dimensions of emotion regulation in future studies. And finally, future research should identify which aspects of cognitive emotion are best predicted course and prognosis of BPD.
In general, the findings of this study showed that maladaptive cognitive emotion strategies for management of emotion, such as self-blame, catastrophizing, other-blame and rumination are of the most important strategies for people with BPD. Therefore, such strategies should be considered in the treatment module.
Ethical Considerations
Compliance with ethical guidelines
In the study all participants voluntarily entered, and gave their informed consent to participate.
Funding
The authors declare that this study was not supported by any financial source.
Conflict of interest
We declare that there is no conflict of interest.
References
The present study aimed at investigating the relationship between cognitive emotion regulation and BPD. In particular, the purpose of the study was to investigate whether cognitive-emotional regulation can provide additional information about the dimensions of emotional regulation in people with BPD and whether there are other dimensions of emotional regulation strategies, such as negative affect, depression and anxiety in these individuals.
The results showed that there was a significant difference between the two groups in negative and cognitive emotion regulation strategies. Results also suggested that cognitive emotional regulation present a robust and unique relationship with BPD symptoms.
Emotional dysregulation resulting from impulse control difficulties and limited access to emotion regulation strategies showed the strongest relationship to BPD, and the cognitive emotion regulation can be defined as a set of conscious strategies that a person uses to deal with emotionally arousing information. Although it has been shown that people with BPD have responses to stress such as rumination, catastrophizing and self-blame, generally associated with more emotional problems, but responses such as a positive reappraisal have been shown to be associated with fewer problems.
Findings supported that in addition to emotion regulation, cognitive emotion regulation strategies is an important feature of BPD. Moreover, results suggested that the assessment of cognitive emotion regulation strategies adds unique information to our knowledge of BPD psychopathology beyond that assessed by other measures of negative emotionality. As, showing self-blame, catastrophizing, other blame and rumination strategies exhibited the largest associations with BPD, and positive strategies such as positive refocus, acceptance and positive reappraisal have been shown to be fewer (or negative) related to BPD. These findings are in accordance with findings in general population samples, adolescents and patients with depression and anxiety (Hopwood et al., 2011; Hutsebaut et al., 2016; Katschnig, 2010; Morey, 2017; Skodol et al., 2011).
Overall, the present study helps to understand cognitive emotional regulation as an essential feature of BPD (Bateman & Fonagy, 2010). However, the study also had limitations, and future research is needed to overcome it. The main limitation of this study primarily relates to the nature of the sample, in which the sample was chosen from the population of prisoners, and all the participants were male with a relatively smaller sample size. Hence, further research is needed on a larger sample, including both male and female, and consisting of a clinical population. The other limitation was the use of self-report tools. It is advisable to use neuropsychological and neurophysiologic instruments to investigate the dimensions of emotion regulation in future studies. And finally, future research should identify which aspects of cognitive emotion are best predicted course and prognosis of BPD.
In general, the findings of this study showed that maladaptive cognitive emotion strategies for management of emotion, such as self-blame, catastrophizing, other-blame and rumination are of the most important strategies for people with BPD. Therefore, such strategies should be considered in the treatment module.
Ethical Considerations
Compliance with ethical guidelines
In the study all participants voluntarily entered, and gave their informed consent to participate.
Funding
The authors declare that this study was not supported by any financial source.
Conflict of interest
We declare that there is no conflict of interest.
References
- American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders, Text Revision. Washington, D.C.: American Psychiatric Association.
- Bateman, A., & Fonagy, P. (2010). Mentalization based treatment for borderline personality disorder. World Psychiatry, 9(1), 11-5. [DOI:10.1002/j.2051-5545.2010.tb00255.x]
- Bender, D. S., Morey, L. C., & Skodol, A. E. (2011). Toward a model for assessing level of personality functioning in DSM–5, part I: A review of theory and methods. Journal of Personality Assessment, 93(4), 332-46. [DOI:10.1080/00223891.2011.583808]
- Doering, S., Burgmer, M., Heuft, G., Menke, D., Baumer, B., Lubking, M., et al. (2013). Reliability and validity of the German version of the Structured Interview of Personality Organization (STIPO). BMC Psychiatry, 13, 210. [DOI:10.1186/1471-244X-13-210]
- First, M. B., Gibbon, M., & Spitzer, R. L. (1997). Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). Washington, D.C.: American Psychiatric Press.
- Garnefski, N., & Kraaij, V. (2007). The cognitive emotion regulation questionnaire. European Journal of Psychological Assessment, 23(3), 141-9. [DOI:10.1027/1015-5759.23.3.141]
- Goldberg, D. (2010). The detection and treatment of depression in the physically ill. World Psychiatry, 9(1), 16-20. [DOI:10.1002/j.2051-5545.2010.tb00256.x]
- Gratz, K. L., Rosenthal, M. Z., Tull, M. T., Lejuez, C. W., & Gunderson, J. G. (2006). An experimental investigation of emotion dysregulation in borderline personality disorder. Journal of Abnormal Psychology, 115(4), 850-855. [DOI:10.1037/0021-843X.115.4.850]
- Groth-Marnat, G. (2009). Handbook of psychological assessment. New York: John Wiley & sons. [PMID]
- Gunderson, J. G., Stout, R. L., McGlashan, T. H., Shea, M. T., Morey, L. C., Carlos M. G., et al. (2011). Ten-year course of borderline personality disorder: psychopathology and function from the collaborative longitudinal personality disorders study. Archives of General Psychiatry, 68(8), 827-37. [DOI:10.1001/archgenpsychiatry.2011.37]
- Hopwood, C. J., Malone, J. C., Ansell, E. B., Sanislow, C. A., Grilo, C. M., McGlashan, T. H., et al. (2011). Personality assessment in DSM-5: Empirical support for rating severity, Style, and Traits. Journal of Personality Disorders, 25(3), 305-20. [DOI:10.1521/pedi.2011.25.3.305]
- Hutsebaut, J., Feenstra, D. J., & Kamphuis, J. H. (2016). Development and preliminary psychometric evaluation of a brief self-report questionnaire for the assessment of the DSM-5 level of personality functioning scale: The LPFS brief form (LPFS-BF). Personality Disorders, 7(2), 192-7. [DOI:10.1037/per0000159]
- Hutsebaut, J., Kamphuis, J. H., Feenstra, D. J., Weekers, L. C., & De Saeger, H. (2017). Assessing DSM-5-oriented level of personality functioning: Development and psychometric evaluation of the Semi-Structured Interview for Personality Functioning DSM-5 (STiP-5.1). Personality Disorders, 8(1), 94-101. [DOI:10.1037/per0000197]
- Jablensky, A. (2010). Psychiatry in crisis? Back to fundamentals. World Psychiatry, 9(1), 29. [DOI:10.1002/j.2051-5545.2010.tb00258.x]
- Katschnig, H. (2010). Are psychiatrists an endangered species? Observations on internal and external challenges to the profession. World Psychiatry, 9(1), 21-8. [DOI:10.1002/j.2051-5545.2010.tb00257.x]
- Kim, S., Sharp, C., & Carbone, C. (2014). The protective role of attachment security for adolescent borderline personality disorder features via enhanced positive emotion regulation strategies. Personality Disorders, 5(2), 125-36. [DOI:10.1037/per0000038]
- Koenigsberg, H. W., Fan, J., Ochsner, K. N., Liu, X., Guise, K., Pizzarello, S., et al. (2010). Neural correlates of using distancing to regulate emotional responses to social situations. Neuropsychologia, 48(6), 1813-22. [DOI:10.1016/j.neuropsychologia.2010.03.002]
- Lotfi, M., Amini, M., Fathi, A., Karami, A., & Ghiasi, S. (2014). Personality traits, emotion regulation and impulsive behaviors in patients with borderline personality disorder. Practice in Clinical Psychology, 2(1), 27-33.
- Maj, M. (2010). Are psychiatrists an endangered species? World Psychiatry, 9(1), 1-2. [DOI:10.1002/j.2051-5545.2010.tb00253.x]
- Millon, T., Grossman, S., Millon, C., Meagher, S., & Ramnath, R. (2004). Personality disorders in modern life (Vol. 1). Hoboken, New Jersey: John Wiley & Sons, Inc.
- Mohammadkhani, P., Jokar, M., Jahani-tabesh, O., & Tamannaei-far, S. (2011). Structured clinical interview for DSM-IV axis II personality disorders (Persian Version). Tehran: Danjeh. [PMCID]
- Morey, L. C. (2017). Application of the DSM-5 Level of Personality Functioning Scale by Lay Raters. Journal of Personality Disorders, 1-12. [DOI:10.1521/pedi_2017_31_305]
- Morey, Leslie. (2017). Development and initial evaluation of a self-report form of the DSM-5 level of personality functioning scale. Psychological Assessment, 29(10), 1302-8. [DOI:10.1037/pas0000450]
- Putnam, K. M., & Silk, K. R. (2005). Emotion dysregulation and the development of borderline personality disorder. Development and Psychopathology, 17(4), 899-925. [DOI:10.1017/S0954579405050431] [PMID]
- Sadock, B. J., Kaplan, H. I., & Sadock, V. A. (2015). Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/clinical Psychiatry. Philadelphia, Pennsylvania: Lippincott Williams & Wilkins.
- Skodol, A. E., Clark, L. A., Bender, D. S., Krueger, R. F., Morey, L. C., Verheul, R., et al. (2011). Proposed changes in personality and personality disorder assessment and diagnosis for DSM-5 Part I: Description and rationale. Personality Disorders, 2(1), 4-22. [DOI:10.1037/a0021891]
Type of Study: Research |
Subject:
Cognitive behavioral
Received: 2017/12/7 | Accepted: 2018/05/12 | Published: 2018/07/1
Received: 2017/12/7 | Accepted: 2018/05/12 | Published: 2018/07/1
References
1. American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders, Text Revision. Washington, D.C.: American Psychiatric Association.
2. Bateman, A., & Fonagy, P. (2010). Mentalization based treatment for borderline personality disorder. World Psychiatry, 9(1), 11-5. [DOI:10.1002/j.2051-5545.2010.tb00255.x] [DOI:10.1002/j.2051-5545.2010.tb00255.x]
3. Bender, D. S., Morey, L. C., & Skodol, A. E. (2011). Toward a model for assessing level of personality functioning in DSM–5, part I: A review of theory and methods. Journal of Personality Assessment, 93(4), 332-46. [DOI:10.1080/00223891.2011.583808] [DOI:10.1080/00223891.2011.583808]
4. Doering, S., Burgmer, M., Heuft, G., Menke, D., Baumer, B., Lubking, M., et al. (2013). Reliability and validity of the German version of the Structured Interview of Personality Organization (STIPO). BMC Psychiatry, 13, 210. [DOI:10.1186/1471-244X-13-210] [DOI:10.1186/1471-244X-13-210]
5. First, M. B., Gibbon, M., & Spitzer, R. L. (1997). Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). Washington, D.C.: American Psychiatric Press.
6. Garnefski, N., & Kraaij, V. (2007). The cognitive emotion regulation questionnaire. European Journal of Psychological Assessment, 23(3), 141-9. [DOI:10.1027/1015-5759.23.3.141] [DOI:10.1027/1015-5759.23.3.141]
7. Goldberg, D. (2010). The detection and treatment of depression in the physically ill. World Psychiatry, 9(1), 16-20. [DOI:10.1002/j.2051-5545.2010.tb00256.x] [DOI:10.1002/j.2051-5545.2010.tb00256.x]
8. Gratz, K. L., Rosenthal, M. Z., Tull, M. T., Lejuez, C. W., & Gunderson, J. G. (2006). An experimental investigation of emotion dysregulation in borderline personality disorder. Journal of Abnormal Psychology, 115(4), 850-855. [DOI:10.1037/0021-843X.115.4.850] [DOI:10.1037/0021-843X.115.4.850]
9. Groth-Marnat, G. (2009). Handbook of psychological assessment. New York: John Wiley & sons. [PMID] [PMID]
10. Gunderson, J. G., Stout, R. L., McGlashan, T. H., Shea, M. T., Morey, L. C., Carlos M. G., et al. (2011). Ten-year course of borderline personality disorder: psychopathology and function from the collaborative longitudinal personality disorders study. Archives of General Psychiatry, 68(8), 827-37. [DOI:10.1001/archgenpsychiatry.2011.37] [DOI:10.1001/archgenpsychiatry.2011.37]
11. Hopwood, C. J., Malone, J. C., Ansell, E. B., Sanislow, C. A., Grilo, C. M., McGlashan, T. H., et al. (2011). Personality assessment in DSM-5: Empirical support for rating severity, Style, and Traits. Journal of Personality Disorders, 25(3), 305-20. [DOI:10.1521/pedi.2011.25.3.305] [DOI:10.1521/pedi.2011.25.3.305]
12. Hutsebaut, J., Feenstra, D. J., & Kamphuis, J. H. (2016). Development and preliminary psychometric evaluation of a brief self-report questionnaire for the assessment of the DSM-5 level of personality functioning scale: The LPFS brief form (LPFS-BF). Personality Disorders, 7(2), 192-7. [DOI:10.1037/per0000159] [DOI:10.1037/per0000159]
13. Hutsebaut, J., Kamphuis, J. H., Feenstra, D. J., Weekers, L. C., & De Saeger, H. (2017). Assessing DSM-5-oriented level of personality functioning: Development and psychometric evaluation of the Semi-Structured Interview for Personality Functioning DSM-5 (STiP-5.1). Personality Disorders, 8(1), 94-101. [DOI:10.1037/per0000197] [DOI:10.1037/per0000197]
14. Jablensky, A. (2010). Psychiatry in crisis? Back to fundamentals. World Psychiatry, 9(1), 29. [DOI:10.1002/j.2051-5545.2010.tb00258.x] [DOI:10.1002/j.2051-5545.2010.tb00258.x]
15. Katschnig, H. (2010). Are psychiatrists an endangered species? Observations on internal and external challenges to the profession. World Psychiatry, 9(1), 21-8. [DOI:10.1002/j.2051-5545.2010.tb00257.x] [DOI:10.1002/j.2051-5545.2010.tb00257.x]
16. Kim, S., Sharp, C., & Carbone, C. (2014). The protective role of attachment security for adolescent borderline personality disorder features via enhanced positive emotion regulation strategies. Personality Disorders, 5(2), 125-36. [DOI:10.1037/per0000038] [DOI:10.1037/per0000038]
17. Koenigsberg, H. W., Fan, J., Ochsner, K. N., Liu, X., Guise, K., Pizzarello, S., et al. (2010). Neural correlates of using distancing to regulate emotional responses to social situations. Neuropsychologia, 48(6), 1813-22. [DOI:10.1016/j.neuropsychologia.2010.03.002] [DOI:10.1016/j.neuropsychologia.2010.03.002]
18. Lotfi, M., Amini, M., Fathi, A., Karami, A., & Ghiasi, S. (2014). Personality traits, emotion regulation and impulsive behaviors in patients with borderline personality disorder. Practice in Clinical Psychology, 2(1), 27-33.
19. Maj, M. (2010). Are psychiatrists an endangered species? World Psychiatry, 9(1), 1-2. [DOI:10.1002/j.2051-5545.2010.tb00253.x] [DOI:10.1002/j.2051-5545.2010.tb00253.x]
20. Millon, T., Grossman, S., Millon, C., Meagher, S., & Ramnath, R. (2004). Personality disorders in modern life (Vol. 1). Hoboken, New Jersey: John Wiley & Sons, Inc.
21. Mohammadkhani, P., Jokar, M., Jahani-tabesh, O., & Tamannaei-far, S. (2011). Structured clinical interview for DSM-IV axis II personality disorders (Persian Version). Tehran: Danjeh. [PMCID] [PMCID]
22. Morey, L. C. (2017). Application of the DSM-5 Level of Personality Functioning Scale by Lay Raters. Journal of Personality Disorders, 1-12. [DOI:10.1521/pedi_2017_31_305] [DOI:10.1521/pedi_2017_31_305]
23. Morey, Leslie. (2017). Development and initial evaluation of a self-report form of the DSM-5 level of personality functioning scale. Psychological Assessment, 29(10), 1302-8. [DOI:10.1037/pas0000450] [DOI:10.1037/pas0000450]
24. Putnam, K. M., & Silk, K. R. (2005). Emotion dysregulation and the development of borderline personality disorder. Development and Psychopathology, 17(4), 899-925. [DOI:10.1017/S0954579405050431] [PMID] [DOI:10.1017/S0954579405050431]
25. Sadock, B. J., Kaplan, H. I., & Sadock, V. A. (2015). Kaplan & Sadock's Synopsis of Psychiatry: Behavioral Sciences/clinical Psychiatry. Philadelphia, Pennsylvania: Lippincott Williams & Wilkins.
26. Skodol, A. E., Clark, L. A., Bender, D. S., Krueger, R. F., Morey, L. C., Verheul, R., et al. (2011). Proposed changes in personality and personality disorder assessment and diagnosis for DSM-5 Part I: Description and rationale. Personality Disorders, 2(1), 4-22. [DOI:10.1037/a0021891] [DOI:10.1037/a0021891]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |