Volume 6, Issue 2 (Spring 2018- 2018)
PCP 2018, 6(2): 83-92 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Moosavian E, Nejati S F. Association Between Facial Affect Recognition and Maladaptive Schema in People With Depressive Symptoms. PCP 2018; 6 (2) :83-92
URL: http://jpcp.uswr.ac.ir/article-1-473-en.html
URL: http://jpcp.uswr.ac.ir/article-1-473-en.html
1- Department of Clinical Psychology, School of Education and Psychology, Shiraz University, Shiraz, Iran. , elham_moosavian@yahoo.com
2- Department of Clinical Psychology, School of Education and Psychology, Shiraz University, Shiraz, Iran.
2- Department of Clinical Psychology, School of Education and Psychology, Shiraz University, Shiraz, Iran.
Full-Text [PDF 647 kb]
(2051 Downloads)
| Abstract (HTML) (4341 Views)
The model was also used to examine the effects of the EMSs and depression on the recognition of individual emotions. Because the recognition of each emotion was reflected by the number of positive responses to six binary questions, the model was used separately for each emotion. In this modeling, emotion recognition was the dependent variable, and the EMSs and depression variable were entered as the independent variables.
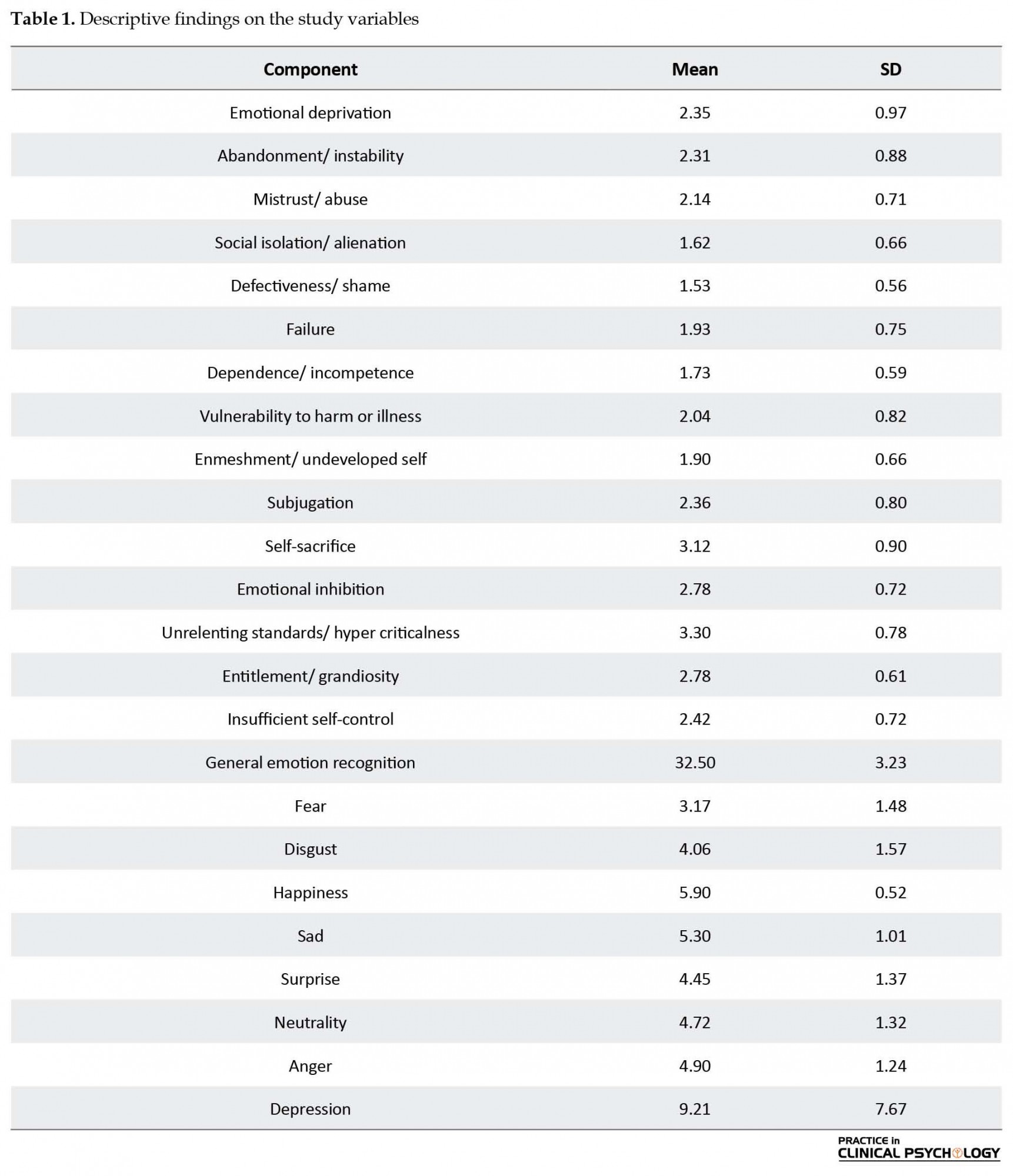
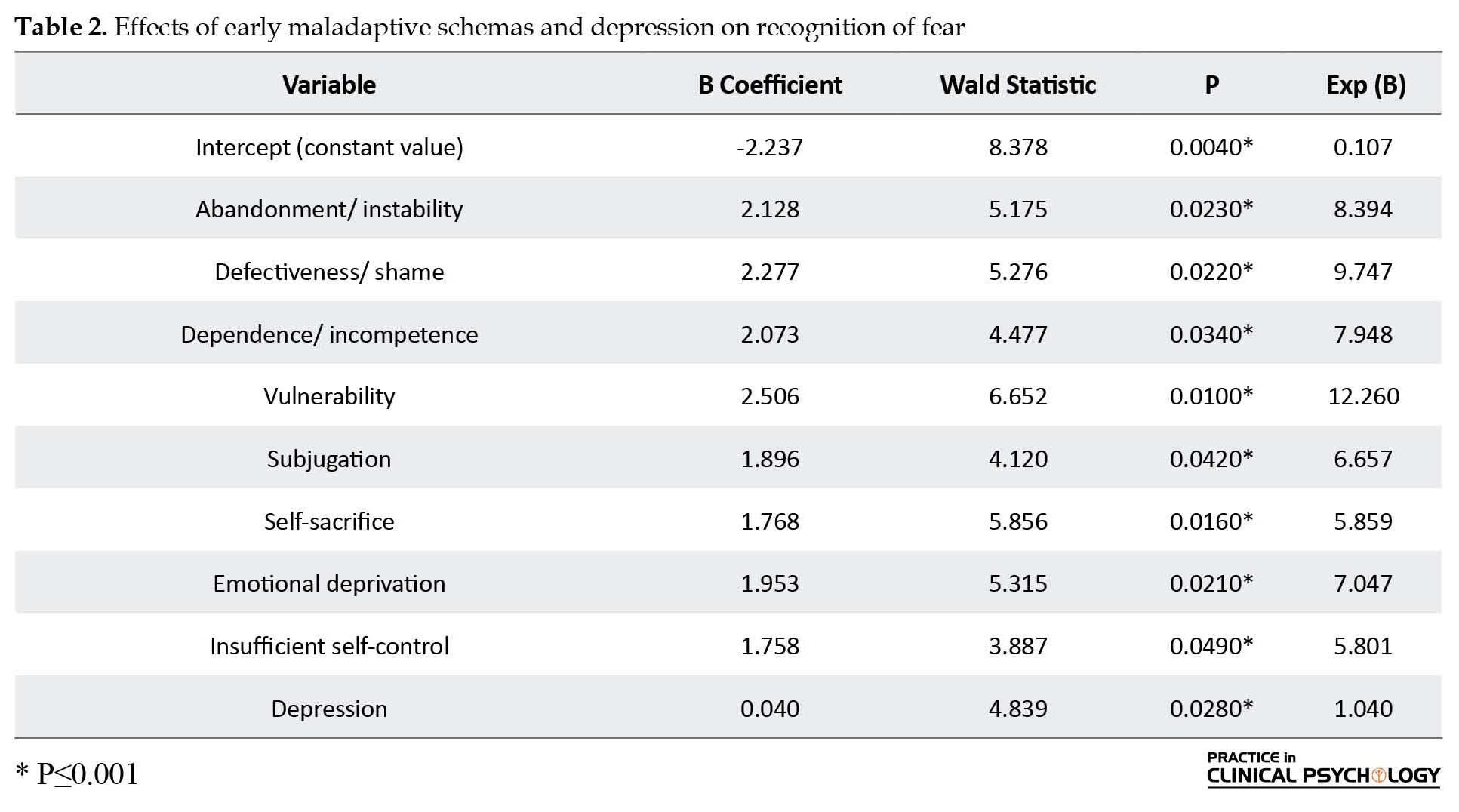
The effects of the EMSs and depression on the recognition of fear were examined. Table 2 lists the variables of the model, along with the regression coefficients, Wald statistics, P values, and Exp (B). Abandonment/ instability, defectiveness/ shame, dependence/ incompetence, vulnerability to harm or illness, subjugation, self-sacrifice, emotional inhibition, insufficient self-control, and depression exerted significant effects (P<0.05) on the recognition of fear, whereas the other EMSs had no statistically significant effects (P≥0.05). The regression coefficient of abandonment/ instability was 2.128, indicating that with a unit increase in the score of abandonment/ instability, the logit value of fear recognition would increase by 2.128 units. This regression coefficient can be interpreted more tangibly on the basis of the Exp (B) column, which indicated that with an increase in the score of abandonment/ instability, the recognition of fear would increase by e2.128 or 8.394 times. The other significant binomial regression coefficients can be interpreted in a similar manner.
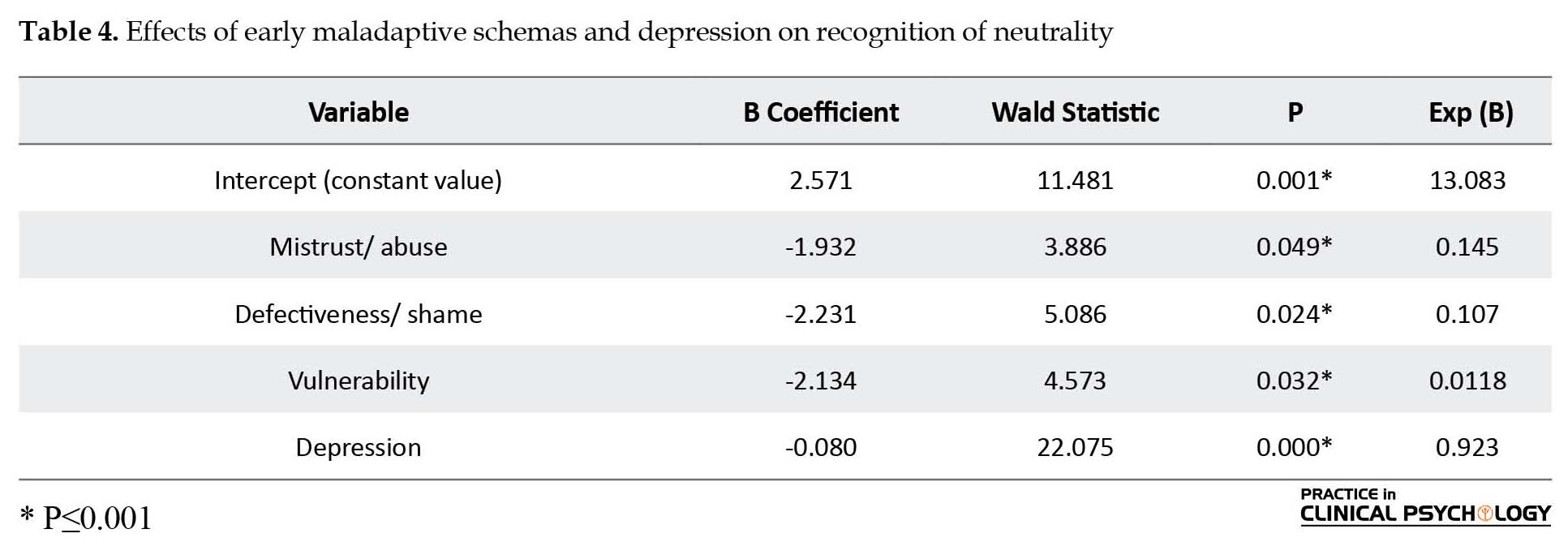
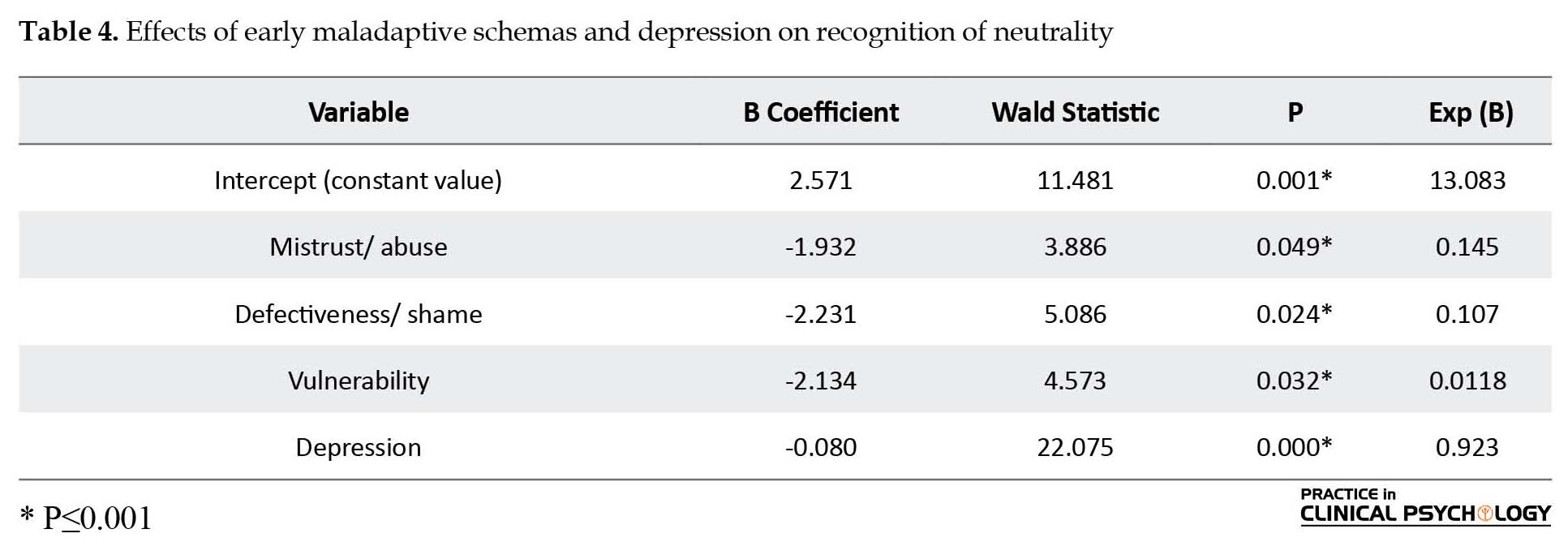
Depression exerted a significant effect (P<0.05) on the recognition of sadness, whereas the EMSs had no significant effects (P≥0.05) on the recognition of this emotion and surprise. As shown in Table 3, the regression coefficient of depression is 0.105, indicating that a one-unit increase in the depression score will increase the logit value of sadness recognition by 0.105 units. This regression coefficient can be interpreted on the basis of the Exp (B) column, which indicates that with an increase in the depression score, the recognition of sadness would increase by e0.105 or 1.111 times. The regression coefficient of a variable, such as abandonment/ instability, was greater than that of depression, but because of the large standard error of the coefficient of this schema, its Wald statistic was xxx, and its P-value exceeded 0.05. Thus, abandonment/ instability and the other EMSs exerted non-significant effects on the recognition of sadness. Table 4 shows that mistrust, defectiveness/ shame, vulnerability to illness and depression exerted significant effects (P<0.05) on the recognition of the neutral state, whereas the other variables had no significant effects (P≥0.05). The regression coefficient of vulnerability to illness is –2.134, as presented in Table 4. This result indicates that with a unit increase in the score of vulnerability to illness, and the logit value of the recognition of the neutral state decreased by 2.134 units. On the basis of the Exp (B) column, with an increase in the score of vulnerability to illness, the recognition of the neutral state would increase by e–2.134 or 0.118 times. This finding suggested a negative effect on an individual’s recognition of the neutral state. The other significant binomial regression coefficients can also be interpreted in a similar manner.
Finally, only depression exerted a significant effect (P<0.05) on the recognition of anger; the other variables exerted little effect (P≥0.05) (Table 5). The regression coefficient of depression was 0.067, indicating that with a unit increase in the depression score, the logit value of anger recognition will increase by 0.067 units. On the basis of the Exp (B) column, an increase in the depression scores would increase the recognition of anger by e0.067 or 1.07 times. The regression coefficient of a variable, such as abandonment/ instability, was larger than that of depression, but because of the considerable standard error in the coefficient of the aforementioned schema, its Wald statistic was small and its P value exceeded 0.05. Thus, the effects of this schema and the other EMSs were non-significant. None of the variables exerted a statistically significant effect (P≥0.05) on the recognition of happiness, surprise, and disgust.
4. Discussion
We investigated the relationship of EMSs and depressive symptoms with the recognition of general emotions and facial affects that reflect anger, fear, disgust, happiness, sadness, surprise, and neutrality. The results indicated that the recognition of fear was significantly amplified by abandonment/ instability, defectiveness/ shame, dependence/ incompetence, vulnerability to illness, subjugation, self-sacrifice, emotional deprivation, insufficient self-control, and depression. In contrast, none of the other EMSs exerted a significant effect on fear recognition. Calder, Lawrence, and Young (2001) emphasized on the role of amygdala in the processing of fear-relevant cues, including corresponding facial expressions. Studies appear to agree on the relationship between the enhanced recognition of fear in individuals with a previous history of depression and the suggested role of amygdala in the disorder. Sheline et al. (2001) stated that acutely depressed patients exposed to facial expressions of fear exhibited high activation of the left amygdala. He also reported that antidepressants normalized abnormal amygdala activation in the patients showing remission.
We found that the recognition of neutral state was significantly impaired by mistrust, defectiveness/ shame, vulnerability to illness, and depression. The rest of the EMSs exerted no such effects. Drevets (2001) argued that the elevated physiological activity of the amygdala can explain the tendency of depressed people to misinterpret the emotional meanings attached to emotionally neutral social cues (neutral facial expressions). The processing of emotionally positive signals by depressed individuals can also be impaired by dysfunction in reward systems (Sloan, Strauss, Quirk, & Sajatovic, 1997). Considering the association of depression with elevated amygdala activity, alongside evidence suggesting the inability of depressed people to modulate their emotional responses (Drevets, 2001) and their inclination to misinterpret neutral expressions as sad expressions (Gur et al., 1992), one can argue that people with depression may have an impaired ability to recognize neutral facial expressions as such.
We found that the ability of the current study’s participants to recognize sadness and anger was significantly amplified by depression. Research has suggested that major depression is associated with selective attention bias in favor of negative emotional stimuli, such as sadness, loss, and failure, and negative cognitions, such as worthlessness, hopelessness, and self-criticism; such bias results in the perception of external stimuli, such as facial expressions, as more negative than normal (Schaefer, Baumann, Rich, Luckenbaugh, & Zarate, 2010).
Our results showed that depression enhanced the recognition of anger. Anger is closely associated with depression in entire populations (Rimes & Watkins, 2005) because it can be simply directed toward the self and cause anxiety (Newman et al., 2006). To illuminate this issue further, Wright et al. (2009) elucidated that when depressed women were asked to classify facial emotional expressions, they often misunderstood the expression of fear and sadness as anger. Jollant et al. (2008) reported that depressed men who have had attempted suicide were more sensitive to angry faces than those who have not attempted suicide. Douglas and Porter (2010) stated that in people with severe depression, the ability to differentiate anger in facial expressions becomes impaired, but Douglas, Porter, Knight, & Maruff (2011) suggested that medication can normalize a patient’s ability to correctly identify anger in facial expressions. So anger could be turned into anger rumination and later to depression. When feeling angry, a person who is in a depressed mood relates anger to previous experiences—a behavior that invokes negative thoughts and then develops into anger rumination, sometimes including a desire to feel antipathy toward others and fantasize about revenge. The likelihood of people to engage in stable rumination may be associated with their belief that rumination is useful and presents some advantages (Papageorgiou & Wells, 2004). People regard active rumination as an uncontrollable and harmful habit with undesirable social consequences, and this negative belief can contribute to depression. Thus, depression experience continues in a cycle of rumination, depression, and specific metacognitive beliefs.
In the current work, no statistically significant association was found between the EMSs or depression and the recognition of disgust, surprise, happiness, or general emotions. In contrary to the expectations, normal people did not outperform patients with major depression in recognizing facially expressed emotions. In view of this result, depression cannot be regarded as consistent with the effects of the experimental induction of negative emotions (e.g. sadness). Additionally, our findings refuted the hypothesis on negative mood induction and impaired emotion recognition from positive facial expressions (e.g. happiness) as being necessary stimuli of depression (Milder, Bell, Platt, Serrano, and Runcie, 2010). Disgust refers to the internal urge to avoid an unpleasant, infected, or spoiled object. Almost all cultures share a set of similar facial expressions for certain emotions. In the case of disgust, this emotion is expressed by gaping, wrinkling of the nose, and jutting of the upper lip (Ekman & Friesen, 1976). Thus, the familiarity of this emotion can cause lack of significant differences in recognition by different individuals (Schaefer et al., 2010).
The effects to be expected from impaired emotion recognition include the inability to receive affective support from intimate relationships and the lack of control over social situations. The maladaptive schemas that underlie depression may both contribute to and be reinforced by these effects. Determining the true causal relationship between emotion recognition and maladaptive schemas and their link to depression requires further research, with healthy and euthymic people as controls. Strong evidence supports the correlation between impairments in facial affect recognition and social behavior (Addington, Saeedi, & Addington, 2006) because, in short, a prerequisite to successful social functioning is the ability to properly understand people’s facial expressions (Venn et al., 2004).
The generalizability of our results is limited by this factor that in the natural environment, facial expressions are not static like photographs, but it represents ever-changing events. Some investigators suggested that due to the lack of important dynamic information in the facial photographs, patients need to interpret facial expressions more accurately. It suggested that future studies that make use of videotaped representations of facial expressions of emotions could address this issue (Hargarave, Maddock & Stone, 2002).
The results of our study indicated that in unmedicated subjects with depressive symptoms, social functioning difficulties, maladaptive schemas, and depressive symptoms are reinforced by certain impairments in emotion recognition. Thus, major depression can be characterized, to some extent, by dysfunctional emotion recognition. In people with major depression, dysfunctional schemas and counterproductive attitudes prevent the appropriate processing of life events (Scher, Ingram, & Segal, 2005).
Acknowledgments
This article had no financial sponsors.
Conflict of Interest
The authors declared no conflicts of interest.
References
Full-Text: (1833 Views)
1. Introduction
An approach that can serve as a suitable systematic framework to explore the association between depression with Early Maladaptive Schemas (EMSs) and emotion recognition from facial expressions is the use of interpersonal models that can explain the development and persistence of depression (Gilbert, 2005). The development of the affective self during the early stages of growth is heavily influenced by attachment mechanisms and facial-affective responses of parents to child behaviors. This influence holds particularly for affective schema that determine how we view ourselves in relation to others (self-to-other schema) and how others view themselves in relation to us (other-to-self schema) (Gergely & Unoka, 2008). Studies suggested that the negative facial expressions exhibited by a social acquaintance can increase the accessibility of interpersonally developed negative self-schemas (Baldwin & Dandeneau, 2004). A person’s misperception of interactions as a result of maladaptive interpersonal affective schemas may develop into etiological depression factors, including social losses (Kendler, Hettema, Butera, Gardner, & Prescott, 2003); inaptitude to take advantage of social support (Brown, Andrews, Harris, Adler, & Bridge, 1986); a tendency toward subservience, as maintained by the social rank theory of depression (Gilbert, 2005); perceived loss of autonomy; and loss of identity (Ehlers, Maercker, & Boos, 2000). Compared to their healthier counterparts, depressed people are less likely to recognize emotions displayed in pictures (Surguladze et al., 2005). They also suffer from a diminished ability to recognize positive emotions and tend to negatively misinterpret facial expressions (Leppanen, Milders, Bell, Terriere, & Hietanen, 2004). Some studies demonstrated that depressed individuals exhibit mood-congruent bias toward facial expression recognition (Newman, Fuqua, Gray, & Simpson 2006), while others found that people suffering from anxiety exhibit such bias in their perception (Bouhuys, Geerts, & Mersch, 1997). Psychological distress significantly contributes to the inability to process emotions and the inclination to interpret neutral facial expressions with a negative bias (Csukly, Czobor, Szily, Takács, & Simon, 2009). Depression impairs the neural processing of happy facial expressions in the core regions of affective facial processing, but this problem can be resolved through treatment (Fu et al., 2007).
As suggested by the findings discussed above, the misperception of facially expressed emotions is correlated with depression and psychiatric distress. The development of negative misperceptions regarding other people’s attitudes and expressions among individuals with depression is driven by negative schemas, as maintained by the cognitive theory of depression (Beck, 1964; Young & Brown, 1990). Schemas are cognitive structures and frameworks, in which a person organizes and processes stimuli and information. EMSs are dysfunctional cognitive patterns that develop during childhood through emotions, memories, and experiences with regard to one’s relationship with others. These schemas may govern a person’s future attitude and perception of others, compel a prejudicial misinterpretation of normal experiences for a dysfunctional favoring of separation or social rejection, and induce misperceptions about other people’s emotions (Lemche, Klann-Delius, Koch, & Joraschky, 2004). Although initially emerging during childhood, EMSs develop through adolescence and become elaborated during one’s lifetime (Young, Klosko, & Weishaar, 2003). Young and Brown (1990) identified 19 EMSs, including beliefs concerning attachment to others, the ability to express valid needs and emotions, autonomy, competence, sense of identity, limit-setting capacity, and self-control. Some researchers suggested that EMSs are strongly associated with personality disorders, mild characterological problems, and axis I disorders, such as depression (Young et al., 2003). On the other hand, scholars also provided more definitive evidence regarding the contribution of EMSs to the development and continuation of depression (Riso et al., 2003). Harris and Curtin (2002), Hoffart et al. (2005), and Schmidt, Joiner, Young, and Telch (1995) used the Young Schema Questionnaire (YSQ) in their cross-sectional studies and found that EMSs can serve as predictors for depression severity. A two-phase study by Riso et al. (2006) revealed moderate to high levels of relative EMS stability (measured with test-retest correlations) in depressed outpatients after the researchers controlled depression severity. They also reported that despite the relative alleviation of the depression levels, the mean score of EMSs remained largely unchanged, even after the exclusion of patients who were not in remission. Halvorsen, Wang, Eisemann, and Waterloo (2009) confirmed that YSQ scales are significant predictors of major depression episodes over a duration as long as 9 years. EMSs can, therefore, serve as factors of vulnerability to depression, both cross-sectionally and longitudinally.
The aforementioned studies implied that the severity of psychopathologic symptoms is negatively correlated with patients’ ability to recognize emotions, especially positive ones. Thus, the maladaptive schemas that underlie misconceptions regarding social reality and impairments in facial expression recognition are both likely to be strongly present in depressed patients. Despite the considerable insights provided by previous studies on maladaptive schemas, however, only Csukly et al. (2011) have investigated the association of these cognitive and emotional patterns with impairments in emotion recognition. Furthermore, the findings of the authors may have been influenced by the fact that the recruited patients received antidepressant medication; antidepressants may help patients develop a positive bias or interpret negative facial expressions as reflective of neutral emotions (Norbury, Mackay, Cowen, Goodwin, & Harmer, 2007). Given the possibility of confounding effects from medication in such studies, we reinvestigated the association between emotion recognition and EMSs in people who showed symptoms of depression but have not been administered with any antidepressant medication. Thus, the objective of the present study was to either confirm or refute the relationship among the aforementioned conditions.
2. Methods
Through purposive sampling, this study selected 18 to 32-year-old male and female students of Shiraz University who were enrolled in BA/S and MA/S programs in the first half of the academic year, 2015 to 2016. The final sample comprised of 100 undergraduate and graduate students (M=22.8, SD=5.72), of which 42 were women (M=24.60, SD=3.44) and 58 were men (M=23.24, SD=3.40). The participants were interviewed by an experienced psychologist, who used a structured clinical interview instrument from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5, 2013). Exclusion criteria included diagnosis of axis 1 disorder, except for depression (determined based on the diagnostic criteria in DSM-5), and a history of drug addiction, physical illness, and neurological disorders, such as epilepsy, any type of brain injury, and mental illness. All examinations involving the human participants were approved by an appropriate ethics committee.
After the subjects signed the consent form, they were interviewed by the experienced psychologist. They were then administered with the test package, which contained forms for filling in basic demographic information, the BDI, the YSQ, the facial affect recognition test, and the corresponding answer sheets.
Schema Questionnaire-Short Form (SQ-SF) is a 75-item questionnaire and was developed by Young (1994) for the evaluation of 15 EMSs. The schemas include the following: Emotional deprivation, Abandonment/ Instability, Mistrust/ Abuse, Social isolation/ Alienation, Defectiveness/ Shame, Failure, Dependence /Incompetence, Vulnerability to harm or illness, Enmeshment/ Undeveloped self, Subjugation, Self-sacrifice, Emotional inhibition, Unrelenting standards/ Hyper criticalness, Entitlement/ Grandiosity, and Insufficient self-control.
Five questions are devoted to each schema, and each question is scored on a 6-point scale (1= Totally false, 6= Quite right”). If the subscale average of a given schema is above 2.5, then the schema is evaluated as inefficient. The reliability and validity of the SQ-SF have been demonstrated in several studies (Oei & Baranoff, 2007), and its validation for the Iranian context was conducted in Tehran universities by Ahi, Mohammadifar, & Besharat (2007). In the current research, the internal consistency of the instrument was 0.97 for the female respondents and 0.98 for the male respondents, as calculated by Cronbach’s alpha. The alpha value of the overall questionnaire was 0.96, and those of the schemas were as follows: Emotional deprivation (0.86), Abandonment /Instability (0.70), Mistrust /Abuse (0.81), Social isolation /Alienation (0.79), Defectiveness /Shame (0.89), Failure (0.89), Dependence /Incompetence (0.84), Vulnerability to illness (0.84), Enmeshment /Undeveloped self (0.77), Subjugation (0.82), Self-sacrifice (0.82), Emotional inhibition (0.78), Unrelenting standards /Hyper criticalness (0.69), Entitlement /Grandiosity (0.78), and Insufficient self-control (0.71).
Beck Depression Inventory (BDI) consists of 21 questions that measure the degree of depression on a 4-point Likert scale. Beck, Street and Garbin (1988) obtained a test-retest reliability coefficient of 0.93 for the instrument over a week’s duration. Goudarzi (2002) also derived appropriate reliability and validity for the Iranian context. The author obtained a reliability of 0.84 on the basis of Cronbach’s alpha calculation for internal consistency and a correlation coefficient of 0.70 on the basis of the split-half method based on odd and couple questions.
By Facial Affect Recognition Task, the participants were tested on their ability to recognize facially expressed emotions from 41 images that measure six emotional states (sadness, happiness, fear, anger, disgust, and surprise) and the neutral state. To adapt this test to the Persian culture, 110 images of facially expressed emotions were first obtained from Ekman and Friesen (1976). The images display the faces of differently aged males and females expressing happiness, sadness, anger, fear, disgust, surprise, and neutral emotions. The images were screened by a 41-person group composed of 19 to 22-year-old clinical psychology students from Shiraz University. With respect to the final 41 images (six images for each emotion, except for fear to which five images were allocated, and six images for the neutral state), more than 85% of the initial screening participants agreed that the emotions related to the images accurately stimulate recognition. There were seven images (six related to emotional states and one to the neutral state) on which subjects had 100% agreement that was considered as the main options (related to the six emotional states and one to the neutral state). On the basis of the screening results, a multiple-choice test with the 41 images was designed. The images of main options, which were laid out on seven 20×30 cm cards, were placed in constant view (front) of the subjects, whereas the other images were displayed consecutively on a handheld computer positioned in front of the subjects. The computer was a 16-inch device with 800×1280 pixel resolution. The presentation of the images was randomly sequenced, but the same number of images was shown to the subjects. After carefully explaining the task procedure to the subjects, they were asked to sit on a comfortable chair and hold the computer at a distance of 40±5 cm. One of the seven images, including the corresponding test options, were shown to a subject, after which one of the other 41 images was displayed on the monitor for 500 ms. After each image was presented, the subjects were given 5 s (Pan et al., 2009) to identify the emotion expressed in the image or identify the picture that showed a similar emotion as that displayed in the target image. The performance of the subjects was measured on the basis of the total number of correct answers.
This research is of cross-sectional design, and the normal distribution of the variables was evaluated using the Shapiro–Wilk test. The P values of all the variables, including the components of emotion recognition from facial expression were significant (P<0.001). These variables were therefore non-normally distributed. Given that the dependent variable (emotion recognition from facial expression) was non-normally distributed and had no distance scale, a linear regression model could not be used. Instead, a binomial distribution was evident given that the variable pertained to the number of positive responses (“yes”) to two binary questions (yes/no questions) regarding emotion recognition from facial expression. Correspondingly, a binomial regression model could be employed.
3. Results
The descriptive findings (means and standard deviations) obtained from the 100 participants are shown in Table 1. Binomial regression is a generalized linear model, wherein a response variable can be obtained from a series of Bernoulli trials or binaries; the implications of these experiments are one of success (Code 1) or failure (Code 0) expressions. A binomial regression model with a logit link function was used to investigate the effects of the EMSs and depression on the recognition of general and individual emotions. The examination was first directed toward the effects of the EMSs and depression on general emotion recognition. Considering that the variable for general emotion recognition was the number of positive responses (“yes”) to 41 binary questions (yes/no questions), the binomial regression model with the logit link function was used. In this modeling, general emotion recognition was adopted as the dependent variable, and the EMSs and depression were incorporated as the independent variables. The results showed that none of the variables exerted a statistically significant effect (P≥0.05) on general emotion recognition from faces.
An approach that can serve as a suitable systematic framework to explore the association between depression with Early Maladaptive Schemas (EMSs) and emotion recognition from facial expressions is the use of interpersonal models that can explain the development and persistence of depression (Gilbert, 2005). The development of the affective self during the early stages of growth is heavily influenced by attachment mechanisms and facial-affective responses of parents to child behaviors. This influence holds particularly for affective schema that determine how we view ourselves in relation to others (self-to-other schema) and how others view themselves in relation to us (other-to-self schema) (Gergely & Unoka, 2008). Studies suggested that the negative facial expressions exhibited by a social acquaintance can increase the accessibility of interpersonally developed negative self-schemas (Baldwin & Dandeneau, 2004). A person’s misperception of interactions as a result of maladaptive interpersonal affective schemas may develop into etiological depression factors, including social losses (Kendler, Hettema, Butera, Gardner, & Prescott, 2003); inaptitude to take advantage of social support (Brown, Andrews, Harris, Adler, & Bridge, 1986); a tendency toward subservience, as maintained by the social rank theory of depression (Gilbert, 2005); perceived loss of autonomy; and loss of identity (Ehlers, Maercker, & Boos, 2000). Compared to their healthier counterparts, depressed people are less likely to recognize emotions displayed in pictures (Surguladze et al., 2005). They also suffer from a diminished ability to recognize positive emotions and tend to negatively misinterpret facial expressions (Leppanen, Milders, Bell, Terriere, & Hietanen, 2004). Some studies demonstrated that depressed individuals exhibit mood-congruent bias toward facial expression recognition (Newman, Fuqua, Gray, & Simpson 2006), while others found that people suffering from anxiety exhibit such bias in their perception (Bouhuys, Geerts, & Mersch, 1997). Psychological distress significantly contributes to the inability to process emotions and the inclination to interpret neutral facial expressions with a negative bias (Csukly, Czobor, Szily, Takács, & Simon, 2009). Depression impairs the neural processing of happy facial expressions in the core regions of affective facial processing, but this problem can be resolved through treatment (Fu et al., 2007).
As suggested by the findings discussed above, the misperception of facially expressed emotions is correlated with depression and psychiatric distress. The development of negative misperceptions regarding other people’s attitudes and expressions among individuals with depression is driven by negative schemas, as maintained by the cognitive theory of depression (Beck, 1964; Young & Brown, 1990). Schemas are cognitive structures and frameworks, in which a person organizes and processes stimuli and information. EMSs are dysfunctional cognitive patterns that develop during childhood through emotions, memories, and experiences with regard to one’s relationship with others. These schemas may govern a person’s future attitude and perception of others, compel a prejudicial misinterpretation of normal experiences for a dysfunctional favoring of separation or social rejection, and induce misperceptions about other people’s emotions (Lemche, Klann-Delius, Koch, & Joraschky, 2004). Although initially emerging during childhood, EMSs develop through adolescence and become elaborated during one’s lifetime (Young, Klosko, & Weishaar, 2003). Young and Brown (1990) identified 19 EMSs, including beliefs concerning attachment to others, the ability to express valid needs and emotions, autonomy, competence, sense of identity, limit-setting capacity, and self-control. Some researchers suggested that EMSs are strongly associated with personality disorders, mild characterological problems, and axis I disorders, such as depression (Young et al., 2003). On the other hand, scholars also provided more definitive evidence regarding the contribution of EMSs to the development and continuation of depression (Riso et al., 2003). Harris and Curtin (2002), Hoffart et al. (2005), and Schmidt, Joiner, Young, and Telch (1995) used the Young Schema Questionnaire (YSQ) in their cross-sectional studies and found that EMSs can serve as predictors for depression severity. A two-phase study by Riso et al. (2006) revealed moderate to high levels of relative EMS stability (measured with test-retest correlations) in depressed outpatients after the researchers controlled depression severity. They also reported that despite the relative alleviation of the depression levels, the mean score of EMSs remained largely unchanged, even after the exclusion of patients who were not in remission. Halvorsen, Wang, Eisemann, and Waterloo (2009) confirmed that YSQ scales are significant predictors of major depression episodes over a duration as long as 9 years. EMSs can, therefore, serve as factors of vulnerability to depression, both cross-sectionally and longitudinally.
The aforementioned studies implied that the severity of psychopathologic symptoms is negatively correlated with patients’ ability to recognize emotions, especially positive ones. Thus, the maladaptive schemas that underlie misconceptions regarding social reality and impairments in facial expression recognition are both likely to be strongly present in depressed patients. Despite the considerable insights provided by previous studies on maladaptive schemas, however, only Csukly et al. (2011) have investigated the association of these cognitive and emotional patterns with impairments in emotion recognition. Furthermore, the findings of the authors may have been influenced by the fact that the recruited patients received antidepressant medication; antidepressants may help patients develop a positive bias or interpret negative facial expressions as reflective of neutral emotions (Norbury, Mackay, Cowen, Goodwin, & Harmer, 2007). Given the possibility of confounding effects from medication in such studies, we reinvestigated the association between emotion recognition and EMSs in people who showed symptoms of depression but have not been administered with any antidepressant medication. Thus, the objective of the present study was to either confirm or refute the relationship among the aforementioned conditions.
2. Methods
Through purposive sampling, this study selected 18 to 32-year-old male and female students of Shiraz University who were enrolled in BA/S and MA/S programs in the first half of the academic year, 2015 to 2016. The final sample comprised of 100 undergraduate and graduate students (M=22.8, SD=5.72), of which 42 were women (M=24.60, SD=3.44) and 58 were men (M=23.24, SD=3.40). The participants were interviewed by an experienced psychologist, who used a structured clinical interview instrument from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5, 2013). Exclusion criteria included diagnosis of axis 1 disorder, except for depression (determined based on the diagnostic criteria in DSM-5), and a history of drug addiction, physical illness, and neurological disorders, such as epilepsy, any type of brain injury, and mental illness. All examinations involving the human participants were approved by an appropriate ethics committee.
After the subjects signed the consent form, they were interviewed by the experienced psychologist. They were then administered with the test package, which contained forms for filling in basic demographic information, the BDI, the YSQ, the facial affect recognition test, and the corresponding answer sheets.
Schema Questionnaire-Short Form (SQ-SF) is a 75-item questionnaire and was developed by Young (1994) for the evaluation of 15 EMSs. The schemas include the following: Emotional deprivation, Abandonment/ Instability, Mistrust/ Abuse, Social isolation/ Alienation, Defectiveness/ Shame, Failure, Dependence /Incompetence, Vulnerability to harm or illness, Enmeshment/ Undeveloped self, Subjugation, Self-sacrifice, Emotional inhibition, Unrelenting standards/ Hyper criticalness, Entitlement/ Grandiosity, and Insufficient self-control.
Five questions are devoted to each schema, and each question is scored on a 6-point scale (1= Totally false, 6= Quite right”). If the subscale average of a given schema is above 2.5, then the schema is evaluated as inefficient. The reliability and validity of the SQ-SF have been demonstrated in several studies (Oei & Baranoff, 2007), and its validation for the Iranian context was conducted in Tehran universities by Ahi, Mohammadifar, & Besharat (2007). In the current research, the internal consistency of the instrument was 0.97 for the female respondents and 0.98 for the male respondents, as calculated by Cronbach’s alpha. The alpha value of the overall questionnaire was 0.96, and those of the schemas were as follows: Emotional deprivation (0.86), Abandonment /Instability (0.70), Mistrust /Abuse (0.81), Social isolation /Alienation (0.79), Defectiveness /Shame (0.89), Failure (0.89), Dependence /Incompetence (0.84), Vulnerability to illness (0.84), Enmeshment /Undeveloped self (0.77), Subjugation (0.82), Self-sacrifice (0.82), Emotional inhibition (0.78), Unrelenting standards /Hyper criticalness (0.69), Entitlement /Grandiosity (0.78), and Insufficient self-control (0.71).
Beck Depression Inventory (BDI) consists of 21 questions that measure the degree of depression on a 4-point Likert scale. Beck, Street and Garbin (1988) obtained a test-retest reliability coefficient of 0.93 for the instrument over a week’s duration. Goudarzi (2002) also derived appropriate reliability and validity for the Iranian context. The author obtained a reliability of 0.84 on the basis of Cronbach’s alpha calculation for internal consistency and a correlation coefficient of 0.70 on the basis of the split-half method based on odd and couple questions.
By Facial Affect Recognition Task, the participants were tested on their ability to recognize facially expressed emotions from 41 images that measure six emotional states (sadness, happiness, fear, anger, disgust, and surprise) and the neutral state. To adapt this test to the Persian culture, 110 images of facially expressed emotions were first obtained from Ekman and Friesen (1976). The images display the faces of differently aged males and females expressing happiness, sadness, anger, fear, disgust, surprise, and neutral emotions. The images were screened by a 41-person group composed of 19 to 22-year-old clinical psychology students from Shiraz University. With respect to the final 41 images (six images for each emotion, except for fear to which five images were allocated, and six images for the neutral state), more than 85% of the initial screening participants agreed that the emotions related to the images accurately stimulate recognition. There were seven images (six related to emotional states and one to the neutral state) on which subjects had 100% agreement that was considered as the main options (related to the six emotional states and one to the neutral state). On the basis of the screening results, a multiple-choice test with the 41 images was designed. The images of main options, which were laid out on seven 20×30 cm cards, were placed in constant view (front) of the subjects, whereas the other images were displayed consecutively on a handheld computer positioned in front of the subjects. The computer was a 16-inch device with 800×1280 pixel resolution. The presentation of the images was randomly sequenced, but the same number of images was shown to the subjects. After carefully explaining the task procedure to the subjects, they were asked to sit on a comfortable chair and hold the computer at a distance of 40±5 cm. One of the seven images, including the corresponding test options, were shown to a subject, after which one of the other 41 images was displayed on the monitor for 500 ms. After each image was presented, the subjects were given 5 s (Pan et al., 2009) to identify the emotion expressed in the image or identify the picture that showed a similar emotion as that displayed in the target image. The performance of the subjects was measured on the basis of the total number of correct answers.
This research is of cross-sectional design, and the normal distribution of the variables was evaluated using the Shapiro–Wilk test. The P values of all the variables, including the components of emotion recognition from facial expression were significant (P<0.001). These variables were therefore non-normally distributed. Given that the dependent variable (emotion recognition from facial expression) was non-normally distributed and had no distance scale, a linear regression model could not be used. Instead, a binomial distribution was evident given that the variable pertained to the number of positive responses (“yes”) to two binary questions (yes/no questions) regarding emotion recognition from facial expression. Correspondingly, a binomial regression model could be employed.
3. Results
The descriptive findings (means and standard deviations) obtained from the 100 participants are shown in Table 1. Binomial regression is a generalized linear model, wherein a response variable can be obtained from a series of Bernoulli trials or binaries; the implications of these experiments are one of success (Code 1) or failure (Code 0) expressions. A binomial regression model with a logit link function was used to investigate the effects of the EMSs and depression on the recognition of general and individual emotions. The examination was first directed toward the effects of the EMSs and depression on general emotion recognition. Considering that the variable for general emotion recognition was the number of positive responses (“yes”) to 41 binary questions (yes/no questions), the binomial regression model with the logit link function was used. In this modeling, general emotion recognition was adopted as the dependent variable, and the EMSs and depression were incorporated as the independent variables. The results showed that none of the variables exerted a statistically significant effect (P≥0.05) on general emotion recognition from faces.
The model was also used to examine the effects of the EMSs and depression on the recognition of individual emotions. Because the recognition of each emotion was reflected by the number of positive responses to six binary questions, the model was used separately for each emotion. In this modeling, emotion recognition was the dependent variable, and the EMSs and depression variable were entered as the independent variables.
The effects of the EMSs and depression on the recognition of fear were examined. Table 2 lists the variables of the model, along with the regression coefficients, Wald statistics, P values, and Exp (B). Abandonment/ instability, defectiveness/ shame, dependence/ incompetence, vulnerability to harm or illness, subjugation, self-sacrifice, emotional inhibition, insufficient self-control, and depression exerted significant effects (P<0.05) on the recognition of fear, whereas the other EMSs had no statistically significant effects (P≥0.05). The regression coefficient of abandonment/ instability was 2.128, indicating that with a unit increase in the score of abandonment/ instability, the logit value of fear recognition would increase by 2.128 units. This regression coefficient can be interpreted more tangibly on the basis of the Exp (B) column, which indicated that with an increase in the score of abandonment/ instability, the recognition of fear would increase by e2.128 or 8.394 times. The other significant binomial regression coefficients can be interpreted in a similar manner.
Depression exerted a significant effect (P<0.05) on the recognition of sadness, whereas the EMSs had no significant effects (P≥0.05) on the recognition of this emotion and surprise. As shown in Table 3, the regression coefficient of depression is 0.105, indicating that a one-unit increase in the depression score will increase the logit value of sadness recognition by 0.105 units. This regression coefficient can be interpreted on the basis of the Exp (B) column, which indicates that with an increase in the depression score, the recognition of sadness would increase by e0.105 or 1.111 times. The regression coefficient of a variable, such as abandonment/ instability, was greater than that of depression, but because of the large standard error of the coefficient of this schema, its Wald statistic was xxx, and its P-value exceeded 0.05. Thus, abandonment/ instability and the other EMSs exerted non-significant effects on the recognition of sadness. Table 4 shows that mistrust, defectiveness/ shame, vulnerability to illness and depression exerted significant effects (P<0.05) on the recognition of the neutral state, whereas the other variables had no significant effects (P≥0.05). The regression coefficient of vulnerability to illness is –2.134, as presented in Table 4. This result indicates that with a unit increase in the score of vulnerability to illness, and the logit value of the recognition of the neutral state decreased by 2.134 units. On the basis of the Exp (B) column, with an increase in the score of vulnerability to illness, the recognition of the neutral state would increase by e–2.134 or 0.118 times. This finding suggested a negative effect on an individual’s recognition of the neutral state. The other significant binomial regression coefficients can also be interpreted in a similar manner.
Finally, only depression exerted a significant effect (P<0.05) on the recognition of anger; the other variables exerted little effect (P≥0.05) (Table 5). The regression coefficient of depression was 0.067, indicating that with a unit increase in the depression score, the logit value of anger recognition will increase by 0.067 units. On the basis of the Exp (B) column, an increase in the depression scores would increase the recognition of anger by e0.067 or 1.07 times. The regression coefficient of a variable, such as abandonment/ instability, was larger than that of depression, but because of the considerable standard error in the coefficient of the aforementioned schema, its Wald statistic was small and its P value exceeded 0.05. Thus, the effects of this schema and the other EMSs were non-significant. None of the variables exerted a statistically significant effect (P≥0.05) on the recognition of happiness, surprise, and disgust.
4. Discussion
We investigated the relationship of EMSs and depressive symptoms with the recognition of general emotions and facial affects that reflect anger, fear, disgust, happiness, sadness, surprise, and neutrality. The results indicated that the recognition of fear was significantly amplified by abandonment/ instability, defectiveness/ shame, dependence/ incompetence, vulnerability to illness, subjugation, self-sacrifice, emotional deprivation, insufficient self-control, and depression. In contrast, none of the other EMSs exerted a significant effect on fear recognition. Calder, Lawrence, and Young (2001) emphasized on the role of amygdala in the processing of fear-relevant cues, including corresponding facial expressions. Studies appear to agree on the relationship between the enhanced recognition of fear in individuals with a previous history of depression and the suggested role of amygdala in the disorder. Sheline et al. (2001) stated that acutely depressed patients exposed to facial expressions of fear exhibited high activation of the left amygdala. He also reported that antidepressants normalized abnormal amygdala activation in the patients showing remission.
We found that the recognition of neutral state was significantly impaired by mistrust, defectiveness/ shame, vulnerability to illness, and depression. The rest of the EMSs exerted no such effects. Drevets (2001) argued that the elevated physiological activity of the amygdala can explain the tendency of depressed people to misinterpret the emotional meanings attached to emotionally neutral social cues (neutral facial expressions). The processing of emotionally positive signals by depressed individuals can also be impaired by dysfunction in reward systems (Sloan, Strauss, Quirk, & Sajatovic, 1997). Considering the association of depression with elevated amygdala activity, alongside evidence suggesting the inability of depressed people to modulate their emotional responses (Drevets, 2001) and their inclination to misinterpret neutral expressions as sad expressions (Gur et al., 1992), one can argue that people with depression may have an impaired ability to recognize neutral facial expressions as such.
We found that the ability of the current study’s participants to recognize sadness and anger was significantly amplified by depression. Research has suggested that major depression is associated with selective attention bias in favor of negative emotional stimuli, such as sadness, loss, and failure, and negative cognitions, such as worthlessness, hopelessness, and self-criticism; such bias results in the perception of external stimuli, such as facial expressions, as more negative than normal (Schaefer, Baumann, Rich, Luckenbaugh, & Zarate, 2010).
Our results showed that depression enhanced the recognition of anger. Anger is closely associated with depression in entire populations (Rimes & Watkins, 2005) because it can be simply directed toward the self and cause anxiety (Newman et al., 2006). To illuminate this issue further, Wright et al. (2009) elucidated that when depressed women were asked to classify facial emotional expressions, they often misunderstood the expression of fear and sadness as anger. Jollant et al. (2008) reported that depressed men who have had attempted suicide were more sensitive to angry faces than those who have not attempted suicide. Douglas and Porter (2010) stated that in people with severe depression, the ability to differentiate anger in facial expressions becomes impaired, but Douglas, Porter, Knight, & Maruff (2011) suggested that medication can normalize a patient’s ability to correctly identify anger in facial expressions. So anger could be turned into anger rumination and later to depression. When feeling angry, a person who is in a depressed mood relates anger to previous experiences—a behavior that invokes negative thoughts and then develops into anger rumination, sometimes including a desire to feel antipathy toward others and fantasize about revenge. The likelihood of people to engage in stable rumination may be associated with their belief that rumination is useful and presents some advantages (Papageorgiou & Wells, 2004). People regard active rumination as an uncontrollable and harmful habit with undesirable social consequences, and this negative belief can contribute to depression. Thus, depression experience continues in a cycle of rumination, depression, and specific metacognitive beliefs.
In the current work, no statistically significant association was found between the EMSs or depression and the recognition of disgust, surprise, happiness, or general emotions. In contrary to the expectations, normal people did not outperform patients with major depression in recognizing facially expressed emotions. In view of this result, depression cannot be regarded as consistent with the effects of the experimental induction of negative emotions (e.g. sadness). Additionally, our findings refuted the hypothesis on negative mood induction and impaired emotion recognition from positive facial expressions (e.g. happiness) as being necessary stimuli of depression (Milder, Bell, Platt, Serrano, and Runcie, 2010). Disgust refers to the internal urge to avoid an unpleasant, infected, or spoiled object. Almost all cultures share a set of similar facial expressions for certain emotions. In the case of disgust, this emotion is expressed by gaping, wrinkling of the nose, and jutting of the upper lip (Ekman & Friesen, 1976). Thus, the familiarity of this emotion can cause lack of significant differences in recognition by different individuals (Schaefer et al., 2010).
The effects to be expected from impaired emotion recognition include the inability to receive affective support from intimate relationships and the lack of control over social situations. The maladaptive schemas that underlie depression may both contribute to and be reinforced by these effects. Determining the true causal relationship between emotion recognition and maladaptive schemas and their link to depression requires further research, with healthy and euthymic people as controls. Strong evidence supports the correlation between impairments in facial affect recognition and social behavior (Addington, Saeedi, & Addington, 2006) because, in short, a prerequisite to successful social functioning is the ability to properly understand people’s facial expressions (Venn et al., 2004).
The generalizability of our results is limited by this factor that in the natural environment, facial expressions are not static like photographs, but it represents ever-changing events. Some investigators suggested that due to the lack of important dynamic information in the facial photographs, patients need to interpret facial expressions more accurately. It suggested that future studies that make use of videotaped representations of facial expressions of emotions could address this issue (Hargarave, Maddock & Stone, 2002).
The results of our study indicated that in unmedicated subjects with depressive symptoms, social functioning difficulties, maladaptive schemas, and depressive symptoms are reinforced by certain impairments in emotion recognition. Thus, major depression can be characterized, to some extent, by dysfunctional emotion recognition. In people with major depression, dysfunctional schemas and counterproductive attitudes prevent the appropriate processing of life events (Scher, Ingram, & Segal, 2005).
Acknowledgments
This article had no financial sponsors.
Conflict of Interest
The authors declared no conflicts of interest.
References
- Addington, J., Saeedi, H., & Addington, D. (2006). Facial affect recognition: A mediator between cognitive and social functioning in psychosis. Schizophrenia Research, 85(1-3), 142–50. doi: 10.1016/j.schres.2006.03.028
- Ahi, G. H., Mohammadifar, M. A., & Besharat, M. A. (2007). [Reliability and validity of Young's Schema Questionnaire-Short Form (Persian)]. Journal of Psychology and Education Science, 37(3), 5-20.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. Washington, D.C.: American Psychiatric Association.
- Baldwin, M. W., & Dandeneau, S. D. (2004). Understanding and modifying the relational schemas underlying insecurity. In M. W. Baldwin (Ed.), Interpersonal Cognition (pp. 33-61). Guilford Publications.
- Beck, A. T. (1964). Thinking and depression. Archives of General Psychiatry, 10(6), 561. doi: 10.1001/archpsyc.1964.01720240015003
- Beck, A. T., Rush, A. J., Shaw, B. F., & Emery, G. (1979). Cognitive therapy of depression. New York: Guilford Press.
- Beck, A. T., Steer, R. A., & Carbin, M. G. (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review, 8(1), 77–100. doi: 10.1016/0272-7358(88)90050-5
- Bouhuys, A., Geerts, E., & Mersch, P. P. (1997). Relationship between perception of facial emotions and anxiety in clinical depression: does anxiety-related perception predict persistence of depression? Journal of Affective Disorders, 43(3), 213–223. doi: 10.1016/s0165-0327(97)01432-8
- Bowlby, J. (1980). Loss: Sadness and depression (No. 3). London: Hogarth Press.
- Brown, G. W., & Harris, T. (1978). Social origins of depression. London: Tavistock.
- Brown, G. W., Andrews, B., Harris, T., Adler, Z., & Bridge, L. (1986). Social support, self-esteem and depression. Psychological Medicine, 16(4), 813-31. doi: 10.1017/s0033291700011831
- Brown, G. W., Harris, T. O., & Hepworth, C. (1995). Loss, humiliation and entrapment among women developing depression: A patient and non-patient comparison. Psychological Medicine, 25(1), 7-21. doi: 10.1017/s003329170002804x
- Calder, A. J., Lawrence, A. D., & Young, A. W. (2001). Neuropsychology of fear and loathing. Nature Reviews Neuroscience, 2(5), 352–63. doi: 10.1038/35072584
- Csukly, G., Czobor, P., Szily, E., Takács, B., & Simon, L. (2009). Facial expression recognition in depressed subjects. The Journal of Nervous and Mental Disease, 197(2), 98–103. doi: 10.1097/nmd.0b013e3181923f82
- Csukly, G., Telek, R., Filipovits, D., Takács, B., Unoka, Z., & Simon, L. (2011). What is the relationship between the recognition of emotions and core beliefs: Associations between the recognition of emotions in facial expressions and the maladaptive schemas in depressed patients. Journal of Behavior Therapy and Experimental Psychiatry, 42(1), 129–37. doi: 10.1016/j.jbtep.2010.08.003
- Douglas, K. M., & Porter, R. J. (2010). Recognition of disgusted facial expressions in severe depression. British Journal of Psychiatry, 197(2), 156–7. doi: 10.1192/bjp.bp.110.078113
- Douglas, K. M., Porter, R. J., Knight, R. G., & Maruff, P. (2011). Neuropsychological changes and treatment response in severe depression. British Journal of Psychiatry, 198(2), 115–22. doi: 10.1192/bjp.bp.110.080713
- Drevets, W. C. (2001). Neuroimaging and neuropathological studies of depression: implications for the cognitive-emotional features of mood disorders. Current Opinion in Neurobiology, 11(2), 240–249. doi: 10.1016/s0959-4388(00)00203-8
- Ehlers, A., Maercker, A., & Boos, A. (2000). Posttraumatic stress disorder following political imprisonment: The role of mental defeat, alienation, and perceived permanent change. Journal of Abnormal Psychology, 109(1), 45–55. doi: 10.1037/0021-843x.109.1.45
- Ekman, P., & Friesen, W. (1976). Photographs of facial a ff ect recognition test consulting. Palo Alto: Psychologists Press.
- Fonagy, P., Gergely, G., Jurist, E., & Target, M. (2002). Affect-regulation, mentalization, and the development of the self. New York: Other Press.
- Fu, C. H. Y., Williams, S. C. R., Brammer, M. J., Suckling, J., Kim, J., Cleare, A. J., et al. (2007). Neural responses to happy facial expressions in major depression following antidepressant treatment. American Journal of Psychiatry, 164(4), 599–607. doi: 10.1176/ajp.2007.164.4.599
- Gergely, G., & Unoka, Z. (2008). Attachment, affect-regulation, and mentalization: The developmental origins of the representational affective self. In C. Sharp, P. Fonagy, & I. Goodyer (Eds.), Social cognition and developmental psychopathology (pp. 305-42). Oxford: Oxford University Press. doi: 10.1093/med/9780198569183.003.0011
- Gilbert, P. (2005). Evolution and depression: Issues and implications. Psychological Medicine, 36(3), 287. doi: 10.1017/s0033291705006112
- Gilboa Schechtman, E., Erhard Weiss, D., & Jeczemien, P. (2002). Interpersonal deficits meet cognitive biases: Memory for facial expressions in depressed and anxious men and women. Psychiatry Research, 113(3), 279–93. doi: 10.1016/s0165-1781(02)00266-4
- Goudarzi, M. A. (2000). [Reliability and validity of Beck Depression Inventory in students of Shiraz University (Persian)]. Journal of Social Science of Shiraz University, 18(2), 26-39.
- Gur, R. C., Erwin, R. J., Gur, R. E., Zwil, A. S., Heimberg, C., & Kraemer, H. C. (1992). Facial emotion discrimination: II. Behavioral findings in depression. Psychiatry Research, 42(3), 241–51. doi: 10.1016/0165-1781(92)90116-k
- Halvorsen, M., Wang, C. E., Eisemann, M., & Waterloo, K. (2009). Dysfunctional attitudes and early maladaptive schemas as predictors of depression: A 9-year follow-up study. Cognitive Therapy and Research, 34(4), 368–79. doi: 10.1007/s10608-009-9259-5
- Hargrave. R., Maddock. R. J., Stone, V. (2002). Impaired Recognition of Facial Expressions of Emotion in Alzheimer's Disease. Journal of Neuropsychiatry & Clinical Neurosciences, 14(1), 64-71. doi: 10.1176/jnp.14.1.64
- Harmer, C. J., Bhagwagar, Z., Perrett, D. I., Völlm, B. A., Cowen, P. J., & Goodwin, G. M. (2003). Acute SSRI administration affects the processing of social cues in healthy volunteers. Neuropsychopharmacology, 28(1), 148–52. doi: 10.1038/sj.npp.1300004
- Harmer, C. J., Hill, S. A., Taylor, M. J., Cowen, P. J., & Goodwin, G. M. (2003). Toward a neuropsychological theory of antidepressant drug action: increase in positive emotional bias after potentiation of norepinephrine activity. American Journal of Psychiatry, 160(5), 990–2. doi: 10.1176/appi.ajp.160.5.990
- Harris, A. E., & Curtin, L. (2002). Parental perceptions, early maladaptive schemas, and depressive symptoms in young adults. Cognitive Therapy and Research, 26(3), 405–16. doi: 10.1023/a:1016085112981
- Hoffart, A., Sexton, H., Hedley, L. M., Wang, C. E., Holthe, H., Haugum, J. A., et al. (2005). The structure of maladaptive schemas: A confirmatory factor analysis and a psychometric evaluation of factor-derived scales. Cognitive Therapy and Research, 29(6), 627–44. doi: 10.1007/s10608-005-9630-0
- Jollant, F., Lawrence, N. S., Giampietro, V., Brammer, M. J., Fullana, M. A., Drapier, D., et al. (2008). Orbitofrontal cortex response to angry faces in men with histories of suicide attempts. American Journal of Psychiatry, 165(6), 740–8. doi: 10.1176/appi.ajp.2008.07081239
- Keedwell, P. A., Andrew, C., Williams, S. C. R., Brammer, M. J., & Phillips, M. L. (2005). The neural correlates of anhedonia in major depressive disorder. Biological Psychiatry, 58(11), 843–53. doi: 10.1016/j.biopsych.2005.05.019
- Kendler, K. S., Hettema, J. M., Butera, F., Gardner, C. O., & Prescott, C. A. (2003). Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Archives of General Psychiatry, 60(8), 789. doi: 10.1001/archpsyc.60.8.789
- Lemche, E., Klann Delius, G., Koch, R., & Joraschky, P. (2004). Mentalizing language development in a longitudinal attachment sample: implications for alexithymia. Psychotherapy and Psychosomatics, 73(6), 366–74. doi: 10.1159/000080390
- Leppänen, J. M., Milders, M., Bell, J. S., Terriere, E., & Hietanen, J. K. (2004). Depression biases the recognition of emotionally neutral faces. Psychiatry Research, 128(2), 123–33. doi: 10.1016/j.psychres.2004.05.020
- Milders, M., Bell, S., Platt, J., Serrano, R., & Runcie, O. (2010). Stable expression recognition abnormalities in unipolar depression. Psychiatry Research, 179(1), 38–42. doi: 10.1016/j.psychres.2009.05.015
- Newman, J. L., Fuqua, D. R., Gray, E. A., & Simpson, D. B. (2006). Gender differences in the relationship of anger and depression in a clinical sample. Journal of Counseling & Development, 84(2), 157–62. doi: 10.1002/j.1556-6678.2006.tb00391.x
- Norbury, R., Mackay, C. E., Cowen, P. J., Goodwin, G. M., & Harmer, C. J. (2007). Short-term antidepressant treatment and facial processing. British Journal of Psychiatry, 190(6), 531–2. doi: 10.1192/bjp.bp.106.031393
- Oei, T. P. S., & Baranoff, J. (2007). Young schema questionnaire: Review of psychometric and measurement issues. Australian Journal of Psychology, 59(2), 78–86. doi: 10.1080/00049530601148397
- Pan, Y., Tarczy-Hornoch, K., Cotter, S. A., Wen, G., Borchert, M. S., Azen, S. P., et al. (2009). Visual Acuity Norms in Pre-School Children: The Multi-Ethnic Pediatric Eye Disease Study. Optometry and Vision Science, 86(6), 607–612. doi: 10.1097/opx.0b013e3181a76e55
- Papageorgiou, C., & Wells, A. (2004). Nature, functions, and beliefs about depressive rumination. In C. Papageorgior & A. Wells (Eds.), Depressive rumination: Nature, theory and treatment. Hoboken, N. J.: John Wiley & Sons. doi: 10.1002/9780470713853.ch1
- Petrocelli, J. V., Glaser, B. A., Calhoun, G. B., & Campbell, L. F. (2001). Cognitive schemas as mediating variables of the relationship between the self-defeating personality and depression. Journal of Psychopathology and Behavioral Assessment, 23(3), 183–91. doi: 10.1023/a:1010969321426
- Platts, H., Tyson, M., & Mason, O. (2002). Adult attachment style and core beliefs: Are they linked. Clinical Psychology & Psychotherapy, 9(5), 332–48. doi: 10.1002/cpp.3450
- Raubenheimer, J. (2004). An item selection procedure to maximise scale reliability and validity. South African Journal of Industrial Psychology, 30(4), 59-64. doi: 10.4102/sajip.v30i4.168
- Rimes, K. A., & Watkins, E. (2005). The effects of self-focused rumination on global negative self-judgements in depression. Behaviour Research and Therapy, 43(12), 1673–81. doi: 10.1016/j.brat.2004.12.002
- Riso, L. P., du Toit, P. L., Blandino, J. A., Penna, S., Dacey, S., Duin, J. S., et al. (2003). Cognitive aspects of chronic depression. Journal of Abnormal Psychology, 112(1), 72–80. doi: 10.1037/0021-843x.112.1.72
- Riso, L. P., Froman, S. E., Raouf, M., Gable, P., Maddux, R. E., Turini-Santorelli, N., et al. (2006). The long-term stability of early maladaptive schemas. Cognitive Therapy and Research, 30(4), 515–29. doi: 10.1007/s10608-006-9015-z
- Rubinow, D. R., & Post, R. M. (1992). Impaired recognition of affect in facial expression in depressed patients. Biological Psychiatry, 31(9), 947–53. doi: 10.1016/0006-3223(92)90120-o
- Schaefer, K. L., Baumann, J., Rich, B. A., Luckenbaugh, D. A., & Zarate, C. A. (2010). Perception of facial emotion in adults with bipolar or unipolar depression and controls. Journal of Psychiatric Research, 44(16), 1229–35. doi: 10.1016/j.jpsychires.2010.04.024
- Scher, C. D., Ingram, R. E., & Segal, Z. V. (2005). Cognitive reactivity and vulnerability: Empirical evaluation of construct activation and cognitive diatheses in unipolar depression. Clinical Psychology Review, 25(4), 487–510. doi: 10.1016/j.cpr.2005.01.005
- Schmidt, N. B., Joiner, T. E., Young, J. E., & Telch, M. J. (1995). The schema questionnaire: Investigation of psychometric properties and the hierarchical structure of a measure of maladaptive schemas. Cognitive Therapy and Research, 19(3), 295–321. doi: 10.1007/bf02230402
- Shaver, P. R., Schachner, D. A., & Mikulincer, M. (2005). Attachment style, excessive reassurance seeking, relationship processes, and depression. Personality and Social Psychology Bulletin, 31(3), 343–59. doi: 10.1177/0146167204271709
- Sheline, Y. I., Barch, D. M., Donnelly, J. M., Ollinger, J. M., Snyder, A. Z., & Mintun, M. A. (2001). Increased amygdala response to masked emotional faces in depressed subjects resolves with antidepressant treatment: An fMRI study. Biological Psychiatry, 50(9), 651–8. doi: 10.1016/s0006-3223(01)01263-x
- Sloan, D. M., Strauss, M. E., Quirk, S. W., & Sajatovic, M. (1997). Subjective and expressive emotional responses in depression1. Journal of Affective Disorders, 46(2), 135-41. doi: 10.1016/s0165-0327(97)00097-9
- Surguladze, S., Brammer, M. J., Keedwell, P., Giampietro, V., Young, A. W., Travis, M. J., et al. (2005). A differential pattern of neural response toward sad versus happy facial expressions in major depressive disorder. Biological Psychiatry, 57(3), 201–9. doi: 10.1016/j.biopsych.2004.10.028
- Venn, H. R., Gray, J. M., Montagne, B., Murray, L. K., Michael Burt, D., Frigerio, E., et al. (2004). Perception of facial expressions of emotion in bipolar disorder. Bipolar Disorders, 6(4), 286–93. doi: 10.1111/j.1399-5618.2004.00121.x
- Wright, S. L., Langenecker, S. A., Deldin, P. J., Rapport, L. J., Nielson, K. A., Kade, A. M., et al. (2009). Gender-specific disruptions in emotion processing in younger adults with depression. Depression and Anxiety, 26(2), 182–9. doi: 10.1002/da.20502
- Young, J. E. (1994). Practitioner's resource series. Cognitive therapy for personality disorders: A schema-focused approach (Rev. ed.). Sarasota, FL: Professional Resource Press.
- Young, J. E., & Brown, G. (1990). Young schema questionnaire. New York: Cognitive Therapy Centre of New York.
- Young, J. E., Klosko, J. S., & Weishaar, M. E. (2003). Schema therapy: A practitioner's guide. New York: Guilford Press.
Type of Study: Research |
Subject:
Approach to biological neural
Received: 2017/04/27 | Accepted: 2017/10/30 | Published: 2018/04/1
Received: 2017/04/27 | Accepted: 2017/10/30 | Published: 2018/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |